Zackary Sholem Berger's Blog, page 26
May 28, 2013
Five things that should be said
Five things I wished I said more often:
1. Look, it’s near the end of the day and I’m stressed. Can you remind me to slow down and listen?
2. Just because I am a radical skeptic when it comes to the utility of many tests doesn’t mean I don’t care about your symptoms.
3. Put your cell phone away, please.
4. Tell me something about yourself that doesn’t have anything to do with your illness.
5. What sort of person are you really, deep down?
May 20, 2013
送别王医生 Au revoir to the visiting Dr. Wang
For the past few months, our Johns Hopkins Division of General Internal Medicine has hosted an internist from Peking Union Medical College Hospital, Dr. Yu Wang [also on Weibo]. She leaves at the end of May. The aim is to help foster a relationship between our two institutions; UCSF and PUMCH are already working together. While I am no expert about the Chinese health system, I wanted to share some of what I learned from her during her visit.
PUMCH is a tertiary care hospital, similar to Hopkins. But while Hopkins has recently taken the bit of primary care in its teeth, PUMCH, says Dr. Wang, is not about to make that its priority. Rather, the Chinese government has apparently launched an initiative to train tens of thousands of new primary care providers across the country. (Johns Hopkins is newly involved in training some of these at Sun Yat-Sen University.)
When Dr. Wang discharges a patient from PUMCH, she gives them a detailed discharge summary to take to the doctor they next see – not their primary care doctor, because they don’t have one. Nor can she expect that they take the medications recommended for them during their stay in the hospital, because most medications, she says, are paid for out of pocket in China.
I am planning a trip to China to visit PUMCH and I hope to have some first-person impressions then. Meanwhile, I hope to find some general sources about the Chinese health care system to enlighten me. A colleague of Dr. Wang’s, in the emergency department at PUMCH, is also on Weibo, and once I sign up for the service, I look forward to learning more about health care in China.
Thank you, Dr. Wang, for your visit and for helping connect our two institutions!
May 13, 2013
What’s your problem? What makes a diagnosis
There has been controversy lately over the new edition of the American Psychiatric Association’s new version of their Diagnostic and Statistical Manual (DSM 5). Among a number of critiques, the most-forwarded on the Internet seeems to be that of the National Institute of Mental Health, which recommended that researchers applying for grants not use the DSM 5 – because, rather than classify diseases and diagnoses based on etiology, it does so based on symptomatology.
The narrative that the psychiatrists are trying to write is a triumphal progression from anecdote to empiricism, from Freud’s couch to the colorful images of the fMRI. 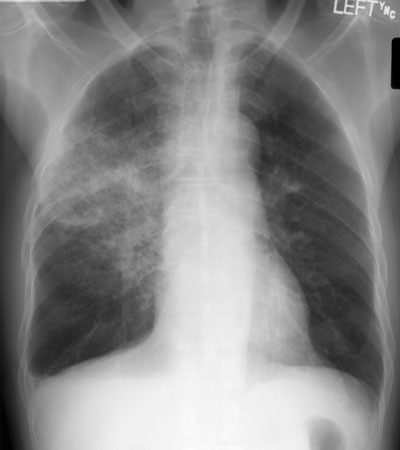
Unfortunately, the example psychiatrists would like to follow – medicine – is not as simple as all that. When we diagnose, we often apply a heuristic which relies not just on results of tests and images but also on the patients’ symptomatic report. Call it “bacterial pneumonia” all you want, but a patient without symptoms can’t be diagnosed with pneumonia even if there’s an infiltrate on the X-ray – and even if a patient is symptomatic, we don’t go and culture the bacteria from the lung tissue except in relatively serious circumstances. The point here is not the details of what makes a pneumonia, merely that we do not have a magic on-off switch within the body that we can examine when making a diagnosis. Psychiatrists know this as much as we do, which is why (to internists’ secret shame) we don’t have anything like a unified diagnostic and statistical manual – and if we did, it would be just as controversial as the DSM.
May 6, 2013
What can and can’t be changed
I am a skeptic by nature. More often than not, however, skepticism has to be suspended to take good care of patients. Many is the time that a person has sworn up and down that they are ready to take the next step in behavioral change. For example, I am not a haranguer, but no matter how subtle I try to be, it’s rare for a patient not to pick up the very clear message that they should quit smoking. People have heard often enough that they should do so.
They come to my office with a natural instinct, to make me happy – and thus they tell me they are going to quit. Or if they aren’t really ready, they feel bad about saying it right out, so they don’t come to that statement right away but save it for later. If they tell me they are going to quit, though, I am duty bound by something older than the Hippocratic oath to say Yes you can! and support them. In other words, I must put aside my skepticism for a moment and believe in the possibility of change.
Then, of course, I realize time and again that I make mistakes in my practice. Despite the ever-present excuse of inertia, I need to believe that I can get better, as well as the system I am a part of.
Believing in the possibility of my change can reinforce my optimism that my patients can change their own lives for the better, with my help.
April 22, 2013
On hot seas of blue cobalt
Herring Barrels
Dvoyre Fogel (1934)
Round like the world, like the city
five hooped barrels of herring
in the grocer’s
at 22 BROAD STREET.
Five round wooden barrels
of fat gray salted herring.
50 GROSCHEN EACH
JOSHUA SCHIMMELS
FAT HERRING
50 GROSCHEN EACH

And on faraway glassy seas
narrow ships loaded with fish
— fish gray and velvety like an autumn sky –
ships cool, blue, the faraway
of resigned steely landscapes
And on hot seas
of blue cobalt and ultramarine
ships loaded with oranges
meaty bananas and humid dates
Ships from brass landscapes
where the sun is a great metal ingot
where on streets elastic like gold foil
everything is for the first time and urgent.
Fantastic and out of nothing
like old world-weary bananas. Like oranges.
Like people who’ve gambled away their constellations.
My translation from the Yiddish (original here). Originally published in Eleven Eleven.
April 15, 2013
Submission to a higher power
I’ve picked a vocation (physician) and avocation (poet) which have a lot in common. Here I’ll leave aside the rareified literary and spiritual aspects and talk instead about the practicalities of self-promotion: getting stuff out there, submitting the carefully polished pantoum*or the clever villanelle – or the report of a study which one slaved over for years.
The two venues, the scientific journal on the one hand and the literary journal on the other, each have something to teach us about the best way editors and writers can interact. (They have plenty to tell us about the worst ways, too, but let me be positive today.)
Poetry journals…
usually acknowledge explicitly that their decisions on acceptance or rejection are by necessity made subjectively. Not laboring under the scientist’s delusion that they are pure empiricists, they are cheerfully prepared to admit that a lot of acceptance is luck.
thus differ one from another in matters of style as much as strict criteria of quality.
usually have frequent special issues with interesting and well-known guest editors.
throw launch parties with snacks

Scientific journals, for their part
provide, through their reviewers, copious and often helpful comments on the submission.
are conveniently searchable through well-indexed databases (providing you are an academic with access to them)
cater to an international audience
are at least supposed to consider submissions while blinded to the authors’ identities
The best journals in both categories should combine all these virtues…what do you think?
*which I’ve never written
April 8, 2013
Patient safety and suppositions
On Friday I went to the Maryland Patient Safety Conference as one of the Armstrong Institute clinical patient safety fellows. I missed Rudy Giuliani’s keynote because I was busy taking care of patients in the hospital. Rudy, of course, is a well known patient-safety expert. Or at least I hope so, because I doubt he spoke for free.
What I did catch, though, were two very interesting talks on aspects of safety and quality which are near and dear to me. Keith Berge of the Mayo Clinic spoke about opioid diversion. Opioids are among the most commonly prescribed medications, and they have street value. Thus they are stolen, oftentimes by health care workers. Sometimes those health care workers are our patients too.
Berge’s presentation was remarkable for its unvarnished, pithy, piquant quality: stories of prostheses used to provide clean urine for witnessed drug tests; mug shots of convicted felons now serving jail time. “Some people say, you are criminalizing a medical problem [of addiction],” he said. “I say, you are medicalizing a criminal problem!”
Both are true, of course: criminal liability must be prosecuted but does that not limit the responsibility of the provider to understand the disease of addiction. In my setting, Johns Hopkins, we need to find those who are diverting opioids but at the same time we need to (a) find help for those addicted, (b) write fewer prescriptions in cases when the medicines don’t work and (c) not ignore pain treatment as we try and address substance abuse.
The second talk was by Jason Wolf, an organizational development specialist and a masterful user of anecdote. Patients, he claimed, are now the masters of the health care system, because they have the power of choice. Leave aside the naivete (many patients have no power to choose anything, much less health care). Wolf’s idea is that health care organizations can flourish in the market only if they provide patients with unforgettable experiences through superlative customer service. He told a couple of stories to this effect. A nurse goes out of her way to escort a patient on discharge to his car, even when the patient forgets where his car is and then the car happens to be parked in by another car. When the nurse finally returns to her unit, she is applauded for going the extra mile. Stories like these make you wonder: what about all the sick patients who need taken care of when the team is a man (or woman) down? Doesn’t safety and reliability matter as much as superior service?
When you’re at a big conference, you feel the crowd around you swept up by these talks, and you try to find the nuggets of useful information among the questionable suppositions.
March 25, 2013
Redemption and freedom
If you’re a religious Jew with some insight into the burdensome nature of the commandments – I mean, look at the way other people live who aren’t saddled by these ancient texts, how they can be perfectly fulfilled, satisfied, enriched, and moral too! – you wonder, some of the time, what the point is. A major holiday like Passover doesn’t make this conundrum go away, but it does place it in context. We were brought out of Egypt to redeem humanity: Jews, sure, but every other people as well, and every person. It’s just that to be a member of a people provides you a tool box to make that redemptive possibility concrete. Modernity means that any individual, no matter who they are, can make their own tools – which has its benefits and downsides.
It’s a powerful but strange box, no matter how it makes its way to you. Anyone can open it. The tools are sharp as the day they were made; they can be put to use right away. But they bear the nicks of previous generations. With use, the tools themselves are changed.
What is made with these tools after all? Every person fashions something different. And in that fashioning, the tools fulfill their true purpose.
March 18, 2013
The second time as farce: a medical student’s note from 2005
This summer will mark ten years since this blog first toddled onto the Internet. There have been many good things about writing it. As a doctor and academic, my every move sometimes feels constrained by protocol and specific aim. What a pleasure to write on occasion about something which moves me, strikes my fancy, or is worthwhile to say, without regard to immediate benefit, evidence-basedness, or fundability!
Once in a while, then, I’ll repost something I blogged a while ago. Here then is a piece I wrote in 2005, in the column about being a medical student that once ran in the Forward under the name Medicine Mensch. Did it age well?
Medicine Mensch goes (Poly)Glatt
Number seven in a series.
Visiting Patients, With Dictionary In Hand
By Zackary Sholem Berger
July 1, 2005
Before I became a medical student, I thought I spoke Spanish pretty well. I spent six months after college researching minority languages in Spain and, after moving to New York, I’ve had many a friendly conversation with miscellaneous Spanish speakers I’ve accosted: random passersby from Puerto Rico, law students from Colombia, grocery packers from the Dominican Republic.
Having a conversation on the street or a chat in a café about politics or literature is one thing. If you don’t understand a word, you can smile or nod and pick up from context what’s going on. But say you’ve been called down to the E.R. to take a history and do a physical, and you find a drunk, toothless man in handcuffs gesturing frantically at something underneath his bed. If you could understand drunken, toothless Spanish a little bit better, it might not take you 15 minutes of sympathetic listening to understand that the man wants his cell phone (which the cops sitting nearby are not about to let him have).
The difficulty isn’t simply a matter of decoding the speaker’s register (someone from a different socioeconomic class can be hard to understand, even in one’s native tongue), nor is it the fact that various dialects of the language are represented at any urban hospital. It’s often the words themselves that make things hard. Like every other medical student, I have a command of several different kinds of medical terminology: the mind-numbing jargon of the scientific literature, the half-macho talk of rounds and last but certainly not least important, the normal words people use to talk in English about whatever’s the matter with them.
It’s this last kind of vocabulary that I lack in Spanish. I can talk a blue streak about genetic predispositions and infectious agents, about endoscopies and anesthesia — these are international terms, much the same in Spanish, English and many other languages. But lay language is different. I’ve already experienced a certain kind of linguistic blockage more than once. I’ve started a conversation with a Spanish-speaking patient, we’ve built up something of a rapport, she’s complimented my Spanish, I’ve figured out why she’s come to the hospital. Then, all of a sudden, I need to ask a specific question to narrow down the field of possible diagnoses. I use what I think is the right word, and one of two expressions appears on the patient’s face: either outright incomprehension, or a polite glazed-over look that means, “I’m going to keep my mouth shut until I can figure out what the heck this nice doctor is saying.” It’s then that I have to search my dusty old neurons for a Spanish word I learned once, many years ago, or for a synonym that’s used in the home country of this particular patient. During one memorable conversation, a patient and I sat through a long, awkward pause before she figured out that I was asking about her period.
Those familiar with the overscheduled life of the medical professional might wonder what’s the point of trying to achieve “medical fluency” in Spanish or another foreign language. For most doctors it might be enough to master a minimal vocabulary, and the extra minutes spent figuring out the Colombian word for “tampon” or “leg splint” can more profitably be devoted to a more extensive history or exam of the other dozen patients that have to be seen today. It’s also true that a translator is (usually) available. That’s if one wants to take the legal route. Many doctors use the Spanish-speaking janitor, or the patient’s sister who’s waiting in the lobby; neither alternative would be applauded by medical ethicists.
It all depends on how the doctor sees her practice. If her task is to see clients who are visiting for necessary medical services, they probably can be more efficiently served (not to say “processed”) with minimal communication. Many common complaints can be divined from the patient’s presentation and demographic with only the bare outlines of a conversation. If this approach isn’t warm and personal, it’s certainly necessary when there are hundreds of patients to see in a week.
But since I’m still a medical student, I can still afford to let my personal tendencies influence the way I see medicine. I’m a person who doesn’t mind sacrificing a little efficiency (or even a lot) to get a good conversation going with the person sitting in front of me. Will that make me a better doctor? Beats me, but I know I’ll have more fun this way.
“You can’t learn every language,” a medical student friend of mine pointed out when she heard about my linguistic ambitions, i.e., trying to learn some Chinese. Many people at Bellevue know some stock Chinese phrases, but if I can avoid it I’d rather not storm into the hospital room of an 80-year old man and blurt out the Chinese version of “Did you piss today?” Most medical students wouldn’t be caught dead asking an older person that question in English; clearly there must be another way to do it in Chinese. And I’m still trying to find the Yiddish speaker who doesn’t assume that accented English will impress me more than mameloshn.
If you happen to speak English, I will make every effort to accommodate you once I’m a physician. Please realize, though, that since I’ll be a doctor, my handwriting will be illegible — in any language.
Still a medical student, Zackary Sholem Berger has a bunch of dictionaries at home, but he never can seem to remember the word he needs. When he’s a physician himself, he can have a medical student look everything up for him. Send him questions in the language of your choice at doctor@forward.com .
March 11, 2013
Gaining on translation
This blog is bilingual. Yiddish is the language on the other side of the blogwall (if this web page smells of garlic, that’s the reason). Sure I have a love for languages in general; there’s a close link between my fascination with what people speak and my research into how people talk to their doctors. More details on that score in my book of a similar title.
But there might be an even closer link between translation and medicine. The philosopher W.V.O. Quine pointed out that there is no one perfect mapping of my words in English, say, into a set of words in Japanese that mean exactly the same thing. Translation, in his words, is indeterminate.
Something similar happens in the doctor-patient conversation. It is very rare (or impossible?) for the two members of that pair to say the same words in the same way to refer to the same health issue.
The way out of this conundrum is probably the same one that working translators take. Just as there is no perfect translation, only different attempts at it, there is no perfect conversation, much less between a doctor and a patient.
The translator tries to produce a work of art which elicits a sought-after effect. Similarly, doctor and patient should seek to improve communication not to get the techniques perfect, but to achieve healthy aims.



