Michelle Stiles's Blog, page 3
December 19, 2016
Can Whole Body Inflammation Affect The Health of Your Knees?






 Osteoarthritis As An Inflammatory Disease?
Osteoarthritis As An Inflammatory Disease?While most of us tend to think of knee arthritis as being caused by good ‘ol wear and tear, a study in the Journal of Osteoarthritis and Carilage might cause us to think otherwise. The article summarizes relevant research in molecular biology that implicates whole body inflammation as a causal factor in degenerative knee arthritis. If this is true, innovative new ways to avoid a knee replacement can be implemented that may have more efficacy than just weight loss alone or similar tactics.
The literature is rich in data suggesting that inflammatory mediators play a pivotal role in the initiation and perpetuation of the OA process. The source of such mediators would be local from joint cells and systemic from other tissues such as adipose tissue released in blood flow and then reaching the joint via the subchondral bone vasculature. These mediators then have a deleterious effect on cartilage, bone and synovium.
Researchers concluded that the anti-cytokine approach has not yet proven significant improvement in OA symptoms and structure modification, as it relates to a search for a new drug. However, Dr Weil, one of the fathers of integrative medicine has been teaching his followers how to lower inflammation in the body through diet and other lifestyle factors. Dr Weil’s expertise can get you started lowering your risk for a total knee replacement in the future and reducing present day joint pain. In addition, healthy eating can lower your risk for many other types of chronic health diseases as well.
Inflammation in the body is a normal and healthy response to injury or attack by germs. We can see it, feel it and measure it as local heat, redness, swelling, and pain. This is the body’s way of getting more nourishment and more immune activity into an area that needs to fend off infection or heal. But inflammation isn’t always helpful. It also has great destructive potential, which we see when the immune system mistakenly targets the body’s own tissues in (autoimmune) diseases like type 1 diabetes, rheumatoid arthritis and lupus.
Whole-body inflammation refers to chronic, imperceptible, low-level inflammation. Mounting evidence suggests that over time this kind of inflammation sets the foundation for many serious, age-related diseases including heart disease, cancer and neurodegenerative conditions such as Alzheimer’s and Parkinson’s diseases. Recent evidence indicates that whole-body inflammation may also contribute to psychological disorders, especially depression – for more on this, see my new book, Spontaneous Happiness, which will be released November 8, 2011.
The extent of this chronic inflammation is influenced by genetics, a sedentary lifestyle, too much stress, and exposure to environmental toxins such as secondhand tobacco smoke. Diet has a huge impact, so much so that I believe that most people in our part of the world go through life in a pro-inflammatory state as a result of what  they eat. I’m convinced that the single most important thing you can do to counter chronic inflammation is to stop eating refined, processed and manufactured foods.
they eat. I’m convinced that the single most important thing you can do to counter chronic inflammation is to stop eating refined, processed and manufactured foods.
You can also try my anti-inflammatory diet, as illustrated by my anti-inflammatory diet and food pyramid. This isn’t a weight-loss diet (though you can lose weight if you follow it). Instead, it is designed to help you reduce chronic inflammation by eating fresh, healthy and delicious foods. One of the most important things the diet does is provide balanced amounts of omega-3 and omega-6 fatty acids. Most people consume an excess of omega-6 fatty acids, which the body uses to synthesize compounds that promote inflammation. You get a lo t of omega 6 fatty acids from snack foods and fast foods. Omega-3 fatty acids – from oily fish, walnuts, flax, hemp and to a lesser degree canola oil and sea vegetables – have an anti-inflammatory effect.
t of omega 6 fatty acids from snack foods and fast foods. Omega-3 fatty acids – from oily fish, walnuts, flax, hemp and to a lesser degree canola oil and sea vegetables – have an anti-inflammatory effect.
If you look at the food pyramid on this site you’ll see that it emphasizes fruits and vegetables, whole grains, beans and legumes, fish and sea food, whole soy foods, and tells you how much of these foods to eat daily or weekly. You get a wide variety of fresh foods on this diet, plus some red wine daily, if you so desire, and healthy sweet treats such as dark chocolate (make sure it has a minimum content of 70 percent cocoa). Along with influencing inflammation, this diet will provide steady energy and ample vitamins, minerals, essential fatty acids, dietary fiber, and protective phytonutrients. What’s more, I think you’ll enjoy it.







December 18, 2016
What Causes a Threefold Increase Risk of Total Knee Replacement?






 Arthroscopic surgery for your meniscus… better think twice!
Arthroscopic surgery for your meniscus… better think twice!Has a doctor recently told you that you need to have your knee scoped? It may be a nuisance to live with the pain for a few months while your body heals but will be well worth it to avoid a knee replacement or even to delay it.
Arthroscopic surgery for degenerative meniscus tears increases risk for eventual knee replacementA recent study published in the journal Osteoarthritis Cartilage showed that patients with osteoarthritis of the knee who undergo arthroscopic surgery for degenerative meniscus tears are at markedly increased risk for potentially having total joint replacement. In the study, 335 patients with osteoarthritis of the knee underwent arthroscopic surgery for degenerative meniscus tears. They were followed for two years.The authors demonstrated that in patients with knee osteoarthritis, arthroscopic knee surgery with meniscectomy is associated with a 3 fold increase in the risk for future knee replacement surgery.Comment: Don’t do it if you can avoid it. The meniscus serves of function. It helps to cushion the knee. Any meniscus tissue should be preserved.







December 11, 2016
Running Lowers Inflammation in Knees?







[image error]Want to avoid a knee replacement? New research has come to some counter intuitive conclusions. You might want to dust off your running shoes if you are young and healthy but have given it up over worries that you were increasing your risk for knee replacment surgery. Read on to learn more.
The soreness runners experience after a workout is usually passed off as a price paid for a healthy heart. But new research from Brigham Young University found that instead of increasing, inflammation actually goes down in knee joints after running.
“It flies in the face of intuition,” said study coauthor Matt Seeley. “This idea that long-distance running is bad for your knees might be a myth.”
Seeley and his colleagues measured inflammation markers in the knee joint fluid of healthy men and women aged 18-35, both before and after running.
They found that the concentration of two specific markers, two cytokines named GM-CSF and IL-15, decreased in the synovial fluid in the subjects after 30 minutes of running. When the same fluids were extracted before and after situations that didn’t involve running, the levels of inflammation markers were similar.
“What we now know is that for young, healthy individuals, exercise creates an anti-inflammatory environment that may be beneficial in terms of long-term joint health,” said study lead author Robert Hyldahl.
Hyldahl said the study results indicate that exercise may help delay the onset of degenerative diseases such as osteoarthritis. Read more







Running Lowers Inflammation in Knees







[image error]Want to avoid a knee replacement? You might have to ask Santa for a pair of walking or running shoes.
The soreness runners experience after a workout is usually passed off as a price paid for a healthy heart. But new research from Brigham Young University found that instead of increasing, inflammation actually goes down in knee joints after running.
“It flies in the face of intuition,” said study coauthor Matt Seeley. “This idea that long-distance running is bad for your knees might be a myth.”
Seeley and his colleagues measured inflammation markers in the knee joint fluid of healthy men and women aged 18-35, both before and after running.
They found that the concentration of two specific markers, two cytokines named GM-CSF and IL-15, decreased in the synovial fluid in the subjects after 30 minutes of running. When the same fluids were extracted before and after situations that didn’t involve running, the levels of inflammation markers were similar.
“What we now know is that for young, healthy individuals, exercise creates an anti-inflammatory environment that may be beneficial in terms of long-term joint health,” said study lead author Robert Hyldahl.
Hyldahl said the study results indicate that exercise may help delay the onset of degenerative diseases such as osteoarthritis. Read more







November 20, 2015
Knee Replacement Exercise Equipment-It Works! However You Want To Make It
I’d like to introduce you to Susan and tell you her success story! When we first made contact she was a bit frustrated that my bonus page had become disconnected from the bonus download. In particular she was looking for the instructions to build the FLEX bar. Her first FLEX bar, one built by her husband out of PVC pipe for the first surgery had been misplaced in a move. Her second surgery was coming up fast and wanting similar success; she was determined to have her husband build another one.
We connected, she got the blueprint [Free with book purchase] and I did not hear from her for about eleven weeks. When she did catch up with me again, she was happy to report another outstanding outcome. She sheepishly reported that her carpenter husband had made the second homemade FLEX bar out of scrape wood instead of PVC pipe and while she thought it looked a “bit primitive” it had nonetheless worked like a charm in accelerating her recovery and allowing her to be in control over pain without sacrificing progress.
Susan graciously agreed to send me the pictures of her “Homemade” FLEX bar and to answer a few questions that might be helpful to others considering surgery.
Questions Regarding “Homemade” Exercise Equipment
 What made you seek other “outside” advice prior to getting your first knee done?
What made you seek other “outside” advice prior to getting your first knee done?
Actually a very good friend of mine took the initiative to seek out a book for me on Amazon when she heard I was getting a knee replacement. She chose the book because it had the most recent pub date so she figured it would have the most current information. Turned out it had the BEST information.
What convinced you that the FLEX bar would actually work properly as knee replacement exercise equipment?
I knew the degree of flex after surgery was important. My doctor told me he wants all his patients to be at 120° by six weeks after surgery. I had read the book cover to cover and it seemed like, based on your charts and information, the FLEX bar would help me accomplish that goal.
What was the thing you liked best about it?
The fact that you are in charge of your pain when using it and not at the mercy of a physical therapist. Over the course of a day it’s easy to sit down numerous times with it and work the knee. It still hurts. The FLEX bar doesn’t take the pain away but it makes it to easier to tolerate through the action of flexing with the bar. It’s great when you start to see results. At six weeks I was at 125° and both knees have made it to 140°.
How did your physical therapist and surgeon respond to it?
With the first knee, since the FLEX bar was new to me, I didn’t share it with either one. The first physical therapist was getting close to retirement and only gave me basic exercises on badly copied sheets. I was pretty much on my own. But by the second knee I knew the FLEX BAR worked and worked well. After the second knee surgery, during one of my early sessions with another PT he worked my knee to get the flex and the pain was terrible. I told him I had my own method and that he didn’t need to do that any more. Next session I brought the bar in to show him and he was amazed. He had a few other clients there at the same time and they gave it a try. I know he was convinced.
For the doctor, I took a copy of the book in to him and brought the bar for a Show and Tell. By then my flex was at 135°. He was very impressed and said hewas going to pass the book and bar information on to future patients.
Did people in your family think it was a crazy idea?
My husband was enthusiastic about it when I explained the concept. He built both of the bars for me and, seeing the results, has also become a real advocate for it.
Were you ever worried you would hurt yourself with the FLEX bar?
No, but I did stay conscious of the pain and each time would work slowly with the bar, moving it as the comfort levels changed.
Any tips and tricks that you would like to pass on?
Yes. Be consistent. Use it as much during a day as you can tolerate. Start using it early on after the surgery. Don’t wait for the swelling to go down or the pain to go away. It works.
While there are pockets of excellent post surgical therapy, there is unfortunately a growing segment of marginal therapy that disadvantages the patient from timely and efficient recovery. Arm yourself with knowledge ahead of time and you’ll be in a much better position to ensure your own success while controlling your own pain levels.
Your Success Story Here
Make your own FLEX bar. Use your noggin, use your hands and get started making your very own knee replacement exercise equipment out of an old walker, wood, PVC, or even steel pipe. You won’t regret it and if you have a unique and interesting version. Please send me a picture and maybe I’ll feature your story on the next blog post. Go here to get started I’m looking for Hero Story #2… Will you be next?
Medicare Pushes Back Start Date For Knee Replacement Payment Model
Some communities will be involuntarily forced to test the new bundled payment model coming in April, 2016. This is a delay from the anticipated start date of January, 2016. In this article I will be helping you to interpret “Government-Speak”. Red-lettered text in brackets, are my editorial comments and interpretation. This article has been reprinted from US News and World Report
Surgeons at Akron General Medical Center are rethinking their whole approach to hip and knee replacement surgery. {The government will eventually force them to if they do not get ahead of the curve now} The transformation underway in Akron will sweep through hospitals in 67 cities {Reduced from an original 75 cities} next year (Originally set to start in January. 2016} and eventually thousands nationwide.
Here is the new list of 67 cities
Comprehensive Care for Joint Replacement Model: Metropolitan Statistical Areas (MSAs)
The stakes are high. Failure to get it right could cost the hospitals millions, as Medicare begins phasing in plans to pay hospitals not for the number of services they provide but for high-quality episodes of care provided at the lowest possible cost. {“Quality care” and “lower costs” are terms inevitably lumped together however this is primarily about cutting costs}
CMS announced Monday {11/16/15} that the most ambitious phase of the new program will begin April 1, 2016, when Medicare will begin putting in place a plan to put each hospital at financial risk for the cost and quality of each joint replacement procedure, including care provided outside the hospital for up to 90 days
Putting hospitals at financial risk for the cost of care is a powerful incentive to get it right. Unnecessary procedures, {How on earth will anyone know if a procedure was unnecessary?} complications, hospital readmissions and extended care provided in costly “post-acute” settings such as rehabilitation centers all may {will} drive up costs and increase the likelihood that hospitals will end the year owing Medicare money. {For the vast majority you can kiss SNF post TKR goodbye} Hospitals that reap savings will be able to reward physicians and other care providers, providing them too with an incentive to boost quality and cut cost {Again this idea that they are going to boost quality and cut costs}
Hip and knee surgery is just the beginning. Goals set by Health and Human Services Secretary Silvia Burwell this year require half of all Medicare payments to be shifted into alternative models like the Comprehensive Care for Joint Replacement (CCJR) program by 2018 {Joints fit into a neat and tidy episode of care but it is doubtful that other disease processes will prove so amenable}, while 90 percent of payments will be tied to the quality of care. {By the way, linking paybacks to quality of care encourages the healthcare system to avoid caring for the sickest individuals or to deny care to those who fall into a high risk category.}
Dr. Patrick Conway, director of the Center for Medicare and Medicaid Innovation, who is in charge of implementing the new approach, says early pilot studies of so-called bundled payment programs have yielded “promising results.”
Large Scale Roll Out
 “We want to test this on a larger scale,” Conway said. “We think hospitals, physicians and post-acute providers will be able to partner together and deliver higher quality and more efficient care.” {In other words the less rehab that is provided the more money the doctors will make.}
“We want to test this on a larger scale,” Conway said. “We think hospitals, physicians and post-acute providers will be able to partner together and deliver higher quality and more efficient care.” {In other words the less rehab that is provided the more money the doctors will make.}
Getting the parties together to talk is an achievement unto itself, says Kevin Bozic, chairman of surgery at the Dell Medical School of the University of Texas, Austin. “It’s the first time that all the people involved in the care of the patient are all sitting down to decide what makes the most sense.” {It’s also the first time in history that some parts of the healthcare system are being asked to cannibalize other parts of the healthcare system in order for them to profit.}
“Patients think we’re already working together,” Bozic added. “It’s shocking to them that these partnerships don’t already exist.” {This is just absolute hogwash-the good surgeons absolutely know what their rehab pipeline is doing because it reflects on them as a surgeon}
To prepare, hospitals are overhauling every aspect of the care they provide to joint replacement patients, {The problem with this is that we already do a damn good job with minimizing complications and re-admissions. There is really no reason for a wholesale restructuring except to save money} says Dr. Thomas Thompson, Akron’s chairman of orthopedic surgery.
“It’s a huge and complicated undertaking,” Thompson said. “It’s a challenge every institution will face. And the smaller ones will find it difficult to accomplish if they’re totally on their own.”{This is why I predict that the smaller ones will eventually just stop doing the procedure. Fewer hospitals providing the surgery will result in longer wait times unless they increase capacity at the larger institutions-We will have to wait to see if that happens}
Hospitals have no choice but to satisfy Medicare; Medicare is their biggest customer. In 2013, the most recent year available, Medicare covered 400,000 inpatient joint replacement procedures with costs totaling more than $7 billion for hospitalization alone. Virtually all the procedures done that year were fee-for-service, meaning the hospital billed Medicare separately for every service it provided.
If a patient ended up with a hospital-acquired infection, or needed a longer length of stay, the hospital billed Medicare for the additional care. If a patient needed extended care in a rehabilitation center or a skilled nursing facility, Medicare paid for that separately too. Studies indicate that quality and cost vary dramatically at facilities nationwide. {One reason is the regional differences in pricing that exist just like in the housing market- a flat rate would discriminate against places that have higher costs to do business like salaries, taxes etc. The other important point here is that if a hospital has a ton of extra costs that seem to stem from poor care why not just put a cap on extra reimbursement after a certain limit or suspend them from doing Medicare joints altogether until they retrain or otherwise demonstrated that care has improved. There are plenty of other less disruptive options that could have been tried first before overhauling an excellent system}
For instance, Medicare data shows that the rate of complications or implant failures is three times higher at some institutions than others. {I’m not sure if they are controlling for comorbidities or not. If they are not then this is a ridiculous and misleading statement. Additionally implant failure almost never happens in the 90 day window that is being addressed in this new proposed rule} And the average Medicare payment for surgery, hospitalization and recovery ranges from $16,000 to $33,000, depending on where the surgery is performed.
Transform Care?
 What makes the change even more significant is that it promises to transform the way care is delivered to every hip or knee replacement patient – not just those 65 and older. {Government Rules and regulations having been the driving force in healthcare for years} Hospitals don’t vary the care they provide based on a patient’s insurance. That means any change put in place to satisfy Medicare will affect every hip or knee replacement patient no matter how old they are.
What makes the change even more significant is that it promises to transform the way care is delivered to every hip or knee replacement patient – not just those 65 and older. {Government Rules and regulations having been the driving force in healthcare for years} Hospitals don’t vary the care they provide based on a patient’s insurance. That means any change put in place to satisfy Medicare will affect every hip or knee replacement patient no matter how old they are.
In response to public comments, however, CMS Monday announced they will make some significant changes in the program’s roll-out phase to refine the payment scheme and give hospitals more time to adapt. The most immediate change was a delay in the program’s start date from Jan. 1 to April 1. In another significant shift, CMS scaled back the scope of the Comprehensive Care for Joint Replacement trial from 75 cities to 67. {This is only because there are enough other places submitting to undergo a voluntary trail of this payment method (BPCI).}
It will also scrap its initial plan for paying hospitals–a plan based on whether hospitals could hit a “target price” for a given procedure without a loss of quality–in favor of a new quality score, in order to provide stronger incentives for more hospitals to improve quality. The quality score is still a work in progress, CMS said. {My initial understanding on this was that the quality score was going to reflect readmissions and complications like infections blood clots, implant failure etc. in addition to a hospital based satisfaction survey but would not be dependent on any specific rehab data (A surgical procedure for getting range of motion being the exception). So far CMS does not appear to be safeguarding therapy quality and quantity. I look for the therapy to be cannibalized the most without penalty to the hospitals.}
The agency also plans to give hospitals more time to get used to the new program before they shoulder the financial burden of costly low-quality care.
Akron General is one of a handful of hospitals that didn’t wait for the program to begin; the hospital’s administration volunteered to test alternatives to traditional fee-for-service payments through a previous Medicare trial, called the Bundled Payments for Care Improvement Initiative (BPCI).
Hospitals that didn’t volunteer for the new program were “obviously very worried” about their ability to adapt {As they should be}, says Bruce Hamory, chief medical officer at the consulting firm Oliver Wyman. Adding to their anxiety was the fact that, until Monday, no one knew precisely what Medicare would propose. CMS reviewed hundreds of comments and concerns before issuing its new rules Monday.
One Size Fits All
 Although most hospitals say they favor the new approach in principle, many worry about how a one-size fits all program will affect hundreds of different institutions. {Reasonable fear} In its comment on the rule, the American Hospital Association, which represents about 5,000 U.S. hospitals, was one of many groups that successfully urged the agency to delay the start date to give hospitals more time to prepare.
Although most hospitals say they favor the new approach in principle, many worry about how a one-size fits all program will affect hundreds of different institutions. {Reasonable fear} In its comment on the rule, the American Hospital Association, which represents about 5,000 U.S. hospitals, was one of many groups that successfully urged the agency to delay the start date to give hospitals more time to prepare.
In Akron General, teams have coalesced around the effort to overhaul joint replacement surgery. Everyone at the hospital involved in the surgery in any way—from the pharmacy to finance, from specialty-care to physical therapy—has been trying to figure out ways to improve quality, cut costs and improve the patients’ experience.
“The nasty surprise in this whole thing is that it also includes hip fractures that requires joint replacement. That’s a different kind of patient,” Thompson says, noting that these cases are often emergencies involving older, weaker patients than those with arthritis who elect to have a joint replaced.
Each team had to rethink the entire continuum of care, from pre-operative preparation to the procedure itself, billing strategies, relationships with inpatient and outpatient extended care centers, and patient outreach.
“We did not do it on our own. We had some excellent advice,” Thompson said, noting that the hospital first turned to the Geisinger Health System for guidance and now has joined the Cleveland Clinic’s network of affiliated hospitals. Both institutions are leaders in figuring out ways to provide high-quality, cost-efficient care.
“We’ve been doing what CCJR calls for in two of our hospitals for a year,” says Dr. John Bulger, Geisinger’s chief medical officer for population health.
Key To Efficiency
 One key to cost efficiency, Bulger says, is increasing the number of patients who can go home after surgery — which every patient prefers {Not true-many people really like them. I definitely advise going home because I think you can get further along if you have good teaching, but nonetheless many people like the camaraderie that SNF provides. Caregivers like it as well because it relieves them of the burden of helping and possibly having to take time off work.}–rather than into an extended-are facility. Another is to diligently gather data to make sure that any facility that takes over the care of a patient who has been discharged following surgery is also efficient, because a long stay could gobble up any savings.
One key to cost efficiency, Bulger says, is increasing the number of patients who can go home after surgery — which every patient prefers {Not true-many people really like them. I definitely advise going home because I think you can get further along if you have good teaching, but nonetheless many people like the camaraderie that SNF provides. Caregivers like it as well because it relieves them of the burden of helping and possibly having to take time off work.}–rather than into an extended-are facility. Another is to diligently gather data to make sure that any facility that takes over the care of a patient who has been discharged following surgery is also efficient, because a long stay could gobble up any savings.
Thompson said that physician charges account for about 15 percent of the cost of a joint replacement procedure. Hospital care accounts for about 40 percent of the cost. Remarkably, he said, post-acute care accounts for roughly the same percentage of the cost as the hospital stay, including surgery.
“That was a really surprising number when we saw these figures,” he said, calling the variation in average length of stay in different extended-care facilities, from 12 days in one center to 40 days in another in 2013, nothing less than “amazing.”
The longer the length of stay, the higher the cost, he said.
The differences in these facilities, both in quality and cost, have prompted Akron General to invite all extended-care centers in the county to come in and figure out a way to provide more efficient care. {Read cheaper, shorter care}
“Some worked with us hand-in-hand, almost as if they’re a part of our system,” Thompson said. “Some didn’t show up.”
It also prompted the hospital to sit down with patients and talk through their options, based on their growing knowledge of the facilities, the hospital’s relationship with them, the federal government’s star-rating system (one to five stars) and the length of stay reported in Medicare data.
“We clearly state that we have preferred providers,” Thompson said. “We never prevent a patient from making a choice, but we do counsel them.” {The hospital will definitely will be greasing the chute that they want the patient to slide down even more now that the amount of Medicare reimbursement is being tied to controlling costs post-hospitalization}
It will be at least a couple of months before Akron General gets its first inkling from Medicare on how well it’s doing. There are, however, a couple of indicators, not least the percentage of joint replacement patients who go home after surgery, which has risen to 60 percent from 45 percent.
And then, Thompson said, there are the reactions from patients who had one joint replaced at Akron General before the change began and another since. “Almost every single one says, ‘I can’t believe how much better this is.” {We’ll see. Count me a skeptic overall, especially for the long term}
Here is Medicare’s disclaimer on potential harms to beneficiaries on their fact sheet
Beneficiaries will benefit from protections including: additional monitoring of claims data from participant hospitals to ensure that hospitals continue to provide all necessary services; continued protection of patient data under the Health Insurance Portability and Accountability Act of 1996 (HIPAA) and other applicable privacy laws; and patient notification by providers and suppliers. Further, all existing safeguards to protect beneficiaries and patients will remain in place. If a beneficiary believes that his or her care has been adversely affected, he or she can call 1-800-MEDICARE or contact his or her state’s Quality Improvement Organization (QIO) by going to http://www.qioprogram.org/contact-zones. If concerns are identified, CMS will initiate audits and corrective action under existing authority.
November 5, 2015
I Have My Father To âBlameâ For The Knee Replacement Adult Cartoon Coloring Book






 It All Started With The Three Stooges
It All Started With The Three StoogesHe was a regular watcher of âThe Three Stoogesâ, a man who appreciated humor and who no doubt would have laughed when the organist much to her horror, inadvertently triggered some sexy Latin b eat during the middle of his funeral.
eat during the middle of his funeral.
So then it was only natural that I would seek to capture some of the humorous themes of recovery common to all ages in the form of a knee replacement adult cartoon coloring book.
If you are new to adult coloring you might be wondering what all the fuss is.
Adult coloring allows those who arenât as artistically gifted to engage in a creative process and reap the therapeutic benefits of art therapy.
âAdult coloring is a growing trend and consumers are really taking to the idea,â reports Matthew Lore of The Experiment Publishing group. âNot only is it calming and good for your health, itâs just fun! The demand is increasing exponentially as the word spreads.â
Meanwhile according to the Cancer Treatment Centers of America, researchers have conducted studies to explore the impact of laughter on health. After evaluating participants before and after a humorous event (i.e., a comedy video), studies have concluded that episodes of laughter helped to reduce pain, decrease stress-related hormones and boost the immune system in participants.
participants before and after a humorous event (i.e., a comedy video), studies have concluded that episodes of laughter helped to reduce pain, decrease stress-related hormones and boost the immune system in participants.
Officially, the American Lung Association recommends 52 stress reducers and coloring hits a few of them: disconnecting from phones, talking problems out with friends, focusing on one thing at a time, simplifying and doing something enjoyable.
Working with Dave Allred, an accomplished cartoonist, 21 unique and irreverently funny cartoons were created that double as coloring pages to bring laughter and stress relief to the knee replacement recovery journey. It’s called “Color And Laugh Your Way Through Knee Replacement Recovery” and it’s a fascinating new entry into the adult coloring book market. Its uniqueness lies in its combined emphasis on coloring as therapeutic stress relief and the use of humor as good medicine.
The 600,000 plus patients who undergo knee replacement surgery understand stress and discomfort. This little book will bring some laughter and joy to the process. Ninety-five percent of the time or more everything works out great but in the meantime mind and emotions tied in a wad of nervousness and fear can get the best of us.
My first book was created with the intention of instilling confidence and empowering patients and while it’s very successful there are still times where levity and/or quiet calm might just be the best medicine.
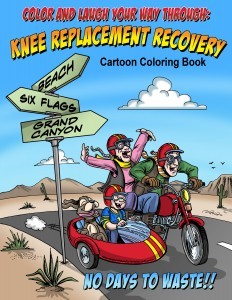 I hope youâll give the book a try and as always I value your feedback. The book is now available on Amazon.
I hope youâll give the book a try and as always I value your feedback. The book is now available on Amazon.
There is nothing like a great âWinston Churchillâ quote to brighten up the day and to round up a post on humor.
In 1946 Churchill meet Bessie Braddock, a plump Labour MP and Tory-hater, who told him: “Winston, you are drunk.” “Madam,” he replied, “you are ugly, and I will be sober in the morning.”
When Churchill was on a lecture tour of America and was served a buffet lunch of cold chicken, “May I have some breast?” he asked his hostess. “Mr. Churchill,” she replied, “In this country we ask for white meat or dark meat.” The following day Churchill sent her an orchid, with the message: “I would be obliged if you would pin this on your white meat.”
When Churchill was told, while he was in the lavatory, that the Lord Privy Seal had come to see him. “Tell the Lord Privy Seal that I am sealed in the privy and can only deal with one s*** at a time,” he bellowed.
Ah the Irish-English sense of humor, I do have my Father to blame.







I Have My Father To “Blame” For The Knee Replacement Adult Cartoon Coloring Book
He was a regular watcher of “The Three Stooges”, a man who appreciated humor and who no doubt would have laughed when the organist much to her horror, inadvertently triggered some sexy Latin b eat during the middle of his funeral.
eat during the middle of his funeral.
So then it was only natural that I would seek to capture some of the humorous themes of recovery common to all ages in the form of a knee replacement adult cartoon coloring book.
If you are new to adult coloring you might be wondering what all the fuss is.
Adult coloring allows those who aren’t as artistically gifted to engage in a creative process and reap the therapeutic benefits of art therapy.
“Adult coloring is a growing trend and consumers are really taking to the idea,” reports Matthew Lore of The Experiment Publishing group. “Not only is it calming and good for your health, it’s just fun! The demand is increasing exponentially as the word spreads.”
Meanwhile according to the Cancer Treatment Centers of America, researchers have conducted studies to explore the impact of laughter on health. After evaluating participants before and after a humorous event (i.e., a comedy video), studies have concluded that episodes of laughter helped to reduce pain, decrease stress-related hormones and boost the immune system in participants.
participants before and after a humorous event (i.e., a comedy video), studies have concluded that episodes of laughter helped to reduce pain, decrease stress-related hormones and boost the immune system in participants.
Officially, the American Lung Association recommends 52 stress reducers and coloring hits a few of them: disconnecting from phones, talking problems out with friends, focusing on one thing at a time, simplifying and doing something enjoyable.
Working with Dave Allred, an accomplished cartoonist, 21 unique and irreverently funny cartoons were created that double as coloring pages to bring laughter and stress relief to the knee replacement recovery journey. It’s called “Color And Laugh Your Way Through Knee Replacement Recovery” and it’s a fascinating new entry into the adult coloring book market. Its uniqueness lies in its combined emphasis on coloring as therapeutic stress relief and the use of humor as good medicine.
The 600,000 plus patients who undergo knee replacement surgery understand stress and discomfort. This little book will bring some laughter and joy to the process. Ninety-five percent of the time or more everything works out great but in the meantime mind and emotions tied in a wad of nervousness and fear can get the best of us.
My first book was created with the intention of instilling confidence and empowering patients and while it’s very successful there are still times where levity and/or quiet calm might just be the best medicine.
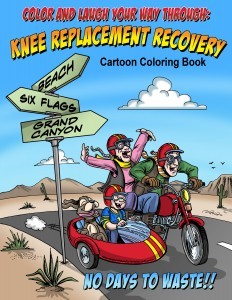 I hope you’ll give the book a try and as always I value your feedback. The book is now available on Amazon.
I hope you’ll give the book a try and as always I value your feedback. The book is now available on Amazon.
There is nothing like a great “Winston Churchill” quote to brighten up the day and to round up a post on humor.
In 1946 Churchill meet Bessie Braddock, a plump Labour MP and Tory-hater, who told him: “Winston, you are drunk.” “Madam,” he replied, “you are ugly, and I will be sober in the morning.”
When Churchill was on a lecture tour of America and was served a buffet lunch of cold chicken, “May I have some breast?” he asked his hostess. “Mr. Churchill,” she replied, “In this country we ask for white meat or dark meat.” The following day Churchill sent her an orchid, with the message: “I would be obliged if you would pin this on your white meat.”
When Churchill was told, while he was in the lavatory, that the Lord Privy Seal had come to see him. “Tell the Lord Privy Seal that I am sealed in the privy and can only deal with one s*** at a time,” he bellowed.
Ah the Irish-English sense of humor, I do have my Father to blame.
October 12, 2015
Use Your Brain And Go With Your Gut In Knee Replacement Protocol
Most readers know by now that I authored a book, available on Amazon, entitled; Fast Track Your Recovery From A Knee Replacement: How To Eliminate Pain and Pain Medicine The Fastest Way Possible.
A recent reader suggested in a review that including a chapter on ways to “move on” if the surgeon/hospital/PT is at odds with the knee replacement protocol defined in the book would be beneficial.
Here I offer up a few thoughts that might be of value on this subject without laying out an entire chapter.
First of all, I don’t know of any surgeon or hospital that would object to the principles laid out in this book and in fact the book has been read and reviewed by an excellent retired total knee surgeon of 25 years from the east coast.
 Secondly, the approach while having many similarities to conventional therapy prescriptions is different in emphasis, empowerment, volume of exercises and monitoring effectiveness. It is not different in kind like an owl being different than say a freshwater trout, but different in degree like a common trail horse being different than a race horse.
Secondly, the approach while having many similarities to conventional therapy prescriptions is different in emphasis, empowerment, volume of exercises and monitoring effectiveness. It is not different in kind like an owl being different than say a freshwater trout, but different in degree like a common trail horse being different than a race horse.
In the book I recommend a sequential emphasis, range of motion then strength and on to functional mobility with defined benchmarks qualifying your move to the next phase.
I also recommend a limited repertoire of exercises, the meat and taters so that you will wisely be able to ramp up your frequency without feeling overwhelmed and causing your faithfulness to flag.
“The greater the number of exercises in a routine the more likely you are to avoid the most difficult ones” is a truism that I have seen proven over and over again. So I keep the core number of exercises nice and compact.
In addition, I spend a lot of time trying to explain the rationale behind the method, hopefully setting you up to make quality decisions should some part of this be at odds with people on your particular path.
Because the method comes with benchmarks, tons of feedback and an emphasis on incremental stretching, I can’t conceive of a safer more protective way to recover.
Synergy
Think of this approach as a way of piecing together valuable tactics to accelerate the overall progress. Each tactic taken individually would not be as powerful. The more pieces you can add the more  synergy you create. This allows creativity when working with others.
synergy you create. This allows creativity when working with others.
If a therapist gives you a bunch of exercises and only one includes a focus on stretching into flexion, I would definitely try to change that ratio especially if you find yourself stagnant trying to improve your range.
If your therapist is encouraging a lot of early walking (first two weeks) and you are having trouble controlling your pain levels think about curtailing that a bit.
If your therapist is doing active assistive range, meaning they are helping you “push” your knee into greater flexion and you have a lot of soreness immediately following or the next day such that you don’t want to do anything, have a talk with your therapist about scaling that portion back and asking for other flexion exercises that can be done on your own.
Many therapists won’t see the real help that a low friction surface provides but on the other hand probably won’t object if you want to use one.
Most therapists will not have seen the FLEX bar but should intuitively recognize that it is just another method of leverage.
So if someone skims briefly through the book he might conclude there is “nothing new” and in a sense they are right “a horse” is “a horse”. But to someone who knows horses, there is a world of difference between a trail horse and a racing horse.
The book has been laid out so that the patient can hopefully understand the principles behind each prescription and make good decisions that will shorten recovery time from knee replacement surgery. Remember, I learned these techniques over the course of 20 years through trial and error helping hundreds of patients. Your therapist may have seen a limited number of “knees” and is relying on the basics taught in school.
 My final word is about trusting yourself and your ability to think. Do your exercises 2 times a day and then do them 4 times a day. How do you feel? What was the result of your stretching? Did it improve?
My final word is about trusting yourself and your ability to think. Do your exercises 2 times a day and then do them 4 times a day. How do you feel? What was the result of your stretching? Did it improve?
Perform your heel slides according to the book method and then do them without. Did it make a difference in effectiveness?
It’s hard for many older people to doubt the absolute expertise of the medical profession. Yet sadly there are abundant reasons in the 21century to be cautious and attempt to think for yourself, gathering information on your own and comparing that with the medical profession. This is not to scare you but to encourage you. Use your brain and go with your gut.
October 6, 2015
ICD-10 Devilish Interference In Healthcare
The ICD-10 code, created in 1983, was finally implemented here in the US on October 1st,2015 and it is all about the details. The devil is in the details as they say and you can believe that the devil is in the ICD-10 code. A recent article goes to the heart of the problems. Healthcare once about people and healing, is now about coding and quantifying.
Quantifiers and coders are looking at healthcare essentially from the outside and healthcare professionals are looking from the inside. Quantifiers and coders want data for what you ask, for everything from billing to monitoring results of treatment, quality of care, to identifying outbreaks of disease, causes of death and community health needs etc., etc., etc..
 I am reminded of a short essay by C.S lewis called Meditations in a Toolshed
I am reminded of a short essay by C.S lewis called Meditations in a Toolshed
I was standing today in the dark toolshed. The sun was shining outside and through the crack at the top of the door there came a sunbeam. From where I stood that beam of light, with the specks of dust floating in it, was the most striking thing in the place. Everything else was almost pitch-black. I was seeing the beam, not seeing things by it.
Then I moved, so that the beam fell on my eyes. Instantly the whole previous picture vanished. I saw no toolshed, and (above all) no beam. Instead I saw, framed in the irregular cranny at the top of the door, green leaves moving on the branches of a tree outside and beyond that, 90 odd million miles away, the sun. Looking along the beam, and looking at the beam are very different experiences.
But this is only a very simple example of the difference between looking at and looking along.
C.S Lewis argues that ,”One must look both along and at everything. In particular cases we shall find reason for regarding the one or the other vision as inferior.”
Forcing healthcare workers to look at healthcare in the manner of the ICD-10 code results in an endless preoccupation with data entry and proper quantification. The living experience of looking along the healthcare beam of light is wreaked in the process. Minds become fixated on something other than care, practicing the art of medicine, and healing. No wonder indeed that Doctors and other healthcare workers are burnt out. The brave new world of healthcare will end up being just that, healthcare for the brave.
Please read this excellent article by Shirie Leng, MD
ICD-10: No wonder why doctors are burnt out
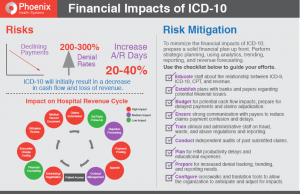
http://www.phoenixhealth.com/Offers/F...
Attention graduates! If you’re looking for a career with a ton of job prospects, look no further than an international classification of diseases coder. This fun and fulfilling career will take you into new worlds of diagnosis, laterality, specificity, and nitpicky-ness as you dive into thousands of columns of numbers and qualifiers. You’ll even get to call doctors and harass them anytime you want. Sign up for your free brochure and get started on the career of your dreams now!
Yes, friends, after two years of delays, ICD-10 is coming to a doctor near you on October 1st. Mark your calendars. To review:
1. ICD-10 stands for the International Classification of Diseases, version 10. The ICD is, according to the World Health Organization, (www.who.int) which publishes and maintains it, “the standard diagnostic tool for epidemiology, health management, and clinical purposes. It is used to monitor the incidence and prevalence of diseases, providing a picture of the general health situation of countries.” In the U.S., the ICD has been adapted for billing.
2. Work on ICD-10 started in 1983, but here, the U.S. Department of Health and Human Services still used ICD-9 (with modifications called ICD-9-CM) until 2013, after which it was delayed twice by Congress.
3. The ICD coding system attaches a number for every disease or trauma known to mankind. For example, if you have a broken forearm you have an ICD-9 base code of 813. If it is a closed fracture (the skin was not broken), you’re an 813.0. If it is the lower end of the arm, you’re an 813.40. If your skin was also broken, and the bone poked through, you’re at an 813.50. If you only broke your radius, but the skin was broken, you’re an 813.52. And so on.
4. There are other codes you need too. Your broken arm will need to be splinted, which requires a current procedural terminology (CPT) code or an ICD-10-PCS code, depending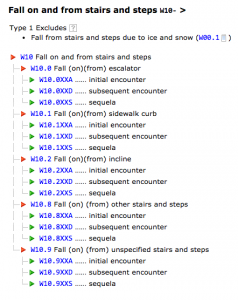 on if you are going home from the ER or have been admitted to the hospital. The Healthcare Common Procedure Coding System (HCPCS), which wrote the CPT codes, also has level II CPT codes for ambulance services, crutches, etc. There are also “E-codes” to record external causes of injury (vs. breaking your own arm, I guess). And there are V codes for supplementary classification of other problems you might have that relate. So if you broke your arm while pregnant, you might be an 813.0V22. I think.
on if you are going home from the ER or have been admitted to the hospital. The Healthcare Common Procedure Coding System (HCPCS), which wrote the CPT codes, also has level II CPT codes for ambulance services, crutches, etc. There are also “E-codes” to record external causes of injury (vs. breaking your own arm, I guess). And there are V codes for supplementary classification of other problems you might have that relate. So if you broke your arm while pregnant, you might be an 813.0V22. I think.
5. A whole industry has been created around these codes. Hospitals hire professional coders whose job it is to read through patient records and determine the correct ICD codes to submit to Medicare. Hospitals also hire computer programmers or computer software companies to link hospital data systems to these codes.
So, why do we need new codes? What’s wrong with the old ones? About 100,000 things. That’s the number of new ICD codes that have been created. These new codes require much more specific information. Now your broken arm is classified according the type (open or closed), pattern (spiral or oblique etc.), etiology (how it happened), healing status (in subsequent visits), localization (head, neck, distal, proximal) displacement, classification (Colles vs. Salter-Harris etc.) and laterality (right or left). Because breaking your left arm is pretty cheap but breaking the right will cost you, I guess.
In ICD-10, your broken arm makes you an S52. Which is, of course, way cooler. If you broke the distal (far) end of your radius you are an 813.4 in ICD-9 but in ICD-10 you could an S52.51 or S52.52 depending on which arm. You could also be an S52.516 or S52.519 or S53.517, depending on alignment and classification. If this is the first time you are being seen for your broken arm, you might be an S52.511A.
The purpose of all this, say the experts, is more specific data collection. According to the New York Times:
The new codes will … make it easier for insurers and federal officials to measure the results of treatment and the quality of care — factors increasingly used in deciding how much to pay doctors and hospitals. Public health officials say the new codes will help them identify outbreaks of disease, causes of death and community health needs. Researchers say the data will help them evaluate new treatments and procedures.
I would also add that coding companies and health care data companies will also benefit greatly.
OK, you say, but the actual dollar reimbursement amounts won’t change, so who cares? Let the coders take care of it. Doctors care. A lot. Who do you think is recording all this extra data? Doctors. The amount of information about the patient that the doctor knows doesn’t always change, but how much of it has to be documented does. It is all about documentation. If that coder doesn’t see it written down somewhere, that coder will call the doctor, or code wrong. If they code wrong, the doctor doesn’t get paid, and the bill goes to you, the patient. There is no short-term benefit for the doctor, but the documentation required goes up significantly. ICD-10 gathers more data. Doctors do the gathering and the typing. Which is what we went to medical school for.




