Leslie Glass's Blog, page 395
February 13, 2018
How To Break Up With Negative Self Talk
Self talk is that inner voice that often chatters to us about all types of things. Unfortunately, it is often negative. Negative self talk impairs our ability to cope with life’s ups and downs. Buddhists refer to this inner chatting as “monkey mind” because monkeys are always chattering about something. And while most human self talk is quiet on the outside, we may even find ourselves talking out loud. Take a minute and think about your inner and outer self talk; is it positive, negative, or both?
Self Talk Habits Form In Childhood
To see where negative self talk comes from, we have to trace its origins. Ask yourself these questions:
Did we start saying negative things to ourselves after others, such as parents and teachers, said negative things about us?
Were we raised in a household that valued perfectionism?
When we weren’t perfect, were highly criticized, and then internalized this negativity?
Did our teachers compare us negatively to our siblings?
Did our religious institution shame us for our beliefs (or lack of beliefs)?
However we learned, negative self talk is highly problematic for living a healthy life. It becomes a tape in our mind which plays over and over. Then we constantly punish ourselves for the negativity of our thoughts, feelings, and behaviors. However, there are many things we can do to grow out of this habit.
First Annihilate Negative Self Talk
Listen to your self talk and hear what it is saying. Most of the time, you don’t even realized the awful things you are say to yourself. When you hear negative self talk, use one or more of the following to challenge the untrue thought:
Turn down the volume of this negative talk and eventually, turn it off. Visualize this as well.
Let go of the negative. Here, examine your self talk and if you see it is negative, focus on letting it go by accentuating the positive.
Reframe the negative as a the positive. For example, if you hear that voice tell you that you are stupid, tell yourself, “I am intelligent.” Make this a mantra that you repeat over and over.
When something bad happens, examine this and do not catastrophize, for most bad things are manageable. Break down the negative thoughts into small, manageable parts.
Examine whether there is any proof that you are a terrible, awful, stupid, ugly, etc., human being. Sometimes you’ll make an unhealthy choice; sometimes you will actually be wrong.
A positive reaction to an unhealthy choice is to make apologies or amends, but shame, that inner voice that tells you that you are bad to the core, must be silenced, for no one is bad to the core.
Throughout the day, practice saying positive things (affirmations) about yourself. By doing so, these positive affirmations become habit and take over from the negatives. Sometimes, even tell these things out loud to yourself in order to better hear and affirm the positive. Remember that positive and negative are the ying/yang of life; you will experience both but you don’t have to wallow in the negative.
Second Cultivate Positive Self Talk
Make a list of your positives and look at them daily. Speak them out loud. Focus on the positives and rejoice in them. Switch gears when you get into a negative focus. Do something positive such as:
Journaling
Reading
Exercising
Walking your dog
Playing on the computer
Watching the clouds in the sky
Singing aloud
Focusing on relaxation exercises
Getting positive feedback from a friend or family member
Volunteering
Visualize a happy situation such as being at the beach
Embrace Your Humanity
Laugh at your foibles – we all have them. Try to decrease or, better yet, eliminate your stress. Then, you can then focus more on the positives in life. Prioritize. Athletes use visualization and positive self talk to help them reach their highest potentials. We can do the same. Just like an athlete, we must practice, practice, and practice.
In summary, if you’ve done the negative self talk for years, you can see how effective this negativity keeps you trapped. Fortunately, positive self talk is a stronger force, that can be more effective in healing your life. You are worth it, and you’ll find yourself enjoying life more.
Negative self talk can be a sign of depression or anxiety, which can be treated. Find physicians, therapists, recovery programs, and support groups near you at Recovery Guidance.
The post How To Break Up With Negative Self Talk appeared first on Reach Out Recovery.
Can Eating Slower Help With Weight Loss
This new study looked specifically at people in Japan with type 2 diabetes who had one to three health check-ups between 2008 and 2013. During those appointments, people were asked about their eating and sleeping habits, including how fast they typically ate and whether they regularly skipped breakfast, snacked after dinner or ate before bed. They were also asked about their alcohol and tobacco use.
At the start of the study, more than half of the people said they ate at a normal speed, while about a third said they tended to eat fast. Only about 7% of people called themselves slow eaters.
Compared to those who wolfed down their food quickly, those who ate at a normal speed were 29% less likely to be obese. People who ate slowly were 42% less likely to be obese. And although absolute reductions in waist circumference over the course of the study were small, they were greater among slow and normal eaters.
People who said they didn’t snack after dinner at least three times a week, and those who didn’t eat within two hours of bedtime, were also less likely to gain weight over the course of the study than those who did those behaviors. Surprisingly, eating breakfast did not appear to make much of a difference for weight gain. Whether people regularly ate or skipped breakfast did not seem to have an effect on change in BMI. (The authors note, however, that skipping breakfast over a long period of time has been linked in other studies to high BMI and elevated disease risk.)
The findings make sense, say the researchers. Eating quickly has previously been linked to impaired glucose tolerance and insulin resistance, which can affect metabolism and fat-burning. Fast eaters may also continue to scarf down food even after they’ve consumed adequate calories, the study authors write in their paper, whereas slow eaters might feel full on less food overall. (The study did not look at how many calories people actually consumed on a regular basis, which likely affected their obesity risk.)
Slow eaters also tended to be healthier, and to have healthier habits, than their faster-eating peers. But even after controlling for other potentially influencing factors, the researchers found that eating speed appeared to be an independent factor in weight and body mass index measures.
Registered dietitian and Slim Down Now author Cynthia Sass, who was not involved in the study, says the findings are not surprising. But they are a good reminder that how and when people eat can be as important as the foods they choose, she adds. “I have had clients simply make changes to their eating pace and times and see weight-loss results without changing what they ate,” she says.
Eating high-calorie snacks after dinner or before bed is “like topping off your gas tank before you park the car in the garage,” says Sass. You’re less likely to burn off those extra calories overnight, when the body’s energy requirement is low.
Other research has shown that a slower eating pace improves satiety, Sass says. “There are apps to help you slow your eating pace,” she says, “but even just putting your fork down between bites and eating without distractions, like your phone or TV, can help.”
The authors point out that about half of the people in the study changed their eating speed throughout the course of the study—suggesting that this type of lifestyle modification is achievable, and that it may make a difference in body weight. Interventions and education initiatives aimed at altering eating habits “may be useful in preventing obesity and reducing the risk of non-communicable diseases,” they concluded.
The post Can Eating Slower Help With Weight Loss appeared first on Reach Out Recovery.
When You Are Addicted To Love
No my friends, this isn’t a sex-addiction article. I’m talking about love, not steamy passion or romance. My whole life I’ve been chasing a familial love, and it’s time for me to face my addiction.
I’ve been working on my co-dependency for almost three years, and I thought admitting this problem was enough. Co-dependency is a nice big umbrella that encompasses several of my unhealthy behaviors:
Controlling
Manipulating
Mothering
Guilting
Giving
Unfortunately, co-dependency isn’t the root of my problem, it is only the manifestation of it. Something is still missing.
Not Enough Childhood Love
I wasn’t born with all the self-love I need. Are any of us? For whatever reason, my childhood didn’t equip me to make this on my own or teach me how to find it. From an early age, I loved love. Then I meticulously remembered every way that it worked, and I tried to recreate the results. Classmates, siblings, parents, aunts, uncles, cousins, friends, and neighbors were all my test subjects.
In particular, I was drawn to the difficult cases. The girl in fourth grade who was too shy to speak, she was one of my greatest successes. She whispered to me, on occasion, but it was just the kind of hit I needed.
Driven To Love
I want to be loved, and I’ve tried to buy, beg, borrow, and perhaps even steal it. I’ve spent thousands on trips I couldn’t afford to see family members who barely acknowledged my existence. For hours, totaling months if not years of my life, I analyzed my actions, honing in on what I did right and what was completely wrong with ME. I gave more than I wanted and threw self-respect out the window years ago. Still what I wanted was not found.
Self-Love Doesn’t Cut It
I still want love, and I want to blame this craving on my lack of recovery. Just this week, I was at home with my loving husband and son. Yet my mind kept darting back to a far away family member. Why hasn’t she called me? I miss her so. What can I do to bring us closer? If I really needed a hug or affirmation, I could have walked into my living room and got it. But I fixated on what was far away, unachievable, and not enough to fill my need.
I am chasing something more. Taking care of myself is the next right thing to get me back on track, but it’s only a band-aid fix. My quest for love occupies most of my day and turns my emotions inside out more than any other problem.
Stepping Towards Love
For me, the 12 steps work. Step 1, my life is unmanageable. This crazy need for love has crept back in and turned my world upside down. Step 2, I came to believe a power greater than myself could restore me to sanity.
I’ve tried everything to get the love I want so badly. Nothing satisfies. If could have solved this alone, by now I would have. I have to turn to something bigger, and I haven’t found a human who fits the bill.
Celebrate Recovery, another popular 12-step program, says this about Step 2:
(I) Earnestly believe that God exists, that I matter to Him and that He has the power to help me recover.
Higher Love
When I first heard that I matter to Him, my heart melted. My Higher Power tells me I’m good enough. I am equal. I am worthy. He has all of the money, safety, power, food, and love I need. Because He loves me, He gives me what I need. The entire world isn’t a cruel scavenger hunt. I don’t have to spend my life searching the far corners of the world for bits and pieces of love. But that is always my first go to instinct.
Instead, to get a different result, I have to try something different. I have to stop running, and be quiet. I have to listen, wait, and trust in something bigger than me.
Co-dependency can be treated. Find therapists, recovery programs, and support groups near you at Recovery Guidance.
The post When You Are Addicted To Love appeared first on Reach Out Recovery.
Economic Cost Of Opioid Crisis $1 trillion
From CNBC by Dan Mangan The economic cost of the growing opioid epidemic topped an estimated $1 trillion from 2001 through 2017, according to an analysis released Tuesday.And the opioid crisis is projected to cost the United States an extra $500 billion through 2020 unless sustained action is taken to stem the tide, the report from health research and consulting institute Altarum said.
The economic toll of the opioid crisis is estimated to have topped $1 trillion from 2001 through 2017, a new report says.
The economic fallout from the epidemic of heroin and prescription painkiller abuse is on track to cost $500 billion from 2018 to 2020 alone.
More than 62,000 Americans are believed to have fatally overdosed from opioids in 2017.
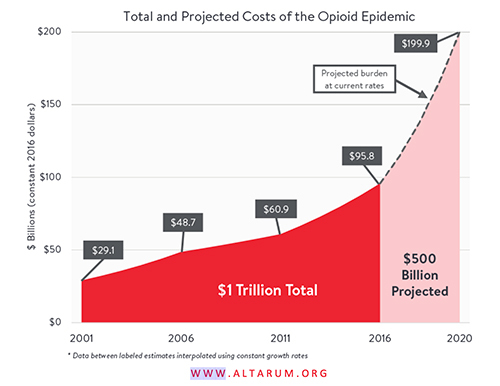
That’s because in recent years the growth rate in the economic fallout from the epidemic has sharply accelerated, along with the number of overdose deaths related to prescription painkillers and heroin.
Altarum said “the greatest cost” identified in its analysis “comes from lost earnings and productivity from overdose deaths — estimated at $800,000 per person based on an average age of 41 among overdose victims.”
The number of fatal opioid-related ODs is estimated to have topped 62,500 last year.
The analysis also estimated the costs from lost tax revenue to state and local governments, additional spending on health care, social services, education and criminal justice.
Health-care costs alone related to the crisis reached $217.5 billion from 2001 to 2017, according to the report.
Altarum estimated that in 2001, the nation’s annual cost from the opioid crisis stood at $29.1 billion. That more than doubled to $60.9 billion in 2011, and then hit a whopping $115 billion in 2017.
“The growth rate between 2011 and 2016 was double the rate observed between the previous five years,” the report said.
President Donald Trump, in a budget proposal released Monday, called for $17 billion in opioid-related spending. Of that, $13 billion is proposed for the Health and Human Services Department to use “to combat the opioid epidemic by expanding access to prevention, treatment and recovery support services, as well as support for mental health.”
The post Economic Cost Of Opioid Crisis $1 trillion appeared first on Reach Out Recovery.
9 Mythbusters About Addicts’ Moms
Time to separate fact from fiction about parenting and children who become addicted to substances and alcohol. Here are nine myths that need debunking.

Myth: #1 Good Mothers Don’t Have Children Who Take Drugs And Overdose
This misconception is painful. Stigma associated with addiction adds to the confusion moms have about themselves as good or bad parents. The truth is terrible moms can have kids that turn out great. By the same token absolutely great moms have kids who take drugs and overdose. Fact: Substance abuse and behavior addictions occur in every of background and socio economic group. Addiction can also persist no matter how great parents are and what they do to try to stop it.
Myth #2 Good Kids Don’t Drink Or Take Drugs
All kids have the potential to experiment with substances, and according to NIDA over 30% do. This number includes students with great grades and good social skills. 15% of teens become addicts and are at risk for death before they leave high school. Neither excellent students, nor troubled ones, take drugs with the intention of becoming an addict. Fact: Good and Bad have no relevance when it comes to addiction.
Myth #3 Substance Abusers Only Come From Dysfunctional Families
This is a common misconception. The potential for addiction does have a genetic component, just as the potential for other diseases, talents, skills and gender identification. But just because a family has addiction in its bloodline or experiences dysfunction doesn’t mean all the children who come from these backgrounds will become addicts, or that all addicts come from such a background.
Myth #3 Addicts’ Moms Should Be Ashamed
Mourning with dignity is essential for all moms who have lost children or are dealing with children who are active users. It’s just as agonizing as any other disease. Friends and colleagues don’t always respond with the same compassion for addiction as they would for another illness and casseroles are not forthcoming when a child is in crisis. Worse, addicts’ moms feel a lot of shame for having children they can’t save. Addiction is like any other progressive disease. With treatment there is the chance for survival. Without it, many people will get worse. Shame has no place in any catastrophic disease.
Myth #4 Addicts’ Moms Should Feel Guilty When Their Children Blame Them For Not Helping Enough
Addiction opens what seems like a black hole of need for money and support. Loving mothers trying to help can become exhausted and depleted of money, resources and spirits. When moms enter recovery and get help for themselves, children, or anyone caught up in an addiction, will resist the transition to taking responsibility for themselves. The resulting drama can make moms feel guilty. As they get stronger, healthy moms learn not to engage.
Myth #5 Addicts’ Moms Should Go Bankrupt Paying All the Bills
Addicts’ moms are not responsible for putting their adult children’s lives and needs above their own until there is nothing left. This is hard to learn but essential for recovery. Often substance abusers begin to heal when moms stop doing everything their children demand. Addicts don’t always recover, but moms can and deserve to heal no matter what happens.
Myth #6 Addicts Moms Can’t Be Happy If Their Children Are Still Using
We’ve met hundreds of moms along the way who lead full and happy lives despite their children’s active substance abuse, and even death. Moms are resilient when they believe that their feelings, productivity and lives matter. As one therapist told me only this week. “You can feel sad, even heartbroken, by a loss, and still cultivate happiness.” We know for a fact that is true.
Myth #7 Marriages Fail When Kids Are Substance Abusers
Anyone who’s been married knows that marriages go through many stages throughout the years. We’ve heard that marriages where both partners listen to each other and work as a team to focus on solution get stronger when dealing with the addiction crises. Where marriages have partners who don’t agree or one is in denial and the other wants to take action, addiction can indeed tear families apart.
Myth #8 Recovery Isn’t Successful If Users Don’t Fulfill The Potential They Had As Children
This is a misconception many families have because they don’t understand the nature of addiction and recovery. The potential of child that is lost in addiction may never return in the same form. But recovery brings different kinds of lives and gifts that are more than acceptable and satisfying. Successful moms need to understand that an adult child in recovery who fixes bikes, or works in a juice bar, or tie-dyes tee shirts at the beach, lights candles, loves sunsets and never wants to do anything else may be leading just as satisfying a life as an overworked professional sibling who never sees the light of day.
Myth #9 A Mom Who Doesn’t Receive Cards, Calls, nd Thanks, Isn’t Loved
We’d like to send a hug and a big fat slice of cake to every mom on every day. We don’t always get the recognition and appreciation we need. And that hurts. The gift of love can come from any source even from within. A mother’s heart wants recognition for the care and devotion she has given. Teens, young adults, and older adults who use are not in the right place to return their mothers’ love. It doesn’t diminish the effort a mother makes every day. We pray that all substance users who are separated from their mom and other loved ones will find their way back some day.
check out www.al-anon.alateen.org
If you need professional help for yourself or your child, check out Recovery Guidance for a free resource to find addiction and mental health professionals near you.
The post 9 Mythbusters About Addicts’ Moms appeared first on Reach Out Recovery.
February 12, 2018
Highly potent cannabis products pose mental health risks
From Science Daily Schizophrenia and other psychiatric issues may be triggered by marijuana use, according to a research analysis in the Journal of the American Osteopathic Association.
With states rapidly legalizing cannabis for medicinal and recreational use, physicians will be increasingly pressed to counsel patients on their frequency of use and dosage, as well as associated risks. The special report in the JAOA aggregates what is known to help physicians give the best evidence-based recommendations.
“We have a special concern for young people in their late teens and early twenties, whose brains are still developing,” says Jeramy Peters, DO, lead study author and psychiatrist at Oregon Health and Science University in Portland.
Dr. Peters adds that while there is no simple way to predict which young people might develop mental health issues as a result of marijuana use, a family history of mental illness could suggest potential risk.
“Pediatricians should be aware of this, especially for patients who have exhibited symptoms of anxiety and depression, and be willing to have candid discussions about cannabis,” says Dr. Peters.
Some longer-term effects associated with cannabis use include impaired memory and concentration, and decreased motivation. Researchers say when cannabis use starts to impair an individual’s health status or social or occupational functioning, he or she should be counseled to stop using cannabis or referred to substance abuse treatment providers.
Patients without mental health or substance abuse problems, who use cannabis recreationally or medicinally, can still benefit from physician counsel.
Know your cannabinoid
The main pharmacologically active chemicals in cannabis are the cannabinoids Tetrahydrocannabinol (THC) and cannabidiol (CBD). THC is responsible for the “high” people experience and there is moderate-quality evidence that THC may help chronic neuropathic or cancer pain. However, it has also been shown to induce symptoms of psychosis among healthy study volunteers and is thought to be a risk factor in developing psychosis.
Conversely, CBD is theorized to have antipsychotic and anxiolytic properties. Currently, CBD is being studied for its possible antiseizure and anti-inflammatory properties.
Many new products contain varied ratios of THC and CBD in order to create specific euphoric and medicinal effects. Researchers recommend physicians be aware of what products their patients are using — as well as how much and how often — in order to best advise them on dosing and risks.
“It is very difficult to tell someone what effect they can expect without knowing the specifics of the product,” says Walter Prozialeck, Ph.D., professor and chair of the Department of Pharmacology, Chicago College of Osteopathic Medicine at Midwestern University. “How much THC is in the product, how it’s consumed — and, of course, the individual’s physiology — all play a role in determining their experience.”
Dosing not always straightforward
The strength of cannabis has been increasing over the past half century. During the 1960s, cannabis was typically about 1% to 5% THC by weight. Many strains available today range from 15% to 25% THC by weight, with some strains reaching 30% or higher. When smoked, about 25% of the cannabinoids present in herbal cannabis get absorbed.
However, when inhaling cannabis via a vaporizer, the user absorbs up to 33% of the total cannabinoids. People who smoke or vape also experience the effects quickly, with intoxication setting in within 2 minutes and lasting 2-4 hours. The near immediate onset of the high allows users to titrate their dosing more effectively.
By comparison, when cannabis products are ingested orally, THC is absorbed inconsistently. Users typically experience the effects of THC about 2 to 4 hours after ingestion, and its effects last for 6 to 8 hours. Persons who ingest cannabis products often experience a more intense and longer-lasting effect. Given the significant delay of intoxication, it is much easier to overdose and experience negative effects.
“The best advice we can give is start low and go slow,” says Prozialeck. He adds that more research is needed from the medical community to create specific protocols that physicians can use to better counsel patients.
The post Highly potent cannabis products pose mental health risks appeared first on Reach Out Recovery.
Brain Alterations and Alcohol Seeking Behavior
About 15.1 million American adults have alcohol use disorder, meaning they cannot stop drinking despite adverse consequences — in other words, they have what is commonly referred to as alcoholism. Although it has been known that alterations in the connections between neurons in the brain likely play a role in alcohol dependence and other addictions, the cause-and-effect between these brain alterations and behavior has been less clear.
Now, Texas A&M research indicates that alcohol-seeking behavior may be induced by altering the strength of connections between particular neurons, according to recent results published in the journal Nature Neuroscience.
“We found that by applying a long-term potentiation protocol to animal models, we could directly induce a persistent change in their drinking behavior,” said Jun Wang, MD, PhD, assistant professor at the Texas A&M College of Medicine and lead author of the study.
Long-term potentiation is thought to be the basis of all learning and memory. It is the strengthening of synapses — the connections between neurons — based on sustained patterns of activity. In some cases, the strengthening may be facilitated by alcohol consumption — but Wang and his colleagues found a way around that.
Wang and his team mimicked the effect of alcohol with optogenetics, in which specially implanted proteins sensitive to light can be rapidly turned on and off within the brain. This process stimulates neuronal activity and essentially recreates the learning and memory that comes from actually performing an activity. Either way, it results in changes to the strength of synapses.
But what is more exciting, Wang and his team were able to reverse the alcohol-mediated synaptic strengthening by reversing the process. They did so with the opposite of long-term potentiation — what they call long-term depression — and decreased drinking behavior.
These changes affected particular neurons called D1, which Wang’s earlier research indicated could tell the brain to keep drinking. He calls them the ‘go’ neurons. Other neurons, called D2, do the opposite, and when they are activated, they give the signal to stop drinking.
“Our results provide pretty solid evidence that there is indeed a cause-and-effect relationship between the long-term synaptic changes and alcohol-seeking behavior,” Wang said. “Essentially, when brain changes are reversed, an individual may not want to drink for a long time.”
Although using this exact process in a human brain wouldn’t be feasible now, the results indicate possible targets for drugs or other therapies in the future. “Ultimately, our long-term goal is a cure for alcoholism, and possibly for other addictions as well,” Wang said. “We think these results that help us better understand how the brain works are an important step toward that goal.”
Content originally published by Science Daily
The post Brain Alterations and Alcohol Seeking Behavior appeared first on Reach Out Recovery.
25 lasting effects of childhood emotional abuse
Emotional abuse isn’t always recognized as abuse but leaves lasting scars nonetheless. I was called “girl child and an ugly one,” and told I was too stupid to have a career. When a husband called me thunder thighs, I didn’t eat anything for two years and still thought I was fat. You get confused about who and what you are and what’s happening around you.
People who have experienced emotional abuse are affected in some or all of the following ways.
1. They have commitment issues, probably because they had a hard time trusting anyone as a child.
2. They sometimes go into auto-pilot mode and blank out entire conversations or events. This is due to disassociation, a skill learned in childhood, and it’s often unintentional.
3. They experience mood swings which seem to come at random times and can be the norm for them. This is often because they had to deal with abuse as a kid, and the only response they knew was to model the behavior.
Emotional Abuse Can Lead To Self Harm
4. They may commit acts of self-harm or other self destructive behaviors. This often follows a pattern established in childhood.
5. They are angry underneath it all, and have outbursts of anger seemingly from nowhere.
6. They are nervous all the time. This may make them seem edgy, or brittle, and they startle easily.
Emotional Abuse Breeds Low Self Esteem
7. They don’t feel valid. No matter what they’re doing, they’re unsure if they can do it.
8. They have low self-esteem.
9. They don’t handle compliments well. They doubt their veracity.
Emotional Abuse Makes People Fearful Of Using Their Voice
10. They are quiet. They don’t feel comfortable using their voice after being worn down as small and wrong throughout their childhood.
11. They may have issues getting close to others, because they may not like people.
12. They may beat themselves up mentally and emotionally, since they were beaten emotionally for many years.
Emotional Abuse Makes People Fear Conflict
13. Conflict gives them immense anxiety, so they often run from it instead of facing it.
14. Making eye contact is extremely difficult and speaking makes them anxious, making it even more difficult.
15. They fear others abandoning or leaving them. They have attachment issues.
Emotional Abuse Can Lead To Feeling You Have To Defend Yourself…All The Time
16. They are often defensive, perceiving people as negative or offensive because of their previous abuse.
17. Often afraid of contact with people, they may be introverted and try to distance themselves as much as possible.
18. They may be sensitive to loud noises, as they were raised in an environment of raised voices and yelling.
People Pleasing Is Another Symptom Of Emotional Abuse
19. Many victims of emotional abuse overdo it because they want to please everyone. They become perfectionistic, tidy, clean and organized.
20. Often they will have trouble making decisions, after hearing throughout childhood that they were not good enough.
21. They are tough, but very sensitive. Because of experiencing a plethora of emotions at a young age, you have considerable emotional sensitivity.
Emotional Abuse Makes People Question Themselves
22. The world of emotional abuse leaves them second-guessing everything.
23. They constantly say that they’re sorry.
24. They will often ask questions to which they already know the answer, due to self-doubt.
25. They have addiction issues.
26. They are actually remarkably humble. They sincerely appreciate the good things in their life. They are a strong, grateful survivor of their past.
You Can Recover
Do any of these symptoms apply to you or anyone you know? There are ways to change the patterns and get healthier.
If you need help to deal with emotional scars or addiction, check out Recovery Guidance for a free and safe resource to find professionals near you.
The post 25 lasting effects of childhood emotional abuse appeared first on Reach Out Recovery.
Substance Abuse Grief Is It Different
Is substance abuse grief different from other kinds of grief? Does grief differ if it’s the death of a child, a breakup of a romantic relationship, a child leaving home, a death of a pet, or the grief of a mental illness or substance use disorder. What we know is that grief is grief – no matter what the loss, grief just is. The pain may be more overwhelming for some losses (for how does one survive and eventually thrive after a child dies), but comparative pain is not helpful. How can you even compare what you go through with someone else as we all have different ways to feel our pain and sorrow?
How Loss from Substance Abuse Grief Is The Same
What we do know that there can be significant grief regarding a family system embroiled in a loved one’s substance use disorder. So while there are many commonalities of grief, there are also some differences in the processes.
What Is the Same About Grief From A Substance Use Loss
grief is grief is grief
some losses may be more difficult than others
we grieve in different ways (sadness, screaming, anger outbursts, doing activities, laughing, remembering, etc.)
grief is different for different age ranges
there are no five stages of grief – this is outdated information
some coping skills are different than others and work better than others – this may vary due to what is lost
there is no such thing as comparative pain (i.e, “My pain is so much worse than yours” – no one knows exactly how someone may be suffering)
many people may be affected by the loss
there is no right or wrong way to grieve as long as it’s healthy
people react differently to loss
we must balance the feelings of the grief with other aspects of our lives
we need to deal with each loss as it comes, otherwise, grief piles up and becomes overwhelming and unmanageable
we tend to learn to be more compassion and accepting when we suffer our own losses
time does not heal all wounds – it merely aids in adjusting to the loss
What Is Different About A Loss From Substance Use
the response to the family’s loss regarding substance use may be disregarded as not being a true loss (i.e, “He’s just drinking so what’s the problem?”)
you may be blamed for the addict’s use ( you’re a bad spouse or mom) so how do your grieve if you’re the perceived problem
you may also be more likely to minimize your own grief as you think it’s not as important as other losses (comparative pain)
you may be so wrapped up in the children’s losses that you minimize your own
you may find it more difficult to find supports and resources to help you through your losses (i.e, there are many support groups for deaths but not for other losses)
As you can see, there are more commonalities than differences in the grief process. As you explore the differences, you can find that there is help. Grief is a natural process and in allowing yourself to feel the pain, sorrow, anger, joy, acceptance, calmness, rage, and all other feelings of bereavement, you can find ways.
For a free and safe resource to find mental health professionals near you.
The post Substance Abuse Grief Is It Different appeared first on Reach Out Recovery.
9 Tips For Family Addiction
Family addiction is not isolated to one person who may be using. Addiction is passed on through generations and everybody is affected.
Family addiction is complicated. Intergenerational addiction studies examine how addictions are passed on through the generations – great grandparents/grandparents/parents/children.
Numerous ongoing studies continue to show the propensity of substance use disorders (SUD) being a family disease, not only regarding how the illness affects all members of a family, but how each generation may have an impact of the course of the disease.
How Does One Become An Alcoholic/Addict?
Genetics/biological impact (most significant cause)
Environmental factors (such as living in high risk communities and/or home, poverty, poor health care)
Peer Pressure and/or being in a relationship with someone who uses (friends, older siblings, college parties, etc.)
Historical trauma (such as the Native American population)
Co‐occurring disorders (such as mental illness or history of personal trauma)
Modeling the behavior of parents, other adults, or friends (they use drugs/alcohol so it’s normal for you to use)
Early use of alcohol or drugs (childhood and teen use make one more susceptible to addiction)
Addictive potential of the chemical itself (for example, cocaine is a highly addictive substance)
Children and Teenagers: Does a family history of SUDs affect you? YES. It can affect you in many ways including:
Family members who are addicts may affect the family dynamic in unhealthy ways (poor boundaries such a child parenting the adult, abuse, neglect, poor living situations or poverty, etc.)
The genetic history is a strong predictor of addictions in each subsequent generation.
But My Parents Don’t Use So I Shouldn’t Have a Problem:
Yes and No. If there is a history of addictions with your biological family, you are still at risk. Genetics account for about 50‐60% for you having a higher risk of being addicted ‐ even if your parents aren’t addicted. So it is very possible if you use substances, you will have a problem. Likewise, a percentage of children won’t have an addiction and can be social users of various substances (social users do not have consequences related to their use such as drunk driving,
increased tolerance, losing a job, etc.) However, as noted above, you are also at risk due to other factors such as peer pressure, the addictiveness of the chemical, etc.)
But it Skipped a Generation:
Genetics continue to influence you, even if your parents aren’t addicted. So it doesn’t really skip a generation although it may appear that way. Also, you may have other relatives such as aunts or uncles who are addicted.
Your parents may not use because they grew up in an addictive family and don’t use because they don’t want to create the same unhealthy family dynamics with you as they had growing up. In actuality, they may be prone to being addicted, but will never know because they don’t use. This is why it appears to skip a generation.
So What Should I Do?
Since addictions thrive in secrecy, you need to talk, talk, and talk some more to trusted family members or other adults such as family friends, a teacher, counselor, or spiritual mentor. Do not allow the “elephant in the living room” syndrome to take over and pretend that nothing is wrong. Communication is a must. You need to understand your family history and how it may impact you.
Secondly, become knowledgeable through your own learning. Read and educate yourself. This helps you to be in charge of your life. Do not allow an addiction to rule you; your life is yours to live and hopefully, to live in a healthy manner.
Set boundaries with others. Do not let peer pressure force you to use to be “popular.” Let others know that you’re at risk for addictions and that you choose not to use because of this.
Model your behavior on those who you admire, trust, and respect.
Socialize with others who want to live free of addiction; they really do exist.
Attend 12‐step meetings such as Ala‐Teen or Al‐Anon and Nara‐Teen or Nar‐Anon which focus on issues that children/teens or adults of addicted parents/other family members may have, or ACA Teen or ACA (adult children of alcoholics – also called ACOA) that explore the special issues and concerns about growing up in an addicted family system.
Be involved in healthy activities such as school groups, the arts, sports, clubs, hobbies, and school‐led support groups for children and teens of addicted families.
See a counselor who can help you deal with family issues, grieve, and learn healthy coping skills.
And finally, know that you are not alone. There is a lot of help out there. Seek it out.
Carol Anderson, D.Min., ACSW, LMSW
For more about Carol Anderson
The post 9 Tips For Family Addiction appeared first on Reach Out Recovery.



