Michelle Stiles's Blog, page 2
July 25, 2018
Opioids After Knee Replacement: How Long?
 How long do you need to use opioids after knee replacement surgery is a common question? Do you need to get back to work and wonder how long before you can drive? Opioid use and driving do not go together. If an accident occurs and you are still taking opioids it could land you in serious legal trouble.
How long do you need to use opioids after knee replacement surgery is a common question? Do you need to get back to work and wonder how long before you can drive? Opioid use and driving do not go together. If an accident occurs and you are still taking opioids it could land you in serious legal trouble.
Many people also worry about opioid addiction following surgery, since they have read or heard about the increasing rates of addiction to prescription pain medications.
Maybe you are just interested in finding out how long the most intense pain lasts and what the typical pain management protocol is like.
The well researched answer is, less than 10% of people who don’t use opioids before surgery are still taking them at 6 months, but that data doesn’t really answer questions about going back to work and driving which you will need to start doing much sooner especially if you are pre-retirement.
How to Effectively Use Opioids After Knee Replacement
My advice, which I offer in more detail in my book, is simply this. The first two weeks you will experience a great deal of chemical pain, which is related to the molecules that rush into the area in an acute injury; and bone pain, pain that is caused by cutting the ends of the long bones. Most people in order to feel comfortable will need some type of opioid during this time to get them through. Opioids have some well known side effects like nausea in limited cases, constipation quite frequently and well let’s just call it brain fog.
Constipation can usually be managed effectively with a preemptive strategy, taking in plenty of water, taking over the counter prescriptions for constipation before you get constipated and paying attention to the types of food you eat. Consuming lots of cheese and meat, which are tough to digest, will exacerbate the problem.
I recommend taking the opioids after knee replacement during this two week time period at the prescribed levels on a time managed program (meaning take them every __ hours even before you start to experience pain) and work your tail off on your range of motion, the hardest task to complete following a knee replacement.
Since you need to be on the pain medicine secondary to the chemical and bone pain, use it to your advantage and knock out the hardest task out right at the start. Most of my patients can get off of narcotics after the week two if they follow the program and transition to over the counter medications allowing them to drive and return to work sooner than average.
The Biggest Mistake With Pain Managment
 The biggest mistake most people make is not utilizing the opioids to their fullest extent early when they are really needed, focusing on restoring range of motion first and foremost. If the range task lingers, so will the opioid use, they go together hand in glove.
The biggest mistake most people make is not utilizing the opioids to their fullest extent early when they are really needed, focusing on restoring range of motion first and foremost. If the range task lingers, so will the opioid use, they go together hand in glove.
If you’ve restored your range of motion and are slowly progressed your strength exercises you should not have a great deal of pain going forward.
The longer one takes an opioid prescription, the more difficult it will be to get off opioids after knee replacement surgery, which leads into this next section about the consequences of using a lot of opioid pain medication prior to surgery.
Opioid Use Before Surgery Leads to Longer Use After Surgery
Only 8.2% of opioid naïve patients (those who had not used opioids prior to surgery) were using opioids at 6 months, while 53.3% of knee replacement patients who reported opioid use the day of surgery continued to use opioids after knee replacement at 6 months.
The strongest predictor of long-term opioid use was taking high-dose opioids before surgery or anything greater than 60 mg of oral morphine a day.
Calculate Your Risk
You can calculate your morphine milligram equivalent MME using this handy conversion graphic put out by the CDC which shows you how to convert other prescription pain medicines into an equivalent morphine dose so you can determine how close you are to this important threshold.
 Those patients taking >60 mg oral morphine equivalents preoperatively had an 80% likelihood of being on opioids after knee replacement at 6 months postoperatively.
Those patients taking >60 mg oral morphine equivalents preoperatively had an 80% likelihood of being on opioids after knee replacement at 6 months postoperatively.
Other preoperative characteristics associated with persistent opioid use at 6 months were worse pain and functioning, which seems logical, symptoms of depression, and greater catastrophizing (exaggerated responses and worries about pain). [7]
Researchers have theorized that continued opioids after knee replacement surgery could be related to other new pain that has emerged, overall body pain, and dependence, self-medicating for emotional distress and hyperalgesia. Remember that term, hyperalgesia because we are going to get back to it later in the article.
Pre-operative Opioid Use and Poor Outcomes
The bad news is that the inability to get off opioids after knee replacement surgery isn’t even the worse outcome of pre-operative opioid use.
Studies have illustrated that chronic preoperative use is associated with worse self-reported outcomes, longer hospitalizations, increased stiffness, higher rates of complications and failures, and higher risk of in-hospital morbidity and mortality following knee replacement surgery. [1-7]
The most recent large-scale study (2018) showed that revision rates and thirty-day re-admission rates were also higher. Researchers concluded that at one year, patients who had been on pre-operative opioid medication for greater than 60 days had 61% and 59% higher odds of revision at one year and 3 years respectively.
The poor outcomes associated with prior opioid use is not limited to knee replacement surgery but includes other varied procedures including bariatric surgery, trauma recovery, kidney transplants and anterior cervical arthrodesis surgery.
So the facts are in, pre-surgical opioid use really throws a wrench in a smooth and successful knee replacement surgery.

Take Home Points
If at all possible, do not start on the opioid prescription route prior to your surgery.
Then what can I do?
Interestingly whole body pain and depression are associated with low-grade body inflammation as the common precursor of all three; diffuse body pain, joint destruction and pain and depression.
Try to make some diet and lifestyle changes like implementing a whole food diet, lowering stress levels and supporting detoxification pathways. These are possible avenues of relief BEFORE resorting to opioid pain medications.
This is true especially if you have pain in both knees and no history of traumatic joint injury because a systemic problem like low-grade inflammation would indiscriminately target both knees. Known issues with biomarkers for inflammation like C-reactive protein and interleukin would be another clue that whole body inflammation could be an issue.
Attempt to taper off opioids prior to surgery to ensure a more successful outcome.
This is of course easier said than done and may require you to get support and assistance but it would be better to face the music before surgery so that you don’t multiply your trouble during knee replacement recovery by having to suffer though a infection in the knee or an early revision both of which could have devastating consequences for the long term function of that knee.
Talk to your primary physician or your orthopedic to create a plan. You should never just stop your opioid prescriptions suddenly as this can lead to dangerous side effects.
The Problem of Paradoxical Pain
A little known phenomenon of chronic opioid use is something called hyperalgesia, which means an increase in pain. This is a paradoxical effect. The remedy that is supposed to reduce pain is actually increasing it. Paradoxical effects can occur with other medications like those taken for depression. At times the very same medication that help some, will cause suicide or violence in others. There is still much we do not know about the effects of medications.
A study in 2015 reported that, “although the effect of opioid tolerance and dependence has gained considerable attention, the problem of opioid-induced hyperalgesia—characterized by a paradoxical increase in pain sensitivity—is a less recognized consequence of opioid use.” [9] In fact, it is little known and little studied.
Bob’s Story
I am going to finish by telling you a story of a friend of mine. Let’s call him Bob. He injured his shoulder doing construction and ended up having three different surgeries on that arm over the course of 10 years. He experienced a growing reliance on opioids for pain relief and yet still had 7-8 out of 10 pain in his shoulder.
During that period, he also gained 30 pounds, experienced increase difficulty with his COPD requiring new medications, he become diabetic and was placed on Metformin, was started on another controlled substance, Lyrica for pain relief and experiencing swelling in his leg for which he took a water pill.
After a snafu with his insurance resulting from a cross country move and loss of paperwork he ended up without insurance to pay the close to $2000 worth of medications he needed each month. Being a crusty Vermont soul, he decided the only thing he could do was go cold turkey. (Do not try this yourself!) Bob was lucky, despite significant withdrawal symptoms and a 911 call that resulted in a recommendation to be hospitalized, he persevered and to everyone’s amazement got radically better in all areas.
Bob Hit The Rewind Button and Look What Happened
Within 6 months, Bob was no longer diabetic. He had lost 3o pounds. His feet no longer swelled so he had no need of the water pill. He no longer needed meds for COPD because his pulse ox stayed in the mid to high 90’s.
Most significantly his pain was now only 3 out of 10 and controlled by over the counter Advil.
This is an example of hyperalgesia. Bob’s pain was being made worse on opioids and causing a host of other downstream issues. I realize that this is anecdotal but I share this story a lot because most people have never heard of anyone getting off their medications and showing improvement in a number of conditions that most people think of as chronic.
If you are facing knee replacement surgery and are currently on opioids, think twice about proceeding without first investigating whether the pain pills themselves may be causing increased pain sensitivity. Create a plan with your doctor.
If you are opioid naïve going into surgery, use them wisely for the purpose of gaining your range of motion back and feeling tolerable in the first two weeks. Sparing opioid use with attempts to gut it out will result in a longer knee replacement recovery and overall longer use of the pain medicines.
Resources
[1] Menendez ME, Ring D, Bateman BT. Preoperative opioid misuse is associated with increased morbidity and mortality after elective orthopaedic surgery. Clin Orthop Relat Res. 2015 ;473(7):2402–12. Epub 2015 Feb 19
[2] Zywiel MG, Stroh DA, Lee SY, Bonutti PM, Mont MA. Chronic opioid use prior to total knee arthroplasty. J Bone Joint Surg Am. 2011 ;93(21):1988–93.
[3] Namba RS, Inacio MCS, Pratt NL, Graves SE, Roughead EE, Paxton EW. Persistent opioid use following total knee arthroplasty: a signal for close surveillance. J Arthroplasty. 2018 ;33(2):331–6. Epub 2017 Sep 13.
[4] Bedard NA, Pugely AJ, Westermann RW, Duchman KR, Glass NA, Callaghan JJ. Opioid use after total knee arthroplasty: trends and risk factors for prolonged use. J Arthroplasty. 2017 ;32(8):2390–4. Epub 2017 Mar 16.
[5] Rozell JC, Courtney PM, Dattilo JR, Wu CH, Lee GC. Preoperative opiate use independently predicts narcotic consumption and complications after total joint arthroplasty. J Arthroplasty. 2017 ;32(9):2658–62. Epub 2017 Apr 12.
[6] Cancienne JM, Patel KJ, Browne JA, Werner BC. Narcotic use and total knee arthroplasty. J Arthroplasty. 2018 ;33(1):113–8. Epub 2017 Aug 17.
[7] Goesling J, Moser SE, Zaidi B, Hassett AL, Hilliard P, Hallstrom B, Clauw DJ, Brummett CM. Trends and predictors of opioid use after total knee and total hip arthroplasty. Pain. 2016 ;157(6):1259–65.
[8] Weick, J, Bawa, H, Dirschl, D, Luu,H. Preoperative Opioid Use Is Associated with Higher Readmission and Revision Rates In Total Knee and Total Hip Arthroplasty The Journal of Bone & Joint Surgery. 2018;100(14):1171-1176.
[9] Trang T, Al-Hasani R, Salvemini D, Salter MW, Gutstein H, Cahill CM. Pain and Poppies: The Good, the Bad, and the Ugly of Opioid Analgesics. The Journal of Neuroscience. 2015;35(41):13879-13888. doi:10.1523/JNEUROSCI.2711-15.2015.
June 28, 2018
Depression After Knee Replacement Common and Should Be Addressed
Studies show that depression after knee replacement surgery is higher than other surgical patients, despite knee replacement surgery being seen as a “new lease on life”. But even more concerning is that it may lead to worse outcomes unless addressed.
A new research study “Perioperative inpatient Use of Selective Serotonin Reuptake Inhibitors Is Associated With a Reduced Risk of THA and TKA Revision,” recently published in the June 2018 edition of Clinical Orthopaedics and Related Research found that treating depression with selective serotonin reuptake inhibitors resulted in lower revision rates with knee replacement surgery.
The co-author, Hilal Kremers M.D. explained, “Arthritis patients with chronic joint pain commonly present with depression and various other mood disorders.”
“Previous studies suggest that when depressed arthritis patients undergo total hip or knee arthroplasty, they continue to experience worse functional outcomes, more surgical complications and more hospital readmissions.”
Anti-depressants Lowered Adverse Results
Lower complication rates of knee replacement surgery resulted from use of Serotonin Reuptake Inhibitors, a particular class of depression drugs used in the study.
While you can treat depression drugs, there are many people who avoid going that route. Color and Laugh Your Way Through Knee Replacement Recovery, a coloring book for knee replacement patients was designed to use coloring as a stress reliever and laughing as an antidote for depression both of which have been shown to be useful to patients in the post-surgical recovery period to keep patients positive and optimistic.
The knee replacement coloring book consists of 20 full page illustrations designed by expert illustrator Dave Allred to bring irreverently humorous scenarios to life: scenarios that help patients turn the table on their frustrations and challenges and instead poke fun at them.
While taking pain medication generally limits more robust intellectual activities like reading and doing work at home, patients have found that coloring pages is a suitable alternative that provides hours of calming diversionary activity.
Laughter Is Good Medicine
 The Mayo Clinic reports that clinical research backs up the idea that laughter is good medicine. In fact, laughter doesn’t just lighten your mental load but it can actually induce bodily changes such as stimulating organs, activating and relieving your chemical stress response and soothing tension in stressed muscles.
The Mayo Clinic reports that clinical research backs up the idea that laughter is good medicine. In fact, laughter doesn’t just lighten your mental load but it can actually induce bodily changes such as stimulating organs, activating and relieving your chemical stress response and soothing tension in stressed muscles.
Meanwhile according to the Cancer Treatment Centers of America, researchers have conducted studies to explore the impact of laughter on health. After evaluating participants before and after a humorous event (i.e., a comedy video), studies have concluded that episodes of laughter helped to reduce pain, decrease stress-related hormones and boost the immune system in participants.
Patients and caregivers alike are having great fun with the book. We now know that many knee replacement patients are struggling with depression after knee replacement as well as the challenges of the surgery itself.
What Users Are Saying
Got this after my first and before my second knee replacement. PERFECT! The author has really captured the entire recovery process very well. If you are heading for a knee replacement, or if you have a family member or friend getting one, this book, a set of first rough weeks of recovery! I showed this to my Orthopedic Surgeon during a follow up visit, he roared with laughter as he paged through it.
I bought this for my mom, who is a nurse, and she LOVED it!! These pages are filled with funny, but actual, situations patients will encounter before and after surgery!! Boredom will make the nicest person turn into a clawing crab and this book along with word searches and crossword puzzles are a must post op!!! I made copies and took to her PT appointments for the therapist to laugh at!! Every doctor should put these along with coloring pencils in a goody bag for their patients!! Five stars from me!!
I got this for a friend who had a knee replacement and she got so much happiness from it. I am glad I chose this book. She took it to show her Therapist and she said the Therapist was going to order some too. She said they laughed and laughed reading it. Thanks for the great product & service.
Instead of picking up a get-well card, flowers or even candy, which is detrimental to recovery; give the gift of laughter and enjoyment to bolster patients’ spirits and promote physical well-being during the knee replacement recovery period.
Resources
Patryk Stecz, Magdalena Wrzesińska, Klaudia Tabała, Katarzyna Nowakowska-Domagała. (2017) Emotional Distress Associated with Surgical Treatment and its Relationship with Coping Profiles Among Chronically ill Older Patients. Current Psychology 36:1, pages 174-183.
Summary
Studies show that depression after knee replacement surgery is more common than in other surgeries and correlated with worse outcomes. Coloring book promotes laughter and stress relief in patients as a drugless antidote to depression.
May 18, 2018
Thinking About Taking A Flight After A Knee Replacement?
 As tempting as it might be to get away after your knee replacement surgery to some place warm and comforting, it’s time to reconsider that idea. New research presented at the 2018 Annual Meeting of the American Academy of Orthopaedic surgeons (AAOS) shows an increase risk of deep vein thrombosis (VTE) in those who took flights to and/or from the hospital compared to those who did not. [1] So if you are planning to have knee replacement surgery sometime soon, don’t schedule any airline flights in the time period around the surgery if possible.
As tempting as it might be to get away after your knee replacement surgery to some place warm and comforting, it’s time to reconsider that idea. New research presented at the 2018 Annual Meeting of the American Academy of Orthopaedic surgeons (AAOS) shows an increase risk of deep vein thrombosis (VTE) in those who took flights to and/or from the hospital compared to those who did not. [1] So if you are planning to have knee replacement surgery sometime soon, don’t schedule any airline flights in the time period around the surgery if possible.
VTE is a serious complication that can follow hip and knee replacement surgery, in the form of a blood clots, and is a leading cause of death and disability worldwide. [2] Although the exact incidence of VTE is unknown, it is believed that 10 million cases occur annually. [2] Risks for VTE include extended hospital stays, surgery and long periods of not moving (e.g., bed rest or long-duration travel). [3]
Patients in the study flew at a mean of six days following knee replacement surgery (range 1-24days) and the mean flight time was 74 minutes (range of 40-85).
No ideas behind the mechanisms causing the increased deep vein thrombosis were given.
In Summary
Blood Clots are a potential complication from knee replacement surgery.
Prolonged bed rest or long duration travel can increase the risk
Taking a flight after a knee replacement may heighten the risk of a blood clot
May 15, 2018
Forced Air Warmers Like Bair Hugger-Do They Increase Your Chance of Infection?
“Bair Hugger” is a trade name of a forced-air warming blanket that has been used now in over 200 million surgeries. There are approximately 4000 people currently suing 3M Co. alleging the unit caused debilitating deep-joint infections. See one mans disaster story here
Two decades ago, Dr. Augustine, an anesthesiologist in Minnesota, helped pioneer the idea that keeping a patient warm during surgery would lower bleeding and improve recovery. Augustine went on to develop a patent that changed surgical practices and made him a good deal of money.
 This is where it gets complicated. In 2002, Augustine resigned as chairman and CEO of his company Arizant, later acquired by 3M for $810 million.
This is where it gets complicated. In 2002, Augustine resigned as chairman and CEO of his company Arizant, later acquired by 3M for $810 million.
In 2009, Dr. Augustine and Arizant settled a court battle related to Medicare Fraud involving a different device Augustine had created, paid a $2 million fine and barred from participating in federal health care programs
A short time later, Dr. Augustine then turned around and successfully sued Arizant in Minnesota state court for the 2 million in Medicare fines plus 3 million more in unpaid salary, receiving 5 million total.
Dr. Augustine contends that he created the new device, “The Hotdog“, because he came to believe that the accumulation of waste air from the device under the surgical table was changing the sterile airflow dynamics in the surgical room causing higher than normal infections in patients receiving implant devices like artificial heart valves and joints.
Arizant executives have been accused by Dr. Augustine, of covering up the device’s problems. Arizant has sued Augustine’s new company charging that it is distributing information that falsely disparages the “Bair Hugger”.
Is Dr. Augustine an honest whistleblower? Did his findings or concerns about the potential dangers of the “Bair Hugger” cause him to be ousted by his original company, which sought to conceal the danger and retain market share?
Or is Dr. Augustine a malcontent whose difficult personality caused company conflict? Was he irritated enough by his perceived mistreatment that he patented a new product as a direct competitor with the old product while continuing to disparage his original company and product to extract revenge on Arizant?
I am afraid that I can’t answer those questions but all of the studies found at the bottom of this page seem to conclude that the air flow dynamics of the surgical room are being changed by the forced air warmer. What they can not conclude is that this dynamic actually caused the surgical site infections until a broader based study is completed.
Hence, in the meantime, it seems highly prudent to avoid forced air warmers for knee replacement surgery especially when there are other alternatives until more definitive evidence is obtained.
Dr Augustine-In His Own Words
Sometimes it is also helpful to listen directly to the person in question to get to the truth of a matter.
Here is a video of Dr. Augustine being interviewed. He directly answers the question about the problems related to forced air heating devices 3:25 into the video.
Studies Related to Forced Air Heating and Infection
Summary
“Until the disruptive effects of forced-air warming on ventilation can be fully evaluated with regard to affecting the sterility of the surgical site, the use of air-free patient warming alternatives might be recommended for procedures involving implants carried out in ultra-clean theatres.”
Summary
“This study does not show that forced-air warming increases the risk of infection – only that in certain types of theatre set-up it can significantly disrupt unidirectional airflow and draw particles from the potentially contaminated area below the sterile surgical field. This is a concern.”
Summary
“The benefits of maintaining normothermia during the perioperative period are without doubt. Many studies suggest that disruption of UCV airflow by FAW [Forced Air Warmers] is significant but the effect on SSI [Surgical site Infection] rates in implant surgery has yet to be determined by robust level 1 evidence.70 We recommend consideration of the use of alternative patient warming devices when performing orthopaedic hip and knee implant surgery until a definitive trial can be performed, but that some caution in condemning FAW [Forced Air Warmers] should be observed.
June 17, 2017
Don’t Be a 510K Knee Replacement Guinea Pig







Most people assume that the FDA fully vets all new medical devices including knee replacement implants. They assume that they have been tested and determined to be safe and effective before they are placed on the market and sold to the American people.
Unfortunately that is not the case.
The 510K PreMarket Approval Process
The 510K as it is called allows companies to rapidly get approval for a knee replacement implant by providing evidence of itsâ similarity to another device currently being marketed.
According to Drug Safety News, “this fast-track process is often abused by deceitful companies who want to skip the many complex clinical trials they are required to plan before a product is approved. The 510(k) regulatory pathway is, in fact, used to bypass the long testing phases whenever a medical device is âsubstantially equivalentâ to others already found on the market.”
The bottom line is that new design or composition changes in knee replacement implants are in reality tested on you the unwary consumer who has no idea how the process works.
Voluntary Registries
In many countries voluntary registries which track data on knee replacement surgeries are used to identify when an implant might be trending toward failure or harm. This data is closely monitored when a trend is identified and it is usually up to the implant manufacturer to initiate the recall.
However in the United States, the registry data is still very small compared to the number of devices that are implanted. So a recall is usually initiated through lawsuits or public outcry. In rare cases the FDA will raise concerns or request a recall from the manufacturer.
This after the fact surveillance while helpful to all the stakeholders is a poor substitute for real assurance about safety and reliability. I doubt potential knee replacement candidates will sleep any better knowing the registry exists.
Between 2003 and 2013 there were 709 recalls of devices or components of knee replacement implants. Buyers beware.
Of course there is always a balance between, the cost of doing clinical trials and the advantages of getting devices to the market quickly that can help people. Except we are not talking about a miracle drug or a tweaked design capable of making a quantum leap in knee replacement outcomes or user experience.
The Last Fly in the Ointment
And finally the last best-kept secret is the amount of money that some surgeons make in the form of consulting fees from the implant companies. For a new design to make money, some surgeons need to start using it. If a surgeon is not convinced that a major improvement is being gained through the adoption of this new technology, why not stick with the devil he knows? A little bit of cash as a consultant can solve that problem.
Are you starting to think of a few more questions you would like to ask your surgeon before you agree to have your knee replaced? Â I hope so.
Sources:
https://drugsafetynews.com/2017/05/03/not-hidden-dangers-medical-devices-approval-process/
https://www.drugwatch.com/knee-replacement/recalls/
American Registry  http://www.ajrr.net/







June 14, 2017
You’ll Want To Go Home After Knee Replacement Surgery When You Know These Three Things







Where should you go after knee replacement surgery, home or to a skilled nursing facility? My choice is home hands down and here is why…
Bugs, Bugs, Bugs
Even the best-managed and highest-ranking facilities have vulnerabilities in this area. Letâs face it, there are many immune-compromised individuals being housed together and there is a lot of foot traffic in and out from visitors as well as health care professionals.
These places are a ripe environment for things like the common cold, flu and pneumonia. Even worse you could be coming in contact with clostridium difficile, various staph infections as well as the grand pappy to be avoided MRSA. MRSA stands for methicillin-resistant staphylococcus aureus, a gram-positive bacterium that is genetically different than other strains of Staphylococcus aureus. MRSA is responsible for several difficult-to-treat infections in humans.
Of course in an ideal world staff would always wash their hands and never come to work sick. They would never improperly change the bandage on your wound and you would never have to eat lunch next to a person who is sick or lay on a non-disinfected treatment table, but of course this is not a perfect world. Get my drift.  Go home to your own limited bug set
Control, Control, Control
Do you like to stay up late and sleep in? Think it would be a good idea to eat the food that works best for your system after knee replacement surgery? Do you prefer to sleep in your own bed at night? Want to get up in the middle of the night when you canât sleep and do some exercises? All this and more is possible at home after after knee replacement surgery.
Progress, Progress, Progress
Get ahead and stay ahead of the âSlackersâ that go to rehab. Ok I am just kidding here, but seriously I know you can get better faster at home. You are not likely to be waited on and that is a good thing. It means you will get up and move more frequently. You can avoid the big time waste of 2 hours a day of OT! Sorry my OT friends and colleagues, but knee replacement patients need to get cracking on the main event- the knee replacement rehab.
But What if…
You might be single, divorced, retired and widowed but do not let that deter you. The first 24-48 hours at home are the hardest when you are transitioning from the hospital meds to oral narcotic pain pills. That would be a good time to have someone around for general support and encouragement. But after that you should be able to reheat meals, get your own ice bag and carry on with your knee replacement rehab program at home.







June 5, 2017
Knee Replacement Information All Sounding the Same?






 All knee replacement information is not created equal.
All knee replacement information is not created equal.A cursury review of the major sites offering wisdom on knee replacement surgery will yield very similar information, all very polly annish, surface level and vanilla sounding. This is because a critical review of real pitfalls and potential hazards has been systematically eliminated leaving nothing but glib and trite sounding pseudo- information.
The following video provides some analysis as to why this is so and how to recognize it.
We utilize the following principles to analyze what exactly is going on.
1. Follow the Money
2. It’s Generally not a good idea to piss off your customer base.
We will also identify and take a look at the following realities…
âAuthorityâ Sites- What are they and how they impact searching for information
Sponsorship/advertising- Where to look for that information and how that impacts the content available to the average truth seeker.
A deeper look at editorial guidelines and policy statements and whether they can be trusted- of course not
Content Farms- How some content is provided to the major authority sites
Summary
Determining who is controlling the knee replacement information and/or who is paying for its’ distribution will go a long way toward being able to identify versions of the knee replacement story that might be more fiction than reality.
Someone is “paying” for you to get free information and in fact it is the very people that are profiting from you having knee replacement surgery in the first place. How detailed or honest do you think they are going to be?
If you want more accurate information you need to identify better sources of information. This site is one example. Other than a small income from book sales that trust me does not come close to my “day job” income, I have no horse in the game other than your successs.
Why Does This Matter?
Everyone knows a few people who have had knee replacements. Some may have turned out great â¦.others not so much.
You want knee replacement information that ensures your total knee surgery will be one of the sucess stories!!
Get the Inside scoop.. Subscribe to my You Tube Channel to get regular updates so that you can avoid the crucial pitfalls. And remember if you want one of your knee replacement questions answered, please leave a comment on my you tube channel.







May 21, 2017
Knee Replacement Surgery Information-Unvarnished







No sugar coating here. You want the truth and I aim to please.
Warning this site is different than most other sites regarding knee replacement surgery and the recovery period that follows. I receive no income from the manufacturers or distributors of knee replacement implants or designs. I do not work for any facility nor am I compensated by any surgeon or surgical group involved in knee replacements. I also do not accept ads by any parties involved in the surgical implantation of knee replacements.
I am a physical therapist by trade for the past 25 years and have worked with hundreds of patients recovering from knee replacement surgery.  I have a few books available for purchase on Amazon as well as a downloadable PDF available on this site.
Regardless of whether or not you ever choose to buy one of my products, the information given reflects my opinion and is provided to help you navigate the maze of knee replacement information available on the net.
True Dangers and Pitfalls Explained
My purpose in creating this site is to give you a much deeper level of understanding than can be obtained from the plain vanilla information that masks the true dangers and pitfalls of such an important surgery. Taking a knife to your God-given knee is an act that cannot be undone and should not be undertaken lightly. I want you to know all the inside Intel that I personally use to counsel friends and family.
On this site I delve into the demographics, the trends, the marketing hype and the little known shenanigans that occurs behind the scenes by the big implant companies. Three quarter of a million knee replacement surgeries are performed yearly in the United States alone and it is Big Money. Donât let them take you for a ride at your expense!
 I created a manual to go with the flex bar on Amazon (which by the way will be back in stock shortly) It was previously only available with that purchase but will be available soon by PDF download on this site. For those who are a bit shy about trying my method, it goes into greater detail in outlining the step-by-step procedure than the original book.
I created a manual to go with the flex bar on Amazon (which by the way will be back in stock shortly) It was previously only available with that purchase but will be available soon by PDF download on this site. For those who are a bit shy about trying my method, it goes into greater detail in outlining the step-by-step procedure than the original book.
Take advantage of the free PDF regarding the 7 Things Your Surgeon Wonât Tell You Unless You Know To Ask because it contains most of the important information in one easy read rather than scattered about in various posts and can be used as a handy reference.
And finally, I have spent the last year adding to my expertise by becoming a Certified FDN Practitioner and a level one certified Precision Nutrition Counselor. Expect to hear much more from me on how you can use nutrition and lifestyle changes to AVOID a knee replacement in the first place.
I welcome your comments and suggestions to make this site even better. At times people have had problems finding the bonus freebies from my book. Please use the contact me tab rather than leaving a comment and I will be able to quickly get that information to you.







May 13, 2017
One Thing That Definitely Won’t Help Prevent Knee Replacement Surgery







Degenerative knee arthritis is not improved by undergoing elective knee arthroscopy. In fact the condition may be made worse as evidenced by an increased risk of future knee replacement surgery in those who have had the surgery compared with those who do not.
While this is not a new revelation, the evidence is now even more compeling. Data was analysized from 13 randomized control trials [the gold standard of reasearch types] by surgeons, physical therapists, clinicians and patients.
After considering the balance of benefits, harms and burdens of knee arthroscopy, as well as the quality of the evidence for each outcome, the 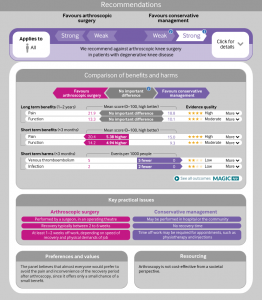 panel made a âstrong recommendation against arthroscopy.â
panel made a âstrong recommendation against arthroscopy.â
Arthroscopic Surgery wonât cure chronic knee pain, âlocking,â âclicking,â a torn meniscus, or other problems related to knee arthritis, according to a panel of international experts. âIt does more harm than good,â Dr. Reed Siemieniuk, chair of the guideline panel, told Reuters Health by email.
Every year, more than two million people with degenerative knee problems have arthroscopic surgery, in which a surgeon inserts a tiny camera into the knee and uses small instruments to try to fix whatâs wrong.
But guidelines published Wednesday in the British Medical Journal recommend against the procedure for just about everyone with knee arthritis. Read More
Just Say No If You Understand the Evidence
Dr. Siemieniuk, who works in the department of Health Research Methods, Evidence and Impact at McMaster University in Hamilton, Ontario, Canada even went so far as to say that âWe believe that no one or almost no one would want this surgery if they understand the evidence.â
Why undergo a surgery with the potential for blood clots and infection for less than a 15 % probability of a small or very small improvement in short term function with most of the positive effects lasting less than a year?
Final Take Home Point: If your goal is to prevent knee replacement surgery, you’ll be better off getting more serious about your weight loss program then having knee arthroscopy surgery for your degenerative knee arthritis. Stay out of the surgical suite and work on noninvasive methods of weight management and inflammation control. Â







May 7, 2017
It Wasn’t A Good Idea 20 Years Ago and It Still Isn’t







Let’s face it; you are being lied to by the medical establishment.
Recently a Spokane Newspaper ran a story about a 40-year-old mother who received bilateral knee replacements in glowing terms. There are two major errors being promoted in this article so let me take a few seconds of your time to correct these mischaracterizations.
Lie Number One
It’s really common now for younger people to get knee replacements so it’s no big deal
“Twenty years ago, the median age in the class was over 80,” said Payne, a registered nurse. “If you were 50, they wouldn’t even look at you. Now, it’s not uncommon to see younger people in the class,” she said.
 While it might be more common now, it is still very unwise. From the article you can learn that people younger than 65 represent the fastest growing group of patients and that this increase is not because that demographic is being targeted with marketing.
While it might be more common now, it is still very unwise. From the article you can learn that people younger than 65 represent the fastest growing group of patients and that this increase is not because that demographic is being targeted with marketing.
You are told that the majority of these patients have had previous athletic injuries and that some have had previous surgeries. Having arthroscopic surgery has been linked with an increased likelihood of eventually having knee replacement surgery, which should tell you something about the wisdom of seekng surgical interventions to your knee problem in the first place.
The story’s surgical hero shopped around until she found a someone who would perform the surgery on a 40 year old, so we know that there are still other surgeons with common sense who will not perform the surgery for those under 50. The other surgical hero had her replacement at 45 after being finally convinced by her husband to go ahead with the procedure.
Under the headline, ‘It was definitely worth it’ we read that “the life expectancy of artificial knees has increased”, and that our surgical superhero expects to get at least 20 years from her new knees.
According to the American Association of Hip and Knee Surgeons, “Most current data suggests that both hip and knee replacements have an annual failure rate between 0.5-1.0%. This means that if you have your total joint replaced today, you have a 90-95% chance that your joint will last 10 years, and a 80-85% that it will last 20 years.
That sounds great right? However that data has been compiled on a population of 60-80 year olds who are much more sedentary than the young surgical candidates being discussed in the article.
Lie Number Two
The rehabilitation is no big deal.
From the article’s sidebar more cheerleading can be found: “Ten years ago, people would spend at least three or four days in the hospital after a total knee replacement.
Advance s in care have cut a typical stay to one or two days, [mostly because of cost saving measures for the insurances/hospital not because it’s the best thing for the patient] said Dr. Jonathan Linthicum, co-medical director of Kootenal Health’s total joint replacement unit. In some cases, patients are cleared to leave the hospital within 23 hours. [This isn’t the hard part because early pain relief is generally quite good. It’s switching over to oral formulations that can be difficult.]
s in care have cut a typical stay to one or two days, [mostly because of cost saving measures for the insurances/hospital not because it’s the best thing for the patient] said Dr. Jonathan Linthicum, co-medical director of Kootenal Health’s total joint replacement unit. In some cases, patients are cleared to leave the hospital within 23 hours. [This isn’t the hard part because early pain relief is generally quite good. It’s switching over to oral formulations that can be difficult.]
Better pain control [There is no magic bullet pain control method and most being used have been around for a while] allows patients to stand on their new knee joint the day of surgery, which reduces the risk of blood clots, Linthicum said. [We have been standing patients the day of surgery to prevent blood clots for a long time.]
Post- surgery recovery takes three to five weeks, but it varies by patient. [This is a very rose colored view and in fact our surgical hero had her second knee replacement surgery March 1 and according to the article is still ” moving carefully” about 9 weeks later.]
“Some people come walking in at two weeks and say, ‘Thanks Doc. That was great, ‘Linthicum said. “Others are still getting their range of motion back at six to eight weeks.”
Don’t be fooled, this puff piece could have been written by the marketing department of the hospital and would be more appropriate on the hospital’s website than a newspaper. There is no critical reporting at all.
If you or someone you know has been told that you are a candidate for knee surgery, don’t just blindly trust they have your best interests at heart.
Consider the following scenarios:
You have the replacement at 40 years old and need to have a revision within 5 years because of an implant failure. At 50 you need a third surgery because your activity levels were much higher than a 70 year old. Will you be a candidate for a 4th surgery at 70 and how well would it take? Will you have any bone left?
Knee replacement surgeries soar to over 3 million a year in 2030 as projected but the government no longer has the money to perform them at that volume and so you are required to fork out a 50% co-pay for your revision or even worse are denied surgery.










