Leslie Glass's Blog, page 312
December 13, 2018
5 Characteristics of Healthy Families
We so often read about dysfunctional families that we may believe that there is no such thing as healthy families. But healthy families aren’t a myth – they really do exist. Your family may be one of them, but if not, you can learn how to help your family go from unhealthy to healthy. Also realize that most families have some healthy and some unhealthy traits – no family is perfect. And we really don’t want a perfect family for if the family has never suffered from any imperfections, it will be hard for children to adjust to an imperfect world. So take heart – your mistakes can be beneficial!
Healthy Families Have These Characteristics
1. Open, Honest And Respectful Communication
For a family to communicate at the highest level, it needs to be open and honest in the talks, family members need to be respectful of each other, and listening (not just hearing) to what is being said are basic skills. This needs to take place in any communication and family meetings can be an excellent way of addressing more significant issues. Everyone must have a voice in the conversation, even the family cat!
2. Acceptance of Each Other
Healthy families accept each other as individuals and as part of the family system. This acceptance indicates that the family will abide by you throughout good and bad times. While behavior may not be accepted (i.e., such as drinking and drugging) the person is always accepted. This leads to #3.
3. Love And Compassion
Each person needs to validate each other through love and compassion no matter what the trial or tribulation. As above, the behavior may not be accepted, but the love is always there (even when we want to throttle someone).
4. Collaboration And Involvement
Families that work together and play together are healthier than those who don’t. This involvement is significant for bonding both on an individual level and on the family level. Eating meals together, being involved in the kids’ school and after-school events, taking the children to work to show them what the jobs are like, having friends visit, visiting with other relatives, and doing leisure activities such playing Pokemon Go, taking walks together, or playing board games are invaluable for healthy living.
5. Healthy Coping Skills
Because life is not always easy or simple, a family has both individual and family coping skills to use when dealing with the difficult times. These coping skills can be in these 5 areas:
Physical: taking care of the basics such as healthy meals, enough sleep, exercise, and hygiene, and basic safety;
Emotional: being able to feel feelings and talk about them with the family, journal, cry or laugh, talk to a teacher or counselor at school, go for family therapy, write/draw/dance/sing and participate in other creative emotional outlets, jog/walk/exercise out the feelings;
Intellectual: read, write, have deep discussions with family members or others, study, learn, teach; do puzzles or healthy video games, do creative activities;
Social/relational: having time with family and others together while also having alone time for we need to also have a relationship with self such as reading, meditating, writing, or doing yoga or tai chi;
Spiritual: having a sense of communion with a higher essence, being with others including the family, taking walks in nature, having fun, being creative, going to a religious ceremony or spiritual event, reading religious/spiritual books, meditating, prayer, being alone.
All of these are healthy family characteristics. Look back over these. You may find your family in the middle. Look over them again. You may find new ideas for a healthier family.
The post 5 Characteristics of Healthy Families appeared first on Reach Out Recovery.
December 12, 2018
8 Ways to Bounce Back After Disappointment
From Health:
Sad but true: bad stuff happens to all of us. Relationships turn toxic and die, trips to the HR department end in pinks slips and tears, loved ones become ill.
It hurts. It sucks. And a lot of times, it’s unfair. You’d like to think that you’re the kind of person who can suck it up and instantly recover, but the fact is, everyone reacts differently to disappointment and pain. Let it go may make for an inspiring (if irritatingly omnipresent) song lyric, but let’s face it: landing on your feet and moving on is a lot easier said than done.
But here’s the thing: While none of us is totally in control of what happens in life, we can control how we react to heinous situations. In honor of National Get Over It Day (yes, that’s a thing), we asked experts for their best strategies for moving on and bouncing back.
Follow these tricks and you’ll not only be able to rebound from disappointments you’ll actually end up a better, smarter, stronger person than before. (Admit it, you’re intrigued, right?)
Throw a (small) pity party
Want to have a good sob? Go medieval on a container of Ben & Jerry’s? By all means, do it. Unless you let yourself feel pain, you can’t heal properly, says Karen Salmansohn, the best-selling author of The Bounce Back Book ($11, amazon.com), who uses a personal story to illustrate her point: While vacationing in Greece a few years ago, I had an accident, in which I basically got squished underneath my moped. I was embarrassed, so even though I was hurt, I put up a brave front, insisting to my friends, I’m OK, I’m OK. Well, my elbow ended up healing badly and to this day I have trouble with my arm. Crashing in a relationship, or in another aspect of your life, is like that, says Salmansohn: When you insist that you’re fine and don’t take time to acknowledge the pain (or grieve, for that matter), you don’t heal properly. Let yourself mourn.
Kelly McGonigal, PhD, author of the upcoming book, The Upside of Stress ($20, amazon.com), puts it this way: Giving yourself permission to grieve about disappointment is how you move on. In fact, she says, research shows that the more upset you are after some kind of loss or adversity, the more likely you are to experience personal growth as a result. Feeling bad is often a catalyst for making positive change, she says. If you try to suppress your feelings and skip the feeling bad part, you’re less likely to learn and grow from the experience.
Pretend you’re Serena Williams
Think of any transition as a kind of major sporting event, says McGonigal. Life is asking a lot of you, so take care of yourself in the same way that an athlete would prepare for an important competition, she says. Think of it as self-care, rather than self-indulgence. By that I mean it should create health, help you sustain energy, or provide a true rest. Salmansohn opts for the second, tapping into the mind-body connection by reaching for the dumbbells. It makes me feel empowered I’m like, Oh yeah! she says. There are studies that show when you’re physically strong, you’re emotionally strong.
Create a distraction
One of the reasons we feel so upset when life throws us for a loop is because we feel out of control. Distractions help you re-gain some of that control, says Salmansohn. Choose something that you’re good at a signature strength or passion, she says then put it on your calendar and do it. The more stuff that you can write down on your to-do list and cross off, the more you’ll feel in control, says Salmansohn. Think of it as a stop-and-swap: Well, I couldn’t control that, but I can control this. You were the person who got dumped or got fired; now you’re the woman who’s a killer tennis player or someone who has the coolest Pinterest page in the world. You’ve got stuff going on! The point here is to remind yourself that there are other aspects to you as a person.
Some of the best distractions, McGonigal says, are the ones that involve doing something positive and constructive (in other words, nix the Netflix binge). Volunteer at a local charity, train for a 5K, even clean out your closet, she suggests. Basically, anything that involves moving energy in a positive direction.
Pick up the phone
Usually when we’re going through a tough time or trauma, we tend to pull inward and push people away. Bad move. You have to get yourself off that merry-go-round of not-so-merry thoughts, says Salmansohn. When we’re by ourselves, we tend to wallow and obsess. But studies show that people who seek out the comfort and safety of friends are the ones who recover fastest. Love does heal, so be around the people who love and support you. There’s another good reason for reaching out, according to Gail Saltz, MD, Health’s contributing psychology editor: Friends can help you recover by offering suggestions and advice that you may not have considered. And while you’re at it, call home, OK? Scientists at the University of Wisconsin at Madison found that when women hear their mother’s voice, it can reduce their stress hormones, producing an effect similar to a hug.
Reframe your identity
Don’t let a bad situation define you. Boost your self-esteem by changing your identity and getting out of that victim mindset: “Think of yourself as a victor, not a victim,†says Salmansohn. “Reassure yourself that whatever happens, you are the type of person who can get through it. Make it a point to say a mantra of positive not pitiful words whenever a defeatist attitude starts to creep in: I’m going to be OK. I’m strong. I have it within me to get through this and get to where I need to be. Another trick to get you in a positive frame of mind: Realize that life is full of curve balls, Dr. Saltz says. Look back and recall how you handled every one of them. What you’ll realize: You got through them, and you can get through this.
Cut yourself a break
Repair your ego by taking time for a personal and compassionate pep talk. Focus on what’s universal about your situation, says McGonigal. Everyone makes mistakes. Everyone experiences rejection. Everyone knows what it’s like to try and fail. All that your experience says is that you are human not that your life is uniquely screwed up. And stop projecting blame inward, Dr. Saltz says: as self-referential to think that the fault lies solely with you and not the other person. For example, maybe your relationship failed because your former partner was a commitment-phobe. You need to spot what someone else has brought or not brought to the situation.
Use the hurt
Think of it as a kind of emotional adrenaline to make some changes in your life. A lot of people are afraid of change or anything new and unfamiliar, says Salmansohn. But when you’re going through a crisis, suddenly the new and unfamiliar doesn’t look as scary as the place you’re in, so you’re more open to change. Remember, the story of your life is a lot bigger than one single moment, so imagine this moment as a turning point in the story that will propel you to something bigger and better, McGonigal says.
Re-write the story
OK, it may sound a little hokey, but it happens to be true: As awful as your situation may be, there’s something positive that can come out of it. McGonigal believes that there’s always an upside to change because it gives you an opportunity to make an intentional choice about what you want in life and who you want to be or become. Without major disruptions in our lives, it’s easy to never really reflect on those things.” Or, as Salmansohn says: Ultimately, it’s all about adopting a student mentality and searching for the good lessons. Happiness isn’t about what happens to you; it’s how you respond to what happens to you. Tell your story as a sad one and it will be a sad story; tell it as a happy one and it will be a happy story with a happy ending.
The post 8 Ways to Bounce Back After Disappointment appeared first on Reach Out Recovery.
Overdose Deaths Involving Fentanyl Doubled Every Year From 2013 to 2016
From Time:
Drug overdose deaths involving the potent synthetic opioid fentanyl are on the rise, and the number of fentanyl-related deaths roughly doubled each year from 2013 through 2016, according to new federal data.
Researchers from the Centers for Disease Control and Prevention’s (CDC) National Center for Health Statistics (NCHS) reviewed death certificates filed from 2011 to 2016 to find out which drugs were mentioned most frequently each year. During this time period, drug overdose deaths increased from 41,340 in 2011 to 63,632 in 2016.
Just as striking as the overall uptick, however, was the sharp increase in deaths involving fentanyl.
Fentanyl was mentioned in about 1,600 U.S. death certificates in both 2011 and 2012, according to the NCHS’ review. In 2013, that number rose slightly to 1,919. But by 2014, it had roughly doubled to 4,223 — a trend that continued in 2015 (8,251) and 2016 (18,335).
By 2016, fentanyl was involved in about 29% of all fatal drug overdoses and had overtaken heroin — which was the most commonly cited drug in the death certificates of people who had died from overdoses from 2012-2015 — as the substance most frequently involved in drug deaths. Cocaine ranked second or third in each year included in the study, and the prescription opioid oxycodone was the leading drug in 2011. Many fatalities also involved multiple drugs, the report says.
While the new study left off at 2016, recent CDC data showed that the rate of drug overdoses involving fentanyl and other synthetic opioids increased by 45% between 2016 and 2017 — evidence that these potent narcotics are not going away. Fentanyl and other synthetic opioids were involved in nearly 30,000 overdoses last year, out of a total of about 70,000, according to federal estimates.
Fentanyl is involved in so many overdoses because of its high potency; it is 80 to 100 times stronger than morphine, and even a small amount can be lethal. Drugs such as heroin and cocaine are increasingly being laced with fentanyl and other synthetic opioids, causing many drug users to consume fatal doses by mistake.
Lawmakers and public health officials have made it a priority to reduce both supply of and demand for synthetic drugs like fentanyl. Most recently, China — which is believed to be the primary source of U.S. fentanyl — pledged to classify fentanyl and all of its chemically similar analogs as controlled substances, which would in theory stem their flow into the U.S. Whether the policy actually results in fewer overdose deaths, however, remains to be seen.
The post Overdose Deaths Involving Fentanyl Doubled Every Year From 2013 to 2016 appeared first on Reach Out Recovery.
December 11, 2018
What Your Heart Needs Now
From Health:
The statistics are sobering: Heart disease is the number-one killer of women in the United States. And an estimated 8 million women have it. What’s more, a new study shows that in recent years the overall heart disease risk for Americans—especially women—hasnt continued the healthy downward trend it showed in previous decades. Ready for some good news? You can do more to prevent heart disease than almost any other serious condition. Start with these age-specific steps.
The 30’s
Declare a trans fat–free zone.
Commonly used to extend the shelf life of packaged foods like cookies and crackers, and also found in margarine, trans fats pack a double whammy: They raise bad cholesterol (LDL) while lowering good, protective HDL (your LDL should be below 100; your HDL, above 60). In a Harvard University study, women with the highest level of trans fats in their blood had triple the risk of heart disease. Take a cue from major U.S. cities like New York and Philadelphia (which have banned trans fats from restaurants), and pitch them out of your pantry.
On ingredient lists, they show up as “hydrogenated” and “partially hydrogenated” oils. But scrutinize any product touted as “trans fat–free” at the supermarket, too: Some manufacturers have replaced hydrogenated oils with tropical oils that are high in saturated fat, which also raises LDL cholesterol. Eating out in a city where trans fats aren’t banned? Skip the fried stuff—many restaurants still use the oils for frying.
The 30’s
Use your OB-GYN as a partner.
During your prime reproductive years, you may visit your OB-GYN more than you go to your regular doctor. Make sure you talk to her about your heart as well as gynecological health, particularly because blood pressure (BP) can rise if you’re taking birth control pills or when you’re pregnant.
Women who develop preeclampsia (pregnancy-related hypertension) are prone to heart disease later in life. And, in general, “how your heart handles pregnancy offers a snapshot of how it will look in middle age,” says Sharonne Hayes, MD, director of the Women’s Heart Clinic at the Mayo Clinic in Rochester, Minnesota. To keep BP from creeping up (the safe zone is lower than 120 over 80), substitute herbs and spices for salt—try cumin for a healthy twist on popcorn, for instance. Too much salt causes blood vessels to retain water, which can lead to high BP.
The 30’s
Simmer down.
If you boil over when the shopper in front of you has 16 grocery items in the 15-or-fewer lane, beware: Losing your temper can damage your arteries, according to research by C. Noel Bairey Merz, MD, director of the Women’s Heart Center and endowed chair in Women’s Health at the Cedars-Sinai Heart Institute in Los Angeles. “Raging causes your blood pressure to surge and stay up there,” Dr. Merz says. That’s why it’s crucial to get a grip on anger at an early age before it takes a toll. Learn now that, instead of venting when a situation makes you furious, you can take a few deep breaths and describe to yourself what’s making you angry. That should help you calm down.
The 40’s
Don’t skimp on sleep.
When your hormones are fluctuating madly, it can be tough to nod off. Its
no wonder, then, that more than half of women in their 40s suffer from insomnia at least a few nights a week. That’s nothing to yawn about, either. When your body is deprived of restorative sleep, your heart has to work harder. And piles of studies show that too little shut-eye can lead to heart attack, stroke, heart failure, and diabetes. How little is too little? A recent study in the Archives of Internal Medicine suggests that less than seven-and-a-half hours per night puts you at risk for heart disease. And recent research from Duke University found that women who take more than a half-hour to fall asleep or those who awaken frequently during the night have inflammation in their arteries and higher levels of insulin, two major risk factors for heart disease.
The soporific Rx: Do your best to unwind with a relaxing bedtime routine, like listening to soothing music or a soaking in a tub with bath salts. And despite how difficult it might sound, obey this rule—no technology or work in the bedroom; your bed should be for sleep and sex only.
The 40’s
Monitor your mood.
Between the demands of work and family, it’s easy to worry that something will fall through the cracks—but don’t let that something be your own peace of mind. Perimenopausal women have nearly double the risk for depression, and that spells trouble for their hearts, says Jennifer Mieres, MD, a cardiologist and associate professor at New York University’s School of Medicine. Uncontrolled stress can raise blood pressure and flood blood vessels with inflammatory chemicals, which in high doses can be toxic to the heart, while depression has been linked to hardening of the arteries. Then there are the unhealthy habits that come with stress and the blues: smoking, excessive drinking, and overeating.
Smart medicine for your mood and your heart? Exercise. Thirty minutes of aerobic activity (walking, biking, swimming) most days of the week has been shown to reduce the symptoms of depression by about half, an effect comparable to antidepressant use while lowering blood pressure and strengthening your cardiovascular system. But if you’re feeling low more often than not, talk to your doctor about therapy, antidepressants, or St. Johns Wort. (New research suggests that this herb works as well as antidepressants and has few side effects.)
The 40’s
Get more fish, flaxseed, and fiber.
In your 40s, as estrogen dips, your blood pressure, cholesterol, and triglycerides (a type of fat stored in the blood) start creeping up, making a heart-healthy menu more important than ever. Aim for two servings of fish, like salmon or tuna, each week for omega-3 fats; or pick omega-3-fortified foods like orange juice, margarine, and eggs. Also, sprinkle ground flaxseed on yogurt or cottage cheese to lower cholesterol. And experiment with dishes that contain high-fiber foods like apples, broccoli, beans, and bran cereal. Health fads come and go, but a high-fiber diet has consistently proven to be good for the heart, says Leslie Cho, MD, director of the Women’s Cardiovascular Center at the Cleveland Clinic in Ohio.
The 50’s Plus
Whittle your waist.
If a few extra pounds have settled around your middle since menopause,
you’re not alone. “Basically, we start putting on weight more like men,” says Nieca Goldberg, MD, medical director of New York University’s Women’s Heart Program and author of Complete Guide to Women’s Health. The “meno potbelly” is especially hard on the heart because it builds up around internal organs, triggers inflammation, and leads to insulin resistance.
Research from the famous Nurses Health Study found that women with a waist circumference of more than 35 inches were twice as likely to die of heart disease than women with a 28-inch waist, regardless of weight. Low-intensity workout routines can help slow down the belly buildup, but to shrink it you’ll need to work up a sweat with 60 minutes of moderate-intensity aerobic exercise at least three times a week. Try jogging, walking on the treadmill on a challenging incline, or swimming laps.
The 50’s Plus
Stay strong.
Since hormone replacement therapy (HRT) is no longer thought to protect your heart, and may even harm it (talk to your doctor about the risks if you decide to try it), you need to safeguard your heart with strong muscles. Add strength training—like a weight-lifting class, yoga, or Pilates—to your exercise routine at least twice a week, Dr. Goldberg recommends. Youll keep blood pressure in check, boost metabolism, zap more calories, control cholesterol, and improve endurance. Sum total? A heart thatll keep pumping happily for years to come.
Enjoy some “friend benefits.”
Whatever causes you stress, leaning on friends for support and commiseration can help keep blood pressure in check. “There are clearly good things that happen to your heart when you care about people and people care about you,” Cedars-Sinai’s Dr. Merz says. Talk out the stress with friends over a walk or at the gym, and you’ll double your heart benefit.
The post What Your Heart Needs Now appeared first on Reach Out Recovery.
Opioid Crackdown An Ethical Issue For Doctors
Doctors are opting to stop prescribing legal opioids – even to people who are left bedridden without them — as insurers, pharmacies, state medical boards and state and federal law enforcement authorities warn them about overstepping federal opioid prescribing guidelines (issued in 2016 by the Centers for Disease Control) and the regulatory or third-party limits that followed on the number of pills and daily dosage they can give patients. Some have stopped prescribing opioids after being faced with losing their medical license or getting arrested.
As federal and state agencies respond to the staggering rate of drug overdose deaths — primarily involving illegal opioids like heroin and illicit fentanyl — doctors who maintain they are responsibly prescribing opioids are getting caught up in the crackdown. This is their side of the story to the opioid crisis and how it has impacted — and for some ruined — their lives.
This is the second of a three-part series on the nation’s struggle to address its crippling opioid crisis, and the unintended victims left in its wake. Read Part 1 here: As doctors taper or end opioid prescriptions, many patients driven to despair, suicide.
Dr. Stephen Nadeau received a warning from the Gainesville, Fla., hospital where he worked.
Their policy on prescribing opioids was changing, to go beyond federal guidelines aimed at the national overdose crisis that has claimed hundreds of thousands of lives.
The hospital would stop treating pain with opioids. And every doctor, including Nadeau, had to stop prescribing them. Doctors otherwise risked losing hospital admitting privileges – and perhaps even their medical license.
In Helena, Mont., Dr. Mark Ibsen was feeling heat from the state medical board – and the U.S. Drug Enforcement Administration (DEA), for the high-dose opioids he was prescribing to patients in severe, chronic pain. An allegation made by what he described as a disgruntled employee charged Ibsen was overprescribing.
As a result, the state medical board suspended his license. The DEA visited five times, Ibsen said, suggesting he was risking his livelihood and could end up in jail if he kept prescribing.
Both doctors complied and stopped prescribing, affecting roughly 230 of their patients. Tragically, among those were several who committed suicide, the doctors said, when they couldn’t find another health care provider to relieve the pain.
That’s a scenario playing out across the country, as government agencies respond to the staggering rate of drug overdose deaths, involving primarily illegal opioids like heroin and illicit fentanyl. Doctors who maintain they are responsibly prescribing opioids are getting caught up in the crackdown, according to dozens of medical care providers interviewed by Fox News, leaving little room to both play by the rules and properly treat huge numbers of patients who legitimately suffer chronic and intense pain.
Some doctors like Ibsen and Nadeau are opting to simply stop prescribing legal opioids, as insurers, pharmacies, and authorities warn them about overstepping guidelines issued in 2016 by the Centers for Disease Control and Prevention (CDC).
Meanwhile, other doctors, nurses and medical associations accuse the federal government of interfering in the physician-patient relationship, and pursuing simplistic, politically expedient solutions that put tens of millions of Americans at risk.
“Not only is the government legislating the way we care for chronic pain patients,” said Nadeau, a professor of neurology at the University of Florida College of Medicine, “they are substantially taking away our ability to do it.”
CDC GUIDELINES CONTROVERSY
Critics of the way the 2016 guidelines have been applied note they were not intended as law, but as a means to advise primary care physicians. The CDC specifically cautioned against abruptly stopping or forcibly tapering opioid treatment for patients already taking them, because of the danger of withdrawals, or debilitation.
More than 300 health care professionals, including former drug czars in the Clinton, Nixon and Obama administrations, have signed an as-yet unpublished public letter to the CDC, warning of a brewing crisis among pain patients, despite the “laudable goals” of the guidelines.
“Within a year of (CDC) Guideline publication, there was evidence of widespread misapplication of some of the Guideline recommendations,” said the letter, written by three doctors and a pharmacist. “Soon, clinicians prescribing higher doses, pharmacists dispensing them, and patients taking them came under suspicion.”
“Patients with chronic pain, who are stable and, arguably, benefiting from long-term opioids, face draconian and often rapid involuntary dose reductions,” the letter continued. “Often, alternative pain care options are not offered, not covered by insurers, or not accessible … Consequently, patients have endured not only unnecessary suffering, but some have turned to suicide or illicit substance use. Others have experienced preventable hospitalizations or medical deterioration.”
Others argue many authorities have misunderstood, or outright ignored, the CDC’s disclaimer. Health care providers who don’t drop opiate painkillers are setting strict limits on dosage limits, even for chronic pain sufferers who require more medicine because of serious conditions, or the way they hyper-metabolize opioids. Many who do so cite the CDC guidelines, saying they were told to follow them — or took them up as a kind of pre-emptive strike.
Not only is the government legislating the way we care for chronic pain patients, they are substantially taking away our ability to do it.
— Dr. Steve Nadeau, a professor of neurology at the University of Florida College of Medicine
Dozens of pain patients have told Fox News they were dropped or forcibly tapered down by doctors who long treated them quite successfully, but who became fearful about losing their license after being formally admonished, or hearing about other doctors who ran afoul of the government.
Meredith Lawrence, who lived in Tennessee with her husband, Jay, while he suffered decades of pain following a tractor-trailer accident, recalled the helplessness she felt watching him suffer, while his dosage of opioids was being sharply reduced.
Lawrence said the doctor who had treated him successfully for years was very clear about his decision to taper down the dosage.
“He said ‘My patients’ quality of life is not worth risking my practice or my license over,'” she told Fox News. “I’ll never forget that.”
“Jay felt like they gave up on him,” she said, recalling what finally prompted her husband to kill himself. “That was the day Jay gave up. He felt the doctor gave up – and he gave up.”
Dr. Stephen Nadeau
DEA TARGETING ‘WORST OF THE WORST’
Much of the opioid overdose epidemic in recent years stems from illegal drugs, not legitimate prescriptions. But more than a decade of overprescribing – out of ignorance for some, and for others the chance to rake in big profits – played a significant part, according to federal authorities and others who have studied the issue.
Assured by what some charged were deliberately deceptive pharmaceutical companies insisting opioids weren’t very addictive, some health care providers prescribed liberally, even for minor procedures such as a pulled tooth, or non-serious orthopedic injuries. Overprescribing led to greater daily dosages or easy-to-get refills – more than were needed. That, along with the theft and resale of opioids from people who had prescriptions, laid the groundwork for the crisis.
Most prescribers say they recognize many health providers were not prudent enough when prescribing opioids. And many doctors noted they were previously criticized for undertreating pain. Medical schools devoted little time to the study of pain and to opioids, they also say.
“Physicians and particularly medical school residency programs should have been taking more responsibility. Pain is the most common condition, and it’s one of the most difficult to treat,” said Nadeau. “And there [have been] pill mills that have relied on physicians to prescribe and many have done so very irresponsibly. But I think many are compassionate physicians … it’s a reflection of the inadequacy of their training that they basically had to learn the ropes on their own.”
John Martin, the DEA’s Administrator of the Diversion Control Division, said an overwhelming percentage of prescribers followed the rules. Of 1.6 million registrants, he said, less than one percent “operate outside the law.”
But there are still unscrupulous prescribers.
“Remember, with the opioid epidemic, just one practitioner that’s operating outside the law can really have a lot of serious consequences. In a small community, it can wreak havoc,” Martin said. “They’re really going after the worst of the worst of the criminal violators.”
Martin said most prescribers have nothing to worry about.
“Doctors are writing less prescriptions. And that goes down to education with the CDC guidelines,” he said. “There’s a new and different way of looking at using opioids for chronic pain.”
But that’s not what prescribers and patients see.
“Doctors around the country are terrified because of what happened to me and other doctors,” Ibsen said. “We don’t arrest car dealers if someone drives a car and gets into a fatal accident.”
“Standards of care are being decided by a jury of people without medical training,” Ibsen added. “It’s a very bad situation. We’re playing Whack-a-mole with the wrong mallet.”
Remember, with the opioid epidemic, just one practitioner that’s operating outside the law can really have a lot of serious consequences. In a small community, it can wreak havoc…[the DEA agents] are really going after the worst of the worst of the criminal violators.
— John Martin, DEA Administrator of the Diversion Control Division
THE CHALLENGE OF PAIN MANAGEMENT
For many medical professionals, treating pain patients has become a thankless task. The stakes are too high, they say, as even those who try to responsibly manage opioid treatment for their sickest pain patients find themselves hounded by authorities or pharmacists.
Many doctors say they view opioids as a last resort. They are very strong medicines, which often come with strong side effects, ranging from constipation, nausea, liver damage and respiratory problems. Many pain patients said in interviews they were reluctant to take them initially, and eventually did only after other treatments and surgeries failed.
“If we had a good alternative to opioids, every physician would be at the front line of it to prescribe that,” said Dr. Lynn Webster, vice president of PRA Health Sciences, and the past president of the American Academy of Pain Medicine.
In a recent survey by the North Carolina Medical Board of its licensees, 43 percent of 2,661 respondents said they had stopped prescribing opioids. They attributed their decision to concern about getting into trouble.
Patients complained to the board doctors had cut them off, pointing to the CDC guidelines or an initiative by the board aimed at cracking down on health care providers who prescribed high doses of opioids, or who had two or more patients die of overdoses in a year.
And of 3,000 doctors responding to a recent nationwide survey by the SERMO physician network for BuzzFeed News, 70 percent said they had dramatically cut down or altogether stopped prescribing opioids. The main reasons were “too many hassles and risks involved,” “improved understanding of the risks of opioids,” and fear of “getting into trouble,” according to BuzzFeed.
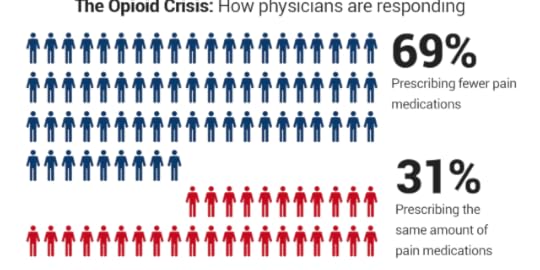
Yet another survey, commissioned by The Physicians Foundation, showed about 70 percent of nearly 9,000 physicians nationwide were prescribing fewer opioids.
In Nevada, where so many doctors stopped taking pain patients after the state implemented strict opioid prescription rules – which increased required record-keeping – physicians like Dan Laird now have a six-month waiting list.
“We turn patients away every day,” said Laird, who last year could fit in patients soon after they called for an appointment. “It’s heartbreaking, but many can’t find doctors.”
Many pain patients told Fox News that after being forcibly tapered down or abandoned by their pain doctors, they have lost much of their ability to function. Many said they have made suicide plans.
“I have heard from — either through email or posts on my blogs — about 1,000 people over past two years who have been denied pain medicine or forced to dramatically reduce their dose who have expressed a desire to die or commit suicide,” Webster said.
Kate Nicholson, a former federal prosecutor who credits her opioid treatment with allowing her to function after years of being bedridden, said: “We’re looking only at the supply, and cutting off people who are not abusing the medication. It made all the difference in the world, I couldn’t sit or stand or walk because of nerve damage. I went from being bed-ridden and completely non-functional to doing my work as a prosecutor.”

Dr. Mark Ibsen
WARNINGS, RAIDS AND ARRESTS
Health care providers who prescribe opioids, particularly to high-impact chronic pain patients, are finding themselves on the radar of any number of sources – pharmacists, state medical boards, insurers, and law enforcement.
In a speech about the national overdose deaths epidemic in March, President Trump said: “Whether you are a dealer or doctor or trafficker or a manufacturer, if you break the law and illegally peddle these deadly poisons, we will find you, we will arrest you, and we will hold you accountable.”
But the red line triggering disciplinary action often is inconsistent, and murky. The CDC considers an opioid’s benefits to outweigh risks if it improves pain and function by at least 30 percent. But, doctors say, those factors rarely are considered when authorities scrutinize prescribing patterns.
More often, it’s large amounts of opioids and high doses – statistics on a spreadsheet or chart, without the context of a patient’s medical condition — that can bring disciplinary action.
On Nov. 2, Dr. J. Julian Grove posted to Twitter a letter his Phoenix office had received from Walgreens. Grove said he wanted to provide chronic pain patients “an insight to the veiled threats” that health care providers treating pain are getting these days.
The letter said: “Walgreens has determined that you may have issued prescriptions for opioids that exceed the CDC guidelines.”
It said Walgreens had the right to refuse to fill a prescription that falls outside the guidelines, and added: “Walgreens pharmacists may notify appropriate regulatory agencies when prescriptions are refused.”
Grove blasted the letter.
“I am a double board-certified anesthesiologist and pain specialist, treating complex pain and cancer pain always w/comprehensive approach,” he said. “Insulting.”
View image on Twitter
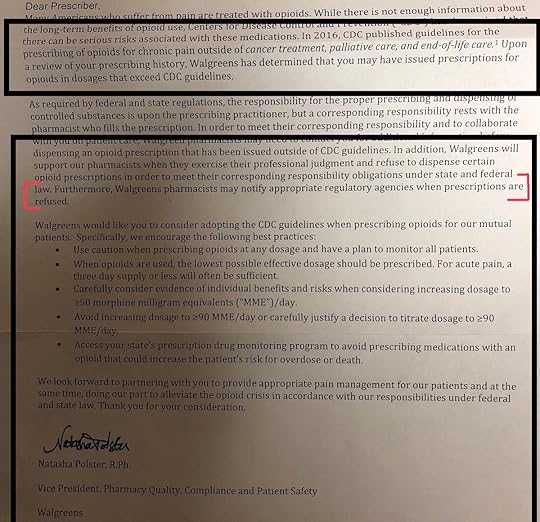
J. Julian Grove@JulianGroveMDChronic Pain Patients: An insight to the veiled threats HCP receive treating pain. From #walgreens on this example to my PA. I am a double board certified Anesthesiologist and Pain Specialist, treating complex pain and cancer pain always w/comprehensive approach. Insulting.
Asked about Walgreen’s pressure on prescribers to follow the CDC guidelines, company spokesman Phil Caruso told Fox News in a statement: “As a key patient touchpoint in the nation’s healthcare delivery system, we regularly communicate with prescribers to help ensure the safe and effective dispensing of medications in the best interest of our customers … Fighting the opioid epidemic requires all parties, including leaders in the community, physicians, pharmaceutical manufacturers, distributors, pharmacies, insurance companies, PBMs (pharmacy benefit managers) and regulators to play a role and coordinate efforts.”
The U.S. Attorney’s Office in Atlanta announced in October that some 30 doctors were put on notice there for prescribing opioids in larger quantities and higher doses than others. Prosecutors enclosed the CDC guidelines with the warning letters.
U.S. Attorney B. Jay Pak called those doctors “outliers,” adding the warning letters were meant to point out “atypical practices.” Significantly, Pak said the doctors may not have done anything wrong.
“It is our plan to strategically reduce the impact of this crisis within our community by notifying outlier prescribers that their opioid prescribing habits are not in conformity with accepted standards, or the prescribing habits of their peers,” the agency said in a statement. “Through this initiative and others, it is the goal of the Department of Justice to reduce opioid prescriptions by one-third over the next three years.”
Prescribers particularly dread getting in the crosshairs of the DEA, which can revoke permission to manufacture, distribute and dispense controlled substances. The agency opens about 1,500 new opioid cases per year and makes more than 2,000 arrests. The arrests include DEA registrants, doctor-shopping patients, and prescription forgery rings.

Martin, the DEA administrator, said that actions against prescribers are not undertaken arbitrarily.
“When we are investigating something like a doctor that may be overprescribing, you know because we’re not doctors, in the course of our investigation we are going to solicit medical experts,” Martin said. “We’ll try to get what’s called prescription drug monitoring program information and that’s information that the states have at their level that shows how many prescriptions are being written by a doctor for a patient and being filled at a certain pharmacy.”
“So we’ll try to look at that stuff and then maybe go out to that pharmacy and do an inspection and look at their records and just see if there’s anything more there and then we’ll follow up with that,” he said.
Roughly 800 prescribers each year surrender their DEA registration – a kind of license – when the agency opens an investigation. DEA investigations can involve having assets and medical records seized. In some cases that can lead to bankruptcy, doctors said, prompting many to surrender their opioid prescribing rights, rather than fight a battle against a behemoth government.
Ibsen was an emergency room doctor in Montana when he became – as he puts it, an “accidental pain doctor,” taking “pain refugees” whose doctors had been arrested. Many patients were very ill and suffered severe chronic pain, said Ibsen, who added he was able to wean many patients down to lower doses.
Ibsen said he became a target of the state board of medical examiners after an employee he fired filed a complaint, saying he over-prescribed. His license was suspended but eventually reinstated – after four years. But he decided to stop prescribing opioids after five visits from the DEA.
“They were very vague,” he said of the DEA agents. “They said ‘You’re risking your freedom by prescribing to patients like these.’ I said ‘Patients like what?’ They said, ‘Patients who might sell the pills.’”
“Doctors are taking plea deals because they don’t want to go to prison,” said Ibsen, who was not charged. “Once they arrest a doctor, they seize all their medical records. A doctor can’t make any more income. They seize your assets, and can’t afford an attorney.”
Ibsen referred patients to a prominent pain doctor in California, Dr. Forrest Tennant, who became known for taking people cut off by other doctors. Tennant for years had been researching non-opioid alternatives.
Then the DEA raided Tennant’s office. The agency never charged him, but he, too, gave up prescribing opioids.
“It’s immoral and unsafe to forcibly taper down or abandon a patient,” said Tennant, whose patients included those with terminal illnesses. “Some doctors don’t give these patients any withdrawal medication. Who is the worst offender, then? The CDC, the DEA, the U.S. attorneys who are shutting down doctors, or the doctors who abandon patients?”
One Tennant patient, Jennifer Adams, a former Montana police officer who had been treated by Ibsen, died from a self-inflicted gunshot in April, after the California doctor’s office was raided by the DEA.
Tennant said he respects the idea “the DEA has a right and responsibility to investigate.”
“But since I used high doses, they said my patients were going to overdose and die,” Tennant said. “I’ve been practicing a long time, I’ve not had a single overdose. I’ve given patients thousands of opioid equivalents. I know how patients should be monitored.”
Dr. Lesly Pompy was one of a few pain physicians in a rural part of Michigan, serving as many as 1,500, the majority of them referrals from other doctors who could not treat their chronic conditions. A pain specialist since 1995, he kept long hours, sometimes going to hospital emergency rooms when he was summoned to help a patient in severe pain. Sometimes he would try nerve blocks, many other times opioids.
On Sept. 26, 2016, roughly 25 law enforcement officers raised Pompy’s office at the ProMedica Monroe Regional Hospital.
“There were DEA agents, county and local police, they had everybody in my waiting room and who worked in my office put their hands up. Children were crying. There was a helicopter over the building. It was like a scene from a Jason Bourne movie,” he said.
Pompy was charged with unlawful distribution of prescription drugs and health care fraud from 2012 to 2016. A federal jury indicted him this summer on 37 counts. The indictment maintained Pompy illegally prescribed some 10 million dosage units of controlled substances that fell outside the realm of standard practice. He was also accused of inappropriately filing claims to insurers.
Pompy denies the charges and claims that because he prescribed large quantities of opioids, some to severe pain patients who require high doses, he became a target.
“The damage that the proliferation of opioid distribution has done to our community, like many across the United States has been devastating,” U.S. Attorney Matthew Schneider said, according to published reports. “It’s particularly disturbing when the distributor is a medical professional.”
Pompy’s former patients and some former employees have stood by him, saying he is being scapegoated. Former patients have held rallies and started a Facebook group in support of him.
Janet Zureki, a former patient of Pompy, said that — as often happens after a prescriber’s arrest — patients were left in limbo, having to scramble to find another pain doctor. “After the raid and he could no longer prescribe, everyone was dangerously cut off of their medicines, including me,” she said. “It took me three months to find another pain doctor and they put me on a lower dose of medicine. During that three month period, I had to go without medicine and go through withdrawal.”
Zureki defends Pompy.
“As a doctor, I found him to be very compassionate and he also ran a tight ship,” she said. “I have been in his office and have heard him address someone who wasn’t taking their medicine properly, so I know he didn’t stand for that. He worked tirelessly to help the people in our community,” she said.
DOCTORS LAMENT WALKING AWAY
Nadeau is bewildered over having to stop treating his pain patients, at least one of whom died by suicide. And he said his hospital’s decision to stop working with opioids is by no means unique.
Hospitals increasingly see opioids as a liability; an overdose can land them in a lawsuit, he said. But he wrestles with the fact there are people he can no longer help.
“I can’t provide comprehensive care for my patients, meaning treatment of pain, depression, sleep problems, anxiety, and other problems,” Nadeau said. “In patients with chronic pain, there nearly always are a lot of problems.”
Nadeau reached out to fellow physicians to see if they would take his pain patients.
“It’s been extremely difficult to find physicians to provide comprehensive pain therapy,” he said. “I don’t blame physicians for being scared to death and for prescribing to CDC guidelines, but I do blame [some of] them for treating patients badly.”
For his part, Ibsen is treating patients with medical marijuana. Ibsen said he always strived to get patients on opioids to agree to taper down, and about 80 percent did, often using medical cannabis. For the others, opioids were the best treatment, Ibsen said. He understands the threat of the overdose epidemic all too well.
“My nephew died of a heroin overdose” in the summer, he said. “But incarcerating doctors is not going to solve the addiction crisis.”
“There are two things doctors do – we save lives and we relieve suffering. If we’re not willing now to relieve suffering, then what are we about?”
The post Opioid Crackdown An Ethical Issue For Doctors appeared first on Reach Out Recovery.
Keep Calm And Carry On
How to keep calm when everything goes wrong? Truth is, we’re not in control of so many aspects of our lives. Projects don’t always run smoothly, commission checks don’t always flood in. We can’t control what the other people in our lives are going to do… The list in my mind of things that go wrong is long and makes it hard sometimes to stay calm. What were the important words in that sentence? I italicized them for emphasis. That’s right, “In my mind.”
Keep Calm To Manage The Fear
The biggest problem I battle? What’s reality, and what are my fears surfacing? I tend to think in terms of catastrophe so I have to challenge that thinking daily. Maybe nothing went wrong this week, maybe everything went right. I’m working on a project with a colleague who wants to change a paradigm in the way we think about a certain issue. Before I started working with him, my thinking about the issue was not correct. Learning about the validity of his thinking actually did change a paradigm in my thinking. Being open to accepting that my reality is not always right allows me move on, instead of feeling ashamed. There is a lot of shame to overcome in recovery. You already knew that, right? Even after twenty years of recovery experience, I still have to work on keeping my thoughts balanced and my fears at bay. Are constant fear and shame battling just addict thinking? No way, humans are anxious. The world is scary. You don’t have to be in recovery to feel unbalanced. You just have to know what to do.
What Matters Is Staying In The Keep Calm Solution
So what are top three things I do to keep calm and carry on?
I run what I’m thinking by a sponsor, reliable friend, or professional of some kind. It always helps to get a second opinion and then I can pivot if necessary based on the advice I get.
I get right-sized by going to recovery places and doing recovery things. Getting out of my head and into action of some kind always gives me that space to detach a little from the problem and return to it when I have more perspective and tolerance.
I work my recovery lifestyle, not the problem. That means, I pay extra time and attention to self-care and recovery routines, like exercise/nutrition/sober friends. That’s also the time I show up to work or life and just do the next right thing. I try not to think three steps ahead and focus entirely on what I can do that day.
I know when my recovery is in a good place because I can feel it.
I feel good and life seems manageable and light. When the winds change suddenly, it can be overwhelming. Having three basic actions to take helps me to keep calm and carry on, no matter what’s going on.
The post Keep Calm And Carry On appeared first on Reach Out Recovery.
Can A Natural High Prevent Addiction
For some, the natural high is found on the top of a cliff, 33 feet in the air, peering over their toes down to the pool of blue water below. Others find their high by thrashing through in the woods searching for this year’s big buck. Tragically many find their high in a dirty alley, with a used needle, a rubber strap, and a powdery substance mixed with who knows what.
The Need For A High Isn’t The Problem
Our brains were designed to seek a high. Loretta G. Breuning Ph.D., from Psychology Today, explains, “The expectation of a reward triggers a good feeling in the mammal brain, and releases the energy you need to reach the reward.” That good feeling is dopamine.
Drugs Change The Way Your Brain Seeks The High
Recreational drugs cause a rush of dopamine to flood your brain, triggering a feel good high. Your brain remembers those warm fuzzy feelings and wants more. More drugs equal more high. Unfortunately, the drugs change your brain’s natural chemistry, causing the cravings for the high to grow more important than anything else. Even worse, your original dose is no longer enough. Your brain begins to demand MORE.
What About Natural Highs
Studies continue to show that thrill-seeking, impulsive kids have a higher risk for substance use disorder. One way to help prevent drug abuse is to teach them to embrace this innate need for risk and reward, and feed it with healthy adventure. Some healthy activities to try are:
Horseback riding
Zip-lining
Skateboarding
BMX racing
Performing Arts
Hiking
Rock-climbing
Go-carting
Paint-balling
Tag
Fishing
Parachuting
Theme parks
Running
Skating
My son loves the thrill of riding a skateboard down tall concrete slopes. I love traveling to new cities on my own, just to prove I can. Something as simple as taking a new way home or dining out at an exotic new restaurant may do the trick. Just as whiskey may be one person’s vice while heroin may be the only thing that works for someone else, the same is true with healthy alternatives. The key is to keep trying healthy ways to meet this need until you find what works for you.
All humans need to experience the excitement of a natural high, and it’s not so hard to find. It’s each family’s own kind of fun. Is it making dinner, hiking, going to the movies for your family? It’s important to bring fun into your life and follow it. Oh yes, and teach your friends that there isn’t a drug or substance out there that can produce a feeling you can’t get yourself in a healthy, adventurous way.
The post Can A Natural High Prevent Addiction appeared first on Reach Out Recovery.
December 10, 2018
Helping A Friend Who’s Suicidal
From Franziska Ross @ notokapp.com: In June, designer Kate Spade’s and chef Anthony Bourdain’s suicides reminded us that suicide does not discriminate. It can impact anyone, and it is often unexpected. Numerous factors can put a person at risk, including family history of suicide, substance abuse, access to firearms, a history of trauma, chronic illness, prolonged stress and isolation. And not everyone who is suicidal has a known mental health condition. In fact, 54 percent of people who died by suicide did not have a mental health diagnosis.
That’s why it’s critical for everyone to be able to recognize the signs that someone may be considering suicide.
Don’t Ignore These 10 Signs Of Suicide
Threatening to hurt or kill himself or herself.
Looking for ways to kill himself or herself.
Talking or writing about death, dying or suicide.
Rage, anger, seeking revenge.
Feeling trapped, like there’s no way out.
Increasing alcohol or drug use.
Withdrawing from friends, family or society.
Anxiety, agitation, unable to sleep or sleeping all the time.
Dramatic changes in mood.
No reason for living, no sense of purpose in life.
People may show one or many of these signs and some may show signs not listed.
According to the Centers for Disease Control and Prevention (CDC), suicide rates are increasing. It’s clear that this is a mental health crisis we need to address.
What Can You Do?
Enroll in a Mental Health First Aid course today to learn more about suicide, how to recognize the signs that someone may be at risk and how to get them the help they need. Mental Health First Aid will also teach you about the risk factors and warning signs for other mental health and addiction issues, strategies for how to help someone in both crisis and non-crisis situations and where to turn for help.
If you or someone you know needs immediate support, call the National Suicide Prevention Lifeline at 800-273-TALK (8255) or call 911.
Other Useful Links:
Emergency Medical Services: 911
National Suicide Prevention Hotline: 1-800-273-8255
Recovery Guidance: www.recoveryguidance.com
SAMHSA Treatment Referral Helpline: 1‑877‑SAMHSA7 (1‑877‑726‑4727)
Veterans Crisis Line: 1-800-273-8255 PRESS 1
NAMI Helpline: 1-800-950-NAMI (6264)
National Domestic Violence Hotline – Call 800-799-SAFE (7233)
*Disclaimer: The notOK App is not a substitute for, nor does it replace, professional medical advice, diagnosis, or treatment. If you are experiencing a medical or mental health emergency or crisis, immediately dial 9-1-1*
is not a substitute for, nor does it replace, professional medical advice, diagnosis, or treatment. If you are experiencing a medical or mental health emergency or crisis, immediately dial 9-1-1*
The post Helping A Friend Who’s Suicidal appeared first on Reach Out Recovery.
Depression, Alcoholism Often An Unbearable Combination
From The Miami Herald:
Clinical depression and alcohol use disorder — commonly known as alcoholism — are among the most frequent mental disorders seen in patients.
Often the same individual suffers from both problems at the same time. The symptoms and suffering caused by either condition alone can be daunting, but when an individual is dealing with both conditions, the suffering and burden on the patient and their families becomes unbearable.
These dual disorders are associated with the highest occurrence of dysfunctions, need for hospitalizations and complications such as suicidal behavior. They are also less responsive to available treatment.
The exact cause of why so many people develop both problems is still unknown.
Chronic alcoholism is known to cause depression, as well as worsen existing depression. Many people with depression resort to heavy drinking to “drown out” their sorrows.
Studies have also pointed to the significant role of heredity in developing these conditions.
Recent scientific evidence has highlighted the role of inflammation and alterations to the immune system in both clinical depression and chronic excessive alcohol drinking. Studies suggest that inflammation plays a bidirectional role in both depression and alcoholism. On one hand, inflammation seems to cause depression and increases the propensity for drinking alcohol. On the other hand, both depression and excessive alcohol use, through different mechanisms, increase the level of inflammation in the brain.
Stem-cell therapy holds great promise for decreasing inflammation in the body as studies have shown that one session of this treatment can decrease inflammation over a one-year period. Stem-cell therapy may undercut a major mechanism underlying the dual disorders of depression and alcoholism and provide new hope for people suffering from these disabling disorders.
The Department of Psychiatry at the University of Miami Miller School of Medicine, in collaboration with the University of Miami’s Stem Cell Institute, is conducting a new study funded by the National Institute of Alcohol Abuse and Alcoholism, National Institute of Health, to test the usefulness of stem cell therapy for people suffering from the “double trouble” of clinical depression and alcoholism.
The post Depression, Alcoholism Often An Unbearable Combination appeared first on Reach Out Recovery.
Parents: 7 Things NOT To Say To Your Teen
Our teen’s choice in partners, schools, work, and recreation will at some point rock the boat. As parents, we want what’s best for them. If they would listen to us, we could save them from so much pain. Alas, they won’t. Here are some ways we can accept our teen’s choices, and some ways we can actually make our relationship worse.
Our Teen’s Choice Isn’t Our Choice
This is such a difficult concept for parents to grasp. Against our wishes and better judgement, our teens are likely to do or at least try any number of these things:
Dating & Marriage. Maybe your teen is LGBTQ. Maybe you are LGBTQ and they are heterosexual. Perhaps they won’t ever get married or produce the number of grandchild we want. She or he might have children without a spouse, or become sexually active before you want them to. All of these relationship issues are strong triggers.
Change religions. Some teens will deny their religious upbringing while others are likely to embrace a new faith or marry outside of the family’s religion.
College and career choices. They may not go to our alma matter or even be accepted there. They may enter the workforce or travel the country for a year.
Dabbling in drugs and alcohol. This one’s particularly scary, especially if we have been affected by addiction.
As parents, it is so very important to respond in a positive manner. While for some parents, our teen’s choice may not be a surprise, others may feel blind-sighted with this revelation. Either way, when our hopes and dreams for the child veer off course, we’re likely to feel:
Sadness
Disappointment
Anger, and
Perhaps, even disgust.
So What To Do?
First, have an open dialogue. Open listening is the most important aspect in any conflict. The child needs to know he or she is loved and accepted because if not, this will create a very difficult path for them.
Second, get up to speed. Don’t be surprised if your child has already done significant research about his or her decision (except in the case of addiction). You can get a better understanding by immediately doing your own research.
Third, accepting their choice may be difficult for you, so aim for damage control. Trying to prove your child wrong or demand he or she conforms to your will isn’t likely to help. It almost always pushes your child away.
Here Are Some Things NOT To Say
“Are you sure?” They may not be, but this is something for your teen to figure out. Saying this makes your teen feel you are questioning their thoughts and feelings. Also, it is seen as a negative comment regarding your own preferences for the teen’s life.
“Don’t tell your… ( dad, grandmother, brother, etc.).” This is a slap in the face and starts a spiral of shame.
“You’re breaking my heart.” This puts undo shame and responsibility on the child. As parents, we are responsible for our own feelings.
“Who have you told?” Underlying this statement is also shame for the parent is looking to control; i.e, “I hope the neighbors, your coach, etc., don’t already know and maybe we can keep this a secret.”
“You’re too young to know.” Letting children go is tough at any age. They might be wrong, but teenage and young adulthood is the age-appropriate time for making mistakes.
“God/Allah/Jesus… will punish you for this is a sin.” Using religion to control behavior is punishing by shame. It doesn’t work and often only drives a wedge between your child and yourself and his or her support group. This is a horribly inappropriate thing to say to the teen as he/she/they already know your views and this makes them feel even worse about the status. Punishing by shaming does not work. Sending them back to church/mosque/synagogue and making them read religious texts about the sinfulness will only cause greater harm.
“You are banned from this house and we do not acknowledge you as our child.” How horrific that a parent would ban a child and unfortunately, this still happens frequently. This will likely strain your relationship for life.
What You Can Say
To be honest, your teen’s choice has just thrown you a curve ball. It’s OK to take some time to figure out how you feel. Before you react, give yourself permission to be quiet and think. You deserve time to research and even seek out opinions of friends, family, and counselors. You can say things like:
I’m not sure what to say.
I’m going to need some time to think about this.
I didn’t see this coming, or I need to do some research.
I love you no matter what.
As parents, we do have to right to set boundaries on appropriate and inappropriate behavior (especially when dealing with alcohol and drug use). We can tell our children what we need. We do not have to accept unacceptable behavior, but if we are very upset, we don’t want to speak and act out of fear or anger. Many of those speeches and tirades only lead to hurt, not healing. Give yourself some time to look for helpful ways to love and support your teen’s choice.
The post Parents: 7 Things NOT To Say To Your Teen appeared first on Reach Out Recovery.






