Michelle Stiles's Blog
November 19, 2019
Jump Start Your Natural Knee Rescue

Natural Knee Rescue Is Possible
Research has shown that low grade whole body chronic Inflammation contributes to knee degeneration. This isn’t wishful thinking, it’s a fact. Too bad the western medicine is light years behind the research but you don’t have to be. Don’t get stuck with an early knee replacement when you could have identified inflammatory knee pain and taken action.
Not that I am criticizing the surgery; it’s an amazing tool but when you are in your 40’s 50’s and 60’s it is not going to feel like your “old” knee. There is also more research that states that younger people who get the surgery are less satisfied than older people.
If you attend the webinar, here is what you will learn
How to Determine If You Have “Inflammatory” Chronic Knee Pain.
Top 6 Reasons To Start Your Knee Rescue Screening for Root Causes of Inflammation?
Identify Specific Conditions That Sabotage Weight Loss Efforts For Even The Most Self-Disciplined.
How To Test For Underlying Conditions AND Save Money.
How to Track Your Progress Toward Knee Rescue by The Numbers and NOT Just Vague Symptoms.
Natural Knee Rescue- The Starting Point
Screening for root causes of inflammation is THE key to jump starting your healing for chronic knee pain. It helps you identify the origins of whole body inflammation quickly and with minimal cost. It is where I start all my clients.
If you’ve changed your diet, tried exercise but still can’t make headway. This is your answer.
Also if you’ve been struggling to lose weight or have lost weight only to gain it right back again, It’s likely that you have an underlying condition that is sabotaging your excellent weight loss efforts and prevent you from getting relief to your knees.


If you can't attend the webinar live, leave any questions that you would like answered on the webinar in the comment section below. There will be a replay. Hope to connect soon on the webinar.
The reply from last webinar can be found at Chronic Knee Pain: A Wake Up Call NOT A Prescription for Sugery
If you'd like more background and information, I was interviewed on the Bees Knee Podcast by PJ Ewing.
August 26, 2019
Alternatives to Knee Replacement Surgery
Let's face it alternatives to knee replacement surgery are limited. So what other options should one consider when faced with chronic knee pain? Here is a short video on the whole concept of what is causing the epidemic of chronic knee pain. If you have pain in only one knee because of a previous injury, you might think that this doesn't apply but there is evidence that lowering inflammation in animal models slows the progression of osteoarthritis post injury.
The Standard American Diet is highly inflammatory and a comprehensive program is key.
Access transcript below if you prefer to read.
Hi, my name is Michelle Stiles. I'm a physical therapist in your knee rescue expert. Today I'm going to kind of jump into your living room and get into your mind a little bit. And if I could do that, I would probably say you're going, you're in your head and you're saying, I cannot take pain pills anymore. Okay.
I just can't do it and I can't. I've got to stop limiting the activities I love like hiking, gardening, playing with grandkids, an active retirement, whatever those things are.
So your, thinking, what are my alternatives to knee replacement surgery? Maybe you're still in the workforce, you're under 65 and you're thinking, I gotta do something besides surgery. So what do you have?
Basically you have three things.
You have physical therapy and exercise for weight loss.
Two, you have some kind of supplements and three expensive biological treatments.
Now again, if I could go kind of into your brain, I would say that your response to those would, might be something like this. If I say try physical therapy. You'd say, "Michelle, I've tried those. They make my knees hurt more." Fair enough. Supplements. I've tried those, right? I've tried. You know, my cousin recommended this. I took that glucosamine, et Cetera, et cetera. Right? They didn't make that much of a difference. Maybe a little bit for a while, but then, hey, I didn't even know if I was throwing money away.
Third, and maybe you haven't tried these, but you're thinking about it. You’re waiting, maybe expensive biological treatments versus the knee replacement surgery. They're 3 to 5k a knee. Can you really afford that? Maybe that's where you are. If that's where you are, I have a message.
Is your problem really your KNee?Here's the issue. Your problem is not your knee, okay? Your problem is whole body inflammation. Your problem is aging too fast. Your knees are wearing out. When they look at your knees on an x -ray, they look like the age of a 70 year old and your, let's say only 50 or you're 55 or you're 60 but you still haven't, you not even to retirement yet.
You still should be living an active lifestyle. And what we need to do is we need to lower whole body inflammation. How do we do that? That's the million dollar question. How do we lower whole body inflammation? Well, there isn't one answer to that.
The answer is not, “Here's one thing you can do,” but the answer is a comprehensive program. And that is the key, my friends. Okay? So imagine this, the last 20 years you've spent, eating the Standard American Diet, raising your kids, not getting much sleep, being high stressed because you maybe worked a full time job and you've got a family, right?
Could Decades eating the Standard american diet be hurting my knees?So you’ve spent the last few decades stressed eating the standard American Diet. If you dug yourself a hole, you feel kinda lousy, right? So here you are in a big hole. Now, the biggest contributor to that hole is you can't keep doing what you're doing because you’re, still digging deeper, you're actively going lower and taking scoops of dirt out by living the way you're living.
So you got to stop and change. You've got to change your diet.
Number one for you, stop consuming the Standard American Diet that puts you at a level now and not going deeper, all right?
And then you can, you can add things to that, right? Step by step. So then you can maybe change your lifestyle a little bit. Add that in. Maybe you can add some supplements in, right? And you can see how now we're actually building and getting out of that hole layer by layer, 5% here, 10% here, another 10% over here with adding this, by diet and exercise, physical therapy to strengthen your knee and slowly you're going to be getting back and not all of a sudden, right?
This takes time. All right? But it's worth it because the alternative is the surgery or the expensive biologics. Why wouldn't you try diet and exercise first?
The only reason you wouldn't is because it's not easy, right? But don't let that be you, opting out because it’s hard. Because once you start doing some things and you start seeing some progress, you really get encouraged. You say, “Oh, this is going to work. I am going to get my mobility back.” Okay? So those are the alternatives.
A comprehensive program is what is going to lower the inflammation. Stop thinking that your knee is the problem. It's your diet and your lifestyle, right? And your whole body, and that can be addressed through a comprehensive program. All right, so that's it for today. We'll see you in the next video.

August 5, 2019
Why Are My Knees In Chronic Pain?
Instead of asking the question, “Why are my knees in pain”?, What if you asked yourself what message your knees were trying to give you? What if the pain in your knee was trying to tell you something really important but you weren’t listening?
Chronic knee pain experienced by millions of people the world over at increasingly younger ages is NOT normal. In fact, there is an epidemic of chronic knee pain. And your best answer is not knee replacement surgery, it’s diet and lifestyle changes. Maybe you already “sort of” knew that…deep in your heart, but hopefully this video will give you a bit more insight and the conviction you need to take a different path. Be honest, what does the mirror say?

Access the transcript below if you prefer to read.
Hi, my name is Michelle Stiles. I’m a physical therapist and your knee rescue expert. Today we’re going to take a look at the question. Why are my knees in pain? We are going to use a mirror, for a prop. I know that sounds a little bit crazy, but we are okay. But just hold onto that one minute and I want to explain something first. Biomarkers of inflammation, like C reactive protein are associated with progression of knee osteoarthritis.
So if you have elevated CRP, right, you’re on the fast track to ruining your knees. All right, now think about that. That’s not a good thing. So you want to get off this. So what, what is causing elevated whole body inflammation? Well, for the most part, the standard American diet, things like boxed and processed foods, vegetable oils, too much sugar in our diets, non organic food items.
We have pesticides and toxins coming in and you know, I mean look around, right? There is an epidemic of knee pain, right? People in their forties and fifties have pain all the time in their knees.
It’s Not Normal
I’m telling you that is NOT normal. Don’t believe that myth, get it out of your head. It’s NOT normal. Don’t go on some forum or something and everybody says, “Oh yeah, it’s normal. It’ll be great.” I’m telling you it’s NOT normal and it won’t be great. I’ve seen plenty of things as a physical therapist and I can look in the future and absolutely recommend solving your knee pain some other way. You need to look into it. And I’m sharing with you part of that thing today.
So let’s take the mirror. Pick up the mirror and I want you to ask yourself the question, am I at least somewhat responsible for my chronic knee pain? What’s your diet like?
Ask yourself that question. Look again, ask yourself very slowly, “Am I partially responsible or somewhat responsible for my chronic knee pain?” I think the answer for most people is yes. Okay. Now, if that’s the case, right? Depending on your personality, that may be actually really bad news or good news. It’s bad news, if you are a quick-fix type person, you’re a pill popper, you want an instant solution, the knee replacement surgery suits you fine. Good. Get it done and move on. Right?
It’s good news if you’re that person who wants to have control, basically control over your own health and control over your own destiny out in the future. So now listen, before you leave, don’t leave this video yet because this is the most important part of the video, okay? You see this dashboard behind me? Your chronic knee pain is like a check engine light on your dashboard! What do I mean?
Check Engine Light On Body Dashboard
So if you were driving from New York to LA and the check engine light came on, you’d stop, pull over and investigate. You probably wouldn’t, pull over, cut the cord and keep on going because something worse might happen. Well that’s exactly what might happen with knee pain. We know that there’s an elevated risk for cancer, heart disease, dementia and early mortality in people who have knee osteoarthritis.
Low grade whole body inflammation is implicated in all those chronic diseases that we see now exploding in our culture around us. So I think that you want to be one of those people that can avoid that whole thing. So listen to the check engine light and be thankful and grateful for your knee pain right now, because it may be warning you of something even worse that could happen to you that you’re not really sensing or aware of and you can avoid. Okay? So diet, lifestyle changes are the key to avoiding all that .I’ll be talking about that more in the future, Thanks for listening.
July 16, 2019
4 Reasons To Avoid Bonesmart Knee Replacement Forum
Advice on whether to have knee replacement surgery or how best to recover from the surgery, seems to be everywhere, but all the information tends to sound the same.
{Enter BoneSmart® Knee Replacement Forum}
BoneSmart® is the most recognized patient forum for all things knee replacement.
There you can get help and advice from other people just like yourself who have experiences to share and hard-earned wisdom to dispense. You’ll be an insider to what really goes on and privy to the real deal ups and downs of surgery recovery, good things to know before you sign on for the actual surgery.
Finally, a knee replacement forum to get unbiased information from people without an agenda…
but is it really?
1. BoneSmart® Receives Limited Funding From Orthopedic Manufacturers
BoneSmart® receives limited funding from the following list of orthopedic manufacturers: Zimmer Biomet, Medtronic, Conformis, smith&nephew, Don Joy Othropedics, CeramTec and MicroPort Orthopedics.
While BoneSmart does receive limited support from organizations including orthopedic manufacturers, the manufacturers are not otherwise affiliated with BoneSmart.org and cannot be held responsible for the content contained herein. This website’s content is managed by BoneSmart.
But who owns BoneSmart®?
According to BoneSmart®, it is part of the consumer outreach division of “The Foundation Advanced Research Medicine, Inc. (FARM)”
Googling that exact name, turns up nothing, an extremely rare find.
However, more research reveals that the official name is “The Foundation for Advancement in Research in Medicine, Inc (FARM).
How odd that BoneSmart® would incorrectly reprint its parent name on the website.
 Follow The Money
Follow The Money2. BoneSmart® receives most of it’s funding from FARM
When I finally located the parent website for FARM, a non-profit organization, I learned that BoneSmart®
is an international consumer awareness campaign to help patient-consumers learn about the exciting new advances in hip and knee implant materials in 2005. Using the powerful reach of video, radio, television, print, CD-ROM and the Internet, BoneSmart® is a one-stop information and clinic and hospital referral network for patient-consumers looking for a user-friendly, neutral environment, to explore their options and find the doctor and implant that’s right for their needs. Clinics in the referral network have access to the program and marketing resources to use in their own outreach and patient education programs.
3. FARM is generously supported by all the same corporate manufacturers that support BoneSmart®
FARM is in essence, a shell organization that hides the fact that BoneSmart® is bankrolled by industry sources who use it as a clinic and hospital referral network among other things.
This arrangement allows them to donate money liberally to a non-profit (tax deductible of course) and maintain the illusion that BoneSmart® is a non-partisan, objective source of information rather then an industry sponsored forum cheerleading the promotion of knee replacement surgery.
FARM also “actively pursues revenue sharing relationships with companies and other organizations who share their goal of improving the lives of people with orthopedic disabilities.”
interestingly, Richard Warner, the CEO of FARM, is also the CEO of Joint Replacement Centers of America, LLC a start up for profit venture capitalizing on the growth of the joint replacement industry by building free standing outpatient surgical centers across America.
4. Guidestar, a non-profit watchdog group blows the whistle
This review of FARM by Guidestar in 2014 is lengthy but worth the read.
How is it that the CEO who owns the ‘Bone Smart’ website/message board needs over a million a year to finance that? Seriously, it does not cost a fraction of that much to run a website and message board unless of course the excess ‘expenses’ associated with it go toward SALARY. His status as ‘non profit’ is also exploited by him for FOR PROFIT endeavors such as: jrhamedical.com/
[Since this was written the jrhamedical.com domain is no longer active]
He needs to be more transparent and disclose what his salary is and also what his FOR PROFIT financial interests are for having this non profit org.
So here’s a guy who’s got MULTI MILLIONS coming in salary for his for profit endeavors who has set up a ‘non profit’ to promote the joint replacement industry (for profit industries) via corporate sponsors and requesting more millions–and from the general public of patients mind you. He’s got enough of HIS OWN money to run his website.
Enough of these ‘non profit’ corp CEOs raking in cash like that. There oughta be more TRANSPARENCY laws.
—-
Savvy entrepreneur exploits loop holes of non profit status to promote for profit corporate endeavors.
 CEO, Richard Warner has set up the non profit ‘charity’ corp: ‘FARM ortho’ under the premise of ‘helping people’ with joint problems as to help ‘educate’ them about the benefits of joint replacement via his website and message board; ‘Bone Smart’. In effect, he has set up a venue to PROMOTE the joint replacement INDUSTRY which is a FOR PROFIT industry and bring in more patient CONSUMERS to this industry for which he has vested financial interests in promoting. Hence the premise for it existing as non profit; ‘to help educate’ patients resolves to furthering his own financial interests in increasing the market share of potential patients and with that, garnering venture capital to develop and build for profit joint replacement centers. He is also on the board of directors and CEO of of start up venture to develop and build joint replacement centers which is clearly a ‘for profit’ endeavor.
CEO, Richard Warner has set up the non profit ‘charity’ corp: ‘FARM ortho’ under the premise of ‘helping people’ with joint problems as to help ‘educate’ them about the benefits of joint replacement via his website and message board; ‘Bone Smart’. In effect, he has set up a venue to PROMOTE the joint replacement INDUSTRY which is a FOR PROFIT industry and bring in more patient CONSUMERS to this industry for which he has vested financial interests in promoting. Hence the premise for it existing as non profit; ‘to help educate’ patients resolves to furthering his own financial interests in increasing the market share of potential patients and with that, garnering venture capital to develop and build for profit joint replacement centers. He is also on the board of directors and CEO of of start up venture to develop and build joint replacement centers which is clearly a ‘for profit’ endeavor.
Hence, I call into question the ‘altruistic’ premise of his non profit status that his website; ‘Bone Smart’ arises from the spirit of ‘charity’ or ‘education’ when it’s so closely tied into MARKETING the joint replacement INDUSTRY as to increase market share while this same non profit status is used in pursuit of venture capital to build and develop his for profit financial endeavors. Further investigation is needed as to which loop holes exist in which non profit status can be also EXPLOITED this way for personal financial gain in the way he is conducting.
It is an industry he has vested financial interests in given that he is also CEO and founder of a start up corporation aimed at developing and building joint replacement centers. His non profit ‘charity’ status aimed at ‘educating’ or ‘raising awareness’ to consumers on the value of joint replacement (he has the largest and most well visited patient website in that venue) resolves to a type of MARKETING the joint replacing industry as to increase the market share of patients. In turn, his ability to do that results in a type of ‘leverage’ where he can use his non profit charity status to further his own for profit financial goals in development and building of joint replacement hospitals (as to garner VENTURE CAPITAL) for such.
In that way, his non profit status is disingenuous given it is tied into promoting joint replacement while garnering private investors in his for profit corporate endeavors to develop and build profitable joint replacement centers.
Summary
 BoneSmart® is an extremely compromised knee replacement forum promoting knee replacement surgery to the patient-consumer under the guise of neutrality and enabling its creators to leverage those community relationships to enrich themselves in related for-profit ventures.
BoneSmart® is an extremely compromised knee replacement forum promoting knee replacement surgery to the patient-consumer under the guise of neutrality and enabling its creators to leverage those community relationships to enrich themselves in related for-profit ventures.
By all means don’t be fooled into donating your hard earned money to this industry marketing tool! 
June 9, 2019
3 Easy Steps To Controlling Pain After Knee Replacement Surgery
STEP #1 Take your pain meds as directed
Expect large amounts of “chemically” induced pain-the kind your body normally secretes in response to “trauma,” the first two weeks.
Trying to bend your knee with pain levels greater than 5/10 is like banging your head against a wall…you simply won’t do it… or you’ll do it very infrequently until the pain lessens.
This is a huge waste of down time. A large majority of my patients are able to recover 110 to 120 degrees range of motion post-surgically in the initial two week period. Any veteran of knee replacement surgery, will tell you that getting the knee to bend fully is arguably one of the most difficult tasks after surgery.
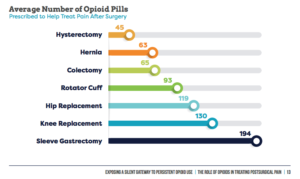 From Choices Matter 2018 Report
From Choices Matter 2018 ReportThis is why you should use your narcotic pain pills to their fullest advantage.
In most cases, you can be off the narcotics in two weeks. Once range of motion has been restored, building strength into the knee is a piece of cake by comparison and narcotics are overkill. [If you want more information on how to do this please consult my book.]
STEP #2 Take your pain meds as directed…if you can get them
Unfortunately today’s strategies for controlling pain after knee replacement are being overtaken by political crusaders against opioid addiction. Trust me, I get it: opioid addiction is real.
However, I just happen to be old enough to remember the misguided home health emphasis undertaken by the Centers for Medicare Services (CMS). They determined that no one suffer with “unmanageable” pain. We were to investigate pain levels every visit.
Most older patients instinctively knew that suffering with pain was better and more healthy than getting hooked on narcotics. However, persistent “sanctioning” can eventually dull the most sensible among us.
 Candy for Everyone!
Candy for Everyone!Narcotics started flying off the shelves like candy on Valentine’s Day, spawning a whole new industry of pain management specialists, a direct result of this official destigmatization.
Of course we have an opioid addiction problem, the medical establishment helped create it. But I digress…
In some states, you will now have to run the gauntlet like a convicted felon to get a narcotics supply that covers you for the initial two weeks. The best thing to do is to talk to your surgeon to find out his exact method for controlling pain after knee replacement.
Then find out how to deftly navigate the logistics of getting the help you need to succeed and thrive, not just survive this period.
State by state prescribing guidelines and whether they have the force of law behind them (your physician is mandated to follow them), can be found here.
STEP #3 Identify Whether You Fit The Likely Profile Of Someone Who Has Trouble Stoping Narcotics After Surgery
Whose NOT at risk?
If you have never used opioid medications prior to surgery, you have a less than .65 % chance of getting hooked long term.
Who is MOST at risk?
Patients who use opioids intensively prior to surgery for at least 4 months are most at risk.
 Know Your Risk Before Surgery
Know Your Risk Before SurgeryIn a recent study, 72% of persistent preoperative users were still using opioids one year after knee replacement surgery.
Presence of chronic pain-related co-morbidities like back pain or fibromyalgia were also associated with long term opioid use.
A general profile of someone likely to have trouble tapering off narcotics after knee replacement surgery consists of:
female sex
older than 50 years
preoperative history of drug abuse, alcohol abuse, depression, benzodiazepine use, or antidepressant use.
Benzodiazepines are anti-anxiety drugs sold under names like Clonazepam, Diazepam, Xanax and Lorazepam.
Opioids happen to be a very good choice for pain control if you are “opioid-naive.” They are effective and generally well tolerated for short periods to help you maximize your knee replacement recovery.
The effectiveness of opioids diminishes with significant preoperative use and they place you at greater risk of prolonged hospital stays, complications and early revision surgery.
So make a commitment to taper off opioids prior to surgery if at all possible! You’ll be glad you did; good things will follow in the wake.
Alarming Trends in Knee Replacement Pain Control?
As I mentioned above, we are in the midst of a profound change in prescribing habits for knee replacement pain control.
During research for this article, I ran across an interesting report entitled, “Exposing a Silent Gateway To Persistent Opioid Use.”
The report promoted three key “alarmist” findings.
1. Opioids to treat post-surgical pain continue to be overprescribed
2. High potency opioids pose risks for orthopedic surgery patients
3. Surgery leads to long-term use of opioids, putting patients at risk of addiction and dependence
While there is some truth in these findings, I labeled them “alarmist” because I think they overexaggerate the true risk that opioids pose.
The most vulnerable surgical candidates represent a narrow minority with a closely defined profile. They could be counseled prior to surgery and perhaps given a different course of treatment. This is a classic case of throwing the baby out with the bathwater because a certain segment is vulnerable.
So who is behind this publication? Let’s connect the dots.
The Opioid Epidemic and Knee Replacement Surgery
The report, “Exposing a Silent Gateway To Persistent Opioid Use.” is found on the website, www.planagainstpain.com
 From Choices Matter 2018 Report
From Choices Matter 2018 ReportThe authors state that their mission is to examine national and state-by-state opioid prescribing trends and the the role that opioid-based post-surgical pain management plays in contributing to the nation’s opioid drug crisis.
The Centers for Disease Control and Prevention (CDC) has declared that we have an opioid epidemic in the United States. Overdoses involving heroin, fentanyl and prescription opioids killed more than 33,000 people in the United States in 2015. Nearly half of those deaths were from prescription opioids.
Following along with this line of thinking approximately 15,000 deaths result from those abusing prescription drugs.
However, I found no attempt, in the report, to separate “deaths from legally obtained prescription drugs” and “deaths from illegally obtained prescription drugs,” which to me is a fairly important distinction.
Hysterically, the report claims that, “Unused Opioids Threaten Families and Communities” and that “9 in 10 surgery patients with leftover opioid pills admit that they haven’t properly disposed of them.”
If this is true, then let’s find a way to inform surgical patients of the need to dispose of pain meds. We can guide thier disposal instead of controlling access to everyone from their benefits on the basis of the few.
Just Who Is A Persistant or Long-Term Narcotic User?
In addition the report claims that 15.2% of knee replacement patients went on to long-term use of opioids. A closer look reveals that “long term” user includes anyone still using at 3 – 6 months after the surgical procedure, which is not that uncommon especially when pain meds are used sparingly to start. Usually those people are still stuggling to get their range of motion back.
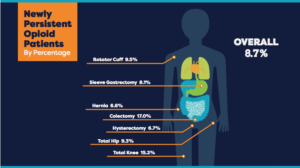 From Choices Matter 2018 Report
From Choices Matter 2018 ReportThe number from less biased research concludes that 7% end up using “long term.” Their definition of “long term” being one year not 3-6 months. The majority of “long term” users fit the general profile that was previously outlined.
The authors recommended guidelines for opioid prescribing…
“if opioids are indicated for acute pain, initiate therapy at the lowest effective dose for no longer than a 3-5 day duration; reassess if pain persists beyond the anticipated duration.”
Marketing Maquarading as Research
Investigating more deeply and one finds…
The report was based on research from IQVIA Institute for Human Data Science and Wakefield Research with funding from Pacira Pharmaceuticals, Inc.
Pacira pharmaceuticals, coincidentally, is dedicated to “improving patient outcomes with opioid-reducing strategies”. Could this be because they market 3 classes of drugs for controlling pain after knee replacement that are in direct competition with opioid use? Humm
These drugs are
1. EXPAREL® (bupivacaine liposome injectable suspension) is a local analgesic administered at the time of surgery to control pain and reduce or eliminate the use of opioids for acute post-surgical pain.
2. The iovera system is a handheld cryoanalgesia device used to deliver precise, controlled doses of cold temperature only to targeted nerves, interrupting the nerve’s ability to transmit a pain signal.
3. DepoFoam® encapsulates drugs, preserving their molecular structure, and releases them over a desired period of time.
The copyright for the website, PlanAgainstPain shows Pacira’s ownership. Copyright @2019 Pacira BioSciences, Inc. Parsippany, NJ 07054
You can imagine the dismay of executives when three recent studies indicated that Exparel or liposomal bupivacaine wasn’t any more effective than the current standard of care in controlling pain after knee replacement surgery and it costs alot more; driving up costs of care for everyone.
This report, funded by Pacira, in essence exaggerates opioid risk to sell more of their own product Exparel, which claims to reduce opioid dependence.
Summary: How to control pain after knee replacement
Take your pain meds as directed.
Figure out how to deftly navigate state/federal regulations so that you don’t waste time in recovery.
Identify if you fit the profile of someone who might have trouble getting off narcotics and take action before surgery.
Resources
Kim SC, Choudhry N, Franklin JM, et al. Patterns and predictors of persistent opioid use following hip or knee arthroplasty. Osteoarthritis Cartilage 2017 Sep;25(9):1399-406. DOI: https://doi.org/10.1016/j.joca.2017.04.002.
Lepasio MJ, Guarino AJ, Mont MA. Pain management associated with total joint arthroplasty: A primer. Perm J 2019;,23:18-169. DOI:http://doi.org.7812/18-169.
June 3, 2019
10 Tips to Master Sleep After Knee Replacement Surgery
There is nothing worse than tossing and turning in bed trying to sleep after knee replacement surgery; your knee the size a large grapefruit, throbbing with your every move!
While most advice centers on what body positions work best to ensure a good nights sleep, these 10 tips will focus on the foundations of rocking the post-surgical knee replacement sleep thing.

You CAN sleep well after a knee replacement but it requires some thoughtful planning and preparation or you chose to wing it and hope for the best.
With a good nights sleep you’ll be ready to attack a day of rehab like nobodies business. Sleep poorly and everything goes downhill from there, the pain seems worse, the
therapist-a jerk, your spouse-a nag.
So let’s get cracking and see what can be done.
1. Lower or eliminate dependence on narcotics prior to surgery
Getting accustomed to narcotics makes then less effective over time, which is why you need to keep increasing the dose. If you want a narcotic pain pill to cut the edge of post-surgery chemical pain (a really good idea), you’ll need to wean off or at least lower your dosages. This will jump start their effectiveness at lower doses when you really need them. Learn more about Opioids here.
I realize this is easier said than done but if you start a few months ahead of time, you’ll be maximizing the pills effectiveness at a critical time. You’ll be glad you did.
2. Optimize sleep hygiene weeks before your surgery
This requires you to be proactive but many people are not sleeping well before they get knee replacement surgery. There are many good articles on how to create a sleep routine that helps you get to bed and stay asleep on a regular basis.
3. Use your pain pills…as directed
Take your pain pills on schedule. Do not take them “as needed.” I repeat. Take your pain pills on schedule. Do not take them “as needed.” As a therapist who has treated hundreds of knee replacement patients, this is probably the number one error that I encounter.
If you allow the medicine to be eliminated totally from your system, when you reach for a pain pill get ready for a disappointment. You let the proverbial “horse out of the barn” and it can take up to 1/2 day to corral that pain back to “manageable.”

I’m usually the first person to suggest reducing dependence on pills as a general rule of thumb, however your post-surgical knee will feel like it has had an encounter with a Mack truck.
Better pain management, better sleep it’s that simple.
Another side benefit to using the pain pills as directed is that it will allow you to do your rehab effectively during those early days. Who wants to sit around the house in misery for two weeks and not get anything accomplished.
4. Find out your state or surgeon’s protocol for narcotic refills
Patients are are now seeing a real bottleneck when attempting to get refills on narcotic pain meds. There are unwieldy regulatory hoops to jump through that differ by state all in the name of solving the opioid crisis. Some will limit the initial script to only a few days and mandate an in person doctor visit to get a refill.
Make sure you find out what the system entails before you are about to run out on a Friday night at 4pm and make sure you surgeons is committed to getting you enough quality meds to get you through the first two weeks.
Again it’s not impossible to make it through that time period without narcotics, but your rehab effectiveness goes down drastically, why waste that time?
Needless to say, you won’t be sleeping well after your knee replacement surgery if you neglect this task.
5. Use your walker for at least two weeks
Lots of people like to brag about how quickly they jettisoned their walker. Do not be that person. Be ”nice” to your knee during the first two weeks and you’ll have less pain.
If you talk to anyone who has had a surgery that needed a bone graft you’ll fliterally been cut off…. This hurts…. the less you put a ton of compressive forces on them in the beginning the better your rehab goes.
So use protected weight bearing and take some weight onto your arms with the walker, slow down at least for the first two weeks.
Less pain means better sleep. Anyone seeing a pattern here?
6. Keep a snack handy by the bedside
Blood sugar dysregulation… a fancy name for glucose levels that are “out of wack” post surgically is common. It is possible that you are walking up because your blood sugar is dropping. When that happens cortisol is secreted to bring it back up. Cortisol is the hormone that wakes you up in the morning. Melatonin helps you go to sleep, they work in opposite cycles.
Having a snack will get the blood sugar back where it should be and reduce the cortisol letting you fall back asleep. It is worth a try if you are staying at the ceiling tiles at 2 am in the morning.
You could also try taking melatonin tablets as a sleep aid before you go to bed. Melatonin is a better option than a sleeping pill.
7. Hydrate well in the AM
Opioids slow intestinal motility and can constipate you in a hurry. Make sure you have a plan to manage this before surgery. Include the concept of pre-hydrating in the morning so that you are not trying to take a lot of water before bedtime and keeping yourself up going to the bathroom. Get started with ab undant water intake in the morning to get ahead of the game.
undant water intake in the morning to get ahead of the game.
8. Plan to eat light
Eating light at night helps you to sleep better, especially when taking pain medications. It is tempting to have food from a pick up window because it’s just easier on family and friends, but avoid it if possible.
Planning ahead with homemade meals that you have frozen and can easily reheat is a much better option or plan for light salads instead.
In short don’t overburden the already slow moving intestines but eating large amounts of cheese, red meat and other things that are hard to digest.
No one sleeps well when they are constipated, bloated or have just eaten a heavy meal. Give your gut a break and to improve sleep after knee replacement surgery.
9. Make sure you are active during the day
Do your exercises 4 times a day like I recommend in my book, get up and walk frequently, just remember to use protected weight bearing. Sit in a chair that is easy to get out of…ahem NOT A RECLINER, so that you will get up more and move.
By staying active, even getting some fresh air you’ll be more naturally tired at the end of the day. If you lay in bed or recline deeply you are more likely to dose off and pay for it later.
10. Find a comfortable position to sleep after knee replacement surgery
The most comfortable position only helps if you have done most of the other nine steps. Below are some videos to help you explore positioning for maximum comfort and optimal sleep after you total knee replacement.
Happy sleeping….zzzzzzzzzzzzzzz
February 19, 2019
How Long Do Knee Replacements Last?
How long do knee replacements last?, is a burning question for many younger people struggling with debilitating knee pain and faced with the decision whether to have early knee replacement surgery.
to have early knee replacement surgery.
A number of years ago I wrote a blog post about why knee replacement surgery in your 40’s was a bad idea. I get more comments from that post than any other post written to date and quite a few of the comments are from angry people who are indignant at my suggestion that they should just wait in pain.
Of course I don’t suggest people just wait in pain, it was simply my attempt to stand by the roadside waving my hands alerting people to the many potential risks that lurk behind the glitzy marketing hype so often encountered throughout the web; the goal being more people making intelligent and well informed decisions based on the real risks. (Link to article one replacement in 40’s)
How Long Does the Average Knee Replacement Last?
The latest research data suggests that 82.3% of total knee replacements and 69.8% of partial knee replacements will last 25 years. [1]
This data is taken from the Finnish Registry, a sub population of the entire study because it is the only available data set without publication bias that has successfully tracked knee replacement surgeries for that length of time. The sample size for this estimate comes from just 89,856 Finnish patients.
Unfortunately, these more optimistic numbers are generated not only from a relatively small sample size but from a population with a mean age of 65 to 74 years.
Lifetime Risk of Revision
 Another study by Bayliss and colleagues concludes that “The lifetime risk of revision, a newer metric for determining risk, is low for patients over 70 years of age, around 5%. [2]
Another study by Bayliss and colleagues concludes that “The lifetime risk of revision, a newer metric for determining risk, is low for patients over 70 years of age, around 5%. [2]
However, when younger patients are segmented out of the larger sample the problems faced are painfully exposed.
For patients aged 50–54 years, lifetime risk of revision for knee replacement surgery increases to 35%. [2]
By the year 2030, patients younger than 65 years old will comprise 55% of knee replacements surgeries. The biggest increase will occur in patients aged 45–55 years. As a consequence, the number of revisions is expected to increase dramatically. [3-4]
What’s So Bad About Having A Revision?
First off, revisions are more expensive, which may or may not be relevant to you the consumer in the future but more importantly they result in worse outcomes than primary surgery, [1] which means more complications and more revisions down the road.
What About Revising a Revision?
Only two studies have investigated re-revision risk for those under 55 and they only looked at total hip patients. One study reported an alarming survival rate of 63% at 10 years, [6] and the other, using a biological reconstruction technique with impaction bone grafting, showed more promising results with a 10 year survival of 87%. [7]
What about the Early Survival Rates of Younger Patients?
Again the news is concerning. 97% of knee replacements worked well after 5 years for those older than 65. This rate dropped to 95% for those aged 56-65 and dropped again to 92% for those less than 55 years old. [8] Rates were not available for patients in their 40’s because the database was not segmented beyond the 55 and under category.
One More Piece of Bad News
Although the survival rate of a knee replacement prosthesis is important, it is not the only measure of success. One in five patients who undergo knee  replacement surgery for osteoarthritis reports an unfavorable pain outcome after surgery. [9]
replacement surgery for osteoarthritis reports an unfavorable pain outcome after surgery. [9]
Pause for a breath, if you are adding all this up. You may want to reevaluate the glowing outcomes promised in slick marketing ads.
Consider this honest comment from an insider. Willem Schreurs, an orthopedic from the Department of Orthopaedics at Radbound University Medical Center in the Netherlands stated in the Lancet (2017),
The current trend to implant total hip and knee implants in ever younger patients, driven by the fact that the short-term outcomes in the first few years after surgery are mostly acceptable, could lead to many patients ceasing to be revisable, and these patients might become a large burden to society in terms of cost and disability. Both patients and surgeons need to be aware of this possibility, and postponing this kind of surgery, despite the realistic limitations of patients with osteoarthritis, should be considered more frequently.[5]
My God, what does he mean “ceasing to be revisable?” This is the unfortunate result when there is little bone material left to work with or is of such poor quality as to prevent the ability to place another implant. At this point you are stuck with a very bum leg.
Doesn’t it Make Sense To Track These in the US?
 A wise person will be asking, hey, “Why don’t we have a United States Registry”?, and this is indeed an excellent question. The fact is, we do, it’s call the American Joint Replacement Registry (AJRR) sponsored by the American Academy of Orthopaedic Surgeons (AAOS).
A wise person will be asking, hey, “Why don’t we have a United States Registry”?, and this is indeed an excellent question. The fact is, we do, it’s call the American Joint Replacement Registry (AJRR) sponsored by the American Academy of Orthopaedic Surgeons (AAOS).
Despite it’s fledgling start in 2010, it is now the largest such database in the world. The registry has amassed information on just over 1 million hip and knee procedures. Despite steady growth, it currently tracks only 25%-30% of the annual procedure volume in the United States, leaving considerable room for future improvement.
Its brief existence however, makes it of little use in answering our primary question here, which is how long knee replacement implants are likely to last.
By the way, the first funded national joint registry was found in Sweden in 1975. There are currently six registries that have more than 15 years of potential follow-up data for knee replacements (those in Australia, Denmark, Finland, New Zealand, Norway, and Sweden), too bad the United States did not take the lead in this.
The Numbers
Realistic expectations about how long knee replacements last can get skewed by million dollar marketing and hype.
If you have your knee replaced at 52 it may last 25 years. You’ll be 77 and maybe the second one lasts for 10 years. One revision over a lifetime, not too bad.
If, however, the initial one lasts only 15 years, your first revision will be at age 67. Will you need another in 10-15 years?
Consider this comment from Ronni on my blog
I was 46 for first tkr and 4 yrs later it failed
Had revision but took a yr plus medical intervention to gain acceptable range of motion
PT was worthless. Swimming did help. Plus exercise in pool
I’m now post 20 yrs on knee and it’s in bad shape
Thinking about doing it again. Or just getting a scooter!
Summary
82% of knee replacements will last 25 years according to the best data we have compiled from a database of majority of people who had their knee replaced after age 65.
Five year survival rates for those younger than 55 show a drop of 5 percentage points from those over age 65, from 97% to 92%
Lifetime risk of revision increases to 35% for those age 50-54 compared to only 5% for those age 70 and over.
Note: I am in the process of completing my latest book entitled, Bone on Bone Under Age 65, A Wake Up Call Not a Prescription for Surgery. This is a work in progress which explores a more comprehensive approach to dealing with knee pain. An early copy is available here.
____________
Resources
[1] Evans, Jonathan et al. “How long does a knee replacement last? A Systematic Review and meta-analysis of case series and national registry reports with more than 15 years of follow-up” 2019 393 (10172) 655-663
[2] Bayliss Lee et al. “The effect of patient age at intervention on risk of implant revision after total replacement of the hip or knee: a datalink study” Lancet 2016; (17) 30059-4
[3] Kurtz SM, Lau E, Ong K, Zhao K, Kelly M, Bozic KJ. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res 2009; 467: 2606–12
[4] Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 2007; 89: 780–85
[5] Schreurs et al. “Total joint arthroplasty in younger patients: heading for trouble?”Lancet. 2017; 389: 1374-1375
[6] Lee PT, Lakstein DL, Lozano B, Safir O, Backstein J, Gross AE. Mid-to long-term results of revision total hip replacement in patients aged 50 years or younger. Bone Joint J 2014; 96-B: 1047–51
[7]fTe Stroet MA, Rijnen WH, Gardeniers JW, van Kampen A, Schreurs BW. Satisfying outcomes scores and survivorship achieved with impaction grafting for revision THA in young patients. Clin Orthop Relat Res 2015; 473: 3867–75
[8] Julin, Jaakko et al. “Younger age increases the risk of early prosthesis failure following primary total knee replacement for osteoarthritis. A follow-up study of 32,019 total knee replacements in the Finnish Arthroplasty Register” Acta orthopaedica 2010; 81(4) 413-9
[9] Beswick Andrew, et al “What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patients” BMJ Open 2012;2:e000435. doi: 10.1136/bmjopen-2011-000435
February 17, 2019
5 Simple Steps to Lower Your Chance of Knee Replacement Infection
This statement means little however if it is you who ends up dealing with an infection after surgery, one of the most serious and dreaded complications of a knee replacement.
The overall early deep infection rate for patients undergoing a primary knee replacement is 0.39%, while revision knee replacement infection rates are 0.97%.
In the first 2 years after surgery, the chance of developing an infection is estimated at 1.5%. After 2 years, the chance of infection goes down to about 0.5%.
While these numbers are exceedingly small, they are not zero, and they are only generalized statistics. YOUR individual knee replacement infection risk may be much higher so read on to find out how to lower your personal risk for one of the worst possible outcomes of knee replacement surgery.
5 Simple Steps To Lower YOUR Personal Risk of Knee Replacement Infection
 The figures above are overall national averages that can be individually influenced for better or worse by the selection of where and who does your surgery.
The figures above are overall national averages that can be individually influenced for better or worse by the selection of where and who does your surgery.
#1 Select a High Volume Hospital
Hospitals with high volumes of knee replacement surgeries have lower infection rates than small community hospitals, so pick your hospital accordingly.
#2 Select The Best Surgeon
Each surgeon will have his own rates of infection as well as overall complication rates which he’ll, no doubt, be happy to share with you… if they are lower than national averages. 
Lower Your Chance of Knee Replacement Infection
Infection after knee replacement surgery is rare. This statement means little however if you end up dealing with a periprosthetic joint infection (PJI), one of the most serious and dreaded complications of knee replacement surgery.
The overall early deep infection rate for patients undergoing a primary knee replacement is 0.39%, while revision knee replacement infection rates are 0.97%.
In the first 2 years after surgery, the chance of developing an infection is estimated at 1.5%. After 2 years, the chance of infection goes down to about 0.5%.
While these numbers are exceedingly small, they are not zero, and they are only generalized statistics. YOUR individual infection risk may be much higher so read on to find out how to lower your personal risk for one of the worst possible outcomes of knee replacement surgery.
Factors That Influence YOUR Personal Risk of Infection
 The figures above are overall national averages that can be individually influenced for better or worse by the selection of where and who does your surgery.
The figures above are overall national averages that can be individually influenced for better or worse by the selection of where and who does your surgery.
Hospitals with high volumes of knee replacement surgeries have lower infection rates than small community hospitals, so pick your hospital accordingly.
Each surgeon will have his own rates of infection as well as overall complication rates which he’ll, no doubt, be happy to share with you if they are lower than national averages.
Hanging out in healthcare facilities after your surgery can negatively affect your chance of infection, so go home as soon as possible to your own germs.
Diabetes, obesity (those with BMI> 40), smoking, alcoholism, steroid use, and rheumatoid arthritis, are all well-known factors that predispose someone toward a higher risk of infection. Correcting these factors aren’t quick or easy.
Nutritional Status
However, I would like to address a different factor that is more amenable to change prior to surgical intervention IF you are aware of it and that is impaired nutritional status. There is a growing body of evidence that implicates malnutrition as a risk factor for infection. [7]
Malnutrition is defined by some researchers as a serum albumin level total lymphocyte count (TLC)
Malnutrition has been shown to interfere with optimal synthesis of collagen and proteoglycan, resulting in disruptions in the wound healing process that can lead to persistent wound drainage and increased risk of infection.
Identifying these risk factors is as easy as examining these common markers on a simple blood chemistry lab.
A recent meta-analysis indicated that an albumin level < 3.5 g/dL had an almost 2.5 fold increased risk of infection in generalized orthopedic surgeries. Researchers of the study recommended a “thorough nutritional consultation for each hospitalized patient in orthopedics.”[1]
In another study patients with hypoalbuminemia (albumin level < 3.5 g/dL) had a higher risk for surgical site infection, pneumonia, extended length of stay, and readmission. [2]
Researchers recommended that “future efforts should investigate methods of correcting nutritional deficiencies prior to total joint arthroplasty. If successful, such efforts could lead to improvements in short-term outcomes for patients.” [2]
The Connection Between Vitamin D and Protein Status
Let’s also look at a closely related finding. Patients with post surgical infection in the hip and knee joints show significantly lower calcium and vitamin D3 levels as well as reduced protein levels (albumin and total protein) compared with primary arthroplasty and aseptic revisions.
The vitamin D status was defined as follows:
deficiency
insufficiency 20–29 ng/mL
normal: 30–100 ng/mL
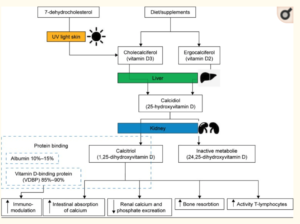 Schematic representation of vitamin D metabolism and its influence on infections. [9]
Schematic representation of vitamin D metabolism and its influence on infections. [9]It has long been established that vitamin D deficiency has been associated with joint infections. [9] It is also known that 99% of the body’s vitamin D exists in the protein-bound form. The vitamin D-binding protein (VDBP), which serves as the most important carrier protein for vitamin D3 and its intermediates, binds about 85%–90%, while 10%–15% are bound to albumin and other lipoproteins. Less than 1% is present as unbound components of the blood. (See Chart Above). [8-9]
So we can easily conclude that reduced protein levels impact Vitamin D delivery to the cells and that all of these markers are early warning signs that you have a higher risk of infection should you choose to move forward with knee replacement surgery.
Of course this scenario assumes that your surgeon provided you with this information and that he did a routine screen of your nutritional status pre-surgically to check for any problems so that you can make an informed decision.
Unfortunately, I’m not sure how prevalent pre-surgical nutritional screening is, but you have been forewarned and are now prepared.
It is something that you can ask your surgeon about and request. It is even possible to get your own testing done if none are being provided for you.
Common Causes of Low Serum Albumin
Liver Congestion: The liver manufactures albumin. So albumin tests are often a part of liver-functioning checks. Many diseases can cause liver failure, including cirrhosis, liver cancer, hepatitis, alcohol-related liver disease, and fatty liver disease. Many livers are congested but don’t yet fall into a “disease” category.
Kidney damage: Problems with the kidneys may cause them to release large amounts of protein into the urine. This can take albumin from the blood, leading to hypoalbuminemia.
Protein losing enteropathy: Some stomach and gastrointestinal conditions, including celiac disease and inflammatory bowel disease, can cause the digestive system to lose a lot of protein. This causes a syndrome called protein losing enteropathy that can lead to low albumin levels.
Low stomach acid: Hypochlorydria is another root cause of faulty protein mal-digestion because the enzymes that breakdown protein need an acid environment to start working in the stomach. Without that head start, protein may end up undigested in the intestines and unavailable for use by the cells.
Malnutrition: People may develop hypoalbuminemia when they do not eat enough key nutrients, or medical conditions make it hard for their bodies to absorb nutrients. Some people who have recently undergone chemotherapy may be malnourished.
Albumin is present in many animal products. Changing your diet to include the following; beef, milk, cottage cheese, eggs, and greek yogurt, may improve albumin status.
If your diet already includes protein rich foods then the root problem could be in your ability to absorb, make or process the proteins.
Absorption: If you have a known GI condition or you suspect you have one, you may have trouble breaking down protein and absorbing it in the small intestine. It is best to work with a functional medicine practitioner before surgery to reduce your risk.
Processing: A congested liver may be causing the deficiency in albumin. A liver and gall bladder flush as described here could go a long way to improving your nutritional status.
Addressing vitamin D deficiency prior to surgery is essential as well. It is not possible for me to go into all the details but check here for an excellent article on symptoms and ways to reverse vitamin D deficiency.
Summary :
Factors That Lower Infection Risk Following Knee Replacement Surgery
Overall knee replacement infection rates are not high but YOUR risk can be higher or lower depending on many different factors.
Hospital and MD selection are important
Going Home as soon as possible will lower risk
Losing weight and quitting smoking will lower risk
Addressing your nutritional status prior to surgery and correcting for low albumin and total protein as well as addressing vitamin D deficiency specifically 25-hydroxyvitamin D or 25(OH) D (calcidiol) will also help lower your infection risk
Resources
[1] Yuwen, Peizhi et al. “Albumin and surgical site infection risk in orthopaedics: a meta-analysis” BMC surgery vol. 17,1 7. 16 Jan. 2017, doi:10.1186/s12893-016-0186-6.
[2] Bohl, Daniel et al. “ Hypoalbuminemia Independently Predicts Surgical Site Infection, Pneumonia, Length of Stay, and Readmission After Total Joint Arthroplasty” J Arthroplasty. 31(1):15-21. Jan. 2016, doi: 10.1016/j.arth.2015.08.028.
[3] Greene, K et al. “ Preoperative Nutritional status of total joint patients. Relationship to postoperative wound complications” Journal of Arthroplasty, 6 (4); 321-5 6 Dec. 1991.
[4] Kamath AF et al. “Low Albumin Is a Risk Factor for Complications after Revision Total Knee Arthroplasty” Journal of Knee Surgery 30(3):269-275. Mar. 2017, doi: 10.1055/s-0036-1584575.
[5] Bohl, Daniel et al. “Is Hypoalbuminemia Associated With Septic Failure and Acute Infection After Revision Total Joint Arthroplasty? A Study of 4517 Patients From the National Surgical Quality Improvement Program” The Journal of Arthroplasty, 31(5): 963 – 967.
[6] Ihle C, Weiß C, Blumenstock G, et al. Interview based malnutrition assessment can predict adverse events within 6 months after primary and revision arthroplasty – a prospective observational study of 351 patients. BMC Musculoskelet Disord. 19(1):83. Mar 15 2018, doi:10.1186/s12891-018-2004-z.
[7] Gu, Alex et al. “Preoperative Malnutrition Negatively Correlates With Postoperative Wound Complications and Infection After Total Joint Arthroplasty: A Systematic Review and Meta-Analysis” The Journal of Arthroplasty, 0 (0) Jan 9, 2019, doi.org/10.1016/j.arth.2019.01.005.
[8] Zajonz, Dirk et al. “The significance of the vitamin D metabolism in the development of periprosthetic infections after THA and TKA: a prospective matched-pair analysis of 240 patients” Clinical interventions in aging vol. 13 1429-1435. 17 Aug. 2018, doi:10.2147/CIA.S171307.
[9] Zajonz D, Prager F, Edel M, et al. The significance of the vitamin D metabolism in the development of periprosthetic infections after THA and TKA: a prospective matched-pair analysis of 240 patients. Clin Interv Aging. 2018;13:1429-1435. Published 2018 Aug 17. doi:10.2147/CIA.S171307.
November 15, 2018
How Do I know If I am Ready For Knee Replacement Surgery?
Knee replacement surgery is now among the most frequently performed medical procedures in the United States costing Medicare alone billions of dollars per year. The annual rate of total knee replacements doubled between 2000 and 2015 with the steepest rate of increase occurring among people aged 45-64. [1]
Now that traditional age limits no longer seem to apply, more and more people are asking, “How exactly do you know when you are ready for a knee replacement surgery?”
Economic Considerations
 And while you are busy asking that question, the powers that be are busy asking…”Are all these operations necessary? Are all these operations beneficial? and How do we save money if we are going to be doing all these operations?”
And while you are busy asking that question, the powers that be are busy asking…”Are all these operations necessary? Are all these operations beneficial? and How do we save money if we are going to be doing all these operations?”
Unbeknownst to you or the casual knee replacement surgical candidate, the crazy bean counting economist -types are busy creating sophisticated models that estimate quality of life improvements based on functional performance scales to predict the cost of various health improvements.
There term”QALY” is one which you should be familiar. The quality-adjusted life year or quality-adjusted life-year (QALY) is a measure of the value of health outcomes. It assumes that health is a function of length of life and quality of life, and combines these values into a single index number.
To determine QALYs, one multiplies the utility value associated with a given state of health by the years lived in that state. A year of life lived in perfect health is worth 1 QALY (1 year of life × 1 Utility value). A year of life lived in a state of less than perfect health is worth less than 1 QALY; for example, 1 year of life lived in a situation with utility 0.5 (e.g. bedridden, 1 year × 0.5 Utility) is assigned 0.5 QALYs. [2]
If this all seems sort of confusing and abstract and makes your eyes roll back into you head, you are not alone.
QALY’s And Knee Replacement Surgery Decision
You should however understand that at the intersection of socialized medicine and western medicine.. these are the only questions that matter. Focus on the collective benefit will demand an answer to the question, “Is it worth the money society coughs up for knee replacement surgery, if you the patient get only minimal improvements in functional outcome?”
Of course, if you were paying for the procedure on your own, you could make that determination yourself but as a Medicare recipient, these questions are going to loom much much larger in the future.
Just for fun, take a look at this article Impact of total knee replacement practice: cost effectiveness analysis of data from the Osteoarthritis Initiative, published in March 2017 as an example decision making rubrics pertaining to knee replacement surgery. 
The following three summary points were highlighted in the conclusion.
Quality of life outcomes generally improve after total knee replacement, with small effects becoming larger with decreasing preoperative functional status
The practice of total knee replacement as performed in a recent US cohort of patients with knee osteoarthritis had minimal effects on QALYs at the group level and was found to be economically unattractive
Total knee replacement practice, however, could be considered cost effective if the procedure were restricted to patients with more severely affected functional status [3]
Deliberations over whether you should have knee replacement surgery or not, ought to include economic considerations.
Now some might say. Gosh, maybe I should rush out and have the surgery because it might not be available to someone my age in the near future.
While that is true, what about future revisions? Can you be so sure that they will be provided? Seated where you are right now, that scenario might seem farfetched, but the baby boomer numbers heading into retirement years are staggering. Is all this surgery really sustainable over the long haul?
Are You Really End-Stage?
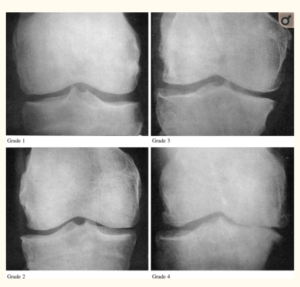 Kellren/Lawrence Scale
Kellren/Lawrence ScaleKnee replacement surgery is typically reserved for those with end-stage knee arthritis, Kellgren/Lawrence grades 3 or 4 as observable on x-rays. This makes complete sense. Surgically altering your knee, an irreversible act, should be the last resort and only undertaken when all conservative alternatives have been exhausted.
What if I told you that in a recent study of one orthopedic practice at least 19 people who had undergone knee replacement surgery in a one year period were found to have only grade 1-2 Kellgren/Lawrence scores. [4] These patients had persistent knee pain issues that were unexplained at follow-up one year post operation.
In another study, researchers determined that one third of participants had inappropriate surgery based on commonly accepted criteria, like the Kellgren/Lawrence noted above and other clinical measures. [5]
Clearly something is amiss and disturbing about these numbers. I fear that these are not isolated events and that the surge in knee replacement numbers reflect a sort of reckless abandon of the traditional criteria used to make determinations for appropriateness.
Sure there are probably some unscrupulous surgeons amongst us, but I think it has more to do with what I call the “End of the Pipeline” crisis.
Medical Pipeline
 Conventional medicine constitutes a medical pipeline that can be envisioned as a funnel, the larger opening is filled with the population of those in the initial stages of osteoarthritis. They work their way down the pipeline by talking to their primary doctor about the problem; trying some conventional treatments like physical therapy or maybe weight loss.
Conventional medicine constitutes a medical pipeline that can be envisioned as a funnel, the larger opening is filled with the population of those in the initial stages of osteoarthritis. They work their way down the pipeline by talking to their primary doctor about the problem; trying some conventional treatments like physical therapy or maybe weight loss.
When attempts to manage pain with over the counter medications fail and if pain continues to escalate, they move down the funnel again and access the orthopedic surgeon, who is likely to suggest cortisone shots. The next typical remedy would be to go on prescription pain medications. The demands of work and driving generally rule out his option for younger clients.
And so, there they are hanging in limbo between opioids, knee replacement surgery and the prospect of a dim future struggling with pain and mobility issues. This is the end of the traditional medical pipeline and massive amounts of people are hitting this benchmark significantly earlier then previous generations.
Compassionate medical personnel are stepping up to help these “end of the pipeline” osteoarthritis sufferers resolve this dilemma even if it means doing the replacement when they are only technically grade 1 or 2 Kellgren/Lawrence.
End of the Pipeline: What Can You Do?
Today many knees are undergoing unprecedented accelerated aging. What is going on? Only a few of our grandparents were severely hobbled by advanced arthritis.
advanced arthritis.
Joint pain and inflammation is one of the major causes of disability around the world, in fact 12% of the worlds population is said to suffer from the affliction.
The joints are one of the most delicate structures in the human body and in many people; they take a lot of punishment. They must be rebuilt continuously to offset the constant wear and tear that occurs, especially on the weight-bearing joints of the body, like the knee.
A catabolic state exists in the knee when of the body cannot rebuild joint cartilage fast enough to overcome the degenerative processes on those same tissues. The degenerative causes of osteoarthritis have long been assumed to be “wear and tear.” Too much activity, too much weight and the knee joint will wear out because of stress and pounding.
This is in contrast to its’ evil twin rheumatoid arthritis caused by a severe inflammatory condition that is easily identified by certain blood tests.
Past research on weight loss and its’ contribution to knee pain seems to support the “wear and tear” theory of osteoarthritis. For example, weight loss of fifteen pounds has been shown to reduce knee pain by 50% in overweight individuals with arthritis [1] and for every pound of weight lost; there is a four-pound reduction in mechanical load exerted on the knee during daily activities. [2]
 Current groundbreaking research however suggests that inflammation plays a much bigger role in osteoarthritis than previously thought.
Current groundbreaking research however suggests that inflammation plays a much bigger role in osteoarthritis than previously thought.
Read Robinson’s summary of recent research from his article entitled, Low-Grade Inflammation as a Key Mediator of the Pathogenesis of Osteoarthritis. (2018)
OA is a disorder of the joint as a whole, with inflammation driving many pathologic changes. The inflammation in OA is distinct from that in rheumatoid arthritis and other autoimmune diseases: it is chronic, comparatively low-grade, and mediated primarily by the innate immune system . For example, elevated serum levels of C-reactive protein, a marker of inflammation, are predictive of the development and progression of OA.
Inflammation as a target of treatment
Thus, current evidence suggests that targeting inflammation therapeutically has the potential to prevent or reduce multiple pathologic features of OA, and slow the progression of the disease.
In addition to local inflammation in the joint, systemic inflammation might also have an important role in OA pathogenesis. For instance, obesity is known to predispose individuals to OA — possibly not only by increasing the mechanical load on joints, but also by causing chronic, systemic inflammation through inflammatory mediators (such as adipokines and other proinflammatory cytokines) that are produced by adipose tissue and released into the bloodstream. Weight loss is associated with a substantial reduction in systemic levels of C-reactive protein and IL-6 in individuals with OA, and can prevent OA onset or alleviate existing OA symptoms . It is possible that the systemic inflammation associated with chronic inflammatory states, such as obesity or certain chronic diseases, promotes local inflammation in joints that ultimately results in OA . [3]
A low-grade inflammatory state may in fact be driving the degenerative changes of osteoarthritis much more than simple excess weight. Weight loss studies that show improved knee pain might need to be evaluated more critically to determine if anti-inflammatory diets might be responsible for some of the improved pain and functional indicators.
This groundbreaking research yields fertile ground for the investigation of numerous targets of intervention to reduce whole body inflammation as a way to curb osteoarthritis.
In a recent New York Times article, Personal Health columnist Jane Brody, herself a recipient of bilateral knee replacements, asked whether prospective patients were really giving lesser remedies a fair trial? Unfortunately, the article fails to mention any of the groundbreaking research into the connection between low-grade inflammation and osteoarthritis.
Summary: Ready For Knee Replacement Surgery?
Here is a short list of action steps you can take to help answer this question.
Ask your Orthopedic surgeon for your Kellgren/Lawrence grade
Consider economic factors before submitting to the surgery
Investigate low-grade inflammation as a potential cause of your OA and make diet and lifestyle changes
Read my latest book Bone on Bone Under Age 65: A Wake Up Call Not a Prescription for Surgery for more information
Take the Free Screening Test to determine if Lowering Inflammation Could Help Save Your Knee?
Resources
[1] https://www.nytimes.com/2018/10/15/well/live/should-you-have-knee-replacement-surgery.html
[2] https://en.wikipedia.org/wiki/Quality-adjusted_life_year
[3] https://www.bmj.com/content/356/bmj.j1131.long
[4] Polkowski GG, Ruh EL, Barrack TN, Nunley RM, Barrack RL. Is Pain and Dissatisfaction After TKA Related to Early-grade Preoperative Osteoarthritis? Clinical Orthopaedics and Related Research. 2013;471(1):162-168. doi:10.1007/s11999-012-2465-6.
[5] https://onlinelibrary.wiley.com/doi/full/10.1002/art.38685