Jeffrey Dach's Blog, page 20
December 25, 2016
Statin Choir Boy Turns Disbeliever
 Statin Choir Boy Turns Disbeliever
Statin Choir Boy Turns Disbelieverby Jeffrey Dach MD
For many years, Stephen Sinatra believed in statin drugs and prescribed them as a cardiologist in Connecticut. He gave lectures to other cardiologists on the merits of statin drugs at medical meetings on behalf of the drug companies. However, after a time, he became disillusioned and was transformed from a “Statin Choirboy” to a “Statin Disbeliever”.
Dr. Stephen Sinatra’s Observations:
1) many patients with low cholesterol will go on to develop heart disease.
2) In many patients with cholesterol above 280, angiograms show normal coronary arteries. They don’t have heart disease.
3) Population studies discredit cholesterol. For example, the French have the highest cholesterol levels in Europe of 250, and they also have lowest incidence of heart disease. On the Greek Island of Crete, average cholesterol is well over 200, yet there was not a single heart attack there in ten years.
4) Half of all heart attacks occur in people with normal total cholesterol.
Cholesterol and statins
 A Vending Machine for Statin Drugs?
A Vending Machine for Statin Drugs?
I refer you to Dr. Stephen Sinatra’s excellent article in the Townsend Letter in which he remarks that drug companies Merck and Pfizer have transformed the medical profession into one big vending machine for statin drugs.(4)
The Old Lipid Panel is Obsolete
Dr. Stephen Sinatra also tells us that the old Cholesterol blood test ordered by your primary care doctor is now obsolete, and has been replaced by the more sophisticated lipoprotein panel, providing a wealth of more information. What is this added information? In addition, the Calcium Score is more sensitive and accurate test than serum cholesterol for determining heart disease risk.
LDL Particles – Not All Sizes are Equal
Firstly, the new test provides LDL particle size. Small LDL particle size is the dangerous one associated with increased risk of heart disease. Large buoyant LDL particle size is the safe one, with less heart disease risk. Secondly the Lipoprotein profile includes Lipoprotein (a), a marker of high risk for heart disease risk.
[image error]
Left Above Image: LDL particle with cholesterol ester in the center (yellow arrow) surrounded by phospholipid outer coating (white arrow).. APO-B Protein at top (red arrow)
Significance of Total Cholesterol
Steven Sinatra says total cholesterol doesn’t mean much unless you have a level over 320 which increases risk of stroke. Reducing cholesterol can be accomplished with weight reduction and increasing dietary fiber. Dr Sinatra would not prescribe a statin drug unless you are a male with documented heart disease.
Low LDL?
Dr. Sinatra says that low LDL below 80 is associated with adverse side adverse side effects of cancer, aggression, cerebral bleeding, amnesia, and immune dysfunction.
Just Don’t Do It
Below you will find Steven Sinatra’s advice if your doctor tells you to take statin based on the standard cholesterol panel:
1) Don’t do it. Ask for a Lipo-protein Subfraction Test such as the NMR LipoPorfile (LabCorp) or Cardio-IQ (Quest)
2) If you are a 50-75 year old male with small dense LDL, then go for the statin drug. It’s a good idea. If you are over 75, don’t take a statin drug as the drugs cause increased mortality in the elderly.
3) If you are a woman, avoid statins, as no statin drug study has ever shown a benefit in all-cause mortality for women by lowering cholesterol, and adverse effects of the drugs are horrendous.
4) If you have elevated lipoprotein (a), do not take a statin. The drugs don’t work for this. Instead use Niacin (B3) 500-2000 mg per day, Fish oil 2-3 grams per day, and Nattokinase 100 mg per day.
The Greatest Scientific Deception of the Century
Data from the Framingham Study was the basis for the cholesterol theory of heart disease, the theory that elevated cholesterol levels causes heart disease, and reducing cholesterol levels with diet or drugs prevented heart disease. A Biochemist and participant in the Framingham study, George V. Mann, later said in his memoirs,
” Saturated fat and cholesterol in the diet are not the causes of coronary heart disease. That myth is the greatest scientific deception of this century, perhaps of any century.”(7,8)
I Stopped My Statin Drug – Now What ?
What replaces the statin drugs once patients gets off? What lifestyle modifications and nutritional supplements are used to prevent or reverse heart disease? There is an entire program devoted to this called is the Track Your Plaque Program devised by William Davis MD, a Wisconsin cardiologist .
William Davis MD Warns About the Evil Trio
 If total cholesterol is not useful as a predictor of heart disease risk, what is? Which lipoprotein markers are the ones to look for? Davis tells us the lipoprotein profile sometimes reveals an evil trio of abnormalities strongly predictive of heart disease, often leading to advanced heart disease at an early age.(6)
If total cholesterol is not useful as a predictor of heart disease risk, what is? Which lipoprotein markers are the ones to look for? Davis tells us the lipoprotein profile sometimes reveals an evil trio of abnormalities strongly predictive of heart disease, often leading to advanced heart disease at an early age.(6)
Here is the evil trio:
1) Low HDL–generally less than 50 mg/dl.
2) Small Particle Size LDL–especially if 50% or more of total LDL.
3) Lipoprotein(a)–an aggressive risk factor by itself.
If you have the evil trio, rather than robotically prescribe a statin drug, Davis recommends lifestyle modification and dietary supplements. Davis remarks that some of his greatest heart disease reversals have been in patient with this evil trio, which responds well to the regimen listed below. Reversal of Heart disease is determined by reduction in coronary calcium score (or less of an increase).
Here is Dr Davis’ program for Reversing Heart Disease and the Evil Trio
1) Niacin–increases HDL, reduces small LDL, and reduces Lp(a)
2) Elimination of wheat, cornstarch, and sugars–Best for reducing small LDL; less potent for Lp(a) reduction.
3) High-fat intake–Like niacin, effective for all three.
4) High-dose fish oil–Higher doses of EPA + DHA 3000 mg per day.
Here are a cases from the office of people on statins that I see very day. Statin Case Reports From the Office:
Number One – Chronic Psoriatic Rash from Statins:
Dan is about 65 with no history of heart disease and has been on a statin drug for a cholesterol of 220 about two years. His major problem is a red raised rash on his forearms, and hands and forehead which looks a lot like psoriasis, present for about 2 years. Dermatologists have been stumped and of no help.
Dan’s Lipoprotein Profile show large buoyant LDL particles indicating low risk for heart disease. His coronary calcium score was 75th per centile indicating only mildly above average risk of heart disease (50% per centile is average risk).
I told Dan that the rash was most likely a reaction to the statin anti-cholesterol drug, and advised a two week trial off the drug to see if the rash resolves. Three weeks later Dan returns to the office, and reports the skin rash is gone.
Number Two- Lupus-like Skin Lesion from Statins
Sarah is an 82 year old with no history of heart disease and on a statin drug for a cholesterol of 235. She had been to the dermatologist because of skin lesions on her face near the temple areas which were biopsied and reported by the pathologist as inflammation in the skin suggestive of lupus erythematosis. Sarah is concerned she has Lupus and cam to see me for a second opinion. I told Sarah she did not have Lupus and advised her that the skin eruptions were a reaction to the statin drug. Sarah stopped the statin drug and three weeks later reported the skin had returned to normal.
Number Three- Early Alzheimer’s from Statins
Lori is a 52 year old post menopausal with chief complaint of memory loss, cognitive dysfunction and severe fatigue. She had no history of heart disease and been on a statin drug for many years for a cholesterol of 230. I advised her to stop the statin drug. However, her cognitive dysfunction and memory loss continued unchanged. She was unable to find the office for a follow up visit, gave up and drove home.
A study by Muldoon showed virtual 100% of patients on statin drugs have some element of cognitive impairment, ranging from mild to severe symptoms of amnesia and cognitive dysfunction. (5) I have found this to be the case in actual clinical practice.
Number Four- Wheelchair bound non-healing deep infections from statins
Jim is a war veteran and was paralyzed from a roadside bomb many years ago, and has since been wheelchair bound. Although there is no history of heart disease, his doctor placed him on a statin drug for a cholesterol of 245 about two years ago. Shortly thereafter, Jim developed non-healing chronic decubitus infections at the ischial tuberosities at the site of pressure sitting in the wheelchair. Jim has had numerous surgical procedure and drainages, debridements, and multiple courses of antibiotics for these chronic infections which refuse to heal. In this case, the statin drug prevents healing of chronic infection. Jim stopped the statin drug, began an intensive nutritional program to boost immunity and healing ability and reported improvement after 6 weeks.
Credit and Thanks to Stephen Sinatra MD and William Davis MD for most of the information in this article.
Articles with Related Interest:
Reducing Calcium Score with Aged Garlic
Cholesterol Lowering Statin Drugs for Women, Just Say No
CAT Coronary Calcium Scoring, Reversing Heart Disease
Cholesterol Lowering Drugs for the Elderly, Bad Idea
Heart Disease, Ascorbate, Lysine and Linus Pauling
Saving Tim Russert and George Carlin
Lipitor and The Dracula of Modern Technology
Reversing Coronary Calcium Score
Jeffrey Dach MD
7450 Griffin Road Suite 190
Davie Florida 33314
954-792-4663
http://www.drdach.com/
http://www.naturalmedicine101.com/
http://www.truemedmd.com/
Links and References:
(1) http://www.spacedoc.net/stephen_sinatra_1
Dr. Stephen Sinatra – From Cholesterol Choirboy to Non-Believer
(2) http://www.spacedoc.net/stephen_sinatra_2
Dr. Stephen Sinatra – How to Determine if You Really Need a Statin
(3) http://www.spacedoc.net/stephen_sinatra_3
Dr. Stephen Sinatra – Statins, CoQ10, and Carnitine
If we have to prescribe a statin we always make sure the patient takes an ample amount of supplemental CoQ10 – at least 100 mg daily and taken with a meal.
4) Townsend Letter, Clearing Up the Cholesterol Confusion by Steven Sinatra, MD A well-known cardiologist explains why he doesn’t think lowering cholesterol is the answer for preventing heart disease, and debunks the routine prescription of statins for all but specific cases.
5) http://www.ncbi.nlm.nih.gov/pubmed/10806282
Am J Med. 2000 May;108(7):538-46.>
Effects of lovastatin on cognitive function and psychological well-being. Muldoon MF, Barger SD, Ryan CM, Flory JD, Lehoczky JP, Matthews KA, Manuck SB. Center for Clinical Pharmacology (MFM), University of Pittsburgh School of Medicine, Pittsburgh, Pennsylvania, USA.
CONCLUSION: Treatment of hypercholesterolemia with lovastatin did result in small performance decrements on neuropsychological tests of attention and psychomotor speed.
(6) http://heartscanblog.blogspot.com/2009/05/lethal-lipids.html
Lethal lipids-Heart Scan Blog William Davis MD
There’s a specific combination of lipids/lipoproteins that confers especially high risk for heart disease. That combination is:
Low HDL–generally less than 50 mg/dl
Small LDL–especially if 50% or more of total LDL
Lipoprotein(a)–an aggressive risk factor by itself
Total Cholesterol and Heart Disease
Dr Malcolm Kendrick (MbChB MRCGP) MD qualified in Aberdeen Scotland. He has worked in family practice for almost twenty years, and learned that treating patients is not like treating textbooks. He has specialized in heart disease and set up the on-line educational website for the European Society of Cardiology.
Disclaimer click here: www.drdach.com/wst_page20.html
The reader is advised to discuss the comments on these pages with
his/her personal physicians and to only act upon the advice of his/her personal physician. Also note that concerning an answer which appears as an electronically posted question, I am NOT creating a physician — patient relationship. Although identities will remain confidential as much as possible, as I can not control the media, I can not take responsibility for any breaches of confidentiality that may occur.
7) http://www.nejm.org/doi/pdf/10.1056/N...
Mann, George V. “Diet-heart: end of an era.” New England Journal of Medicine 297.12 (1977): 644-650.
8) http://www.epi.umn.edu/cvdepi/essay/i...
Heart Attack Prevention A History of Cardiovascular Disease Epidemiology U of Minnesota
“It Isn’t Always Fun.” – A Mann Apart A Biographical Story
Saturated fat and cholesterol in the diet are not the causes of coronary heart disease. That myth is the greatest scientific deception of this century, perhaps of any century.
Link to this article:http://wp.me/p3gFbV-4hr
Jeffrey Dach MD
7450 Griffin Road Suite 190
Davie, Florida 33314
954-792-4663
http://www.drdach.com/
http://www.naturalmedicine101.com/
http://www.truemedmd.com/
http://www.bioidenticalhormones101.com/
Disclaimer click here: http://www.drdach.com/wst_page20.html
The reader is advised to discuss the comments on these pages with his/her personal physicians and to only act upon the advice of his/her personal physician. Also note that concerning an answer which appears as an electronically posted question, I am NOT creating a physician — patient relationship.
Although identities will remain confidential as much as possible, as I can not control the media, I can not take responsibility for any breaches of confidentiality that may occur.
Copyright (c) 2014 Jeffrey Dach MD All Rights Reserved
This article may be reproduced on the internet without permission, provided there is a link to this page and proper credit is given.
FAIR USE NOTICE: This site contains copyrighted material the use of which has not always been specifically authorized by the copyright owner. We are making such material available in our efforts to advance understanding of issues of significance. We believe this constitutes a ‘fair use’ of any such copyrighted material as provided for in section 107 of the US Copyright Law. In accordance with Title 17 U.S.C. Section 107, the material on this site is distributed without profit to those who have expressed a prior interest in receiving the included information for research and educational purposes.
Serving Areas of: Hollywood, Aventura, Miami, Fort Lauderdale, Pembroke Pines, Miramar, Davie, Coral Springs, Cooper City, Sunshine Ranches, Hallandale, Surfside, Miami Beach, Sunny Isles, Normandy Isles, Coral Gables, Hialeah, Golden Beach ,Kendall,sunrise, coral springs, parkland,pompano, boca raton, palm beach, weston, dania beach, tamarac, oakland park, boynton beach, delray,lake worth,wellington,plantation
December 23, 2016
Statins Reduce Peri-Operative Mortality Surely You Must Be Joking
[image error] Statins Reduce Peri-Operative Mortality, Surely You Must Be Joking
Another Medical Hoax
I was intrigued by Dr London’s report in December 2016 JAMA of decreased peri-operative mortality in statin users.(1) This result does not seem immediately intuitive. Statin drugs inhibit an enzyme in the liver called HMG-CoA reductase involved in cholesterol production, thereby reducing cholesterol levels. Left Image: Surgeons by Reginald Brill 1934 courtesy of Wikimedia Commons.
Higher Cholesterol is Protective of Post Operative Sepsis
Higher cholesterol in the surgical patient is protective of endotoxemia, a dreaded complication of non-cardiac surgery which carries a high mortality rate. According to Dr Wilson writing in Critical Care 2003, ” lipoproteins can bind and neutralize lipopolysaccharide, hypocholesterolemia can negatively impact outcome.” (2)
Severly ILL Patients Have Low Cholesterol
Another observation made by Dr Wilson is that severely ill patients tend to have low cholesterol. If so, then these severely ill patients would not be good candidates for statin drugs in the days prior to their surgical procedure as their cholesterol levels are already low. No need to give a drug to make it lower. On the other hand non-critically ill patients tend to have higher cholesterol values which does make them good candidates for a statin drug.
The Cholesterol Endotoxin Hypothesis
This explains the spurious findings of the JAMA article. The patients not taking statins were sicker with lower cholesterol values, a marker for increased mortality from sepsis.
Conclusion:
Low cholesterol is an excellent marker for increased mortality from sepsis. (3-7) Therefore driving down serum cholesterol with a statin drug is not a way to reduce surgical complications, most of which are related to post op sepsis. This Study in JAMA by Dr London is therefore a medical hoax, a result of patient selection bias, not due to any imaginary benefits of statin drugs, which are non-existent.
The damage of this JAMA article could produce is frightening, since some surgeons may actually believe it and give their patients statin drugs. This would be a catastrophe of monumental proportions.
Jeffrey Dach MD
Articles with Related Interest:
Low Level Endotoxemia and Cholesterol
Jeffrey Dach MD
Links and References:
1) Association of Perioperative Statin Use With Mortality and Morbidity After Major Noncardiac Surgery. Martin J London, JAMA Dec 19 2016.
Question Is exposure to a statin in the early perioperative period associated with reduced postoperative complications after noncardiac surgery?
Findings This observational cohort analysis of veterans linked risk and outcome data from the Veterans Affairs Surgical Quality Improvement Program database to statin prescriptions in 180 478 patients and evaluated the associations of early statin exposure on 30-day mortality. After adjustment for risk, other medications used, and potential selection biases, 30-day mortality was significantly reduced in the statin-exposed group.
Meaning Perioperative statin use may be beneficial in reducing 30-day mortality, although the effects of selection biases cannot be excluded.
Abstract
Importance The efficacy of statins in reducing perioperative cardiovascular and other organ system complications in patients undergoing noncardiac surgery remains controversial. Owing to a paucity of randomized clinical trials, analyses of large databases may facilitate informed hypothesis generation and more efficient trial design.
Objective To evaluate associations of early perioperative statin use with outcomes in a national cohort of veterans undergoing noncardiac surgery.
Design, Setting, and Participants This retrospective, observational cohort analysis included 180 478 veterans undergoing elective or emergent noncardiac surgery (including vascular, general, neurosurgery, orthopedic, thoracic, urologic, and otolaryngologic) who were admitted within 7 days of surgery and sampled by the Veterans Affairs Surgical Quality Improvement Program (VASQIP). Patients were admitted to Department of Veterans Affairs hospitals and underwent 30-day postoperative follow-up. Data were collected from October 1, 2005, to September 30, 2010, and analyzed from November 28, 2013, to October 31, 2016.
Exposure Statin use on the day of or the day after surgery.
Main Outcomes and Measures All-cause 30-day mortality (primary outcome) and standardized 30-day cardiovascular and noncardiovascular outcomes captured by VASQIP. Use of statins and other perioperative cardiovascular medications was ascertained from the Veterans Affairs Pharmacy Benefits Management research database.
Results A total of 180 478 eligible patients (95.6% men and 4.4% women; mean [SD] age, 63.8 [11.6] years) underwent analysis, and 96 486 were included in the propensity score–matched cohort (96.3% men; 3.7% women; mean [SD] age, 65.9 [10.6] years). At the time of hospital admission, 37.8% of patients had an active outpatient prescription for a statin, of whom 80.8% were prescribed simvastatin and 59.5% used moderate-intensity dosing. Exposure to a statin on the day of or the day after surgery based on an inpatient prescription was noted in 31.5% of the cohort. Among 48 243 propensity score–matched pairs of early perioperative statin-exposed and nonexposed patients, 30-day all-cause mortality was significantly reduced in exposed patients (relative risk, 0.82; 95% CI, 0.75-0.89; P
Conclusions and Relevance: Early perioperative exposure to a statin was associated with a significant reduction in all-cause perioperative mortality and several cardiovascular and noncardiovascular complications. However, the potential for selection biases in these results must be considered.
2) Wilson, Robert F., Jeffrey F. Barletta, and James G. Tyburski. “Hypocholesterolemia in sepsis and critically ill or injured patients.” Critical Care 7.6 (2003): 1.
3) Leardi, S., et al. “[Blood levels of cholesterol and postoperative septic complications].” Annali italiani di chirurgia 71.2 (1999): 233-237.
Hypocholesterolemia seems to represent a significant predictive factor of morbidity and mortality in critically ill patients. The authors, on the basis of recent literature data, aim to clarify the possible correlation between preoperative hypocholesterolemia and the risk of septic postoperative complications .205 patients undergoing to surgery for gastrointestinal diseases were the object of the study. Patients undergoing “minor” abdominal surgery or video-laparoscopic surgery and classified ASA III-IV were excluded. In all the patients, we considered retrospectively risk factors for postoperative septic complications as follows: preoperative blood concentration of cholesterol, malnutrition, obesity, diabetes, neoplasm, preoperative sepsis, type and duration of operations, antibiotics and regimen of use. Type and incidence of postoperative local or systemic septic complications were recorded. The patients have been stratified according to blood concentration of cholesterol and to the presence or absence of other risk factors. The incidence of postoperative sepsis was 35.1%. The highest incidence of postoperative septic complications (72.7%) was encountered, significantly (X2 = 7.6, p < 0.001), in the patients (11 cases, 5.9%) with cholesterol levels below 105 mg/dl). The results of this study seems to indicate a significant relationship between preoperative hypocholesterolemia and the incidence of septic complications after surgery. Moreover, evaluation of blood cholesterol levels before major surgery might represent a predictive factor of septic risk in the postoperative period.
4) Marik, Paul E. “Dyslipidemia in the critically ill.” Critical care clinics 22.1 (2006): 151-159. Total and HDL cholesterol levels fall at the onset of acute illness and the cholesterol levels normalize as the patient recovers. Hypocholesterolemia may predispose the critically ill patient to sepsis and adrenal failure. Early enteral nutrition and tight glycemic control accelerate the recovery of the cholesterol levels.
5) Chiarla, Carlo, et al. “Severe hypocholesterolemia in surgical patients, sepsis, and critical illness.” Journal of critical care 25.2 (2010): 361-e7.
After surgery, in sepsis and various critical illnesses, factors such as severity of the acute phase response, liver dysfunction, and hemodilution from blood loss have cumulative impacts in decreasing cholesterol; therefore, degree of hypocholesterolemia often reflects severity of illness. The direct correlation between cholesterol and several plasma proteins is mediated by the parallel impact of commonly shared determinants. Cholestasis is associated with a moderation of the degree of hypocholesterolemia. In human sepsis, the poor implications of hypocholesterolemia seem to be aggravated by the simultaneous development of hypertriglyceridemia. Cholesterol and triglyceride levels reflect altered lipoprotein patterns, and the issue is too complex and too poorly understood to be reduced to simple concepts; nevertheless, these simple measurements often represent helpful adjunctive clinical tools.
6) Biller, Katharina, et al. “Cholesterol rather than procalcitonin or C-reactive protein predicts mortality in patients with infection.” Shock 42.2 (2014): 129-132.
Serum cholesterol procalcitonin (PCT) and C-reactive protein (CRP) levels were measured consecutively in 76 critically ill patients at admission to the intensive care unit. The presence of infection was defined according to the CDC (Centers for Disease Control and Prevention) criteria; in-house mortality, underlying diseases, and severity of sepsis were monitored. Nonsurvivors had significantly lower cholesterol levels compared with survivors (69 mg/dL [range, 37-88 mg/dL] vs. 96 mg/dL [range, 71-132 mg/dL], P = 0.006) whereas no significant differences were noted for serum PCT and CRP levels. In a cohort of patients with cholesterol levels of 50 mg/dL or less, 82% did not survive as compared with patients with cholesterol levels of 100 mg/dL or greater (mortality, 21%). In a control group without infection, no difference of cholesterol, PCT, or CRP was found between survivors and nonsurvivors. Our data show that low cholesterol levels in patients with infectious disease have a prognostic value and may be useful markers to identify high-risk patients already at admission.
7) free pdf Thomas Whitney Serum cholesterol Superior Prognostic Marker Sepsis Mortality in ICU 2015 Thomas, Whitney. “Serum cholesterol: A Superior Prognostic Marker of Sepsis Mortality in the ICU Compared to Procalcitonin or C-reactive Protein.” (2015).
Total cholesterol may be a useful and superior prognostic marker of mortality for patients admitted to the ICU with sepsis secondary to infection compared to its CRP and PCT counterparts. Serum cholesterol could provide ICU clinicians a more sensitive screening tool for identifying those patients at highest risk for morbidity and mortality irrespective of other underlying comorbidities, whereas CRP may be more useful for monitoring response to therapy. Cholesterol pathophysiology may also yield insight on experimental therapy including the use of statin medications in septic patients in the ICU.
8) Sandek A., Utchill S, Rauchhaus M. The endotoxin-lipoprotein hypothesis-an update. Arch Med Sci. 2007;3(4A):S81. The endotoxin lipoprotein hypothesis Anja Sandek 2007
9) Pajkrt D, Doran JE, Koster F, et al. Antiinflammatory effects of reconstituted high-density lipoprotein during human endotoxemia. J Exp Med. 1996;184(5):1601-8.
10) Vreugdenhil AC, Rousseau CH, Hartung T, et al. Lipopolysaccharide (LPS)-binding protein mediates LPS detoxification by chylomicrons. J Immunol. 2003;170(3):1399-405.
11) Statin Drugs Tied to Better Surgery Outcomes By NICHOLAS BAKALARDEC. 21, 2016
12) Shock. 2016 Jan;45(1):10-5. Incidence of Sepsis and Mortality With Prior Exposure of HMG-COA Reductase Inhibitors in a Surgical Intensive Care Population.
Schurr JW1, Wu W, Smith-Hannah A, Smith CJ, Barrera R.
1*Department of Pharmacy Services, Brigham and Women’s Hospital, Boston, Massachusetts †St John’s University College of Pharmacy and Health Sciences, Queens, New York ‡Department of Surgery, North Shore-LIJ Health System Long Island Jewish Medical Center, New Hyde Park, New York.
The anti-inflammatory properties of hydroxymethylglutaryl coenzyme A (HMG-CoA) reductase inhibitors (statins) may reduce the risk of developing sepsis in surgical intensive care patients and improve outcomes in those who do become septic. The objective of this study was to assess whether surgical intensive care unit (SICU) patients with prior exposure to HMG-CoA reductase inhibitors had a lower incidence of developing sepsis and improved outcomes. A retrospective cohort study was conducted. Patient demographic data, statin use, sequential organ failure assessment (SOFA) scores, vasopressor requirements, ventilator days, length of SICU stay, and mortality in septic patients were collected. Incidence of development of sepsis was determined using systemic inflammatory response syndrome criteria. Patients were grouped into cohorts based on whether they met the sepsis criteria and if they had previously received statins. Cohorts of patients who did and did not become septic with prior statin exposure were compared and an odds ratio was calculated to determine a protective effect. The setting was a SICU. The study comprised of 455 SICU patients and had no interventions. Among the 455 SICU patients, 427 patients were included for the final results. Patients receiving statins verses not receiving statins were similar in demographics. Previous statin exposure had a protective effect in the development of sepsis (9.77% on statins vs. 33.6% without statins; odds ratio 0.203, confidence interval 0.118-0.351). Of those patients who developed sepsis, there was a statistically significant decrease in 28-day mortality in patients with prior statin exposure (P = 0.0341). No statistical difference was noted in length of stay, vasopressor requirements, or days on mechanical ventilation. Prior exposure to statins may have a protective effect on the development of sepsis and decrease mortality in critically ill surgical patients.
13) McAuley, Danny, Pierre-Emmanuel Charles, and Laurent Papazian. “Statins in patients with sepsis and ARDS: is it over? We are not sure.” (2016): 1-3.
link to this article: http://wp.me/p3gFbV-4gE
Jeffrey Dach MD
7450 Griffin Road Suite 190
Davie, Fl 33314
954-792-4663
www.jeffreydachmd.com
http://www.drdach.com
http://www.naturalmedicine101.com
http://www.truemedmd.com
Disclaimer click here: http://www.drdach.com/wst_page20.html
The reader is advised to discuss the comments on these pages with his/her personal physicians and to only act upon the advice of his/her personal physician. Also note that concerning an answer which appears as an electronically posted question, I am NOT creating a physician — patient relationship. Although identities will remain confidential as much as possible, as I can not control the media, I can not take responsibility for any breaches of confidentiality that may occur.
Copyright (c) 2016-2017 Jeffrey Dach MD All Rights Reserved. This article may be reproduced on the internet without permission, provided there is a link to this page and proper credit is given.
FAIR USE NOTICE: This site contains copyrighted material the use of which has not always been specifically authorized by the copyright owner. We are making such material available in our efforts to advance understanding of issues of significance. We believe this constitutes a ‘fair use’ of any such copyrighted material as provided for in section 107 of the US Copyright Law. In accordance with Title 17 U.S.C. Section 107, the material on this site is distributed without profit to those who have expressed a prior interest in receiving the included information for research and educational purposes.
Serving Areas of: Hollywood, Aventura, Miami, Fort Lauderdale, Pembroke Pines, Miramar, Davie, Coral Springs, Cooper City, Sunshine Ranches, Hallandale, Surfside, Miami Beach, Sunny Isles, Normandy Isles, Coral Gables, Hialeah, Golden Beach ,Kendall,sunrise, coral springs, parkland,pompano, boca raton, palm beach, weston, dania beach, tamarac, oakland park, boynton beach, delray,lake worth,wellington,plantation.
The post Statins Reduce Peri-Operative Mortality Surely You Must Be Joking appeared first on Jeffrey Dach MD .
December 20, 2016
Testosterone Therapy Prolongs Life and Improves Survival
 Testosterone Therapy Prolongs Life and Improves Survival
Testosterone Therapy Prolongs Life and Improves Survival
by Jeffrey Dach MD
Unfounded Fears
More recently, in the past few years a flurry of articles and studies have come to light by Drs Traish and Morgentaler debunking the two unfounded fears regarding testosterone therapy in androgen deficient males.(7-13)
The first unfounded fear is the false medical myth that testosterone therapy somehow causes prostate cancer. This has been shown to be false.(7,8)
The second unfounded fear is that testosterone somehow increases cardiovascular disease. Not only is this false, the exact opposite is true. Testosterone therapy in androgen deficient males decreases cardiovascular mortality in numerous studies.(7,8) Indeed, Dr Traish makes the plea to the medical community to treat more androgen deficient men.(7,8) He says” “There is an urgent need among the medical community for greater awareness of the impact of TD on general health in men with TD.” (7,8)
Testosterone Treated Group Shows Improved Survival
 Left image shows mortality rate In Diabetic Males with Normal or Low testosterone. Note the increased mortality in Low Testosterone untreated group. Mortality rate of androgen deficient group returns to Normal after testosterone treatment.(13)
Left image shows mortality rate In Diabetic Males with Normal or Low testosterone. Note the increased mortality in Low Testosterone untreated group. Mortality rate of androgen deficient group returns to Normal after testosterone treatment.(13)
Above Left image courtesy of Muraleedharan, Vakkat, et al. “Testosterone deficiency is associated with increased risk of mortality and testosterone replacement improves survival in men with type 2 diabetes.” European Journal of Endocrinology 169.6 (2013): 725-733.
Conclusion: Low testosterone in males is associated with loss of libido, depression. metabolic syndrome , increased coronary artery disease and increased mortality. (4,5,7-13) These are all prevented or reversed by testosterone therapy. The great tragedy of modern medicine is that many androgen deficient males are either ignored or denied treatment. Hopefully this will soon be rectified. Our mission at TrueMedMD is to treat every androgen deficient male with testosterone therapy.
Related Articles:
Low Testosterone Increases Mortality
Testosterone Prevents Heart Attacks in Older Men
Low Testosterone – Diagnosis and Treatment
Does Testosterone Cause Prostate Cancer? by Jeffrey Dach MD
PSA Prostate Cancer and Testosterone Part Two
PSA Screening for Cancer, the Failed Medical Experiment by Jeffrey Dach MD
Jeffrey Dach MD
7450 Griffin Road Suite 190
Davie, Florida 33314
954-792-4663
http://www.drdach.com/
http://www.naturalmedicine101.com/
http://www.truemedmd.com/
http://www.bioidenticalhormones101.com/
Links and References
(1) http://www.ncbi.nlm.nih.gov/pubmed/16908801
Low Serum Testosterone and Mortality in Male Veterans Arch Intern Med. 2006;166:1660-1665 Molly M. Shores, MD; Alvin M. Matsumoto, MD; Kevin L. Sloan, MD; Daniel R. Kivlahan, PhD .Conclusions Low testosterone levels were associated with increased mortality in male veterans.
(2) http://jcem.endojournals.org/cgi/content/full/93/1/68http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2190742/
The Journal of Clinical Endocrinology & Metabolism 2008 Jan;93(1):68-75.
Low Serum Testosterone and Mortality in Older Men. Gail A. Laughlin, Eliza beth Barrett-Connor and Jaclyn Bergstrom. Department of Family and Preventive Medicine, School of Medicine, University of California, San Diego, La Jolla, California 92093
Results: During an average 11.8-yr follow-up, 538 deaths occurred. Men whose total testosterone levels were in the lowest quartile (
Conclusions: Testosterone insufficiency in older men is associated with increased risk of death over the following 20 yr, independent of multiple risk factors and several preexisting health conditions.
(3)http://abcnews.go.com/Health/ActiveAging/story?id=3247773&page=1&page=1
Low Testosterone Could Kill You. Low Levels of Male Hormone May be More Dangerous Than Previously Thought By SUPINDA BUNYAVANICH, M.D. ABC News Medical Unit June 6, 2007
Low testosterone may lead to a greater risk of death, according to a study presented Tuesday at the annual meeting of the Endocrine Society in Toronto.
Men with low testosterone had a 33 percent greater death risk over their next 18 years of life compared with men who had higher testosterone, according to the study conducted by Dr. Elizabeth Barrett-Connor and colleagues at the University of California at San Diego. “It’s very exciting and potentially a groundbreaking study,” said Barrett-Connor. “But it needs to be confirmed.” The study tracked nearly 800 men, 50 to 91 years old, living in California. Their testosterone level was measured at the beginning of the study, and their health was then tracked over the next 20 years.
4) http://www.medicalnewstoday.com/articles/153822.php
Testosterone Replacement For Men With Low Testosterone Improves Liver Function, Metabolic Syndrome. Testosterone deficiency, which becomes more common with age, is linked not only to decreased libido but also to a number of medical problems. These include the metabolic syndrome a cluster of metabolic risk factors that increase the chances of developing heart disease, stroke and type 2 diabetes.
5) http://www.news-medical.net/news/2008/03/04/35897.aspx
Low testosterone levels linked to depression in older men March 2008
Older men with lower free testosterone levels in their blood appear to have higher prevalence of depression, according to a report in the March issue of Archives of General Psychiatry.
6) Malkin, Chris J., et al. “Low serum testosterone and increased mortality in men with coronary heart disease.” Heart 96.22 (2010): 1821-1825. low-serum-testosterone-and-increased-mortality-in-men-with-coronary-heart-disease-malkin-chris-heart-2010 Background To examine the effect of serum testosterone levels on survival in a consecutive series of men with confirmed coronary disease and calculate the prevalence of testosterone deficiency.
Design Longitudinal follow-up study. Setting Tertiary referral cardiothoracic centre. Patients 930 consecutive men with coronary disease referred for diagnostic angiography recruited between June 2000 and June 2002 and followed up for a mean of 6.9±2.1 years.
Outcome All-cause mortality and vascular mortality. Prevalence of testosterone deficiency.
Results The overall prevalence of biochemical testosterone deficiency in the coronary disease cohort using bio-available testosterone (bio-T) Excess mortality was noted in the androgen-deficient group compared with normal (41 (21%) vs 88 (12%), p=0.002). The only parameters found to influence time to all-cause and vascular mortality (HR ± 95% CI) in multivariate analyses were the presence of left ventricular dysfunction (3.85; 1.72 to 8.33), aspirin therapy (0.63; 0.38 to 1.0), β-blocker therapy (0.45; 0.31 to 0.67) and low serum bio-T (2.27; 1.45 to 3.6).
Conclusions In patients with coronary disease testosterone deficiency is common and impacts significantly negatively on survival. Prospective trials of testosterone replacement are needed to assess the effect of treatment on survival.
!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!! 2016
7) Traish, Abdulmaged. “Testosterone therapy in men with testosterone deficiency: Are we beyond the point of no return?.” Investigative and Clinical Urology 57.6 (2016): 384-400.
Although testosterone therapy in men with testosterone deficiency was introduced in the early 1940s, utilization of this effective treatment approach in hypogonadal men is met with considerable skepticism and resistance. Indeed, for decades, the fear that testosterone may cause prostate cancer has hampered clinical progress in this field. Nevertheless, even after considerable knowledge was acquired that this fear is unsubstantiated, many in the medical community remain hesitant to utilize this therapeutic approach to treat men with hypogonadism. As the fears concerning prostate cancer have subsided, a new controversy regarding use of testosterone therapy and increase in cardiovascular disease was introduced. Although the new controversy was based on one ill-fated clinical trial, one meta-analysis with studies that utilized unapproved formulation in men with liver cirrhosis, and two retrospective studies with suspect or nonvalidated statistical methodologies and database contaminations, the flames of such controversy were fanned by the lay press and academics alike. In this review we discuss the adverse effect of testosterone deficiency and highlight the numerous proven benefits of testosterone therapy on men’s health and debunk the myth that testosterone therapy increases cardiovascular risk. Ultimately, we believe that there is considerable scientific and clinical evidence to suggest that testosterone therapy is safe and effective with restoration of physiological levels in men with testosterone deficiency, irrespective of its etiology.
TD is associated with increased incidence of metabolic syndrome, obesity, sexual dysfunction, impaired fertility, reduced motivation, increased fatigue, depressed mood, loss of bone and muscle mass, anemia, decreased energy and vigour, insulin resistance, diabetes, inflammation, dyslipidemia, sarcopenia and frailty, reduced quality of life (QoL) and increased mortality [1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 40, 41, 42, 43, 44]. A substantial body of evidence indicates that coronary artery disease incidence and severity, carotid intima-media thickness, atherosclerosis is inversely correlated with serum T concentrations [45]. There is an urgent need among the medical community for greater awareness of the impact of TD on general health in men with TD.
8) Traish, Abdulmaged M. “Testosterone therapy in men with testosterone deficiency: are the benefits and cardiovascular risks real or imagined?.” American Journal of Physiology-Regulatory, Integrative and Comparative Physiology. Vol. 311. No. 3. American Physiological Society, 2016.
In the adult male, testosterone (T) deficiency (TD) also known as male hypogonadism, is a well-established medical condition, which has been recognized for more than a century. T therapy in men with TD was introduced as early as 1940s and was reported to improve overall health with no concomitant serious adverse effects. A wealth of recent studies demonstrated that T therapy in men with TD is associated with increased lean body mass, reduced fat mass and waist circumference, improvement in glycemic control, and reduced obesity. T therapy is also associated with improvements in lipid profiles, amelioration of metabolic syndrome (Met S) components, reduced inflammatory biomarkers, reduced systolic and diastolic blood pressure, and improvements in sexual function. More importantly, T therapy is associated with amelioration of diabetes and reduced mortality. However, few studies, marred with serious methodological and analytical flaws reported between 2010 and 2014, suggested that T therapy is associated with increased cardiovascular (CV) risk. As summarized in this review, a thorough and critical analysis of these studies showed that the risks purported are unsubstantiated and such studies lacked credible scientific and clinical evidence. Moreover, recent observational, registry studies, clinical trials, and meta-analyses, all revealed no increase in CV risks in men receiving T therapy. In this review, the benefits of T therapy in adult men with TD and the lack of credible evidence suggesting that T therapy is linked to increased CV risks are discussed. It should be noted that the literature is replete with studies demonstrating beneficial effects of T therapy on CV and overall health.
Of importance, the study by Snyder et al. [3] and the resolutions of the consensus panel on T [2] debunked the notion that age-related hypogonadism is not a clinical condition and should remain untreated. As reported in the study [3], T therapy in older men has several benefits and age-related hypogonadism is a clinical condition worthy of treatment. We hope that the findings of this large and well executed study [3] and the summary provided by the consensus panel [2] will serve as a reminder to those who are beating the drums of fear and hysteria on the dangerous use of T in the treatment of men with TD and reassure men suffering from TD and their physicians that such fears and hysteria are unfounded.
9) free pdf Anderson Jeffrey testosterone replacement myocardial infarction low testosterone 2016 Anderson, Jeffrey L., et al. “Impact of testosterone replacement therapy on myocardial infarction, stroke, and death in men with low testosterone concentrations in an integrated health care system.” The American journal of cardiology 117.5 (2016): 794-799.
The aim of this study was to assess the effect of testosterone replacement therapy (TRT) on cardiovascular outcomes. Men (January 1, 1996, to December 31, 2011) with a low initial total testosterone concentration, a subsequent testosterone level, and >3 years of follow-up were studied. Levels were correlated with testosterone supplement use. The primary outcome was major adverse cardiovascular events (MACE), defined as a composite of death, nonfatal myocardial infarction, and stroke at 3 years. Multivariate adjusted hazard ratios (HRs) comparing groups of persistent low (742 ng/dl, n = 1,694) achieved testosterone were calculated by Cox hazard regression. A total of 4,736 men were studied. Three-year rates of MACE and death were 6.6% and 4.3%, respectively. Subjects supplemented to normal testosterone had reduced 3-year MACE (HR 0.74; 95% confidence interval [CI] 0.56 to 0.98, p = 0.04) compared to persistently low testosterone, driven primarily by death (HR 0.65, 95% CI 0.47 to 0.90). HRs for MI and stroke were 0.73 (95% CI 0.40 to 1.34), p = 0.32, and 1.11 (95% CI 0.54 to 2.28), p = 0.78, respectively. MACE was noninferior but not superior for high achieved testosterone with no benefit on MI and a trend to greater stroke risk. In conclusion, in a large general health care population, TRT to normal levels was associated with reduced MACE and death over 3 years but a stroke signal with high achieved levels suggests a conservative approach to TRT.
10) Saad, Farid, et al. “Testosterone Deficiency and Testosterone Treatment in Older Men.” Gerontology (2016).
Gerontology Testosterone Deficiency and Testosterone Treatment in Older Men Saad F.a, b · Röhrig G.c, d · von Haehling S.e · Traish A.f, g
aGlobal Medical Affairs Andrology, Bayer AG, Berlin, Germany;
Frailty is a clinical condition related to changes in metabolism, to sarcopenia, and to decline in muscle mass and strength, bone mineral density, and physical function with aging. The pathophysiology of frailty is multifactorial and associated with comorbidities. Testosterone is implicated in regulating metabolic functions, maintenance of muscle and bone, and inhibition of adipogenesis. In older individuals, reduced testosterone is thought to contribute to an altered state of metabolism, loss of muscle and bone, and increased fat, leading to sarcopenia, sarcopenic obesity, and frailty. While no direct relationship between testosterone deficiency (commonly known as hypogonadism) and frailty has been established (due to the multifactorial nature of frailty), clinical evidence suggests that testosterone deficiency is associated with increased sarcopenia and obesity. Testosterone treatment in frail older men with limited mobility and with testosterone deficiency improved insulin resistance, glucose metabolism, and body composition. These changes contribute to better physical function and improved quality of life. Because frailty increases disability, comorbidities, and the risk of hospitalization, institutionalization, and mortality in older men, it is warranted to explore the potential usefulness of testosterone treatment in frail men with hypogonadism in order to attenuate the progression of sarcopenia and frailty. In this paper, we will discuss the impact of testosterone deficiency on frailty and the potential role of testosterone treatment in ameliorating and reducing the progression of frailty. Such an approach may reduce disability and the risk of hospitalization and increase functional independence and quality of life.
11) free pdf Morgentaler Abraham Testosterone therapy and cardiovascular risk Mayo Clinic 2015
Morgentaler, Abraham, et al. “Testosterone therapy and cardiovascular risk: advances and controversies.” Mayo Clinic Proceedings. Vol. 90. No. 2. Elsevier, 2015.
a modest number of randomized controlled
trials (RCTs), indicate that low serum T concentrations
are associated with increased CV
risk and mortality and that T therapy may
have clinically relevant CV benefits
Established benefits of T therapy in hypogonadal
men include improved sexual desire
and function,12-15 improved energy, mood,
and vitality,15-19 increased lean mass,14,19-22
decreased waist circumference,23-27 reduced
total body fat mass,19-22 and increased bone
mineral density.28-31 Promising new data
reveal that T therapy improves insulin sensitivity32-
34 and reduces blood glucose23,25,35
and hemoglobin A1c (HbA1c)23,25,27,35 levels
in men with type 2 diabetes or obesity.
In summary, we find no scientific basis for
the suggestion that T therapy increases CV
risk. In fact, as of this date, we are unaware
of any compelling evidence that T therapy is
associated with increased CV risk. On the contrary,
the weight of evidence accumulated by
researchers around the world over several decades
clearly indicates that higher levels of T
are associated with amelioration of CV risk
factors and reduced risk of mortality.
12) Sharma, Rishi, et al. “Normalization of testosterone level is associated with reduced incidence of myocardial infarction and mortality in men.” European Heart Journal (2015): ehv346.
Aims There is a significant uncertainty regarding the effect of testosterone replacement therapy (TRT) on cardiovascular (CV) outcomes including myocardial infarction (MI) and stroke. The aim of this study was to examine the relationship between normalization of total testosterone (TT) after TRT and CV events as well as all-cause mortality in patients without previous history of MI and stroke.
Methods and results We retrospectively examined 83 010 male veterans with documented low TT levels. The subjects were categorized into (Gp1: TRT with resulting normalization of TT levels), (Gp2: TRT without normalization of TT levels) and (Gp3: Did not receive TRT). By utilizing propensity score-weighted Cox proportional hazard models, the association of TRT with all-cause mortality, MI, stroke, and a composite endpoint was compared between these groups. The all-cause mortality [hazard ratio (HR): 0.44, confidence interval (CI) 0.42–0.46], risk of MI (HR: 0.76, CI 0.63–0.93), and stroke (HR: 0.64, CI 0.43–0.96) were significantly lower in Gp1 (n = 43 931, median age = 66 years, mean follow-up = 6.2 years) vs. Gp3 (n = 13 378, median age = 66 years, mean follow-up = 4.7 years) in propensity-matched cohort. Similarly, the all-cause mortality (HR: 0.53, CI 0.50–0.55), risk of MI (HR: 0.82, CI 0.71–0.95), and stroke (HR: 0.70, CI 0.51–0.96) were significantly lower in Gp1 vs. Gp2 (n = 25 701, median age = 66 years, mean follow-up = 4.6 years). There was no difference in MI or stroke risk between Gp2 and Gp3.
Conclusion In this large observational cohort with extended follow-up, normalization of TT levels after TRT was associated with a significant reduction in all-cause mortality, MI, and stroke.
13) Muraleedharan, Vakkat, et al. “Testosterone deficiency is associated with increased risk of mortality and testosterone replacement improves survival in men with type 2 diabetes.” European Journal of Endocrinology 169.6 (2013): 725-733.
Objective Men with type 2 diabetes are known to have a high prevalence of testosterone deficiency. No long-term data are available regarding testosterone and mortality in men with type 2 diabetes or any effect of testosterone replacement therapy (TRT). We report a 6-year follow-up study to examine the effect of baseline testosterone and TRT on all-cause mortality in men with type 2 diabetes and low testosterone.
Research design and methods A total of 581 men with type 2 diabetes who had testosterone levels performed between 2002 and 2005 were followed up for a mean period of 5.8±1.3 s.d. years. Mortality rates were compared between total testosterone >10.4 nmol/l (300 ng/dl; n=343) and testosterone ≤10.4 nmol/l (n=238). The effect of TRT (as per normal clinical practise: 85.9% testosterone gel and 14.1% intramuscular testosterone undecanoate) was assessed retrospectively within the low testosterone group.
Results Mortality was increased in the low testosterone group (17.2%) compared with the normal testosterone group (9%; P=0.003) when controlled for covariates. In the Cox regression model, multivariate-adjusted hazard ratio (HR) for decreased survival was 2.02 (P=0.009, 95% CI 1.2–3.4). TRT (mean duration 41.6±20.7 months; n=64) was associated with a reduced mortality of 8.4% compared with 19.2% (P=0.002) in the untreated group (n=174). The multivariate-adjusted HR for decreased survival in the untreated group was 2.3 (95% CI 1.3–3.9, P=0.004).
Conclusions Low testosterone levels predict an increase in all-cause mortality during long-term follow-up. Testosterone replacement may improve survival in hypogonadal men with type 2 diabetes.
Several longitudinal population studies have reported that a low testosterone at baseline is associated with an increase in all-cause mortality (1). Some individual studies have specifically identified increases in cardiovascular, respiratory and cancer deaths (2, 3, 4). A meta-analysis of published research papers with a mean follow-up period of 9.7 years confirmed that low testosterone was associated with increased risk of all-cause and cardiovascular mortality in community based studies (1). Men with specific co-morbidities such as proven coronary artery disease and renal failure have also found that low testosterone predicts an increased risk of earlier death than those with the same condition and are testosterone replete (5, 6).
In summary, this is the first study to demonstrate that low testosterone levels are associated with an increase in all-cause and cardiovascular mortality in men with type 2 diabetes. This study demonstrates that long-term testosterone replacement is not only safe in terms of mortality but may also improve survival in men with type 2 diabetes and hypogonadism.
Jeffrey Dach MD
7450 Griffin Road Suite 190
Davie, Florida 33314
954-792-4663
http://www.drdach.com/
http://www.naturalmedicine101.com/
http://www.truemedmd.com/
http://www.bioidenticalhormones101.com/
Disclaimer click here: http://www.drdach.com/wst_page20.html
The reader is advised to discuss the comments on these pages with his/her personal physicians and to only act upon the advice of his/her personal physician. Also note that concerning an answer which appears as an electronically posted question, I am NOT creating a physician — patient relationship. Although identities will remain confidential as much as possible, as I can not control the media, I can not take responsibility for any breaches of confidentiality that may occur.
Link to this article:http://wp.me/p3gFbV-45X
Copyright (c) 2009- 2017 Jeffrey Dach MD All Rights Reserved. This article may be reproduced on the internet without permission, provided there is a link to this page and proper credit is given.
FAIR USE NOTICE: This site contains copyrighted material the use of which has not always been specifically authorized by the copyright owner. We are making such material available in our efforts to advance understanding of issues of significance. We believe this constitutes a ‘fair use’ of any such copyrighted material as provided for in section 107 of the US Copyright Law. In accordance with Title 17 U.S.C. Section 107, the material on this site is distributed without profit to those who have expressed a prior interest in receiving the included information for research and educational purposes.
Serving Areas of: Hollywood, Aventura, Miami, Fort Lauderdale, Pembroke Pines, Miramar, Davie, Coral Springs, Cooper City, Sunshine Ranches, Hallandale, Surfside, Miami Beach, Sunny Isles, Normandy Isles, Coral Gables, Hialeah, Golden Beach ,Kendall,sunrise, coral springs, parkland,pompano, boca raton, palm beach, weston, dania beach, tamarac, oakland park, boynton beach, delray,lake worth,wellington,plantation.
The post Testosterone Therapy Prolongs Life and Improves Survival appeared first on Jeffrey Dach MD .
December 19, 2016
Low Testosterone Associated with Increased Mortality
 Low Testosterone Associated with Increased Mortality
Low Testosterone Associated with Increased Mortality
by Jeffrey Dach MD
Forty Per Cent More Likely to Die
Two reports published in the recent medical literature showed that low testosterone is associated with increased mortality.(1)(2)(3) Upper Left Image: Chemical structure of human, bio-identiical testosterone courtesy of wikimedia commons.
In the first study from 2006, low testosterone was found to be associated with increased mortality among veterans. (1) . A low testosterone level was a total testosterone level of less than 250 ng/dL and 858 men were followed for 8 years. Those with low testosterone levels had an increased mortality rate (hazard ratio, 1.88). (1)
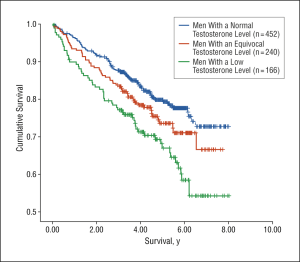 Left chart from Arch Int Med 2006 Molly Shores (1) Low Testosterone group (Green Line) had highest mortality rate.
Left chart from Arch Int Med 2006 Molly Shores (1) Low Testosterone group (Green Line) had highest mortality rate.
In the second study published in 2008 tracked nearly 800 men, 50 to 91 years old, living in California. Their testosterone level was measured at the beginning of the study, and their health was then tracked over the next 20 years. Low testosterone symptoms reported by these men included decreased libido, erectile dysfunction, fatigue, loss of strength, decrease in bone density and decreased muscle mass. Also, these men tended to be overweight or obese, and at higher risk for cardiovascular disease and diabetes. Men with the lowest testosterone, below 241 total serum level, were 40% more likely to die.(2)
A third study published by Dr Malkin in Heart 2010 showed that men with known coronary artery disease commonly had low testosterone levels which was associated with double the mortality rate compared with men with normal levels. (6) Dr Malkin says: “Excess mortality was noted in the androgen-deficient group compared with normal (41 (21%) vs 88 (12%)”
Conclusion:
Low testosterone in males is associated with increased mortality from coronary artery disease. Androgen deficiency is also associated with increased rate of depression. metabolic syndrome and low libido.(4,5) Testosterone supplementation in androgen deficient males is therefore beneficial.
Related Articles:
Low Testosterone – Diagnosis and Treatment
Does Testosterone Cause Prostate Cancer? by Jeffrey Dach MD
PSA Prostate Cancer and Testosterone Part Two
PSA Screening for Cancer, the Failed Medical Experiment by Jeffrey Dach MD
Jeffrey Dach MD
7450 Griffin Road Suite 190
Davie, Florida 33314
954-792-4663
http://www.jeffreydach.com/
http://www.drdach.com/
http://www.naturalmedicine101.com/
http://www.truemedmd.com/
http://www.bioidenticalhormones101.com/
Links and References
(1) http://www.ncbi.nlm.nih.gov/pubmed/16908801
Low Serum Testosterone and Mortality in Male Veterans Arch Intern Med. 2006;166:1660-1665 Molly M. Shores, MD; Alvin M. Matsumoto, MD; Kevin L. Sloan, MD; Daniel R. Kivlahan, PhD .Conclusions Low testosterone levels were associated with increased mortality in male veterans.
(2) http://jcem.endojournals.org/cgi/content/full/93/1/68http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2190742/
The Journal of Clinical Endocrinology & Metabolism 2008 Jan;93(1):68-75.
Low Serum Testosterone and Mortality in Older Men. Gail A. Laughlin, Eliza beth Barrett-Connor and Jaclyn Bergstrom. Department of Family and Preventive Medicine, School of Medicine, University of California, San Diego, La Jolla, California 92093
Results: During an average 11.8-yr follow-up, 538 deaths occurred. Men whose total testosterone levels were in the lowest quartile (
Conclusions: Testosterone insufficiency in older men is associated with increased risk of death over the following 20 yr, independent of multiple risk factors and several preexisting health conditions.
(3)http://abcnews.go.com/Health/ActiveAging/story?id=3247773&page=1&page=1
Low Testosterone Could Kill You. Low Levels of Male Hormone May be More Dangerous Than Previously Thought By SUPINDA BUNYAVANICH, M.D. ABC News Medical Unit June 6, 2007
Low testosterone may lead to a greater risk of death, according to a study presented Tuesday at the annual meeting of the Endocrine Society in Toronto.
Men with low testosterone had a 33 percent greater death risk over their next 18 years of life compared with men who had higher testosterone, according to the study conducted by Dr. Elizabeth Barrett-Connor and colleagues at the University of California at San Diego. “It’s very exciting and potentially a groundbreaking study,” said Barrett-Connor. “But it needs to be confirmed.” The study tracked nearly 800 men, 50 to 91 years old, living in California. Their testosterone level was measured at the beginning of the study, and their health was then tracked over the next 20 years.
4) http://www.medicalnewstoday.com/articles/153822.php
Testosterone Replacement For Men With Low Testosterone Improves Liver Function, Metabolic Syndrome. Testosterone deficiency, which becomes more common with age, is linked not only to decreased libido but also to a number of medical problems. These include the metabolic syndrome a cluster of metabolic risk factors that increase the chances of developing heart disease, stroke and type 2 diabetes.
5) http://www.news-medical.net/news/2008/03/04/35897.aspx
Low testosterone levels linked to depression in older men March 2008
Older men with lower free testosterone levels in their blood appear to have higher prevalence of depression, according to a report in the March issue of Archives of General Psychiatry.
6) Malkin, Chris J., et al. “Low serum testosterone and increased mortality in men with coronary heart disease.” Heart 96.22 (2010): 1821-1825. low-serum-testosterone-and-increased-mortality-in-men-with-coronary-heart-disease-malkin-chris-heart-2010 Background To examine the effect of serum testosterone levels on survival in a consecutive series of men with confirmed coronary disease and calculate the prevalence of testosterone deficiency.
Design Longitudinal follow-up study. Setting Tertiary referral cardiothoracic centre. Patients 930 consecutive men with coronary disease referred for diagnostic angiography recruited between June 2000 and June 2002 and followed up for a mean of 6.9±2.1 years.
Outcome All-cause mortality and vascular mortality. Prevalence of testosterone deficiency.
Results The overall prevalence of biochemical testosterone deficiency in the coronary disease cohort using bio-available testosterone (bio-T) Excess mortality was noted in the androgen-deficient group compared with normal (41 (21%) vs 88 (12%), p=0.002). The only parameters found to influence time to all-cause and vascular mortality (HR ± 95% CI) in multivariate analyses were the presence of left ventricular dysfunction (3.85; 1.72 to 8.33), aspirin therapy (0.63; 0.38 to 1.0), β-blocker therapy (0.45; 0.31 to 0.67) and low serum bio-T (2.27; 1.45 to 3.6).
Conclusions In patients with coronary disease testosterone deficiency is common and impacts significantly negatively on survival. Prospective trials of testosterone replacement are needed to assess the effect of treatment on survival.
Jeffrey Dach MD
7450 Griffin Road Suite 190
Davie, Florida 33314
954-792-4663
http://www.drdach.com/
http://www.naturalmedicine101.com/
http://www.truemedmd.com/
http://www.bioidenticalhormones101.com/
Disclaimer click here: http://www.drdach.com/wst_page20.html
The reader is advised to discuss the comments on these pages with his/her personal physicians and to only act upon the advice of his/her personal physician. Also note that concerning an answer which appears as an electronically posted question, I am NOT creating a physician — patient relationship. Although identities will remain confidential as much as possible, as I can not control the media, I can not take responsibility for any breaches of confidentiality that may occur.
Link to this article:http://wp.me/p3gFbV-45v
Copyright (c) 2009- 2017 Jeffrey Dach MD All Rights Reserved. This article may be reproduced on the internet without permission, provided there is a link to this page and proper credit is given.
FAIR USE NOTICE: This site contains copyrighted material the use of which has not always been specifically authorized by the copyright owner. We are making such material available in our efforts to advance understanding of issues of significance. We believe this constitutes a ‘fair use’ of any such copyrighted material as provided for in section 107 of the US Copyright Law. In accordance with Title 17 U.S.C. Section 107, the material on this site is distributed without profit to those who have expressed a prior interest in receiving the included information for research and educational purposes.
Serving Areas of: Hollywood, Aventura, Miami, Fort Lauderdale, Pembroke Pines, Miramar, Davie, Coral Springs, Cooper City, Sunshine Ranches, Hallandale, Surfside, Miami Beach, Sunny Isles, Normandy Isles, Coral Gables, Hialeah, Golden Beach ,Kendall,sunrise, coral springs, parkland,pompano, boca raton, palm beach, weston, dania beach, tamarac, oakland park, boynton beach, delray,lake worth,wellington,plantation.
The post Low Testosterone Associated with Increased Mortality appeared first on Jeffrey Dach MD .
December 13, 2016
Why Are One in Six On Psychiatric Meds ?
 Why Are One in Six On Psychiatric Meds ?
Why Are One in Six On Psychiatric Meds ?
by Jeffrey Dach MD
A JAMA article reported one in six Americans take psychiatric medications. These are mostly SSRI antidepressants such as Lexepro, benzodiazepines (Xanax), and sleeping pills (Ambien and Lunesta). (1) Above left image Jack Nicholson on Meds in Psych Ward One Flew Over the KooCoos Nest. Image Courtesy of Mental Floss.
The Numbers are Even Greater For Women
According to Julie Holland, a psychiatrist writing in the New York Times, One in Four women are on Psych Meds, compared to one in seven for men.(5)
You Might Be Curious To Know Why
You might be curious to know why so many people are taking psych meds. You might ask, “why are so many of our citizens on psych meds. Are they really needed on such a massive scale? Or is something else going on?
National Statement
Is this a statement about our nation, our culture, our way of life? What is the explanation for this sad state of affairs? Here are a number of different possible explanations
The pharmaceutical industry, also known as”Big Pharma”, has used deceptive advertising techniques to convince us we need psych meds in order to avoid unhappiness in our lives. If we have any life challenges which cause unhappiness, anxiety, insomnia, grief, hostility, or fear, then this has been redefined as a “psychiatric disease”. If only we took more psych meds, we could be truly happy with our lives. The result is one in six on psych meds, and windfall profits for Big Pharma. Left image Big Pharma courtesy of Before Its News.
 The Industrial Food GMO Explanation
The Industrial Food GMO Explanation
Our GMO food supply is genetically modified to withstand massive amounts of herbicides and pesticides which we unknowingly consume. These toxic food residues, along with red yellow and blue food colorings, chemical food additives, MSG, and Aspartame cause neurotoxicity and neuro-psychiatric disturbances in the population, all of which are treated with psych meds. The result: One in Six on Psych Meds. Left Image GMO Corn Courtesy of Anonymous Anti-GMO web Site.
The Politics Election Explanation
We are upset because the wrong candidate won the election and is saying the wrong things. We have been emotionally damaged by our “politics as usual” which inundated us with lies, distortions and propaganda designed to induce fear loathing and hatred on a grand scale. The politicians rake in more corporate campaign contributions, easily win re-election and create thousands of pages of new senseless legislation they don’t even read. Result: one in six on psych meds,
 The Evil Capitalism Explanation
The Evil Capitalism Explanation
Because our factories and jobs have been outsourced to third world countries, and our unemployed, depressed population is now standing in line at K-Mart buying Cheetos with Food Stamps, one in six are now taking psych meds.
The Evil Enemy Explanation
An opposing foreign nation has been agitating, and instigating unrest in the wrong places, or engaging in outright warfare in a foreign country where we happen to be supporting the opposite side. This could lead to global thermo-nuclear war leaving our poor planet a cinder heap. This has been reported in the papers causing agitation, nervousness and hysteria in our population. The final result: one in six on psych meds.
Psych Med Deficiency Syndrome
Through some accident of breeding, or perhaps reverse Darwinian evolution, many of us now have a genetic mutation called “Psych Med Deficiency Syndrome” in which we actually have a deficiency in our blood stream of these life saving medications. This is somehow producing a “chemical imbalance” in our brains. How is this treated? With Psych Meds, of course.
 Conclusion: Whatever the explanation, one in six on psych meds is a blinking red warning light on our national dashboard. Time to pull over and check the engine.Left upper image Warning Light on Dashboard courtesy of CarBuyer.
Conclusion: Whatever the explanation, one in six on psych meds is a blinking red warning light on our national dashboard. Time to pull over and check the engine.Left upper image Warning Light on Dashboard courtesy of CarBuyer.
Articles with Related Interest:
Attention Deficit Disorder Exposed as Drug Marketing Ploy
Exposing the False Prophets of Pediatric Psychiatry
Lithium Orotate the Great Protector
SSRI Induced Suicide in the Military
SSRI Drugs No Better Than Placebo
Getting Off SSRI Drugs Naturally
Links and References
1) Research Letter December 12, 2016
Adult Utilization of Psychiatric Drugs and Differences by Sex, Age, and Race
Thomas J. Moore, AB1; Donald R. Mattison, MD, MS2
Author Affiliations Article Information
JAMA Intern Med. Published online December 12, 2016.
These data show 1 of 6 US adults reported taking psychiatric drugs at least once during 2013, but with 2- to 3-fold differences by race/ethnicity, age, and sex. Moreover, use may have been underestimated because prescriptions were self-reported, and our estimates of long-term use were limited to a single survey year.
Among adults reporting taking psychiatric drugs, more than 8 of 10 reported long-term use. Prescribing information for the leading antidepressants includes limited information about appropriate duration of treatment. However, benzodiazepines have warnings about drug dependence, tolerance, withdrawal, and rebound symptoms.4 In a previous study,5 we found most patients were long-term users of the hypnotic zopidem tartrate despite recommendations for short-term use, and many were combining it with other central nervous system depressants despite warnings.
2) One in 6 Americans Take Antidepressants, Other Psychiatric Drugs: Study
by Maggie Fox
3) One in six U.S. adults takes a psychiatric drug, study says
By Steven Reinberg, HealthDay News | Dec. 12, 2016 at 9:06 PM
4) One in 6 US adults reports taking psychiatric drugs
5) Medicating Women’s Feelings By JULIE HOLLAND FEB. 28, 2015 New York Times
6) By Rachel Jones on August 22, 2013 in Health Nothing Is Wrong: Women, Mental Illness, and Medication
7) Stop the Madness: Coming off Psych Meds
by Kelly Brogan, MD
Jeffrey Dach MD
7450 Griffin Road Suite 180/190
Davie, Florida 33314
954-792-4663
http://www.jeffreydachmd.com/
http://www.drdach.com/
http://www.naturalmedicine101.com/
http://www.truemedmd.com/
Disclaimer click here: http://www.drdach.com/wst_page20.html
The reader is advised to discuss the comments on these pages with his/her personal physicians and to only act upon the advice of his/her personal physician. Also note that concerning an answer which appears as an electronically posted question, I am NOT creating a physician — patient relationship. Although identities will remain confidential as much as possible, as I can not control the media, I can not take responsibility for any breaches of confidentiality that may occur.
Link to this article:http://wp.me/p3gFbV-41i
Copyright (c) 2013-2017 Jeffrey Dach MD All Rights Reserved. This article may be reproduced on the internet without permission, provided there is a link to this page and proper credit is given.
FAIR USE NOTICE: This site contains copyrighted material the use of which has not always been specifically authorized by the copyright owner. We are making such material available in our efforts to advance understanding of issues of significance. We believe this constitutes a ‘fair use’ of any such copyrighted material as provided for in section 107 of the US Copyright Law. In accordance with Title 17 U.S.C. Section 107, the material on this site is distributed without profit to those who have expressed a prior interest in receiving the included information for research and educational purposes.
Serving Areas of: Hollywood, Aventura, Miami, Fort Lauderdale, Pembroke Pines, Miramar, Davie, Coral Springs, Cooper City, Sunshine Ranches, Hallandale, Surfside, Miami Beach, Sunny Isles, Normandy Isles, Coral Gables, Hialeah, Golden Beach ,Kendall,sunrise, coral springs, parkland,pompano, boca raton, palm beach, weston, dania beach, tamarac, oakland park, boynton beach, delray,lake worth,wellington,plantation.
The post Why Are One in Six On Psychiatric Meds ? appeared first on Jeffrey Dach MD .
December 8, 2016
Needless Fear of Estrogen Replacement Causes Suffering
 Needless Fear of Estrogen Replacement Causes Massive Suffering and Increased Mortality
Needless Fear of Estrogen Replacement Causes Massive Suffering and Increased Mortality
by Jeffrey Dach MD
According to a new study, fifty thousand women died needlessly because of fear of estrogen replacement after hysterectomy.(3) Both Time Magazine and the LA Times declared 50,000 women’s lives could have been saved.(3,4) Hysterectomy causes estrogen deficiency, a heath risk associated with increased mortality. Above Left Image Actress Elizabeth Taylor underwent hysterectomy, courtesy of Wikimedia Commons.
 Left Image Arlington Cemetary courtesy of wikimedia commons.
Left Image Arlington Cemetary courtesy of wikimedia commons.
The Mortality Toll of Estrogen Avoidance Yale University-
Published on Jul 18, 2013.
Dr Phillip M. Sarrel says: “Estrogen therapy has been widely misunderstood, and may offer important benefits to women in their 50s who have had a hysterectomy.” Watch this video from Philip M. Sarrel, MD , professor of Obstetrics and Gynecology at Yale Medical School.(3)
This information is old news. For many years, medical studies show HRT after hysterectomy reduces mortality and improves quality of life.
Bioidentical Estrogen Hormones Reduce Mortality After Hysterectomy
 For example, Dr. Parker followed 30,000 women over 24 years after hysterectomy. Half the women had ovaries removed and half had ovaries preserved. The group with ovaries removed had estrogen deficiency, and higher all cause mortality rate. Therefore, Dr. Parker recommended ovarian preservation.
For example, Dr. Parker followed 30,000 women over 24 years after hysterectomy. Half the women had ovaries removed and half had ovaries preserved. The group with ovaries removed had estrogen deficiency, and higher all cause mortality rate. Therefore, Dr. Parker recommended ovarian preservation.
Dr Parker also found that post-operative hormone replacement is very beneficial for reducing heart disease risk in women after hysterectomy. (1)
In a second study, Dr Cathleen Rivera followed 1,000 Pre-Menopausal women, under age 45, after hysterectomy, and found that removal of the ovaries resulted in a disturbing 84% increase in death from heart disease. However, if these women were given estrogen replacement after ovarian removal, they were protected with a 35% decrease in mortality from heart disease.(2) I thought this was rather impressive.
 Second Arm of Women’s Health Initiative- Premarin Only for Women After Hysterectomy
Second Arm of Women’s Health Initiative- Premarin Only for Women After HysterectomyThe Second Arm of the Women’s Health Initiative showed reduced mortality in the Estrogen users after hysterectomy. (11)
For the Premearin treated post-menopausal women 50-59 years of age, the authors reported an impressive 27% reduction in mortality compared to placebo group. (11) The obvious take-home message is that estrogen replacement is beneficial for women after hysterectomy. Doctors who deny women estrogen replacement cause needless suffering and increased mortality. Left Image: Pregnant Horse source of Premarin courtesy of wikimedia commons
Here is the quote from the 2011 JAMA publication of the Women’s Health Initiative (8):
“Younger postmenopausal women (aged 50-59 years) who were randomized to Premarin estrogen (CEE) vs. placebo had a lower risk of death (HR, 0.73) Note: HR is Hazard Ratio. This represents a 27% decrease in mortality for the estrogen users compared to placebo users (8)
Avoid Carcinogenic Synthetic Progestins
Synthetic versions of progesterone called “Progestins” such as medroxyprogesterone (MPA) are known to be carcinogenic based on data from the 2002 Womens Health Initiative WHI First Arm.(12) This study was halted early because synthetic progestins increased the risk of breast cancer. For this reason, avoiding carcinogenic progestins is recommended. Instead, use natural human bioidentical progesterone having the same chemical structure as ovarian progesterone, made by the female ovary.
Conclusion
We have known for decades the benefits of estrogen replacement after hysterectomy. Yet, thousands of women have been denied estrogen replacement causing needless suffering. Our stated mission at TrueMedMD is to oppose this trend by offering bioidentical hormones for every post menopausal woman who requests hormone replacement. That is our goal and mission.
Update 2016: Dr JoAnn Mason is in Agreement. See: Menopause-management-getting-clinical-care-back-on-track-new-england-journal-manson-joann-2016 Manson, JoAnn E., and Andrew M. Kaunitz. “Menopause Management Getting Clinical Care Back on Track New England Journal Manson JoAnn 2016 .(10)
A few quotes from Dr. Jo Ann Manson’s editorial in NEJM 2016: (10)
HRT Effective, Yet Few Woman Are Treated
“Despite the availability of effective hormonal …treatments for menopausal symptoms, few women with these symptoms are evaluated or treated.1,2″
Leading Medical Societies Agree that HRT is Effective and Should Be Recommended
Leading medical societies …agree that hormone therapy is the most effective treatment currently available for (menopausal) symptoms and should be recommended.”
Yet 20% of Symptomatic Women in Early Menopause Remain Untreated
Yet, “20% of women in early menopause… remain untreated despite having symptoms that adversely affect their daily activities, sleep, and quality of life.”
New Doctors Lack Training in Managing Menopausal Symptoms
“the new generation of …primary care providers often lacks training and core competencies in management of menopausal
symptoms and prescribing of hormonal …treatments.
2,3″
Doctor’s Reluctance to Treat has Created Needless Burden of Suffering
“Reluctance to treat menopausal symptoms has derailed and fragmented the clinical care of midlife women, creating a large and unnecessary burden of
suffering.”
Articles with Related Interest:
Bioidentical Hormones Found Beneficial After Hysterectomy
Bioidentical Hormones Prevent Osteoarthritis
Bioidentical Hormones Prevent Heart Disease
The Safety of Bioidentical Hormones
The Importance of Bioidentical Hormones
References:
(1) http://www.ncbi.nlm.nih.gov/pubmed/19384117
Obstet Gynecol. 2009 May;113(5):1027-37. Ovarian conservation at the time of hysterectomy and long-term health outcomes in the nurses’ health study. Parker WH, Broder MS, Chang E, Feskanich D, Farquhar C, Liu Z, Shoupe D, Berek JS, Hankinson S, Manson JE. John Wayne Cancer Institute at Saint John’s Health Center, Santa Monica, California 90401, USA. Comment in:
OBJECTIVE: To report long-term health outcomes and mortality after oophorectomy or ovarian conservation.
METHODS: We conducted a prospective, observational study of 29,380 women participants of the Nurses’ Health Study who had a hysterectomy for benign disease; 16,345 (55.6%) had hysterectomy with bilateral oophorectomy, and 13,035 (44.4%) had hysterectomy with ovarian conservation. We evaluated incident events or death due to coronary heart disease (CHD), stroke, breast cancer, ovarian cancer, lung cancer, colorectal cancer, total cancers, hip fracture, pulmonary embolus, and death from all causes.
RESULTS: Over 24 years of follow-up, for women with hysterectomy and bilateral oophorectomy compared with ovarian conservation, the multivariable hazard ratios (HRs) were1.12 (95% confidence interval [CI] 1.03-1.21) for total mortality, 1.17 (95% CI 1.02-1.35) for fatal plus nonfatal CHD, and 1.14 (95% CI 0.98-1.33) for stroke. Although the risks of breast (HR 0.75, 95% CI 0.68-0.84), ovarian (HR 0.04, 95% CI 0.01-0.09, number needed to treat=220), and total cancers (HR 0.90, 95% CI 0.84-0.96) decreased after oophorectomy, lung cancer incidence (HR=1.26, 95% CI 1.02-1.56, number needed to harm=190), and total cancer mortality (HR=1.17, 95% CI 1.04-1.32) increased.
For those never having used estrogen therapy, bilateral oophorectomy before age 50 years was associated with an increased risk of all-cause mortality, CHD, and stroke. With an approximate 35-year life span after surgery, one additional death would be expected for every nine oophorectomies performed.
CONCLUSION: Compared with ovarian conservation, bilateral oophorectomy at the time of hysterectomy for benign disease is associated with a decreased risk of breast and ovarian cancer but an increased risk of all-cause mortality, fatal and nonfatal coronary heart disease, and lung cancer. In no analysis or age group was oophorectomy associated with increased survival.
(2) http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2755630/?tool=pubmed
Menopause. 2009 Jan–Feb; 16(1): 15–23.
Increased cardiovascular mortality following early bilateral oophorectomy
Cathleen M. Rivera, MD,1 Brandon R. Grossardt, MS,2 Deborah J. Rhodes, MD,1 Robert D. Brown, Jr., MD, MPH,3 Véronique L. Roger, MD, MPH,4,5 L. Joseph Melton, III, MD, MPH,5 and Walter A. Rocca, MD, MPH3,5
We conducted a cohort study with long-term follow-up of women in Olmsted County, MN, who underwent either unilateral or bilateral oophorectomy before the onset of menopause from 1950 through 1987. Each member of the oophorectomy cohort was matched by age to a referent woman from the same population who had not undergone any oophorectomy. We studied the mortality associated with cardiovascular disease in a total of 1,274 women with unilateral oophorectomy, 1,091 women with bilateral oophorectomy, and 2,383 referent women.
Results: Women who underwent bilateral oophorectomy before age 45 years experienced anincreased mortality associated with cardiovascular disease compared with referent women (HR, 1.44; 95% CI, 1.01–2.05; P = 0.04).
Within this age stratum, the HR for mortality was significantly elevated in women who were not treated with estrogen through age 45 years or longer (HR, 1.84; 95% CI, 1.27–2.68; P = 0.001) but not in women treated (HR, 0.65; 95% CI, 0.30–1.41; P = 0.28; test of interaction, P = 0.01). Mortality was further increased after excluding deaths associated with cerebrovascular causes.
Conclusions: Bilateral oophorectomy performed before age 45 years is associated with increased cardiovascular mortality, especially with cardiac mortality. However, estrogen treatment may reduce this risk.
From a clinical perspective, our findings suggest that women who underwent bilateral oophorectomy at a young age are at increased risk of cardiovascular death, especially of cardiac death. This increased mortality may be attenuated by adequate estrogen treatment. Our findings provide new evidence to guide the individualized assessment of the risks and benefits of prophylactic bilateral oophorectomy in young women.1,4–6,8,14 This preventive practice currently involves approximately 4.5 million women older than 55 years living in the United States who have undergone bilateral oophorectomy before reaching natural menopause.28,34
In addition, our findings provide observational evidence for a long-term cardiovascular protective effect of estrogen either naturally produced by the ovaries or given as treatment to women who underwent bilateral oophorectomy at younger ages. These findings emphasize the importance of estrogen treatment after the surgery.6,9–14
We focused our analyses on age at estrogen deficiency rather than on the length of estrogen treatment after the surgery to study the combined effects of age at the surgery and length of treatment.
Several studies have shown increased cardiovascular mortality in women who experienced early menopause (before age 45 years) from either natural or medical causes,35–40 and a statistical model has linked prophylactic bilateral oophorectomy before age 65 years with an increase in overall mortality and coronary heart disease mortality.1,4,5
Similarly, in the Women’s Health Initiative Observational Study, hysterectomy plus oophorectomy performed over a broad age range was a significant predictor of cardiovascular disease during a short-term follow-up.28
Recent analyses from the Women’s Health Initiative Coronary Artery Calcium Study showed an increased risk of subclinical coronary artery disease in women who underwent both hysterectomy and bilateral oophorectomy and were not treated with estrogen compared to women who underwent hysterectomy alone. The increased risk was independent of traditional cardiovascular risk factors.12
Our results for estrogen treatment after bilateral oophorectomy are consistent both with findings from previous clinical studies40–44 and with findings from animal studies. Primates who underwent premenopausal oophorectomy and did not receive exogenous estrogen had significantly accelerated atherosclerosis compared with those that did not have oophorectomy
This study showed that women who underwent early bilateral oophorectomy are at increased risk of death involving cardiovascular disease, especially cardiac diseases. However, treatment with estrogen through age 45 years or longer may reduce this risk. These findings, in conjunction with the results of other studies,1,4,5,8 have important clinical implications and should prompt a reassessment of prophylactic bilateral oophorectomy in premenopausal women.6,14
3) http://ajph.aphapublications.org/doi/abs/10.2105/AJPH.2013.301295 American Journal of Public Health. The Mortality Toll of Estrogen Avoidance: An Analysis of Excess Deaths Among Hysterectomized Women Aged 50 to 59 Years. Philip M. Sarrel, MD, Valentine Y. Njike, MD, MPH, Valentina Vinante, MD, and David L. Katz, MD, MPH
Objectives. We examined the effect of estrogen avoidance on mortality rates among hysterectomized women aged 50 to 59 years.
Methods. We derived a formula to relate the excess mortality among hysterectomized women aged 50 to 59 years assigned to placebo in the Women’s Health Initiative randomized controlled trial to the entire population of comparable women in the United States, incorporating the decline in estrogen use observed between 2002 and 2011.
Results. Over a 10-year span, starting in 2002, a minimum of 18 601 and as many as 91 610 postmenopausal women died prematurely because of the avoidance of estrogen therapy (ET).
Conclusions. ET in younger postmenopausal women is associated with a decisive reduction in all-cause mortality, but estrogen use in this population is low and continuing to fall. Our data indicate an associated annual mortality toll in the thousands of women aged 50 to 59 years. Informed discussion between these women and their health care providers about the effects of ET is a matter of considerable urgency. (Am J Public Health. Published online ahead of print July 18, 2013:)
Time Magazine
Hormone-Replacement Therapy: Could Estrogen Have Saved 50,000 Lives?
By Alexandra Sifferlin July 20, 201316
Dr. Philip Sarrel, professor emeritus of obstetrics, gynecology and reproductive sciences at Yale University School of Medicine and lead author of the study, said in a video discussing the study that none of these women, who were aged 50 to 59 at the start of the study, lived to reach their 70s. Most died of heart disease, bolstering the connection that earlier studies had found between estrogen-only therapy and a lower risk of heart problems among women who had a hysterectomy.
LA Times
Avoiding estrogen therapy proved deadly for nearly 50,000: study
By Eryn Brown This post has been updated. See below for details.
July 18, 2013, 3:44 p.m.
Huffington Post
6) http://www.huffingtonpost.com/david-katz-md/estrogen-meopause_b_3639915.html
Huffington Post – David Katz, M.D. Director, Yale Prevention Research Center. Estrogen and Evidence Posted: 07/23/2013 2:48 pm
Web MD
Did Avoidance of Hormone Therapy Harm Certain Women?
For older women without a uterus, estrogen may save lives, researchers say
The use of hormone therapy — both estrogen-only and the combination of estrogen plus progestin — declined greatly after the U.S. Women’s Health Initiative Study found in 2002 that combination therapy had ill effects, including an increase in breast cancer, heart disease, stroke and blood clots. Prescriptions for both regimens plummeted even though the research didn’t apply to women without a uterus or to women on estrogen-only therapy, said Sarrel, who is a consultant for Noven Therapeutics, which makes an estrogen patch.
They found that use of estrogen-only therapy in U.S. women aged 50 to 59 declined nearly 79 percent between 2001 and 2011.
During that time, at least 18,000 excess deaths occurred because of estrogen avoidance and possibly more than 91,000, depending on the calculations used, Sarrel’s team said. For this reason, their best estimate — of about 50,000 deaths — may be conservative, said Sarrel.
=====================
JAMA WHI
8) http://jama.jamanetwork.com/article.aspx?articleid=896193 April 6, 2011, Vol 305, No. 13 Health Outcomes After Stopping Conjugated Equine Estrogens Among Postmenopausal Women With Prior Hysterectomy A Randomized Controlled Trial the WHI Investigators
The HRs for total mortality and the global index of chronic diseases differed by age as previously suggested.7
Younger postmenopausal women (aged 50-59 years) who were randomized to CEE vs placebo had a lower risk of death (0.35% [n = 65] vs 0.48% [n = 89], respectively; HR, 0.73 [95% CI, 0.53-1.00]) compared with no increased risk among women in their 60s (1.00% [n = 254] vs 0.96% [n = 253], respectively; HR, 1.04 [95% CI, 0.88-1.24]), and a slight increased risk of death among women in their 70s (2.02% [n = 258] vs 1.83% [n = 239], respectively; HR, 1.12 [95% CI, 0.94-1.33]; P = .04 for interaction). A similar pattern was observed by age for women randomized to CEE vs placebo for the global index of chronic diseases with a possible overall benefit among younger women (aged 50-59 years: 1.04% [n = 184] vs 1.22% [n = 217], respectively; HR, 0.85 [95% CI, 0.70-1.03]) and possible harm among the oldest women (aged 70-79 years: 4.04% [n = 466] vs 3.56% [n = 423], respectively; HR, 1.15 [95% CI, 1.01-1.32]; P = .009 for interaction).
9) http://www.pr.com/press-release/505829
Dr. Tim Bilash Announces New Findings Refuting Previous Studies on Hormone Replacement Therapy, Offers Free Consultations
Dr. Timothy Bilash, MD’s has announced his new research findings that refute a 2002 WHI study that post menopausal women should not take estrogen.
———————————————
Bioidentical Hormones could have saved 50,000 Lives according to Dr. Philip Sarrel
Dr Cathleen Rivera followed 1,000 Pre-Menopausal women (under age 45) after hysterectomy, and found that removal of the ovaries resulted in a disturbing 84% increase in death from heart disease. However, if these women were given estrogen replacement after ovarian removal, they were protected with a 35% decrease in mortality from heart disease. I thought this was rather impressive.
The 2nd arm of the Women’s Health Initiative also showed reduced mortality in the estrogen users (50-59 yrs) after hysterectomy. They showed a 27% reduction in mortality with estrogen use. So this supports the hypothesis that estrogen deficiency is associated with increased mortality and other health risks, while estrogen replacement for post-hysterectomy women is very beneficial. Of course, women should avoid Progestins and other synthetic hormones such as medroxyprogesterone (MPA) which is known to be carcinogenic from the First Arm WHI data. The use of natural, bioidentical estrogen and progesterone in the proper balance is the preferred choice. Bioidentical hormones are not chemically altered, having chemical structures identical to our own hormones, naturally occurring in ourselves.
10) menopause-management-getting-clinical-care-back-on-track-new-england-journal-manson-joann-2016
Manson, JoAnn E., and Andrew M. Kaunitz. “Menopause Management—Getting Clinical Care Back on Track.” New England Journal of Medicine 374.9 (2016): 803-806.
11) Anderson, G. L., et al. “Women’s Health Initiative Steering Committee. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women’s Health Initiative randomized controlled trial.” Jama 291.14 (2004): 1701-1712.
12) Writing Group for the Women’s Health Initiative Investigators. “Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trial.” Jama 288.3 (2002): 321-333.
14) Seven Celebrities Who Braved a Hysterectomy.
Jeffrey Dach MD
7450 Griffin Road Suite 180/190
Davie, Florida 33314
954-792-4663
http://www.jeffreydachmd.com/
http://www.drdach.com/
http://www.naturalmedicine101.com/
http://www.truemedmd.com/
Disclaimer click here: http://www.drdach.com/wst_page20.html
The reader is advised to discuss the comments on these pages with his/her personal physicians and to only act upon the advice of his/her personal physician. Also note that concerning an answer which appears as an electronically posted question, I am NOT creating a physician — patient relationship. Although identities will remain confidential as much as possible, as I can not control the media, I can not take responsibility for any breaches of confidentiality that may occur.
Link to this article:http://wp.me/p3gFbV-40z
Copyright (c) 2013-2017 Jeffrey Dach MD All Rights Reserved. This article may be reproduced on the internet without permission, provided there is a link to this page and proper credit is given.
FAIR USE NOTICE: This site contains copyrighted material the use of which has not always been specifically authorized by the copyright owner. We are making such material available in our efforts to advance understanding of issues of significance. We believe this constitutes a ‘fair use’ of any such copyrighted material as provided for in section 107 of the US Copyright Law. In accordance with Title 17 U.S.C. Section 107, the material on this site is distributed without profit to those who have expressed a prior interest in receiving the included information for research and educational purposes.
The post Needless Fear of Estrogen Replacement Causes Suffering appeared first on Jeffrey Dach MD .
December 6, 2016
Online Information for Hashimotos Thyroid Disease
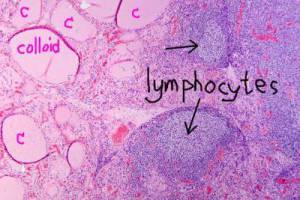 Online Information for Hashimotos Thyroid Disease
Online Information for Hashimotos Thyroid Disease
Susan has Hashimotos’ thyroid disease, and has been online gathering information and learning as much as she can. However, Susan is bewildered by the amount of contradictory and conflicting information, and is asking me for a list of recommended information sites. One such recommended information site is Thyroid Pharmacist, Isabella Wentz.
Above left image shows microscopic histology of hashimotos thyroiditis with arrows pointing to lymphocytic infiltration of stroma. Area marked (c) is colloid storage area for thyroglobulin. Image courtesy of Wikimedia commons.
Here is the complete list.
Recommended Thyroid Disease Online Information Sites
Graves’ Elaine Moore
Hashimotos Awareness
Mary Shomon
Hypo Thyroid Mom
Stop the Thyroid Madness
Thyroid Pharmacist Isabella Wentz
Thyroid Skeptic
Another excellent resource is the chapter on Hashimotos’ Thyroid Disease in the book, Stop the thyroid Madness Vol Two edited by Janie Bowthorpe. (this chapter was written by me)
Articles with related interest:
Stop the thyroid Madness Vol Two
Hashimotos Molecular Mimicry and Thyroid Disease
Hashimotos and Manic Depression
Hashimotos and Selenium Part One
link to this article:http://wp.me/p3gFbV-409
Jeffrey Dach MD
7450 Griffin Road Suite 190
Davie, Fl 33314
954-792-4663
www.jeffreydachmd.com
http://www.drdach.com
http://www.naturalmedicine101.com
http://www.bioidenticalhormones101.com
http://www.truemedmd.com
The reader is advised to discuss the comments on these pages with his/her personal physicians and to only act upon the advice of his/her personal physician. Also note that concerning an answer which appears as an electronically posted question, I am NOT creating a physician — patient relationship. Although identities will remain confidential as much as possible, as I can not control the media, I can not take responsibility for any breaches of confidentiality that may occur.
Copyright (c) 2016 Jeffrey Dach MD All Rights Reserved. This article may be reproduced on the internet without permission, provided there is a link to this page and proper credit is given.
FAIR USE NOTICE: This site contains copyrighted material the use of which has not always been specifically authorized by the copyright owner. We are making such material available in our efforts to advance understanding of issues of significance. We believe this constitutes a ‘fair use’ of any such copyrighted material as provided for in section 107 of the US Copyright Law. In accordance with Title 17 U.S.C. Section 107, the material on this site is distributed without profit to those who have expressed a prior interest in receiving the included information for research and educational purposes.
Serving Areas of: Hollywood, Aventura, Miami, Fort Lauderdale, Pembroke Pines, Miramar, Davie, Coral Springs, Cooper City, Sunshine Ranches, Hallandale, Surfside, Miami Beach, Sunny Isles, Normandy Isles, Coral Gables, Hialeah, Golden Beach ,Kendall,sunrise, coral springs, parkland,pompano, boca raton, palm beach, weston, dania beach, tamarac, oakland park, boynton beach, delray,lake worth,wellington,plantation.
The post Online Information for Hashimotos Thyroid Disease appeared first on Jeffrey Dach MD .
November 13, 2016
Low Thyroid, Hashimotos and Pregnancy
 Low Thyroid, Hashimotos and Pregnancy
Low Thyroid, Hashimotos and Pregnancy
by Jeffrey Dach MD
Today is a happy day for Susan. She just delivered a healthy baby girl, and sent me a cute baby photo with a thank you note. Six months before, Susan was weeping in my office, recounting her story of repeated miscarriages and fertility problems. Her lab panel showed a borderline low thyroid status and elevated anti-thyroid antibodies indicating Hashimoto’s Autoimmune Thyroiditis. Upper Left Image courtesy of wikimedia commons.
After a complete evaluation, we started Susan on our usual program of natural desiccated thyroid One and a Half Grains per day, selenium 400 mcg/day, iodine 450 mcg per day and a good prenatal multivitamin. That must have done the trick, and Susan’s thank you card has the “pitter patter of little feet” on the cover.
Since ten to twenty per cent of all women of reproductive age have elevated anti thyroid antibodies, we see this scenario quite often. There are literally thousands of low thyroid Susans ignored by mainstream medicine, left to suffer through repeated miscarriages and other fertility problems, representing yet another tragic error by conventional endocrinology. Left image mother and baby courtesy of wikimedia commons.
Dr Peter Taylor Makes a Plea
Dr Peter Taylor made exactly this point at a recent Endocrine Society Meeting when he said that more pregnant women would benefit from thyroid hormone treatment to prevent miscarriages and stillborn babies.(8) His pleas to screen all pregnant women were ignored, as they have been for many years.(9) Further studies show that many women with thyroid anti-bodies have better pregnancy outcomes when treated with thyroid hormones.(10,11)
The New York Times Gets the Story Right
A few years back in 2009, Dr Alex Stagnaro-Green gave the New York Times an accurate accounting of the role of thyroid in pregnancy. (1) These are Dr Green’s points:
1) Pregnancy is like a stress test for the thyroid. increasing thyroid hormone requirement by 50%
2) Hypothyroidism during pregnancy is linked to miscarriage (5), and preterm delivery. (5) Compared to aged matched controls, children of hypothyroid mothers have lower I.Q.s by seven points on average when tested seven to nine years later. (3) Nineteen per cent of these children had IQ’s of 85 or less.(3)
3) Even though thyroid hormone levels may be completely normal, the presence of Hashimoto’s anti-thyroid antibodies is associated with a 200-300% increase of miscarriage.
Dr. Roberto Negro from Italy published a study in 2006 of women who were thyroid antibody-positive. Treatment of these women with thyroid hormone resulted in a dramatic reduction of stillbirths and preterm deliveries.(4) Upper left image courtesy of wikimedia commons.
How to Make Smarter Babies
As mentioned above, children born to hypothyroid mothers, have lower IQ when tested 7-9 years later. Giving thyroid hormones to the mother makes smarter babies.(3) In addition, maternal iodine deficiency is associated with reduced educational outcomes in the offspring.(14) This is precisely why we screen women for iodine levels, and make sure they have adequate iodine supplementation. In Hashimotos patients, we use low-dose iodine supplementation of 225-450 mcg per day which is a safe level.
Perhaps the one person most dedicated to getting this message out is Dana Trentini who runs HypoThyroid Mom. (left image courtesy of Dana Trentini Hypothyroid MOM.
After suffering through a miscarriage herself, she discovered the importance of thyroid in pregnancy, and has been a tireless advocate ever since. Regretting her misplaced trust in doctors who failed to treat her low thyroid condition, HypothyroidMom now encourages all women to take charge of their thyroid health. The EcoFeminist Blog run by Aimee picks up and amplifies this message in her article, hypothyroidism and miscarriage.
Conclusion: Another tragedy of modern endocrinology is the manner in which the hypothyroid mom is ignored, leading to unnecessary suffering. All pregnant women should be screened for thyroid antibodies and more pregnant women should be treated with thyroid hormones which will result in reduction in miscarriages, reduction in preterm infants, and improvement in IQ and educational outcomes in the newborn
Jeffrey Dach MD
7450 Griffin Road Suite 190
Davie, Fl 33314
954-792-4663
Articles with Related Interest
Why Natural Thyroid is Better than Synthetic
TSH SUppression Benefits and Adverse Effects
How to Make Smarter Children with Iodine Supplementation
Hashimotos, Iodine and Selenium
Links and references
1) http://www.nytimes.com/ref/health/healthguide/esn-hypothyroidism-expert.html?pagewanted=all
Pregnancy and the Thyroid New York Times 3/13/2009
By INGFEI CHEN Dr. Alex Stagnaro-Green is a professor of medicine and obstetrics and gynecology at Touro University College of Medicine in Hackensack, N. J. He was a member of an international panel of experts convened by the Endocrine Society that issued a clinical practice guideline in 2007 on managing thyroid dysfunction during pregnancy and after childbirth.
It turns out that pregnancy is like a stress test for the thyroid: the amount of thyroid hormone that needs to be released during pregnancy is increased by about 50 percent, and that’s because of some of the hormones related to pregnancy. If there is a dysfunction with the thyroid, it has been linked — especially hypothyroidism — to miscarriage, preterm delivery, and also with decreased I.Q. in the unborn child when tested at 7 to 9 years old. Furthermore, if a woman has Hashimoto’s disease with antibodies, but with the thyroid hormone levels still being normal, that’s also been associated with a two- to threefold increase of miscarriage. So that’s why all this is very important.
But the women who were antibody-positive who didn’t get the thyroid hormone had a miscarriage rate that was four times higher.
First I educate her that about 50 to 60 percent of women who have thyroid disease and are on thyroid hormone replacement therapy will need an increase in the hormone very early in the first trimester. I explain that this is extremely important so as to prevent complications like miscarriage. And therefore we try to adjust the thyroid hormone level before a woman gets pregnant so that she’s clearly in the normal range.
Secondly, as soon as they get pregnant, I have my patients call me immediately to get thyroid function tests so that I can modify their dose as early as possible in the pregnancy. Bottom line is that as soon as a woman knows she is pregnant she should be tested and see her doctor.
2) https://www.ncbi.nlm.nih.gov/pubmed/2118190
JAMA. 1990 Sep 19;264(11):1422-5.
Detection of at-risk pregnancy by means of highly sensitive assays for thyroid autoantibodies.
Stagnaro-Green A1, Roman SH, Cobin RH, el-Harazy E, Alvarez-Marfany M, Davies TF. Department of Medicine, Mount Sinai School of Medicine, New York, NY 10029.
We screened 552 women who presented to their obstetrician in the first trimester of pregnancy using highly sensitive enzyme-linked immunosorbent assays for the presence of thyroglobulin and thyroid peroxidase autoantibodies and found an incidence of positivity of 19.6%. The tendency to secrete detectable levels of thyroid autoantibodies was significantly correlated with an increased rate of miscarriage. Thyroid autoantibody-positive women miscarried at a rate of 17%, compared with 8.4% for the autoantibody-negative women. Individual levels of thyroglobulin and thyroid peroxidase autoantibodies were similarly related to this increased miscarriage rate, with no evidence of autoantibody specificity in the relationship. Furthermore, the increase in miscarriages could not be explained by differences in thyroid hormone levels, the presence of cardiolipin autoantibodies, maternal age, gestational age at the time of maternal entry into the study, or previous obstetric history. We conclude that thyroid autoantibodies are an independent marker of “at-risk” pregnancy.
3) https://www.ncbi.nlm.nih.gov/pubmed/10451459
N Engl J Med. 1999 Aug 19;341(8):549-55.
Maternal thyroid deficiency during pregnancy and subsequent neuropsychological development of the child.
Haddow JE1, Palomaki GE, Allan WC, Williams JR, Knight GJ, Gagnon J, O’Heir CE, Mitchell ML, Hermos RJ, Waisbren SE, Faix JD, Klein RZ.
When thyroid deficiency occurs simultaneously in a pregnant woman and her fetus, the child’s neuropsychological development is adversely affected. Whether developmental problems occur when only the mother has hypothyroidism during pregnancy is not known.
METHODS:In 1996 and 1997, we measured thyrotropin in stored serum samples collected from 25,216 pregnant women between January 1987 and March 1990. We then located 47 women with serum thyrotropin concentrations at or above the 99.7th percentile of the values for all the pregnant women, 15 women with values between the 98th and 99.6th percentiles, inclusive, in combination with low thyroxine levels, and 124 matched women with normal values. Their seven-to-nine-year-old children, none of whom had hypothyroidism as newborns, underwent 15 tests relating to intelligence, attention, language, reading ability, school performance, and visual-motor performance.
RESULTS:The children of the 62 women with high serum thyrotropin concentrations performed slightly less well on all 15 tests. Their full-scale IQ scores on the Wechsler Intelligence Scale for Children, third edition, averaged 4 points lower than those of the children of the 124 matched control women (P= 0.06); 15 percent had scores of 85 or less, as compared with 5 percent of the matched control children. Of the 62 women with thyroid deficiency, 48 were not treated for the condition during the pregnancy under study. The full-scale IQ scores of their children averaged 7 points lower than those of the 124 matched control children (P=0.005); 19 percent had scores of 85 or less. Eleven years after the pregnancy under study, 64 percent of the untreated women and 4 percent of the matched control women had confirmed hypothyroidism.
CONCLUSIONS:Undiagnosed hypothyroidism in pregnant women may adversely affect their fetuses; therefore, screening for thyroid deficiency during pregnancy may be warranted.
4) https://www.ncbi.nlm.nih.gov/pubmed/16621910
J Clin Endocrinol Metab. 2006 Jul;91(7):2587-91.
Levothyroxine treatment in euthyroid pregnant women with autoimmune thyroid disease: effects on obstetrical complications.
Negro R1, Formoso G, Mangieri T, Pezzarossa A, Dazzi D, Hassan H.
Euthyroid women with autoimmune thyroid disease show impairment of thyroid function during gestation and seem to suffer from a higher rate of obstetrical complications.
OBJECTIVE:We sought to determine whether these women suffer from a higher rate of obstetrical complications and whether levothyroxine (LT(4)) treatment exerts beneficial effects.
DESIGN:This was a prospective study.
SETTING:The study was conducted in the Department of Obstetrics and Gynecology.
PATIENTS:A total of 984 pregnant women were studied from November 2002 to October 2004; 11.7% were thyroid peroxidase antibody positive (TPOAb(+)).
INTERVENTION:TPOAb(+) patients were divided into two groups: group A (n = 57) was treated with LT(4), and group B (n = 58) was not treated. The 869 TPOAb(-) patients (group C) served as a normal population control group.
MAIN OUTCOME MEASURES:Rates of obstetrical complications in treated and untreated groups were measured.
RESULTS:At baseline, TPOAb(+) had higher TSH compared with TPOAb(-); TSH remained higher in group B compared with groups A and C throughout gestation. Free T(4) values were lower in group B than groups A and C after 30 wk and after parturition. Groups A and C showed a similar miscarriage rate (3.5 and 2.4%, respectively), which was lower than group B (13.8%) [P < 0.05; relative risk (RR), 1.72; 95% confidence interval (CI), 1.13-2.25; and P < 0.01; RR = 4.95; 95% CI = 2.59-9.48, respectively]. Group B displayed a 22.4% rate of premature deliveries, which was higher than group A (7%) (P < 0.05; RR = 1.66; 95% CI = 1.18-2.34) and group C (8.2%) (P < 0.01; RR = 12.18; 95% CI = 7.93-18.7).
CONCLUSIONS:Euthyroid pregnant women who are positive for TPOAb develop impaired thyroid function, which is associated with an increased risk of miscarriage and premature deliveries. Substitutive treatment with LT(4) is able to lower the chance of miscarriage and premature delivery.
============================================
5) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4229690/
Maternal Subclinical Hypothyroidism, Thyroid Autoimmunity, and the Risk of Miscarriage: A Prospective Cohort Study
Liu Haixia, Shan Zhongyan, Li Chenyan, Mao Jinyuan, Xie Xiaochen, Wang Weiwei, Fan Chenling, Wang Hong, Zhang Hongmei,
Han Cheng, Wang Xinyi, Liu Xin, Fan Yuxin, Bao Suqing, and Teng Weiping. Thyroid. November 2014, 24(11): 1642-1649.
ABSTRACT Background: Increasing data suggest that subclinical hypothyroidism (SCH) and thyroid autoimmunity (TAI) are associated with adverse pregnancy outcomes, but there are limited data on the association of these conditions in early pregnancy with subsequent miscarriage.
Methods: In this prospective cohort study, we screened 3315 women at low risk for thyroid dysfunction at four to eight weeks’ gestation from iodine-sufficient areas of China between January 2012 and September 2012. Thyrotropin (TSH), free thyroxine (fT4), and the autoantibodies thyroid-peroxidase antibody (TPOAb) and thyroglobulin antibody (TgAb) were measured. Based on these results, women were divided into four groups for comparison: euthyroidism (ET), isolated SCH, isolated TAI (positive TPOAb or/and TgAb), and SCH with TAI (SCH+TAI). The SCH group was stratified into two subgroups (SCH 1 and SCH 2) on the basis of the level of TSH (2.5≤TSH
Results: Compared to women with ET, the risk of miscarriage was significantly higher among women with SCH 2 (7.1% vs. 2.2%, aOR 3.40 [CI 1.62–7.15]; p=0.002), isolated TAI (5.7% vs. 2.2%, aOR 2.71 [CI 1.43–5.12]; p=0.003), SCH+TAI 1 (10.0% vs. 2.2%, aOR 4.96 [CI 2.76–8.90]; p=0.000), and SCH+TAI 2 (15.2% vs. 2.2%, aOR 9.56 [CI 3.76–24.28]; p=0.000). The gestational ages of 110 women at miscarriage were lower among women with subclinical thyroid abnormalities compared to ET (11.13±3.21 weeks with subclinical thyroid abnormalities vs. 9.33±1.71 weeks with ET; p=0.024). In parallel with the higher TSH levels, there were earlier gestation ages at miscarriage between subgroups of SCH and SCH+TAI (SCH 1 vs. SCH 2: 10.79±1.77 vs. 9.70±1.47 weeks, p=0.039; SCH+TAI 1 vs. SCH+TAI 2: 9.59±1.97 vs. 8.88±1.24 weeks, p=0.031).
Conclusions: Women with SCH and TAI are at an increased risk of miscarriage between four and eight gestational weeks. Women with a combination of SCH and TAI were found to have the highest risk and earlier gestational ages of miscarriage.
6) http://hypothyroidmom.com/what-every-pregnant-woman-needs-to-know-about-hypothyroidism/
What Every Pregnant Woman Needs To Know About Hypothyroidism
October 8, 2012 by Dana Trentini
The launch of my blog Hypothyroid Mom is intentionally timed this October 2012 during Miscarriage Awareness Month in memory of the baby I lost to hypothyroidism and in dedication to my two boys who beat the odds and made it to the world. This is Part 2 of my 5-part series entitled Miscarriage Awareness Month: The Dangers of Hypothyroidism And Pregnancy.
7) https://theecofeminist.com/2016/08/30/hypothyroidism-and-miscarriage/
Hypothyroidism and Miscarriage August 30, 2016 Eco Feminist
Nov 9, 2016 Peter Taylor
8) https://www.sciencedaily.com/releases/2016/11/161109090353.htm
Giving more pregnant women common thyroid medicine may reduce risk of complications. Date: November 9, 2016
Source: Society for Endocrinology
Summary: Extending the number of pregnant women given the common drug levothyroxine to boost thyroid hormone levels may lead to a reduced number of stillbirths, early caesarean sections and low-weight babies, according to a new study.
In this study, researchers from the University of Cardiff investigated whether pregnant women with mild hypothyroidism and their babies would also benefit from levothyroxine treatment. They combined data from a thyroid screening study and linked it to routinely collected clinical data to study the effect of correcting borderline thyroid function on obstetric outcomes.
The researchers analysed over 13,000 women who were 12-16 weeks pregnant, 518 of whom had mild hypothyroidism. Of these, 263 women received levothyroxine and the rest received no treatment. They assessed the women’s pregnancy outcomes by measuring stillbirth rates, preterm delivery, length of stay at hospital, birth weight and the number of early caesarean sections.
They found that women with mild hypothyroidism treated with levothyroxine had a lower risk of giving birth to low weight babies and were also less likely to undergo an early caesarean. Untreated women with mild hypothyroidism were more likely to have a stillbirth than women with normal thyroid function and no stillbirths occurred in the treated group. However, there was no significant difference between the other obstetric outcomes or when all outcomes were combined.
“Our work raises the possibility of providing real benefits from using a safe, cheap and well established treatment by simply extending it to the number of pregnant women we treat,” said Dr Peter Taylor, lead author of the study.
Dr Taylor believes more substantial benefits might be found by treating the pregnant women at an earlier stage than used in this study. “We should consider universal thyroid screening in pregnancy as it compares favourably in terms of cost-effectiveness with other conditions that we currently screen for,” he added.
9) http://www.futuremedicine.com/doi/abs/10.2217/whe.15.7?journalCode=whe
Taylor, Peter N., et al. “Should all women be screened for thyroid dysfunction in pregnancy?.” Women’s Health 11.3 (2015): 295-307.
The subject of universal thyroid screening in pregnancy generates impassioned debate. Thyroid dysfunction is common, has significant adverse implications for fetal and maternal well-being, is readily detectable and can be effectively and inexpensively treated. Furthermore, the currently recommended case-finding strategy does not identify a substantially proportion of women with thyroid dysfunction thus favoring universal screening. On the other hand subclinical thyroid dysfunction forms the bulk of gestational thyroid disorders and the paucity of high-level evidence to support correction of these asymptomatic biochemical abnormalities weighs against universal screening. This review critically appraises the literature, examines the pros and cons of universal thyroid screening in pregnancy, highlighting the now strong case for implementing universal screening and explores strategies for its implementation.
10) http://www.endocrine-abstracts.org/ea/0044/ea0044OC6.3.htm
Endocrine Abstracts (2016) 44 OC6.3
Controlled Antenatal ; Obstetric Outcomes
Peter Taylor1, Arron Lacey2, Daniel Thayer2, Mohd Draman1, Arshiya Tabasum1,3, Ilaria Muller1, Luke Marsh1, Arwel Poacher1, Aled Roberts3, Marian Ludgate1, Alex Rees3, Kristien Boelaert4, Aled Rees1, Shiao Chan4,5, John Lazarus1, Scott Nelson6, Bijay Vaidya7 & Onyebuchi Okosieme1
Context: Suboptimal thyroid function in pregnancy is associated with adverse obstetric outcomes but it is unclear whether levothyroxine treatment, initiated during pregnancy is beneficial.
Design & Participants: Retrospective analysis of the Controlled Antenatal Thyroid Screening (CATS) study with obstetric outcomes obtained through data-linkage in the Secure Anonymised Information Linkage (SAIL) databank. We studied 13,224 pregnant women; 12,608 had normal thyroid function, 340 had subclinical hypothyroidism (SCH), 305 had isolated hypothyroxinemia (IH). 518 women with abnormal thyroid function were randomized to receive levothyroxine (N=263) or no treatment (N=255) at the end of the first trimester.
Main Outcome Measures: Composite measure (primary outcome) of stillbirth, neonatal death, preterm delivery 5 days. Secondary analyses included early gestational age (
Results: In individuals with abnormal thyroid function randomized to treatment or control, treatment had no discernible effect on the composite outcome. 29 events occurred in the untreated group vs 22 in the treated. OR (treated) = 0.75 95%CI (0.40, 1.40). Untreated women with SCH had increased odds of stillbirth compared to women with normal thyroid function OR=4.37 (95%CI 1.04, 18.3). No stillbirths occurred in women on levothyroxine. Untreated women with IH had increased odds of an early gestational age at delivery (
Conclusion: Both SCH and IH were associated with key adverse obstetric outcomes. Although there was no difference in composite outcome there were some benefits observed with levothyroxine therapy. Larger studies are required to confirm the benefits of screening and treatment in pregnancy.
11) http://www.bmj.com/content/342/bmj.d2616
Thangaratinam, Shakila, et al. “Association between thyroid autoantibodies and miscarriage and preterm birth: meta-analysis of evidence.” Bmj 342 (2011): d2616.
This systematic review was conducted with a prospective protocol with widely recommended methods.15
Conclusion The presence of maternal thyroid autoantibodies is strongly associated with miscarriage and preterm delivery. There is evidence that treatment with levothyroxine can attenuate the risks.
What is already known on this topic
Thyroid autoantibodies are relatively common in women of reproductive age
Thyroid autoimmunity might be associated with adverse pregnancy outcomes
What this study adds
In women with normal thyroid function and thyroid autoantibodies the risk of miscarriage is more than tripled and the risk of preterm birth is doubled
Treatment with levothyroxine can halve the risk of miscarriage in women with normal thyroid function and thyroid autoantibodies
=============
12) http://acb.sagepub.com/content/53/4/421.short
Thyroxine replacement: a clinical endocrinologist’s viewpoint
V Eligar1 PN Taylor1 OE Okosieme1,2⇑ GP Leese3 CM Dayan1 1Thyroid Research Group, Institute of Molecular and Experimental Medicine, School of Medicine, Cardiff University, Cardiff, UK 2Endocrine and Diabetes, Department Prince Charles Hospital, Cwm Taf University Health Board Merthyr Tydfil, UK
3Department of Medicine, University of Dundee, Ninewells Hospital, Dundee, UK
OE Okosieme, University Hospital of Wales Cardiff, UK. Email: OkosiemeOE@Cardiff.ac.uk
Background Hypothyroidism affects 2–5% of the general population. Patients with uncorrected disease suffer significant morbidity and have an increased risk of cardiovascular disease and neurocognitive impairment. Levothyroxine, the treatment of choice, is inexpensive, easy to administer and in most cases restores well-being while normalizing thyroid function. However, 30–50% of individuals on levothyroxine are either over-treated or under-treated and others remain dissatisfied with treatment despite achieving thyroid hormone concentrations within the laboratory reference interval.
Methods This review is based on a systematic search of the literature for controlled trials, systematic reviews, guideline papers and cohort studies addressing best practice in thyroid hormone replacement.
Results Recent decades have seen improvements in patient management strategies driven by a better appreciation of levothyroxine pharmacokinetics. However, aspects of therapy such as the optimal timing of medication, strategies to overcome treatment non-adherence and target thyroid stimulating hormone concentrations in pregnancy and in patients with differentiated thyroid cancer remain challenging. Furthermore, there is now a substantial body of literature on common genetic variations in the deiodinases and thyroid hormone transporters and their role in the local regulation of thyroid hormone delivery. The benefits of combination therapy with liothyronine and levothyroxine are uncertain, and while it is theoretically probable that subsets of genetically predisposed individuals will benefit from combination therapy the existing evidence is as yet limited.
Conclusion Despite the availability of thyroid hormone replacement for more than a century, there are still substantial challenges in practice and opportunities to improve treatment outcomes.
13) http://arbl.cvmbs.colostate.edu/hbooks/pathphys/endocrine/thyroid/thyroid_preg.html
Thyroid Hormones: Pregnancy and Fetal Development
Thyroid hormones are critical for development of the fetal and neonatal brain, as well as for many other aspects of pregnancy and fetal growth. Hypothyroidism in either the mother or fetus frequently results in fetal disease; in humans, this includes a high incidence of mental retardation.
Isolated maternal hypothyroidism: Overt maternal hypothyroidism typically is not a significant cause of fetal disease because it usually is associated with infertility. When pregnancy does occur, there is increased risk of intrauterine fetal death and gestational hypertension. Subclincial hypothyroidism is increasingly being recognized as a cause of developmental disease – this is a rather scary situation. Several investigators have found that mild maternal hypothyroidism, diagnosed only retrospectively from banked serum, may adversely affect the fetus, leading in children to such effects as slightly lower performance on IQ tests and difficulties with schoolwork. The most common cause of subclinical hypothyroidism is autoimmune disease, and it is known that anti-thyroid antibodies cross the human placenta. Thus, the cause of this disorder may be a passive immune attack on the fetal thyroid gland.
===============================
14) http://press.endocrine.org/doi/full/10.1210/jc.2012-4249
http://ecite.utas.edu.au/99264
Hynes, Kristen L., et al. “Mild iodine deficiency during pregnancy is associated with reduced educational outcomes in the offspring: 9-year follow-up of the gestational iodine cohort.” The Journal of Clinical Endocrinology & Metabolism 98.5 (2013): 1954-1962.
Iodine is essential for neurodevelopment in utero and in childhood, with deficiency being a major cause of preventable intellectual impairment (1). The serious neurodevelopmental consequences of severe iodine deficiency (ID) on the fetus are well documented and include cretinism, which manifests as motor, cognitive, and auditory defects (2). ID, however, results in a spectrum of disorders with many speculating that even mild maternal ID has subtle impacts on fetal development. Recent reviews are not conclusive as to whether low maternal dietary iodine intake in areas of mild deficiency leads to measurable effects on cognition and neurodevelopment of the offspring (3, 4).
Clinical trials of iodine supplementation in pregnancy in regions of mild ID have typically focused on positive changes in maternal and fetal thyroid function and volumes but have not examined long-term developmental consequences in the offspring. To our knowledge, there are only three studies reporting neurodevelopmental outcomes in offspring after supplementation of mothers with mild ID. Berbel et al (5) reported significantly delayed neurobehavioral performance in children (aged 18 months) if their mothers did not receive iodine supplementation by 4 to 6 weeks of gestation. Similarly, Velasco et al (6) found that children (aged 3–18 months) had higher psychomotor development scores if their mothers were given supplements from the first trimester. Both interventions provide preliminary evidence that even mild gestational ID may have an adverse impact on fetal neurodevelopment and subsequent infant functioning. In contrast, Murcia et al (7) reported that higher maternal intake of iodine-containing supplements was associated with lower scores on the Psychomotor Development Index of the Bayley Scales of Infant Development in their children (aged 1 year).
In addition to gestational studies, there is increasing evidence from observational population studies that less severe cognitive and motor impairment occurs in apparently normal individuals from areas of ID (8). Children without cretinism from iodine-deficient regions of Iran were found to have growth retardation and neurological, auditory, and psychomotor impairments (9). Boyages et al (10) reported impaired intellectual and neuromotor development in apparently normal Chinese children, with a shift in the distribution of cognitive skills to a lower level. Furthermore, randomized controlled trial data show that postgestational supplementation can lead to significantly improved mental performance of children from areas of mild (11), moderate (12), and severe ID (13).
We compared educational outcomes of children (aged 9 years) born to women assessed as being iodine deficient (urinary iodine concentration [UIC]
===
15) http://www.thyroidmanager.org/question/repeated-miscarriages-in-a-young-woman-with-hashimoto%E2s-thyroiditis-and-antibodies/
Repeated Miscarriages in a Young Woman with Hashimoto’s Thyroiditis and Antibodies Last Updated: March 5, 2008 · Leslie J. DeGroot, M.D.
Question
This is a 32 yr old female who first saw me 3/7/7 when she was 8 weeks IUP, G4M3. First pregnacy was 5yrs ago FTND. Subsequent 3 miscarriages at 6-8wks IUP. Hypothyroidism diagnosed 3yrs ago, not treated for reasons unclear. 6/06 she was started on LT4 50 mcg, gradually increased to 100mcg by 2/07. When I saw her 3/7/7 – TSH was 6.9 (1st trim N- 0.3-4.5), FT4-1.3, TPO> 1000, TGAb>3000, TSI – 132 (N 1000, TGAb1050. I reduced her LT4 back to 100mcg/day.
She also had a tennis ball sized fibroid which was subsequently removed. She has also had extensive testing by her reproductive endo, for etiology for her miscarriages, all which seem negative.
She wants to conceive again.
Since 11/07 her TFT have been normal on LT4 88mcg/day. 2/07 – TSH- 2.87, FT4 1.4, T3-122, TPO>1000, TGAb> 3000.
She weighs 123lbs, and was hyperthyroid on 100mcg LT4.So, I have not changed her current dose.
Is she a candidate for IVIG? Is there anything else I can do from endo standpoint to reduce her risk for miscarriage? What would you advice her?
Radha Reddy, MD
Rancho Cucamonga CA
Response
I am not too familiar with the medical phraseology used in the U.S. when presenting case histories, but I think I understood correctly that this patient has been pregnant 4 times, with three previous miscarriages, and a fourth – and last miscarriage – during her most recent pregnancy in 2007. Obviously, she also has chronic autoimmune thyroiditis, with hypothyroidism diagnosed a couple of years ago. It is not clear to me whether the 3 previous miscarriages took place while she was an untreated hypothyroid patient or whether the obstetrical history occurred before that period (where, by the way, she may also have already been hypothyroid, without a diagnosis). In her most recent pregnancy, the patient received L-thyroxine ‘almost’ from the onset of gestation. However, and despite increasing her l-T4 dosage, the “best” TSH obtained was still clearly suboptimal in the first trimester (6.9 mU/L). After that, she miscarried once again. Finally, the antibody data indicate high titers of anti-Tg (>1000-3000) and anti-TPO (>1000) Abs and a positive TBII value (30% TSH binding inhibition).
Comments:
1) This is the sad – but not unusual – story of those patients who miscarry early (in the first trimester) and repeatedly, who have autoimmune thyroiditis and a not well-controlled thyroid function. Most studies on recurrent abortion in such ‘thyroid’ cases indicate that the best that can be done to help them is to make sure that their thyroid function is perfectly equilibrated before they become pregnant (serum TSH below 2.5 mU/L is probably the best target). In my own practice, I tend to titrate them even ‘higher’, to obtain a serum TSH around 1 mU/L. As soon as they become pregnant (spontaneously or medically-assisted), their thyroid function tests need to be monitored extremely closely to make sure that thyroid function remains entirely normal. This can only be achieved by sequential monitoring (every three-four weeks) of serum free T4 and TSH, with rapid (or even anticipated, as I like to do) increments in L-T4 dosage, and a close follow up until 24 weeks gestation, at least.
2) If this Hashimoto patient also has TSH-receptor antibodies (again from my understanding of the data presented), she may well be one of those rare cases with blocking-type TSHR-Abs. In principle, this should not affect the mother other than enhancing the risk of hypothyroidism, but could constitute a risk for fetal thyroid function during the second half of pregnancy (if she ever gets to that point !).
3) She may well be a candidate for IVIG (in addition to L-T4?). This decision is usually taken by our Ob-Gyn colleagues. The rate of pregnancy success with IVIG in the study by E. Vaquero (Amer J Reproductive Immunology in 2000) was improved (54.5%) but less than with l-T4 administration (81.2%). However, that study was not randomized nor controlled and the number of cases in each branch was small (see my Editorial with this article on pages 202-203).
4) I have followed personally a small number of women with the similar difficult medical conditions. Some have undergone medically-assisted procreation, some have even eventually adopted children, and despite these heavy antecedents, we have witnessed a few (but remarkable) successes since some women finally achieved natural conception and successful outcome of pregnancy (after many failed attempts) by treating adequately their Hashimoto’s disease. Thus, there is still hope since the patient is only 32 years of age, but this of course is not to say that success is obtained in all those cases !!
I hope my comments will be helpful to you.
Prof Daniel Glinoer
University of Brussels
16) https://www.holtorfmed.com/thyroid-miscarriage/
Subclinical Hypothyroidism and Thyroid Antibodies Increase Risk of Early Miscarriage . by Holtorf Medical Group
17) http://www.stopthethyroidmadness.com/2012/11/28/hypothyroidism-pregnancy-dangerous/
Ladies: Hypothyroidism in pregnancy can be dangerous, says this woman who suffered a miscarriage
November 28, 2012 By Janie Bowthorpe
18) Endocrine Society (2012, June 23). Mild thyroid dysfunction in early pregnancy linked to serious complication. Newswise. Retrieved July 3, 2012 from http://www.newswise.com/articles/mild-thyroid-dysfunction-in-early-pregnancy-linked-to-serious-complications
19) Allan, W.C., J.E. Haddow, G.E. Palomaki, J.R. Williams, M.L. Mitchell, R.J. Hermos, J.D. Faix, R.Z. Klein. Maternal thyroid deficiency and pregnancy complications: implications for population screening. J Med Screen 2000; 7:127-130. Retrieved from http://171.66.127.126/content/7/3/127.full.pdf
20) Rao VR, Lakshmi A, Sadhnani MD. Prevalence of hypothyroidism in recurrent pregnancy loss in first trimester. Indian J Med Sci 2008;62:357-61. Retrieved from http://www.indianjmedsci.org/text.asp?2008/62/9/357/43122
21) http://drclark.typepad.com/dr_david_clark/2011/11/thyroid-antibodies-and-risk-of-miscarriage-premature-birth.html
Thyroid Antibodies and Risk of Miscarriage, Premature Birth
TriangleThyroidDoctor.com
Dr. David Clark, DC -Center for Low Thyroid Solutions Durham, NC- explains a hidden cause of why many women suffer miscarriages and premature births.
Link to this article: http://wp.me/p3gFbV-3UK
Jeffrey Dach MD
7450 Griffin Road Suite 190
Davie, Fl 33314
954-792-4663
www.jeffreydachmd.com
http://www.drdach.com
http://www.naturalmedicine101.com
http://www.bioidenticalhormones101.com
http://www.truemedmd.com
The reader is advised to discuss the comments on these pages with his/her personal physicians and to only act upon the advice of his/her personal physician. Also note that concerning an answer which appears as an electronically posted question, I am NOT creating a physician — patient relationship. Although identities will remain confidential as much as possible, as I can not control the media, I can not take responsibility for any breaches of confidentiality that may occur.
Copyright (c) 2016 Jeffrey Dach MD All Rights Reserved. This article may be reproduced on the internet without permission, provided there is a link to this page and proper credit is given.
FAIR USE NOTICE: This site contains copyrighted material the use of which has not always been specifically authorized by the copyright owner. We are making such material available in our efforts to advance understanding of issues of significance. We believe this constitutes a ‘fair use’ of any such copyrighted material as provided for in section 107 of the US Copyright Law. In accordance with Title 17 U.S.C. Section 107, the material on this site is distributed without profit to those who have expressed a prior interest in receiving the included information for research and educational purposes.
Serving Areas of: Hollywood, Aventura, Miami, Fort Lauderdale, Pembroke Pines, Miramar, Davie, Coral Springs, Cooper City, Sunshine Ranches, Hallandale, Surfside, Miami Beach, Sunny Isles, Normandy Isles, Coral Gables, Hialeah, Golden Beach ,Kendall,sunrise, coral springs, parkland,pompano, boca raton, palm beach, weston, dania beach, tamarac, oakland park, boynton beach, delray,lake worth,wellington,plantation.
The post Low Thyroid, Hashimotos and Pregnancy appeared first on Jeffrey Dach MD .
November 4, 2016
Can Chronic Stress Cause Cancer ?
 Chronic Stress – Nervous Breakdown and Catatonia
Chronic Stress – Nervous Breakdown and Catatonia
The classic 1949 war movie, “Twelve Oclock High” starring Gregory Peck, reveals the effect of chronic stress on B-17 pilots during the war. After many weeks of stressful daylight bombing raids, Gregory Peck suffers a nervous breakdown, and is carried away in a catatonic state. I was impressed with this brutally honest depiction of the effects of chronic stress in war time. (left image courtesy of Bantam Books)
Chronic Stress is a Bad Thing
Chronic stress is undoubtedly a bad thing for our health because of release of massive adrenal hormones called catecholamines. This is extremely deleterious to our immune system, and increases our susceptibility to viral infection and delays wound healing. (1-2) Chronic stress causes release of pro-inflammatory cytokine implicated in cardiovascular disease, osteoporosis, arthritis, type 2 diabetes, gastric ulcer, as well as cancer (2) This leads us to the main question of the article, can chronic stress cause cancer? Let’s examine an animal model of chronic stress to answer this question.
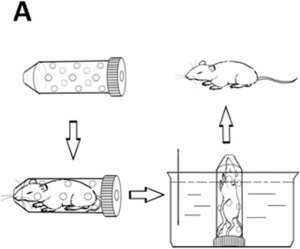 Animal Model of Chronic Stress
Animal Model of Chronic Stress
The animal model of chronic stress involves restraining mice in narrow tubes for a few hours every day. To make matters worse, the mice may be immersed in cold water.
image at left courtesy of Zhang, Fang, et al. “acute gastric injury in mice: ” Scientific reports 6 (2016).
Does Chronic Stress Causes Cancer ?
Dr Donald Lamkin used restraint stress in mice to answer the question, does chronic stress cause cancer?(3) Dr Lamkin’s 2012 study published in Brain Behavior showed that mice suffering from restraint stress (Red Ellipse in below image) had accelerated progression of cancer compared to controls (Green Ellipse). This effect was abrogated by giving the mice a Beta-Blocker drug called propranolol, which blocks the activation of the sympathetic nervous system. (see image below). The Propranolol treated mice actually showed regression of cancer compared to controls. Thus proving that beta-adrenergic stimulation drives cancer growth, and by blocking the effect of chronic stress with a beta blocker drug, we can slow the progression of cancer..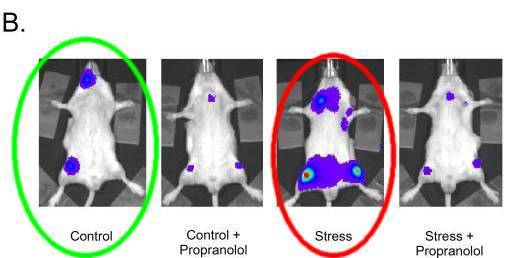 Fig 3 B Beta-adrenergic signaling in stress-enhanced Acute Lymphoblastic Leukemia progression. Mice were injected with cancer cells tagged with fluorescent marker (blue spots)Green Ellipse shows control mice NO STRESS, injected with cancer cells. Red Ellipse shows STRESSED mice with increased cancer growth compared to controls. Propranolol treated mice (Beta Blocker) had actual regression of cancer compared to controls. Courtesy of Lamkin, Donald M., et al. (3)
Fig 3 B Beta-adrenergic signaling in stress-enhanced Acute Lymphoblastic Leukemia progression. Mice were injected with cancer cells tagged with fluorescent marker (blue spots)Green Ellipse shows control mice NO STRESS, injected with cancer cells. Red Ellipse shows STRESSED mice with increased cancer growth compared to controls. Propranolol treated mice (Beta Blocker) had actual regression of cancer compared to controls. Courtesy of Lamkin, Donald M., et al. (3)
How does stress produces Beta-Adrenergic nervous system stimulation?
Chronic stress stimulates the adrenal medulla to secrete massive amounts of the catecholamines, epinephrine and norepinephrine. These stress hormones stimulate the Beta Adrenergic receptors in the nervous system, as well as in cancer cells.
Mobile cancer cells will frequently migrate to the adrenal glands, seeking the adrenal medulla which secretes high concentration of catecholamines thus causing large adrenal masses. See image below.
Adrenal Metastatic Disease is Quite Common
Above Image: Adrenal lymphoma CAT scan. (a) Both Adrenals replaced by large masses (white arrows) (b) bulky retro-peritoneal nodal masses with renal invasion (black arrows) Courtesy of Indian Journal of Endocrinology and Metabolism
REVIEW ARTICLE 2015 Volume 19 Issue 1 Page : 16-24
Adrenal imaging (Part 2): Medullary and secondary adrenal lesions
Ekta Dhamija, Ananya Panda, Chandan J Das, AK Gupta Department of Radiodiagnosis, All India Institute of Medical Sciences, Ansari Nagar, New Delhi, India
Reducing Diet to Down Regulate the Sympathetic Nervous System
In addition to the use of Beta Blocker Drugs, the sympathetic nervous system can be down regulated by dietary interventions as advocated by Nicholas Gonzalez MD as a part of his cancer treatment protocol.(19-22).
Conclusion: Chronic Stress is unhealthy because it releases catecholamines which activate the Sympathetic Nervous system. This in turn, stimulates cancer cell growth.
Articles with Related Interest: Adrenal Fatigue
Jeffrey Dach MD
7450 Griffin Road Suite 190
Davie, Florida 33314
954-792-4663
Links and References
free pdf
1) Glaser, Ronald, and Janice K. Kiecolt-Glaser. “Stress-induced immune dysfunction: implications for health.” Nature Reviews Immunology 5.3 (2005): 243-251. stress-induced-immune-dysfunction-implications-for-health-nature-reviews-immunology-2005-glaser-ronald
free pdf
Reiche, Edna Maria Vissoci, Sandra Odebrecht Vargas Nunes, and Helena Kaminami Morimoto. “Stress, depression, the immune system, and cancer.” The lancet oncology 5.10 (2004): 617-625.stress-depression-the-immune-system-cancer-lancet-oncology-reiche-edna-maria-2004
stress promotes cancer – Nice flourescent mouse images
3) Lamkin, Donald M., et al. “Chronic stress enhances progression of acute lymphoblastic leukemia via ß-adrenergic signaling.” Brain, behavior, and immunity 26.4 (2012): 635-641.
Clinical studies suggest that stress-related biobehavioral factors can accelerate the progression of hematopoietic cancers such as acute lymphoblastic leukemia (ALL), but it is unclear whether such effects are causal or what biological pathways mediate such effects. Given the network of sympathetic nervous system (SNS) fibers that innervates the bone marrow to regulate normal (non-leukemic) hematopoietic progenitor cells, we tested the possibility that stress-induced SNS signaling might also affect ALL progression. In an orthotopic mouse model, Nalm-6 human pre-B ALL cells were transduced with the luciferase gene for longitudinal bioluminescent imaging and injected i.v. into male SCID mice for bone marrow engraftment. Two weeks of daily restraint stress significantly enhanced ALL tumor burden and dissemination in comparison to controls, and this effect was blocked by the ß-adrenergic antagonist, propranolol. Although Nalm-6 ALL cells expressed mRNA for ß1- and ß3-adrenergic receptors, they showed no evidence of cAMP signaling in response to norepinephrine, and norepinephrine failed to enhance Nalm-6 proliferation in vitro. These results show that chronic stress can accelerate the progression of human pre-B ALL tumor load via a ß-adrenergic signaling pathway that likely involves indirect regulation of ALL biology via alterations in the function of other host cell types such as immune cells or the bone marrow microenvironment.
Chronic restraint stress significantly enhanced pre-B ALL tumor burden and dissemination in a well-established mouse xenograft model of the most prevalent form of human pediatric leukemia. Pharmacologic inhibition studies showed that stress effects were mediated by ß-adrenergic signaling in vivo
Mechanistic investigations have documented a key role of ß-adrenergic signaling in mediating stress effects on progression of several types of solid tumor (Sloan et al., 2010; Stefanski & Ben-Eliyahu, 1996; Thaker et al., 2006).
the present results raise the possibility that cancer-related anxiety might contribute to disease recurrence and that pharmacologic inhibition of such effects at the level of the ß-adrenergic receptor may represent an effective strategy for managing those effects in patients with pre-B ALL who are in remission or still have active disease.
=================================================
Beta Blockers and Cancer
nice review
4) http://www.tandfonline.com/doi/full/10.1517/13543784.2013.825250
Nagaraja, Archana S., et al. “ß-blockers: a new role in cancer chemotherapy?.” Expert opinion on investigational drugs 22.11 (2013): 1359-1363.
ß-blockers are a class of drugs that are widely used in treating cardiac, respiratory and other ailments. They act by blocking ß-adrenergic receptor-mediated signaling. Studies in various cancers have shown that patients taking a ß-blocker have higher survival and lower recurrence and metastasis rates. This is supported by several preclinical and in vitro studies showing that adrenergic activation modulates apoptosis, promotes angiogenesis and other cancer hallmarks, and these effects can be abrogated by ß-blockers. These studies provide a rationale for the use of ß-blockers as adjuvants with cancer chemotherapy. However, all published studies so far are retrospective and most do not take into account the specific ß-blocker used or address which is most likely to benefit cancer patients. The published epidemiological studies are correlative and have not examined the adrenergic receptor status of the tumors. Knowledge of the ß-adrenergic receptor status of tumor cells is essential in choosing the best ß-blocker for adjuvant therapy. A comprehensive, prospective study is necessary to definitively prove the utility of using ß-blockers with chemotherapy and to identify the specific ß-blocker most likely to benefit patients with cancer.
There are three subtypes of ß-adrenergic receptors, designated ADRB1, ADRB2 and ADRB3, which are encoded by genes located on chromosomes 10, 5 and 8, respectively. ADRBs are activated by catecholamines (such as noradrenaline and adrenaline) that are secreted largely in response to sympathetic nervous system stimulation, resulting in the ‘fight-or-flight’ response. Although acute activation of adrenergic receptors has been shown to be beneficial for human health, prolonged activation is associated with decreased immune function, heart failure, arrhythmia and hypertension. Sustained activation can be a result of altered behavioral states such as those seen in depression, anxiety and chronic stress.
5) https://www.ncbi.nlm.nih.gov/pubmed/23912960
Breast Cancer Res Treat. 2013 Aug;140(3):567-75. doi: 10.1007/s10549-013-2654-3. Epub 2013 Aug 3. Therapeutic effect of ß-blockers in triple-negative breast cancer postmenopausal women. Botteri E1, Munzone E, Rotmensz N, Cipolla C, De Giorgi V, Santillo B, Zanelotti A, Adamoli L, Colleoni M, Viale G, Goldhirsch A, Gandini S.
Beta-blockers (BB) drugs have been used for decades worldwide, mainly to treat hypertension. However, in recent epidemiological studies, BBs were suggested to improve cancer prognosis. In the wake of this evidence, we evaluated the possible therapeutic effect of BBs in triple-negative breast cancer (TNBC) patients. We identified 800 postmenopausal women operated between 1997 and 2008 for early primary TNBC. The effect of BB intake on the risk of breast cancer (BC) recurrence and death was evaluated through competing risk and Cox regression survival models. At cancer diagnosis, 74 (9.3 %) women out of 800 were BBs users. Median age was 62 years in BB users and 59 years in non-users (P = 0.02). BB users and non-users were similarly distributed by all tumor characteristics. The 5-year cumulative incidence of BC-related events was 13.6 % in BB users and 27.9 % in non-users (P = 0.02). The beneficial impact of BBs remained statistically significant at multivariable analysis (HR, 0.52; 95 % CI 0.28-0.97), after the adjustment for age, tumor stage, and treatment, peritumoral vascular invasion and use of other antihypertensive drugs, antithrombotics, and statins. Adjusted HRs for metastases and for BC deaths were 0.32 (95 % CI 0.12-0.90) and 0.42 (95 % CI 0.18-0.97), respectively, in favor of BBs. Hypertension, other antihypertensive drugs, antithrombotics, and statins did not impact prognosis. In this series of postmenopausal TNBC patients, BB intake was associated with a significantly decreased risk of BC-related recurrence, metastasis, and BC death. Innovative therapeutic strategies including BBs should be urgently explored in cancer patients.
6) https://www.ncbi.nlm.nih.gov/pubmed/21632501
J Clin Oncol. 2011 Jul 1;29(19):2645-52. Beta-blocker use is associated with improved relapse-free survival in patients with triple-negative breast cancer.
Melhem-Bertrandt A1, Chavez-Macgregor M, Lei X, Brown EN, Lee RT, Meric-Bernstam F, Sood AK, Conzen SD, Hortobagyi GN, Gonzalez-Angulo AM.
1The University of Texas MD Anderson Cancer Center, Houston, TX, 77030, USA.
To examine the association between beta-blocker (BB) intake, pathologic complete response (pCR) rates, and survival outcomes in patients with breast cancer treated with neoadjuvant chemotherapy.
PATIENTS AND METHODS:We retrospectively reviewed 1,413 patients with breast cancer who received neoadjuvant chemotherapy between 1995 and 2007. Patients taking BBs at the start of neoadjuvant therapy were compared with patients with no BB intake. Rates of pCR between the groups were compared using a ?² test. Cox proportional hazards models were fitted to determine the association between BB intake, relapse-free survival (RFS), and overall survival (OS).
RESULTS:Patients who used BBs (n = 102) were compared with patients (n = 1,311) who did not. Patients receiving BBs tended to be older and obese (P < .001). The proportion of pCR was not significantly different between the groups (P = .48). After adjustment for age, race, stage, grade, receptor status, lymphovascular invasion, body mass index, diabetes, hypertension, and angiotensin-converting enzyme inhibitor use, BB intake was associated with a significantly better RFS (hazard ratio [HR], 0.52; 95% CI, 0.31 to 0.88) but not OS (P = .09). Among patients with triple-negative breast cancer (TNBC; n = 377), BB intake was associated with improved RFS (HR, 0.30; 95% CI, 0.10 to 0.87;P = .027) but not OS (HR, 0.35; 95% CI, 0.12 to 1.00;P = .05).
CONCLUSION:In this study, BB intake was associated with improved RFS in all patients with breast cancer and in patients with TNBC. Additional studies evaluating the potential benefits of beta-adrenergic blockade on breast cancer recurrence with a focus on TNBC are warranted.
7) https://www.ncbi.nlm.nih.gov/pubmed/26516037
Clin Breast Cancer. 2015 Dec;15(6):426-31. doi: 10.1016/j.clbc.2015.07.001. Epub 2015 Jul 10.
ß-Blockers Reduce Breast Cancer Recurrence and Breast Cancer Death: A Meta-Analysis.
Childers WK1, Hollenbeak CS2, Cheriyath P3.
The normal physiologic stress mechanism, mediated by the sympathetic nervous system, causes a release of the neurotransmitters epinephrine and norepinephrine. Preclinical data have demonstrated an effect on tumor progression and metastasis via the sympathetic nervous system mediated primarily through the ß-adrenergic receptor (ß-AR) pathway. In vitro data have shown an increase in tumor growth, migration, tumor angiogenesis, and metastatic spread in breast cancer through activation of the ß-AR. Retrospective cohort studies on the clinical outcomes of ß-blockers in breast cancer outcomes showed no clear consensus. The purpose of this study was to perform a systematic review and meta-analysis of the effect of ß-blockers on breast cancer outcomes. A systematic review was performed using the Cochrane library and PubMed. Publications between the dates of January 2010 and December 2013 were identified. Available hazard ratios (HRs) were extracted for breast cancer recurrence, breast cancer death, and all-cause mortality and pooled using a random effects meta-analysis. A total of 7 studies contained results for at least 1 of the outcomes of breast cancer recurrence, breast cancer death, or all-cause mortality in breast cancer patients receiving ß-blockers. In the 5 studies that contained results for breast cancer recurrence, there was no statistically significant risk reduction (HR, 0.67; 95% confidence interval [CI], 0.39-1.13). Breast cancer death results were contained in 4 studies, which also suggested a significant reduction in risk (HR, 0.50; 95% CI, 0.32-0.80). Among the 4 studies that reported all-cause mortality, there was no significant effect of ß-blockers on risk (HR, 1.02; 95% CI, 0.75-1.37). Results of this systematic review and meta-analysis suggest that the use of ß-blockers significantly reduced risk of breast cancer death among women with breast cancer.
!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!
8) http://www.mdpi.com/2073-4409/5/1/2/htm
Entschladen, Frank, Dane A. Thyssen, and David W. Drell. “Re-Use of Established Drugs for Anti-Metastatic Indications.” Cells 5.1 (2016): 2.
To date, the by far most striking discovery in the context of drug repurposing in oncology is the anti-metastatic function of beta-blockers
—
beta blocker and ovarian cancer 2015
9) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4575637/
Cancer. 2015 Oct 1; 121(19): 3444–3451.
Published online 2015 Aug 24. doi: 10.1002/cncr.29392
PMCID: PMC4575637
NIHMSID: NIHMS717272
Clinical Impact of Selective and Non-selective Beta Blockers on Survival in Ovarian Cancer Patients
Jack L. Watkins,1,* Premal H. Thaker,2,* Alpa M. Nick,3 Lois M. Ramondetta,3 Sanjeev Kumar,4 Diana L. Urbauer,5 Koji Matsuo,6 Kathryn Squires,2 Susan K. Lutgendorf,7 Pedro T. Ramirez,3 and Anil K. Sood3,8,
Preclinical evidence suggests that sustained adrenergic activation can promote ovarian cancer growth and metastasis. We examined the impact of beta-adrenergic blockade on clinical outcome of women with epithelial ovarian, primary peritoneal or fallopian tube cancers (collectively, EOC).
METHODS A multicenter review of 1,425 women with histopathologically confirmed EOC was performed. Comparisons were made between patients with documented beta blocker use during chemotherapy and those without beta blocker use.
RESULTS The median age of patients in this study was 63 years (range, 21–93 years). The sample included 269 patients who received beta blockers. Of those, 193 (71.7%) were receiving beta-1 adrenergic receptor (ADRB1) selective agents, and the remaining patients were receiving non-selective beta antagonists. The primary indication for beta blocker use was hypertension but also included arrhythmia and post-myocardial infarction management. For patients receiving any beta blocker, the median overall survival (OS) was 47.8 months versus42 months (P = 0.04) for non-users. The median OS based on beta blocker receptor selectivity was 94.9 months for those receiving non-selective beta blockers versus 38 months for those receiving ADRB1 selective agents (P < 0.001). Hypertension was associated with decreased OS compared to no hypertension across all groups. However, even in patients with hypertension, users of a non-selective beta blocker had a longer median OS than non-users observed (38.2 vs 90 months, P < 0.001).
CONCLUSION Use of non-selective beta blockers in epithelial ovarian cancer patients was associated with longer OS. These findings may have implications for new therapeutic approaches.
10) Yuan, Aihua, et al. “Psychological aspect of cancer: From stressor to cancer progression (Review).” Experimental and therapeutic medicine 1.1 (2010): 13-18.
Substantial evidence indicates that psychological stress can influence the incidence and progression of cancers, and adequate psychotherapies are beneficial to cancer patients. Recently, the mechanisms responsible for the effects of psychological stress on cancer cells have been extensively investigated at the systemic, biochemical and molecular levels. Accumulating data indicate that the effects of psychological stress on cancer cells are mainly mediated by key stress-related mediators and their corresponding receptors in multi-fold pathways: chronic stressors act on the paraventricular nucleus and the suprachiasmatic nuclei. The effects are then transmitted through the sympathetic nervous system and the hypothalamic-pituitary-adrenal axis, amplified by the unchecked release of stress-related mediators and altered behaviors. These mediators act as immunosuppressors or mitogens in the tumor micro-environment. The converging effects of psychological stress on cancer cells finally signal through receptors of the stress mediators and cytokines to activate the intracellular pro-proliferative and pro-migratory signaling pathways, and reset the molecular clock in tumor cells. Understanding these action mechanisms of psychological stress in promoting the growth and invasion of cancer cells is crucial for devising effective interventions.
Not until the recent past few years, by using in vitro animal models and human clinical perspective study approaches, have researchers begun to uncover the complex relationship between psychosocial stress and cancer progression at the systemic, biochemical and molecular levels. Accumulating data indicate that the psychological stress caused by chronic stressors is a major risk factor for cancer occurrence, growth and metastasis (5–8).
11) Jin Shin, Kyeong, et al. “Molecular mechanisms underlying psychological stress and cancer.” Current pharmaceutical design 22.16 (2016): 2389-2402.
Curr Pharm Des. 2016;22(16):2389-402.
Psychological stress is an emotion experienced when people are under mental pressure or encounter unexpected problems. Extreme or repetitive stress increases the risk of developing human disease, including cardiovascular disease (CVD), immune diseases, mental disorders, and cancer. Several studies have shown an association between psychological stress and cancer growth and metastasis in animal models and case studies of cancer patients. Stress induces the secretion of stress-related mediators, such as catecholamine, cortisol, and oxytocin, via the activation of the hypothalamic-pituitary-adrenocortical (HPA) axis or the sympathetic nervous system (SNS). These stress-related hormones and neurotransmitters adversely affect stress-induced tumor progression and cancer therapy. Catecholamine is the primary factor that influences tumor progression. It can regulate diverse cellular signaling pathways through adrenergic receptors (ADRs), which are expressed by several types of cancer cells. Activated ADRs enhance the proliferation and invasion abilities of cancer cells, alter cell activity in the tumor microenvironment, and regulate the interaction between cancer and its microenvironment to promote tumor progression. Additionally, other stress mediators, such as glucocorticoids and oxytocin, and their cognate receptors are involved in stress-induced cancer growth and metastasis. Here, we will review how each receptor-mediated signal cascade contributes to tumor initiation and progression and discuss how we can use these molecular mechanisms for cancer therapy.
12) Cole, Steven W., et al. “Sympathetic nervous system regulation of the tumour microenvironment.” Nature Reviews Cancer 15.9 (2015): 563-572.
Experimental analyses in in vivo animal models have now shown that behavioral stress can accelerate the progression of breast, prostate, and ovarian carcinomas 35,49–52, neuroblastomas 53,54, malignant melanomas 55,56, pancreatic carcinoma 24,57, and some haematopoietic cancers such as leukaemia 58,59. In many of these experimental models, the biological effects of stress could be efficiently blocked by β-adrenergic antagonists and mimicked by pharmacologic β-agonists 14
13) Magnon, Claire. “Role of the autonomic nervous system in tumorigenesis and metastasis.” Molecular & Cellular Oncology 2.2 ( 15): e975643.
14) Gao, Guolan, et al. “Chronic stress promoted the growth of ovarian carcinoma via increasing serum levels of norepinephrine and interleukin-10 and altering nm23 and NDRG1 expression in tumor tissues in nude mice.” Bioscience trends 7.1 (2013): 56-63.
.
The current study aimed to examine the effects and underlying mechanisms of chronic psychological stress on the growth of ovarian carcinoma. Human ovarian carcinoma cells SKOV-3 were subcutaneously inoculated into nude mice to establish an ectopic mouse model. The animals were experimentally stressed 6 h daily for a total of 42 days with a physical restraint system. We examined the effects of stress on the growth of tumor cells that were inoculated 7 days after the initiation of stress. The growth of SKOV-3 xenografts in the stress group showed a more rapid trend than that in the control. The mean weight of tumors that were removed at the end of the experiment increased by 71.7% in the stress group as compared to the control. In order to explore the underlying mechanisms, we first determined the serum levels of norepinephrine (NE) and interleukin 10 (IL-10) in the mice using an enzyme-linked immunoabsorbent assay (ELISA) and then analyzed protein expression profiles of SKOV-3 xenografts using a proteomics-based approach combining two-dimensional electrophoresis with ultra performance liquid chromatography-electrospray tandem mass spectrometry (nanoUPLC-ESI-MS/MS). Results demonstrated that serum levels of NE and IL-10 were obviously increased in the mice receiving 6 h of immobilization daily for 42 days. In xenografts exposed to stress, a tumor promoting protein nm23 was significantly upregulated while a tumor suppressing protein NDRG1 was obviously downregulated, which were confirmed by subsequent Western blot analysis. Results obtained in the current study suggested that chronic stress promoted the growth of ovarian carcinoma in nude mice through increasing serum levels of NE and IL-10 and altering nm23 and NDRG1 expression in tumor tissues.
15) Krizanova, O., Petr Babula, and K. Pacak. “Stress, catecholaminergic system and cancer.” Stress 19.4 (2016): 419-428.
Stress as a modern civilization factor significantly affects our lives. While acute stress might have a positive effect on the organism, chronic stress is usually detrimental and might lead to serious health complications. It is known that stress induced by the physical environment (temperature-induced cold stress) can significantly impair the efficacy of cytotoxic chemotherapies and the anti-tumor immune response. On the other hand, epidemiological evidence has shown that patients taking drugs known as β-adrenergic antagonists (“β-blockers”), which are commonly prescribed to treat arrhythmia, hypertension, and anxiety, have significantly lower rates of several cancers. In this review, we summarize the current knowledge about catecholamines as important stress hormones in tumorigenesis and discuss the use of β-blockers as the potential therapeutic agents.
16) Exp Oncol. 2011 Dec;33(4):222-5. Depressive-like psychoemotional state versus acute stresses enhances Lewis lung carcinoma metastasis in C57BL/6J mice.
Amikishieva AV1, Ilnitskaya SI, Nikolin VP, Popova NA, Kaledin VI.
The effect of a depression-like status formed by chronic stress on the development of Lewis lung carcinoma metastases in C57Bl/6J mice was investigated. Two types of acute stress (restraint and social stress) were used for comparison.
METHODS:The depression-like status was induced by eight-week exposure to repeated but unpredictable stressors (chronic mild stress model) and was assessed in the forced swim test. Tumor cells were inoculated an hour after the onset of social stressor or immediately after physical or chronic stressor impacts. The number of metastases was counted 17 days after the inoculation.
RESULTS:Chronic mild stress provokes the development of a depression-like state in mice and causes a twofold increase in the number of metastases in the lungs, while both types of acute stress have no such effects.
CONCLUSION:Depressive-like psychoemotional state of animals enhances the metastasis of Lewis lung carcinoma.
17) Lamkin, Donald M., et al. “α 2-adrenergic blockade mimics the enhancing effect of chronic stress on breast cancer progression.“ Psychoneuroendocrinology 51 (2015): 262-270.
=============================
Propranolol reduces Cancer risk
18) Chang, Ping-Ying, et al. “Propranolol reduces Cancer risk: a population-based cohort study.” Medicine 94.27 (2015).
β-Blockers have been reported to exhibit potential anticancer effects in cancer cell lines and animal models. However, clinical studies have yielded inconsistent results regarding cancer outcomes and cancer risk when β-blockers were used. This study investigated the association between propranolol and cancer risk.
Between January 1, 2000 and December 31, 2011, a patient cohort was extracted from the Longitudinal Health Insurance Database 2000, a subset of the Taiwan National Health Insurance Research Database. A propranolol cohort (propranolol usage >6 months) and nonpropranolol cohort were matched using a propensity score. Cox proportional hazard models were used to estimate the hazard ratio (HR) and 95% confidence intervals (CIs) of cancer associated with propranolol treatment.
The study sample comprised 24,238 patients. After a 12-year follow-up period, the cumulative incidence for developing cancer was low in the propranolol cohort (HR: 0.75; 95% CI: 0.67–0.85; P
This study supports the proposition that propranolol can reduce the risk of head and neck, esophagus, stomach, colon, and prostate cancers. Further prospective study is necessary to confirm these
Diet – Nicholas Gonzalez / Kelly
19) Pancreatic Cancer, Proteolytic Enzyme Therapy and Detoxification
Excerpted with permission from the November 1999 Clinical Pearls News
Gonzalez NJ: Pancreatic cancer, proteolytic enzyme therapy and detoxification [excerpts].
20) Cancer and Enzyme Therapy, Dr. Kelley’s Enzyme Therapy
Dr. Nicholas Gonzalez’s Enzyme Therapy
So, whatever other effect a vegetarian diet has, in terms of autonomic nervous system function, such a diet will reduce sympathetic activity and stimulate the parasympathetic system.
A meat diet is loaded with minerals such as phosphorous and zinc, which tend to have the opposite effect. A high-meat diet stimulates the sympathetic system and tones down parasympathetic activity. Furthermore, such a diet is loaded with sulfates and phosphates that in the body are quickly converted into free acid that in turn stimulates the sympathetic nervous system while suppressing parasympathetic activity.
21) The Sympathetic and Parasympathetic Nervous Systems
Chapter 15 / Lesson 6 Transcript
Gonzalez NJ, Isaacs LL: Evaluation of pancreatic proteolytic enzyme treatment of adenocarcinoma of the pancreas, with nutrition and detoxification support. Nutr Cancer 33 (2): 117-24, 1999. [PUBMED Abstract]
22) Gonzalez N: Dr. Nicholas Gonzalez on nutritional cancer therapy: a Moneychanger interview. The Moneychanger July 1995.
—— —- —–
PATENT
23) http://www.google.ch/patents/WO200915...
Beta adrenergic receptor agonists for the treatment of b-cell proliferative disorders
WO 2009151569 A2
Zusammenfassung
24) https://www.ncbi.nlm.nih.gov/pubmed/2...
Oncol Res. 2010;19(1):45-54.
Beta-adrenergic receptors in cancer: therapeutic implications.
Pérez-Sayáns M1, Somoza-Martín JM, Barros-Angueira F, Diz PG, Gándara Rey JM, García-García A.
The beta-adrenergic receptors transduce catecholamine signals to the G protein, which through a cascade of chemical reactions in cells generates highly specific parallel signals. The beta2-adrenergic receptor (ADRB2) is the most involved in the carcinogenic processes. Previous studies have determined the relationship of ADRB2 with various aspects related to cancer. Basically, it seems to be related with cell proliferation and apoptosis, chemotaxis, development of metastasis and tumor growth, and angiogenesis. The purpose of this review is to update the implications of these receptors in the pathogenesis of cancer and study the possible application of agonist drugs and/or antagonists in antitumor therapy.
25) https://www.ncbi.nlm.nih.gov/pmc/arti...
Cole, Steven W., and Anil K. Sood. “Molecular pathways: beta-adrenergic signaling in cancer.” Clinical cancer research 18.5 (2012): 1201-1206.
β-adrenergic signaling has been found to regulate multiple cellular processes that contribute to the initiation and progression of cancer, including inflammation, angiogenesis, apoptosis/anoikis, cell motility and trafficking, activation of tumor-associated viruses, DNA damage repair, cellular immune response, and epithelial-mesenchymal transition. In several experimental cancer models, activation of the sympathetic nervous system promotes the metastasis of solid epithelial tumors and the dissemination of hematopoietic malignancies via β-adrenoreceptor-mediated activation of PKA and EPAC signaling pathways. Within the tumor microenvironment, β-adrenergic receptors on tumor and stromal cells are activated by catecholamines from local sympathetic nerve fibers (norepinephrine) and circulating blood (epinephrine). Tumor-associated macrophages are emerging as key targets of β-adrenergic regulation in several cancer contexts. Sympathetic nervous system regulation of cancer cell biology and the tumor microenvironment has clarified the molecular basis for long-suspected relationships between stress and cancer progression and now suggest a highly leveraged target for therapeutic intervention. Epidemiologic studies have linked the use of β-blockers to reduced rates of progression for several solid tumors, and pre-clinical pharmacologic and biomarker studies are now laying the groundwork for translation of β-blockade as a novel adjuvant to existing therapeutic strategies in clinical oncology.
Weddle, D. L., et al. “β-Adrenergic growth regulation of human cancer cell lines derived from pancreatic ductal carcinomas.” Carcinogenesis 22.3 (2001): 473-479.
pdf
Eng, Jason W-L., et al. “A nervous tumor microenvironment: the impact of adrenergic stress on cancer cells, immunosuppression, and immunotherapeutic response.” Cancer Immunology, Immunotherapy 63.11 (2014): 1115-1128.
pdf
Powe, D. G., et al. “Alpha-and beta-adrenergic receptor (AR) protein expression is associated with poor clinical outcome in breast cancer: an immunohistochemical study.” Breast cancer research and treatment 130.2 (2011): 457-463.
link to this article: http://wp.me/p3gFbV-3TE
The post Can Chronic Stress Cause Cancer ? appeared first on Jeffrey Dach MD .
October 24, 2016
Hypothyroid Risks for Infection
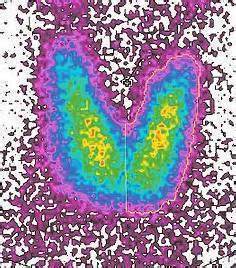 Low Thyroid Condition Predisposes to Death From Infectious Disease
Low Thyroid Condition Predisposes to Death From Infectious Disease
The greatest American Endocrinologist, Broda Barnes MD, was an astute clinician who observed the low thyroid condition is associated with reduced immunity to infectious diseases. These teachings of Dr Barnes (1906-1988) can be found in his book, Hypothyroidm, the Unsuspected Illness. Unfortunately, the mainstream endocrinologists of his time rejected Dr. Barnes teachings, including this one about hypothyroidism associated with reduced immunity.
A new study using hypothyroid mice shows that Dr Barnes was right all along.
The Hypothyroid Mouse and Infectious Disease
The ability to battle and withstand an infectious insult was studied in hypothyroid mice in 2014 by Dr Cristiana Perrotta from Milan Italy entitled,”The thyroid hormone triiodothyronine controls macrophage maturation and functions: protective role during inflammation.” (1)
In this hypothyroid mouse model,” T3 (thyroid hormone tri-iodothyronine) significantly protected mice against endotoxemia induced by lipopolysaccharide i.p. injection.”(1)
 Dr Perrotta injected hypothyroid mice with gram negative bacteria lipopolysaccharide (LPS) to induce endotoxemia, and recorded the mortality of the mice over 96 hours. The hypothyroid mice had 90% mortality from the infection. However, when the hypothyroid mice were injected with T3 (thyroid hormone) for five days before gram negative endotoxemia, they were now protected from death with 70 % survival. (see Fig 10A below) from Dr Perrotta (1). Notice the T3 treated mice enjoyed the greatest survival and best outcome.
Dr Perrotta injected hypothyroid mice with gram negative bacteria lipopolysaccharide (LPS) to induce endotoxemia, and recorded the mortality of the mice over 96 hours. The hypothyroid mice had 90% mortality from the infection. However, when the hypothyroid mice were injected with T3 (thyroid hormone) for five days before gram negative endotoxemia, they were now protected from death with 70 % survival. (see Fig 10A below) from Dr Perrotta (1). Notice the T3 treated mice enjoyed the greatest survival and best outcome.
Protecting Us from Infection
I thought this was very impressive demonstration of the importance of thyroid hormone for boosting our immune system, and protecting us from infectious disease.
Jeffrey Dach MD
7450 Griffin Road Suite 180
Davie Florida 33314
954-792-4663
Articles with related Interest
Ten Reasons Why You Have A Low thyroid condition
Links and references
1) Perrotta, Cristiana, et al. “The thyroid hormone triiodothyronine controls macrophage maturation and functions: protective role during inflammation.” The American journal of pathology 184.1 (2014): 230-247.
Of interest, T3 significantly protected mice against endotoxemia induced by lipopolysaccharide i.p. injection; in these damaged animals, decreased T3 levels increased the recruited (potentially damaging) cells,
The endocrine system participates in regulating macrophage maturation, although little is known about the modulating role of the thyroid hormones. In vitro results demonstrate a negative role of one such hormone, triiodothyronine (T3), in triggering the differentiation of bone marrow-derived monocytes into unpolarized macrophages. T3-induced macrophages displayed a classically activated (M1) signature. A T3-induced M1-priming effect was also observed on polarized macrophages because T3 reverses alternatively activated (M2) activation, whereas it enhances that of M1 cells. In vivo, circulating T3 increased the content of the resident macrophages in the peritoneal cavity, whereas it reduced the content of the recruited monocyte-derived cells. Of interest, T3 significantly protected mice against endotoxemia induced by lipopolysaccharide i.p. injection; in these damaged animals, decreased T3 levels increased the recruited (potentially damaging) cells, whereas restoring T3 levels decreased recruited and increased resident (potentially beneficial) cells. These data suggest that the anti-inflammatory effect of T3 is coupled to the modulation of peritoneal macrophage content, in a context not fully explained by the M1/M2 framework. Thyroid hormone receptor expression analysis and the use of different thyroid hormone receptor antagonists suggest thyroid hormone receptor β1 as the major player mediating T3 effects on macrophages. The novel homeostatic link between thyroid hormones and the pathophysiological role of macrophages opens new perspectives on the interactions between the endocrine and immune systems.
in Vivo Inflammation Experiments
As previously reported,45 and 57 acute illness was induced by a single i.p. injection of 10 to 15 μg/g body weight of LPS (endotoxin, Escherichia coli serotype O55:B5). Survival was monitored for 96 hours. In another set of experiments, mice received a single injection i.p. of LPS for 16 hours before the isolation and flow cytometry analysis of resident peritoneal cavity cells.
Thyroid Hormone TH Levels Affect Animal Mortality and Peritoneal Macrophage Subsets during Endotoxemia
LPM and SPM differ markedly in their in vivo responses to inflammatory stimuli, 56 and M1 cells (CD14 ) have a classic proinflammatory profile; we evaluated whether alterations of TH levels affected the animal survival rate during systemic inflammation. To this end, we injected euthyroid and hypothyroid mice i.p. with LPS to induce endotoxemia, and we recorded the mortality of the animals over 96 hours. As shown in the Kaplan-Meier curve of Figure 10A, hypothyroid mice exhibited significantly increased mortality during the course of the experiment (10% survival of hypothyroid mice versus 35% survival of euthyroid mice). When injected i.p. with 0.2 μg/g body weight per day T3 for 5 days before the onset of endotoxemia, hypothyroid animals were significantly protected from death (70% survival).
Accordingly, we show that circulating T3 significantly protected mice against inflammation induced by LPS i.p. injection, a model of endotoxemia resembling sepsis.
relevant data on TH (thyroid hormone) levels as indicators of sepsis severity and predictors of mortality come from human studies. For instance, in patients with septic shock, tissue responses are orientated to decrease production and increase degradation (muscle) or decrease uptake (adipose tissue) of T3, as well as to decrease thyroid hormone actions.89 In addition, T3 levels were significantly lower in patients with sepsis compared with patients with an inflammatory response without underlying infection,90 and the levels of THs have been found to be a parameter for evaluating meningococcal septic shock severity. 91 and 92 A systematic review regarding the association between thyroid hormone abnormalities and the outcome of patients with sepsis or septic shock suggests the existence of an association between lower T3 or T4 and worse outcome,
Link to this article:http://wp.me/p3gFbV-3SW
Jeffrey Dach MD
7450 Griffin Road, Suite 180
Davie, Fl 33314
954-972-4663
www.jeffreydachmd.com
www.drdach.com
www.naturalmedicine101.com
www.bioidenticalhormones101.com
www.truemedmd.com
Web Site and Discussion Board Links:
jdach1.typepad.com/blog/
disc.yourwebapps.com/Indices/244124.html
disc.yourwebapps.com/Indices/244066.html
disc.yourwebapps.com/Indices/244067.html
disc.yourwebapps.com/Indices/244161.html
disc.yourwebapps.com/Indices/244163.html
Disclaimer click here: www.drdach.com/wst_page20.html
The reader is advised to discuss the comments on these pages with his/her personal physicians and to only act upon the advice of his/her personal physician. Also note that concerning an answer which appears as an electronically posted question, I am NOT creating a physician — patient relationship. Although identities will remain confidential as much as possible, as I can not control the media, I can not take responsibility for any breaches of confidentiality that may occur.
Copyright (c) 2016 Jeffrey Dach MD All Rights Reserved. This article may be reproduced on the internet without permission, provided there is a link to this page and proper credit is given.
FAIR USE NOTICE: This site contains copyrighted material the use of which has not always been specifically authorized by the copyright owner. We are making such material available in our efforts to advance understanding of issues of significance. We believe this constitutes a ‘fair use’ of any such copyrighted material as provided for in section 107 of the US Copyright Law. In accordance with Title 17 U.S.C. Section 107, the material on this site is distributed without profit to those who have expressed a prior interest in receiving the included information for research and educational purposes.
Serving Areas of: Hollywood, Aventura, Miami, Fort Lauderdale, Pembroke Pines, Miramar, Davie, Coral Springs, Cooper City, Sunshine Ranches, Hallandale, Surfside, Miami Beach, Sunny Isles, Normandy Isles, Coral Gables, Hialeah, Golden Beach ,Kendall,sunrise, coral springs, parkland,pompano, boca raton, palm beach, weston, dania beach, tamarac, oakland park, boynton beach, delray,lake worth,wellington,plantation.
The post Hypothyroid Risks for Infection appeared first on Jeffrey Dach MD .
Jeffrey Dach's Blog
- Jeffrey Dach's profile
- 3 followers