Leslie Glass's Blog, page 380
April 7, 2018
The Reality Of Alcohol Abuse On America
It’s National Alcohol Awareness Month, so I thought I’d pull a few alcohol stats to remind us that on top of the opioid crisis, meth destruction, and other drug horrors, we still have an alcohol problem in this country.
In these complicated times, it’s easy to look at alcohol as the lesser of the evils, but let’s not forget that alcohol is at the center of many of America’s biggest problems. For example,
Economically costly:
“Excessive alcohol consumption cost the U.S. $223.5 billion in 2006 alone, and nearly half of that burden was borne by the government, according to a new study conducted by the Centers for Disease Control and Prevention (CDC).” Time
Car Accidents:
“Every day in America, another 29 people die as a result of drunk driving crashes. That’s one person every 50 minutes.” MADD
Rape:
“Quite honestly, alcohol is the No. 1 date rape drug,” said Mike Lyttle, regional supervisor for the Tennessee Bureau of Investigation’s Nashville crime lab. “… Roofies are very rarely — if ever — seen in real life.” USA Today
Assault:
“Alcohol Use Increases the Risk of Sexual Assault. At least half of sexual assaults among college students occur after the perpetrator, the victim, or both consume alcohol. Alcohol use can increase the risk of sexual assault in several ways. Alcohol use by a potential assailant can lead to increased aggressive behavior and an inability to interpret another person’s sexual interest accurately.” National Institute of Justice
Child Abuse:
“STRONG LINKS HAVE BEEN FOUND between child maltreatment and alcohol use, especially when drinking is harmful or hazardous. A number of studies have established that alcohol is a significant contributory factor to child maltreatment, and many show that being maltreated as a child is associated with marked increases in the risk of hazardous or harmful drinking in later life.” Govt. of Canada
Mental Illness:
“Mental illness and alcoholism or drug abuse interact in a complex dance, “says James Garbutt, MD, professor of psychiatry at the University of North Carolina at Chapel Hill and research scientist at UNC’s Bowles Center for Alcohol Studies. “Mental illnesses can increase the risk for alcoholism or drug abuse, sometimes because of self-medicating. On the other hand, alcoholism can lead to significant anxiety and depression that may appear indistinguishable from a mental illness. Finally, one disorder can be worse than the other.” Everyday Health
Disease:
“Here are 12 conditions linked to chronic heavy drinking. Anemia, Cancer, Cardiovascular disease, Cirrhosis, Dementia, Depression, Seizures, Gout, High blood pressure, Infectious disease, Nerve damage, and Pancreatitis.” Web MD
Sadly, this is just a short list of the things alcohol abuse affects, but let it serve as a warning in case anyone has any questions about how harmful alcohol can be in comparison to other substances.
If you need treatment help, click here
The post The Reality Of Alcohol Abuse On America appeared first on Reach Out Recovery.
Parental Alcohol Abuse Linked To Child Deaths And Injuries
From The Guardian One in three child deaths or serious injuries from neglect or abuse linked to alcohol misuse. A report commissioned by a cross-bench group of MPs and peers in Britain found that alcohol abuse by parents was behind horrific problems for children and warned that budgets of alcohol and drug treatment programmes were being cut.
More than one in three deaths or serious injuries suffered by a child through neglect or abuse is linked to parental drinking, a study has found.
“Parental alcohol misuse scars kids for life and can lead many into a life of drinking too much themselves,” said Liam Byrne, the Labour MP and chairman of the All-Party Group for Children of Alcoholics.
“Millions of parents drink too much and their misuse of alcohol causes horrific problems for their children.”
Alcohol misuse was implicated in 37% of cases of a child’s death or serious injury after abuse or neglect between 2011 and 2014, the study found.
More than half of councils did not have a strategy to help children of alcoholics. Referrals to alcohol treatment services were falling in more than 50% of local authorities, according to information released under freedom of information laws.
The study also found that 92% of the 53 councils that responded were cutting budgets for alcohol and drug treatment services. Cuts differed in severity, from £9.6m – or 58.1% – in Lancashire, to £87,000 – or 1.1% – in Wolverhampton. The average cut to local authority funding was around £198,000.
The group also found that 15% of children had their bedtime routine disrupted due to their parents’ drinking and 18% were embarrassed at seeing their parent drunk.
The report called for better funding to help youngsters affected by parents who drink. Byrne, who lost his father to alcoholism in 2015, said the group’s campaign had won a “new commitment from government for a national strategy to stop parental alcohol misuse”.
He added that the report showed “just why the government must act fast to put an effective plan in place”.
The study, published by the Parliamentary Office of Science and Technology following a request by the all-party parliamentary group for children of alcoholics, found that 61% of care applications in England involved misuse of alcohol and/or drugs.
Children living with alcohol-dependent parents reported feeling socially isolated and reluctant to seek help, due to feelings of stigma, shame and guilt about not wanting to betray parents, the study found.
A Department of Health and Social Care spokeswoman said: “We are acutely aware of the impact some parents drinking can have on their children – that’s why work is well underway on a new children of alcoholics strategy, which will look at what further support we can provide to families to tackle alcohol harms.
“This comes in addition to our new higher duties to target cheap, high strength cider and the UK chief medical officers’ guidelines, which help adults make informed decisions about their drinking.”
The shadow health secretary, Labour’s Jonathan Ashworth, said: “This report lays bare the real and damaging impact parental drinking can have on children. The findings of this report make me more determined than ever to prioritise tackling addiction while supporting the children and families affected.
“Having recently spoken about my own father’s drinking problems, I welcomed the government’s commitment to support children of alcoholics. However, this report emphasises there is still a long way to go. Almost all local authorities have cut treatment services and many still do not have strategies for children of alcoholics in place.
“It’s time we as a society took these issues more seriously so that children no longer need suffer in silence.”
The post Parental Alcohol Abuse Linked To Child Deaths And Injuries appeared first on Reach Out Recovery.
April 6, 2018
More Americans Aware Of Opioid Addiction
From Science Daily
A new survey by The Associated Press-NORC Center for Public Affairs Research reveals the number of Americans who see opioid addiction as a significant issue for their community today is up significantly over just two years ago. Forty-three percent of Americans now say the misuse of prescription drugs is a serious problem, compared with 33 percent in 2016.
A majority of Americans report having experience with substance abuse of various types, and 13 percent have had a relative or close friend die from an opioid overdose. Although 53 percent of the public sees prescription drug addiction as a disease, many regard such addiction as a behavioral failing. Forty-four percent say opioid addiction indicates a lack of willpower or discipline; 32 percent say it is caused by a character defect or bad parenting, and less than 1 in 5 Americans are willing to associate closely with a friend, colleague or neighbor who is addicted to prescription drugs. This indicates that stigma surrounding opioid addiction is an issue.
The findings are among many in a survey exploring attitudes and awareness of Americans about the opioid epidemic in particular and drug misuse in general, as well as how to address the crisis.
“In the national effort to grapple with the enormous issue of opioid addiction, it is important to know the level of awareness and understanding of Americans who find themselves in the midst of an epidemic that is claiming growing numbers of lives,” said Caitlin Oppenheimer, senior vice president of public health at NORC. “This survey provides important, and in some cases troubling, information.”
Additional findings from the survey include:
Two-thirds of respondents say their community is not doing enough to make treatment programs accessible and affordable or to find improved methods of treating addiction.
Sixty-four percent would like to see more effort to crack down on drug dealers.
Fifty-seven percent of Americans have experience dealing with substance misuse ranging from taking a painkiller that wasn’t prescribed to overdosing.
Twenty-four percent say they have an addicted relative, close friend, or that they themselves are addicted to opioids.
“The number of people who recognize how serious the opioid epidemic is in this nation is growing,” said Trevor Tompson, vice president for public affairs research at NORC. “There is clearly a continuing challenge to ensure that what is learned about the crisis is grounded in fact.”
Facebook is the dominant source of information on social media about the opioid crisis. Of the 74 percent of adults who use Facebook, 41 percent say they have seen messages about opioids or about death from overdoses. Fewer users of other platforms report seeing such information.
Story Source:
Materials provided by NORC at the University of Chicago. Note: Content may be edited for style and length.
A new survey by The Associated Press-NORC Center for Public Affairs Research reveals the number of Americans who see opioid addiction as a significant issue for their community today is up significantly over just two years ago. Forty-three percent of Americans now say the misuse of prescription drugs is a serious problem, compared with 33 percent in 2016.
A majority of Americans report having experience with substance abuse of various types, and 13 percent have had a relative or close friend die from an opioid overdose. Although 53 percent of the public sees prescription drug addiction as a disease, many regard such addiction as a behavioral failing. Forty-four percent say opioid addiction indicates a lack of willpower or discipline; 32 percent say it is caused by a character defect or bad parenting, and less than 1 in 5 Americans are willing to associate closely with a friend, colleague or neighbor who is addicted to prescription drugs. This indicates that stigma surrounding opioid addiction is an issue.
The findings are among many in a survey exploring attitudes and awareness of Americans about the opioid epidemic in particular and drug misuse in general, as well as how to address the crisis.
“In the national effort to grapple with the enormous issue of opioid addiction, it is important to know the level of awareness and understanding of Americans who find themselves in the midst of an epidemic that is claiming growing numbers of lives,” said Caitlin Oppenheimer, senior vice president of public health at NORC. “This survey provides important, and in some cases troubling, information.”
Additional findings from the survey include:
Two-thirds of respondents say their community is not doing enough to make treatment programs accessible and affordable or to find improved methods of treating addiction.
Sixty-four percent would like to see more effort to crack down on drug dealers.
Fifty-seven percent of Americans have experience dealing with substance misuse ranging from taking a painkiller that wasn’t prescribed to overdosing.
Twenty-four percent say they have an addicted relative, close friend, or that they themselves are addicted to opioids.
“The number of people who recognize how serious the opioid epidemic is in this nation is growing,” said Trevor Tompson, vice president for public affairs research at NORC. “There is clearly a continuing challenge to ensure that what is learned about the crisis is grounded in fact.”
Facebook is the dominant source of information on social media about the opioid crisis. Of the 74 percent of adults who use Facebook, 41 percent say they have seen messages about opioids or about death from overdoses. Fewer users of other platforms report seeing such information.
Story Source:
Materials provided by NORC at the University of Chicago. Note: Content may be edited for style and length.
The post More Americans Aware Of Opioid Addiction appeared first on Reach Out Recovery.
Get Up And Get Moving To Be Happier
From the NY Times
When people get up and move, even a little, they tend to be happier than when they are still, according to an interesting new study that used cellphone data to track activities and moods. In general, the researchers found, people who move are more content than people who sit.
There already is considerable evidence that physical activity is linked to psychological health. Epidemiological studies have found, for example, that people who exercise or otherwise are active typically are less prone to depression and anxiety than sedentary people.
But many of these studies focused only on negative moods. They often also relied on people recalling how they had felt and how much they had moved or sat in the previous week or month, with little objective data to support these recollections.
For the new study, which was published this month in PLoS One, researchers at the University of Cambridge in England decided to try a different approach. They would look, they decided, at correlations between movement and happiness, that most positive of emotions. In addition, they would look at what people reported about their activity and compare it with objective measures of movement.
To accomplish these goals, they first developed a special app for Android phones. Available free on the Google app store and ultimately downloaded by more than 10,000 men and women, it was advertised as helping people to understand how lifestyle choices, such as physical activity, might affect people’s moods. (The app, which is no longer available for download, opened with a permission form explaining to people that the data they entered would be used for academic research.)
The app randomly sent requests to people throughout the day, asking them to enter an estimation of their current mood by answering questions and also using grids in which they would place a dot showing whether they felt more stressed or relaxed, depressed or excited, and so on.
Periodically, people were also asked to assess their satisfaction with life in general.
After a few weeks, when people were comfortable with the app, they began answering additional questions about whether, in the past 15 minutes, they had been sitting, standing, walking, running, lying down or doing something else.
They also were asked about their mood at that moment.
At the same time, during the 17 months of the study, the app gathered data from the activity monitor that is built into almost every smartphone today. In essence, it checked whether someone’s recall of how much he or she had been moving in the past quarter-hour tallied with the numbers from the activity monitor.
In general, the information provided by users and the data from activity monitors was almost exactly the same.
Of greater interest to the researchers, people using the app turned out to feel happier when they had been moving in the past quarter-hour than when they had been sitting or lying down, even though most of the time they were not engaged in rigorous activity.
In fact, most of the physical activity that people reported was gentle walking, with little running, cycling or other more strenuous exercise.
But the links between moving in any way and feeling happy were consistent for most people throughout the day, according to the data from their apps. It also didn’t matter whether it was a workday or weekend.
The researchers also found that people who moved more frequently tended to report greater life satisfaction over all than those who reported spending most of their time in a chair.
In general, the results suggest that “people who are generally more active are generally happier and, in the moments when people are more active, they are happier,” says Gillian Sandstrom, a study co-author who was a postdoctoral researcher at Cambridge and is now a lecturer in psychology at the University of Essex.
In other words, moving and happiness were closely linked, both in the short term and longer term.
Of course, this type of study does not establish causation. It cannot tell us whether being more active actually causes us to become happier or, conversely, whether being happy causes us to move more. It only shows that more activity goes hand-in-hand with greater happiness.
104COMMENTS
The study also is limited by its reliance on cellphone data, Dr. Sandstrom says, because it may not have captured information about formal exercise. People often do not carry their phones when they run, cycle or engage in other types of vigorous activity, she and her colleagues point out in the study. So those types of workouts would not be reflected in the app or the phones’ activity monitor, making it impossible to know from this data set whether formal exercise is linked to happiness, for better or worse.
Still, the size of the study group and the consistency of the findings are compelling, Dr. Sandstrom says. They do indicate that if you get up and move often, you are more likely to feel cheerful than if you do not.
Physical activity has long been known to reduce depression and anxiety, and is commonly prescribed to prevent or cure negative mental health conditions. A new review suggests the physical activity frequency and volume are essential factors in the relationship between physical activity and happiness.
The post Get Up And Get Moving To Be Happier appeared first on Reach Out Recovery.
10 Ways To Know If You Are An Adult
As my children grew from toddlers, to teens, to towering over me, I often find myself looking for signs that they are full fledged adults or as they say, “adulting.” I see people who think of themselves as adults everyday, but sometimes they are only emotional toddlers stomping around demanding others make their life easier.
The 10 signs I look for are small and often overlooked, but as far as I am concerned they tell me a great deal about an individual’s maturity level. Here are my top ten signs someone is an adult:
1. An Adult Make Their Bed Every Day
I know this sounds silly, but it starts the day off with an accomplishment and as an added bonus it rewards us at the end of our day with a made up bed. Our Intern wrote a article about the importance of making your bed. Making your bed everyday may not be easy, but nothing adults do is easy.
2. Adults Finish What They Start
From putting the clean clothes away to painting the baseboard. “Children start projects, but adults finish them.” I have heard it said, “When you are stuck for an answer find the nearest finish line and cross it.” It can be anything from wiping the fingerprints off the front door to returning a DVD to the RedBox to putting your grocery cart back. Once some of my grown-up kids discovered the good feeling of crossing finish lines they started looking for them everywhere. They stopped starting a new project every weekend and started looking instead for projects to complete.
3. Adults Are On Time
Ask any boss what is important to them. Simple stuff, like being on time every day. Yes, life is busy and we can all over schedule ourselves. That is one reason I love the slogan, “Keep It Simple.” If I can’t make it to places on time it is often a sign for me to stop trying to please too many people. Being on time, every time, to everything, will put someone miles ahead of someone who is constantly “running late.”
4. Adults Don’t Come Empty Handed
Even if they have little to offer, adults will find a way to share something. I often look to see if my children remember to bring something when they are invited to a celebration. For Thanksgiving one year my daughter was flat broke, but she stopped and bought an off-brand of soda to share. It costs her $.50, but showed that she was thinking of others even during her own hard times. She was only 19 years old, and her siblings were impressed that she contributed what she could. I have seen adults stop and pick flowers if they had nothing else to bring. Adults think of others and reflect that with their actions.
5. Adults Pick Up After Themselves And Others
My kids were like so many others when they were teens, just close the door and hope for better days. Well, they aren’t kids anymore and how they keep their places tells a lot about their ability to manage their life. While cleaning up after ourselves makes sense to most people, even harder is the idea of picking up after someone else. Walking down a beach and finding litter left by a total stranger is fairly common. My friend is great about picking up litter others have thrown down. I try hard to adopt his attitude of remembering the higher good is to have a cleaner environment. Messes are a part of life. Cleaning up after ourselves and others is a big part of being an adult. Our town has a clean up day every year. It was where I first learned the importance of cleaning up after others.
6. Adults Know How To Manage Money
Adults understand the concept of delayed gratification. I like to think my children are in control of their money and not panicked because they forgot to look before buying an item they felt they “had to have.” Adults keep track of where the money goes and more than that they tell their money where to go. I am still trying to be better with my money, but I know starting with a goal of knowing where it is keeps me in touch with my limitations and helps me avoid financial drama.
7. An Adult Know How To Argue
Grown Ups find ways to compromise with each other. Adults allow others to finish what they are saying. Adults don’t always agree, but they know it is important that everyone feels heard. To avoid a heated argument they can say, “You may be right.” With this attitude, adults look for common ground and focus on finding solutions. Being level headed, tolerant, and calm is a welcome characteristic in today’s world.
8. Adults Know How To Entertain Themselves
Children fuss when life is boring. Adults enjoy the opportunity to let their brain decompress. Adults don’t need constant stimulation and understand that quiet is a rare gift in our often over-stimulated culture. They embrace the quiet and are simply patient or find something to occupy themselves with until the situation changes.
9. Adults Return The Things They Borrow
Adults return things they borrowed in better condition than when they received them. How many times in my youth did I return something I had accidentally broken while using and thought an apology was sufficient. Eventually I learned if I broke it I would need to buy a replacement. Adults take borrowed clothes to the dry cleaners before returning them. They wash the car and fill it with gasoline before returning it. They know the owner risked trusting them and want to show appreciation for that trust. This also helps get a yes the next time you need to borrow something from a friend.
10. Finally, Adults Don’t Constantly Complain
They accept life on life’s terms. Adults have survived bad teachers, bad bosses, and bad days. They have learned words of gratitude can pause their desire to bitch and moan about everything that doesn’t go their way. I pay close attention to what my children do when they have a job or college class they don’t like. It can be a real marker of where they are on the road to maturity.
I would like to thing my adult children are making progress toward becoming fully developed adults, but only time will tell. Too many times in our culture today there seems to be a disconnect between being of service to our fellow man and being served. The good news is it is never too late to grow up.
Save
Save
The post 10 Ways To Know If You Are An Adult appeared first on Reach Out Recovery.
Co-Dependent’s Fear-less Gluten-Free Blueberry Cobbler
For years, I felt sick when I ate foods made with flour and sugar, but I ate them anyway. I should have the independence to refuse such foods by saying, “That doesn’t work for me.” Yet, I’m too scared to even say that. This week I gave myself an ultimatum: Do I want to live in fear for the rest of my life or be brave?
Fear Stems From My Childhood
When I was growing up, I had no control over what I had to eat. Liver and onions, slimy canned spinach, fried squirrel, and fried rabbit, were all dishes I HATED. They were all served weekly. The dinner table rule was “Eat it or wear it.” Although my parents’ mandates might sound innocent, the pain remains.
I Still Live In Fear
I am a grown up, and I almost never share a meal with my parents. Why does this still haunt me? Because I deny the truth of the original hurt. When I was a kid, I should have been given a choice to eat what was prepared or make my own food. How I was treated was wrong, but I’m too afraid to say it out loud. Just typing it makes me break out in a cold sweat. Until I can admit the truth, I will be imprisoned by the lie.
Deep-seated fears like this are quite common among adult children of alcoholics and survivors of child abuse. Emotional abuse makes people fearful. They are particularly afraid of confrontation or using their voice.
Saved By A Higher Authority
Recently, I learned I am allergic to gluten. What a relief! Now I have someone bigger and braver than me who supports my food choices. However, I want that same freeing endorsement for all of my choices. And I have that choice. The only person holding me back is me.
I don’t have to stand up to all of my fears at once. Taking each day, one day at a time keeps the new habit manageable. Likewise, I don’t have to give this much thought. All I need to do is practice my canned response, “That doesn’t work for me.”
Blueberry Cobbler Sans Gluten & Fear for One
I used this new principle to tackle one of my favorite recipes, blueberry cobbler with a crumb top. Since wheat flour “No longer works for me,” I replaced the flour with blended oats. If you are allergic like me, make sure the oats are gluten free. Oats are essentially a gluten free grain, however, they are often cross-pollinated by nearby wheat. Be sure to read the label.
For The Filling:
1 pint fresh blueberries, rinsed
2 tablespoons of sugar
½ teaspoon of vanilla
1 tablespoon of butter cut into small pieces
1 small oven-proof dish. I use a 4 cup glass bowl.
Spray the baking dish with non-stick spray. Add the berries, sugar, vanilla, and butter to the bowl and stir to combine.
For The crust:
1 cup gluten-free quick-cooking oats
2 tablespoons of sugar
½ teaspoon of cinnamon
3 tablespoons of butter
Place all of the ingredients in a food-processor and blend until the crust is the consistency of small pea-sized clumps. For a more refined crust, blend the oats first then blend in remaining ingredients. Spread the crust mixture on top of berries. Bake at 350 degrees for approximately 30 minutes.
* White flour may be substituted for the oats and tastes just as good. Sometimes I use brown sugar instead of white.
The post Co-Dependent’s Fear-less Gluten-Free Blueberry Cobbler appeared first on Reach Out Recovery.
NIH Launches HEAL Initiative To Combat Opioid Crisis
NIH launches the HEAL (Helping to End Addiction Long-term) Initiative, an aggressive, trans-agency effort to speed scientific solutions to stem the national opioid public health crisis. This Initiative will build on extensive, well-established NIH research, including basic science of the complex neurological pathways involved in pain and addiction, implementation science to develop and test treatment models, and research to integrate behavioral interventions with Medication-Assisted Treatment (MAT) for opioid use disorder (OUD). Successes from this research include the development of the nasal form of naloxone, the most commonly used nasal spray for reversing opioid overdose, the development of buprenorphine for the treatment of opioid use disorder, and evidence for the use of nondrug and mind/body techniques such as yoga, tai chi, acupuncture, and mindfulness meditation to help patients control and manage pain.
Over the past year, NIH has worked with experts from public and private organizations to identify the areas that would benefit from focused efforts by NIH alone or in partnerships with outside organizations.
The NIH HEAL Initiative will bolster research across NIH to:
Prevent Addiction through Enhanced Pain Management
More than 25 million Americans suffer from daily chronic pain. NIH will support research to understand how chronic pain develops, making patients susceptible to risks associated with opioid use. NIH will work with partners from the biopharmaceutical industry to develop a data sharing collaborative, new biomarkers for pain, and a clinical trials network for testing new pain therapies. NIH will also enhance the pipeline of treatments for pain and enhance clinical practice for pain management.
Improve Treatments for Opioid Misuse Disorder and Addiction
More than 2 million Americans have OUD. Millions more misuse opioids, taking opioid medications longer or in higher doses than prescribed. NIH will support research that can prevent and treat opioid misuse and addiction, and that will help people with OUDs achieve and maintain a meaningful and sustained recovery.
The post NIH Launches HEAL Initiative To Combat Opioid Crisis appeared first on Reach Out Recovery.
44,000 Deaths Every Year From Binge Drinking
How Was It Studied
Behavioral Risk Factor Surveillance System 2015 data (analyzed in 2016) were used to estimate the prevalence, frequency, intensity, and total binge drinks among U.S. adults. Total annual binge drinks was calculated by multiplying annual binge-drinking episodes by binge-drinking intensity.
Results
In 2015, a total of 17.1% of U.S. adults (37.4 million) reported an annual average of 53.1 binge-drinking episodes per binge drinker, at an average intensity of 7.0 drinks per binge episode, resulting in 17.5 billion total binge drinks, or 467.0 binge drinks per binge drinker. Although binge drinking was more common among young adults (aged 18–34 years), half of the total binge drinks were consumed by adults aged ≥35 years. Total binge drinks per binge drinker were substantially higher among those with lower educational levels and household incomes than among those with higher educational levels and household incomes.
Conclusions
U.S. adult binge drinkers consume about 17.5 billion total binge drinks annually, or about 470 binge drinks/binge drinker. Monitoring total binge drinks can help characterize disparities in binge drinking and help plan and evaluate effective prevention strategies.
The post 44,000 Deaths Every Year From Binge Drinking appeared first on Reach Out Recovery.
April 5, 2018
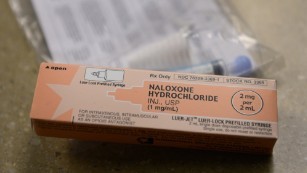
Surgeon General Issues Rare Advisory On Narcon
(CNN)The US surgeon general issued an advisory Thursday recommending that more Americans carry the opioid overdose-reversing drug, naloxone.
The drug, sold under the brand name Narcan (among others), can very quickly restore normal breathing in someone suspected of overdosing on opioids, including heroin and prescription pain medications.
Dr. Jerome Adams emphasized that “knowing how to use naloxone and keeping it within reach can save a life.” To make his point, Adams relied on a rarely used tool: the surgeon general’s advisory. The last such advisory was issued more than a decade ago and focused on drinking during pregnancy.
What is naloxone?
Adams noted that the number of overdose deaths from prescription and illicit opioids doubled in recent years: from 21,089 deaths across the nation in 2010 to 42,249 in 2016.
America’s top doctor attributed this “steep increase” to several contributing factors, including “the rapid proliferation of illicitly made fentanyl and other highly potent synthetic opioids” and “an increasing number of individuals receiving higher doses of prescription opioids for long-term management of chronic pain.”
“Research shows that when naloxone and overdose education are available to community members, overdose deaths decrease in those communities,” Adams said. Naloxone is used by police officers, first responders and emergency medical techs to reverse opioid overdoses. Adams added that increasing both the availability of naloxone and effective treatment is critical to ending the opioid epidemic.
ER visits for opioid overdose up 30%, CDC study finds
The surgeon general’s recommendation is an important public message that lifts opioid misuse and opioid overdose deaths from the margins and places these issues in the mainstream, according to CNN Chief Medical Correspondent Dr. Sanjay Gupta.
Gupta agrees with Adams and believes that naloxone can save lives. Still, there are challenges, he said.
“You’re basically saying, as a doctor, ‘I’m giving you this opioid for your pain, and by the way, you might kill yourself, so here’s this as well,’ ” Gupta said. “The next step in this would be truly defining who is high-risk and should be getting Narcan along with their opioid prescriptions.”
Outside of medicine, some see the Surgeon General’s Advisory as a pragmatic gesture.
‘A new reality’
“The surgeon general is addressing a new reality in a practical way by encouraging people to have access to naloxone and to know when and how to administer it,” Dallas lawyer Jeffrey Simon said. “I equate having naloxone at the ready to having a CPR kit at the ready: Both can save lives as emergency care if administered in time.
“No one would find it strange if a surgeon general encouraged more people to learn CPR or the Heimlich maneuver,” said Simon, whose firm, Simon Greenstone Panatier Bartlett P.C., has represented counties suing pharmaceutical companies for their alleged roles in opioid addiction.
Simon added that people are regularly encouraged to learn how to perform CPR or the Heimlich maneuver to render aid to someone — even a stranger — who might require assistance. Carrying and using naloxone is no different, he said.
However, a recent study suggested that state laws providing wider access to naloxone may unintentionally increase opioid abuse.
Access isn’t enough
With access to naloxone reducing the risk of overdose death, more dangerous drug use — including higher doses — may become more appealing, the researchers speculated based on the data. Such increased abuse may even lead to higher death rates, according to Jennifer Doleac, one of the study’s authors and an assistant professor of public policy and economics at the University of Virginia.
Overdose antidote availability doesn’t always mean fewer deaths, study says
“Our research shows that expanding access to naloxone is not enough to reduce opioid-related mortality and may even increase opioid abuse,” Doleac said. “We found that effects were more beneficial in places where more drug treatment is available. So, if we are going to increase naloxone access, then it is also important to increase funding for drug treatment.”
The necessity of recovery treatment to end the opioid epidemic is a point on which seemingly all agree.
Simon said that “when we speak of opioid addicts, we need to remember that addiction is a disease. We want addicts to get into recovery, and if they die from an overdose, that can’t happen. Keeping them alive long enough for them to make headway with addiction treatment is crucial, and naloxone is often a key component to achieving that goal.”
Quoting a statistic cited by a deputy attorney general, Simon noted that more Americans under the age of 50 die each year from opioids than from any other cause, including heart attacks and choking.
“Unfortunately, it’s easy for anyone to overdose on opioids, so we are not just talking about saving the lives of addicts,” he said.
‘Urgent need’
In the US, drug overdoses led to 632,331 deaths from 1999 to 2016, with 351,630 being opioid overdose deaths, according to the Morbidity and Mortality Weekly Report released Thursday by the CDC.
Across the nation, 63,632 people died from drug overdoses in 2016, with opioids accounting for about two-thirds of that total.
Still, the CDC found wide variation across the states. For example, New Hampshire, Ohio and West Virginia experienced the highest overdose death rates in multiple drug categories in 2016, while other states — primarily those in the Midwest and West — recorded the highest rates of psychostimulant-involved deaths. And in 2016, some states, including Maryland, Rhode Island and West Virginia, had higher rates of prescription opioid-involved overdose deaths than those involving heroin.
Deaths due to synthetic opioids such as fentanyl and carfentanil accounted for 30.5% of all drug overdose deaths in 2016, a 100% increase over 2015, the report noted.
There is an “urgent need” to implement a multifaceted public health approach, according to the authors of the government report. Suggested measures include increased naloxone availability, harm reduction services and recovery treatment.
Speaking at the National Prescription Drug Abuse & Heroin Summit in Atlanta on Thursday morning, Adams addressed the belief that providing naloxone “doesn’t make a difference,” since many people with drug addictions will just “go on and misuse substances again.”
His experience from traveling all over the country is that there are “countless examples” in which naloxone has changed an individual’s life for the better.
Mothers’ tales
Adams noted that in 46 states, people who are or who know someone at risk for opioid overdose can get trained to use naloxone properly and may receive naloxone by “standing order” — without a prescription — from pharmacies or some community-based programs.
He also said that for many people, the “opioid crisis is not only pressing, it’s personal. My own brother, as many of you know, is serving a 10-year prison sentence for stealing $200 to support his addiction.”
Follow CNN Health on Facebook and Twitter
See the latest news and share your comments with CNN Health on Facebook and Twitter.
On the plane to Atlanta, Adams said, a flight attendant told him about her son who died from an opioid overdose, while a few weeks ago, another mother, Missy Owen, shared her own tragic story. Her son, once president of his high school senior class, an honor student and a community volunteer, turned to opioids from his family’s medicine cabinet when he was overcome with stress and unable to sleep. Though he battled his addiction, he ultimately died from an overdose.
“No mother should have to bury their child — and especially not when there’s a life-saving medication that virtually anyone can access,” Adams said. “It is for this reason that I am issuing the first Surgeon General’s Advisory in 13 years.”
The post Surgeon General Issues Rare Advisory On Narcon appeared first on Reach Out Recovery.
Reversal On Peanut Allergy
Peanuts are back on the menu. In a significant reversal from past advice, new national health guidelines call for parents to give their children foods containing peanuts early and often, starting when they’re infants, as a way to help avoid life-threatening peanut allergies.
The new guidelines, issued by the National Institute of Allergy and Infectious Diseases on Thursday, recommend giving babies puréed food or finger food containing peanut powder or extract before they are 6 months old, and even earlier if a child is prone to allergies and doctors say it is safe to do so. One should never give a baby whole peanuts or peanut bits, experts say, because they can be a choking hazard.
If broadly implemented, the new guidelines have the potential to dramatically lower the number of children who develop one of the most common and lethal food allergies, said Dr. Anthony Fauci, the institute’s director, who called the new approach “game changing.”
Could the new guidelines mark the end of the peanut-butter-and-jelly sandwich bans so common in school lunchrooms? “If we can put this into practice over a period of several years, I would be surprised if we would not see a dramatic decrease in the incidence of peanut allergies,” Dr. Fauci said.
Peanut allergies are responsible for more deaths from anaphylaxis, or constriction of the airways, than any other food allergy. Though deaths are extremely rare, children who develop a peanut allergy generally do not outgrow it and must be vigilant to avoid peanuts for the rest of their lives.
Dr. Lack and fellow scientists tested the hypothesis in a large clinical trial in England. They recruited hundreds of infants aged 4 to 11 months, all of whom were deemed at high risk of developing a peanut allergy because they had eczema or an allergy to eggs. After running skin-prick tests on the babies and excluding those who were already allergic to peanuts, they randomly assigned some babies to be regularly fed peanut products, and others to be denied all peanut-containing foods.
By the time they turned 5, only 1.9 percent of 530 allergy-prone children who had been fed peanuts had developed an allergy, compared with 13.7 percent of the children who were denied peanuts. Among another group of 98 babies who were more sensitive to peanuts at the start of the study, 10 percent of those who were given peanuts developed an allergy, compared with 35 percent of those denied peanuts. The findings, published in The New England Journal of Medicine in 2015, “shook the foundation of the food allergy world,” Dr. Greenhawt said.
The new guidelines divide children by risk. Low-risk infants, who don’t have eczema or an egg allergy and who have started solid foods, can be introduced to peanut-containing foods around 6 months at home by their parents. So can moderate risk children, who have mild eczema.
High-risk infants, who have severe eczema or an egg allergy, should be introduced to peanut-containing foods as early as 4 to 6 months, after they start other solid foods and are evaluated by a doctor for safety.
If your baby is determined to be high-risk, the guidelines recommend an evaluation by an allergy specialist, who may order allergy testing and introduce a peanut food in the doctor’s office, Dr. Greenhawt said. Even if allergy tests show sensitivity to peanuts, the baby isn’t necessarily allergic and may benefit from eating peanut foods, he said. A baby with a stronger reaction to the skin test may already be allergic, however, and the doctor may decide to recommend complete avoidance.
One way to introduce your baby to peanuts safely is to mix a couple of teaspoons of smooth peanut butter with a couple of teaspoons of warm water and stir until it has a smooth soupy or purée-like consistency, suggested Dr. J. Andrew Bird, pediatric allergist with UT Southwestern Medical Center and Children’s Medical Center in Dallas, who wrote a paper on the subject.
Foods containing peanuts should not be the first solid a baby eats, Dr. Greenhawt said. It’s also important to continue feeding the peanut-containing food regularly, aiming for three times a week, through childhood.
He acknowledged the new recommendations may face resistance. “The nuts and bolts of getting everyone to buy in to this and trust the recommendation and the data is a big unknown,” Dr. Greenhawt said. But the potential, he says, is enormous.
“This won’t outright prevent every single case of peanut allergy – there will still be some cases – but the number could be significantly reduced by tens of thousands,” Dr. Greenhawt said. “In the best case scenario, every allergist across the U.S. could be seeing fewer cases of peanut allergy — and that’s a good problem to have.”
The post Reversal On Peanut Allergy appeared first on Reach Out Recovery.