Zackary Sholem Berger's Blog, page 19
September 16, 2013
Doctor Yogi
My wife went to a good yoga class the other day. (It was on Yom Kippur, actually – not the most typical yoga class.) I asked my wife what qualities make for a good yoga instructor, and this is what she came up with:
Clarity
Flow
Pacing
Explanation
Kindness
I am biased, of course, but I think that this list summarizes the essential qualities of many different guides, including doctors, nurses, et al.
You can also interpret these terms in various ways. Clarity can be a quality of the practitioner themselves – someone who is transparent, easily read – or of their speech. Flow refers to the transition between parts of the visit, and pacing – to a perception of the patient (or yoga student) as much as to any objective rate. Explanation and kindness, of course, are less susceptible to interpretation.
According to that comparison, we should aim for someone to feel as refreshed and challenged coming out of the health care provider’s office as they do when leaving the yoga studio, meditation space, or house of prayer.
September 12, 2013
How do you like your visit flipped?
Cross-posted you know where.
Lately I ‘ve seen a lot about “flipping the visit.” Presumably that means this: the doctor has been in the driver’s seat for far too long with the patient looking on bemused, confused, and bamboozled. Switch it around! Put the patient in the driver’s seat. 
Except – wait. Is the patient treating the physician? Probably not. The patient is treating themselves! Lovely. So the physician…?
Right, right, we are talking shared decision making. There are two parties to the conversation.
So flipping, perhaps, is not the right way to think about it. We need to come to the visit with the mind of an interior designer. Put the couch over there and get rid of that hideous, unnecessary wall.
In this modified metaphor, who are the clients? Just the patient. She might want the doctor across the room, giving advice after a decision has been made; sitting at the table, sorting through the data with her; or perhaps down the hall, answering queries by email while she lounges at her leisure in her bathrobe, looking at open notes.
Meta-preferences – how the patient wants the visit to be organized, what level of involvement she prefers for the physician, what she wants to get out of any given visit – are more important than is commonly realized. Neat switcheroos like “flipping the visit” are convenient mnemonics for patient-centering our system, but don’t get at what individuals really want. Because that we won’t know till we actually ask them.
September 11, 2013
Elements of chronic pain are often overlooked
I think everyone who sees patients, and treats a lot of them with a particular condition, comes to see that condition as a microcosm of all of medicine. And that’s the way with me and pain. For some reason—perhaps it’s because I tend to see these patients more frequently than others—I think I have more of them.
Pain, and I mean here chronic pain, has certain characteristics which are shared with many other chronic diseases. Such elements of illness are often overlooked, and focusing on the forms they take in pain might be useful in conceptualizing them.
Check out a post of mine at the ACP Internist Blog.
September 10, 2013
An Attitude to Life, or: “the pathetic inadequacy of our knowledge” (more from David Mendel’s “Proper Doctoring”)
Do you agree with the following? In the face of unavoidable uncertainty, should providers and patients be unfailingly optimistic?
We are not very good at forecasting outcome. Firstly there is the range of severity within a particular disease. Then there is the variation in human response to disease, both physical and psychological. The will to fight the disease can lead to “miracles”of survival. Finally there are the errors of diagnosis, coupled with the pathetic inadequacy of our knowledge. The world is full of eighty-year-old aunties who were told that they had “weak chests” and that they would not live a normal lifespan. Modern equivalents of weak chests abound. The diagnoses are more precise, but the acuracy of prognosis is about the same. In the individual patient who conronts you [or as you yourself, as patient, confront your disease! -- ZB], in the face of all these likelihoods and possibilities, optimism seems to be the most rational approach. it is certainty the most fruitful and least harmful.
I edited the quote to make it relevant to today’s patient-centered culture, certainly a salutary change from thirty years ago when Mendel wrote his book.
September 9, 2013
Continuing, or advancing, the transformation of American health care
On a weekend trip to Baltimore’s reductio ad freedonium of a used bookstore, a k a The Book Thing, a warehouse full of books that are yours for the taking, I finally got my hands on The Social Transformation of American Medicine. It’s a classic for its sociologic description of how American medicine got this way: physicians managing to hold onto their control by dint of social and economic power. The book is 30 years old but its conclusions are still spot on.
As with any great work of history, the reader wonders if the clock can be turned back without sacrficing what we have gained. It used to be, shows Starr, that sickness was treated at home; laypeople acted as their own practitioners; and physicians had difficulty maintaining the social prestige that enabled them to set their own fees and wall off outsiders from their guild.
Of course, we wouldn’t like to return to all of this. But we could imagine a health care system which involves a multiplicity of certified, qualified providers, and a greater inclusion of common sense which recognizes that for some common and nonserious conditions, a layperson can treat herself at home without any advanced imaging at all.
Can we get there from here?
September 6, 2013
Help me, I’m deciding
Reposted from January. The panel referred to is still meeting, and we are working on its final report. Stay tuned!
I went to a meeting of a panel this past week under the auspices of the Institute of Medicine. Called the Evidence Communication Innovation Collaborative [yes, I know], the group discusses a number of topics around the general ambit of communicating medical evidence to patients. We spent a lot of time, productively, on the topic of decision aids. A lot of people at the meeting really like them. (Here’s a collection of decision aids, which includes a short primer on what they are; the Wikipedia article is informative.)
I like them, too, and it’s not hard to understand why. Decision aids are the fuel of shared decision making. Information should not be concentrated in the hands of the doctor; rather, it should be presented to the decider – which we presume is the patient, the ordinary person – in a way relevant to them.
But they are not the panacea:
We forward thinking doctors know in our heart of hearts that decision-making should be shared with the patient; unfortunately, not all patients think that way. Some still rely on the physician to make their decisions.
Even the alternatives, and the risks and benefits attached to each one, are not so obvious without some thought. And that thought is not the view from nowhere, as a philosopher put it, but dependent on the point of view of the person thinking. The risks, benefits, and preferred alternatives depend on the kind of person doing the choosing. And who’s to say that a patient from one race, say, or economic stratum, will react to alternatives the same way as another?
Count me encouraged but skeptical: there were a lot of people in that room ready to share decision making. But a decision aid is only as good as the decisions it includes. We need to know a lot more about how people make decisions, and how they talk to their doctors, before we can expect such aids to do more than reproduce our current health care system’s inequalities and insensitivities.
September 5, 2013
Reasons the doctor might be talking down to you
Reposted from last year.
After a talk I gave about doctor-patient communication, a woman in her 30s raised her hand and said, “I work at a university, and whenever I see the doctor, he assumes I’m a student, and he talks down to me. This makes me very unhappy and I’m not sure what to do about that.” I assumed from her circumstances, and from the tone of her question, that she was not free to choose another doctor. What should be done by someone who has this problem? There are various strategies, but part of the answer is to understand why the doctor might be talking down to someone.
1. The doctor’s personality is unsuited to an egalitarian interaction. If they were a chimneysweep there would be the same problem.
2. The doctor was not trained to appreciate the importance of doctor-patient communication.
3. The doctor does not know what to recommend, or recognizes, perhaps subconsciously, that there is no good evidence to prefer one route of treatment over another. This leads to a basic conflict: she wants to help the patient but also acknowledges to herself that there is no one convincing path. Since she has been conditioned to present a front of omniscience to patients, both through the system and the influence of colleagues, she is not allowed to present that ignorance, or to partner with the patient to address it. Thus, she appears abrupt or condescending.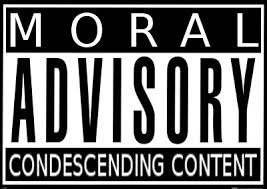
Perhaps I am giving such a doctor too much slack? I would do the same for a patient. Systematic changes mean we should, on occasion, refrain from blaming people without considering the entire differential.
September 4, 2013
The concealed center of life: a poem about going to the hospital
My neighbor, the famous pianist,
has gotten ever sicker the past two years,
his body has slowly shrunk
as if he were hiding himself from the world
and somewhere, with trembling hands,
holding onto a concealed
center of life.
And then one day
he entrusted me
with his apartment keys.
He had to go into the hospital
for an operation
and he asked me
to take care of his two vases
in the window.
“I can bring them to my place,”
I offered.
“No, no,” he stammered.
“The piano has to live with somebody.”
He hung his head
and added as if embarrassed,
“If you have time, it would be good
if once a week, in the evening,
you could just sit for a moment
by the piano.”
(from Der Finfter Zman, CYCO Farlag, 2008. Original Yiddish here. Translation mine.)
September 3, 2013
Sick, with data
Last week I had an absorbing conversation with Natasha Gajewski, someone who, besides being the daughter of a former patient, is also the CEO of Symple Health, a company that has produced a new app helping patients to keep track of their symptoms. That patient of mine was by training a statistician, and to each visit with me he would bring piles and piles of printouts, records of lab results, readings from dialysis. I felt it less than relevant to his care – at least most of the information was just superfluous. But, on the other hand, I didn’t want to talk him out of something that was obviously important to him.
To hear now her daughter tell it, though, his data collecting was an obsessive thing, keeping his grandchildren away from him because - by his own personal calculations – a visit from them might disturb his homeostasis.
Obviously, his daughter knew him much better than I did (he passed away a few years ago). But I can’t help think that here we have several sides of an important phenomenon: that of the engaged patient who records their own data for the sake of their health. This medical version of the “quantified self” can lead – as this story hints – to reassurance and obsession both.
The quantified self, for those who don’t know, refers to the practice of recording – through means both more and less technologically advanced – “readings” from daily life, and using that information for the benefit of health. Such an initiative has something in common with “big data”: the effort to amass large-scale collections of data on a population level.
From a medical perspective, I don’t know what we can expect from big data. Certainly many claims have been made for population-level data and its potential to improve health on a global scale. Who knows if that will pan out? But what about big data on an individual scale?
Data collection works if there is a question waiting for an answer. Otherwise it’s like playing the stock market without any real investment, watching random numbers jump up and down. If you have high blood pressure, checking your blood pressure at home might help to control it. If you have diabetes and check your blood sugar, ditto. But to monitor yourself with thousands of data points, most of which will not answer any askable question, verges on what Abraham Verghese has termed the iPatient – the electronic version of the patient, the tests and results visible on the screen that doctors view to the exclusion of contact with the actual human being. Only, in the case of this hyper-self-analysis, the iPatient is analyzing themselves in a data-centric way to the exclusion of the bigger picture.
What we need is at least two things:
1. A sense of what data will actually be helpful for a given patient, and what “help” (i.e. clinical improvements, patient-relevant outcomes) can be expected
2. A realization that any new source of data will, in general, not be the game-breaking change that people are looking for. Health care problems, in general, are just hard, and data are only part of the solution, which involves patient preferences, the multitiude of possible ways to identify the problem (differential diagnosis), and the goal of patient and physician.
3. An appreciation that data collection can provide, to the individual, both very real reassurance and self-empowerment, as well as a source of obsession and paradoxical lack of control
As Natasha said about our conversation, there are no easy answers, neither unlimited data nor its lack.
August 31, 2013
Leaving the hospital when the doctor doesn’t want you to: some observations from 1984
More from David Mendel’s Proper Doctoring. I can’t say I agree with every single jot and tittle of this selection, but it is thought provoking. See you Tuesday on the other side of the Labor Day weekend – or at least, we get a long weekend in the U.S.A.
Patients Who Take Their Own Discharge
Patients who discharge themselves rarely come to any harm, and doctors who advise against it tend to err on the “safe” side, as of course they should. When faced with a patient who has summoned up the courage to take his own discharge, against everyone’s advice, having signed all those forms, remember that he has had a great deal to put up with, and that he may not have the self-discipline to continue. He may also have motives for discharge which he is unwilling to reveal. Remember too, that you may behave in exactly the same way in similar circumstances. Your natural exasperation at the thought that all the good work may be undone, to say nothing of the anoyance at having your advice rejected “after all you have done,” should be concealed. You are paid to treat the whole patient, and it is he who has to suffer the treatment. Practising medicine is its own reward, and the patients owe neither compliance nor gratitutde. It is your duty to make it perfectly clear to the patient if you feel that he should remain in hospital. Your manner must be neither hectoring nor disapproving nor threatening. It should be doctorly: if complications develop because the patient leaves prematurely, you are prepared to treat them. The patient has not “blotted his copy book,” and no offence has been taken.




