Leslie Glass's Blog, page 319
November 17, 2018
Alcohol Is Killing More People, And Younger
From USA Today:
The Biggest Increases Are Among Women
The last time lawyer Erika Byrd talked her way out of an alcohol rehab center, her father took her to lunch.
“Dad, I know what alcohol has done to me,” she told him that day in January 2011. “I know what it has made me do to you and mom. But that wasn’t me.”
By the time she died three months later, Byrd had blocked her parents’ calls because they kept having her involuntarily committed. They once had a magistrate judge hold a hearing at her hospital bed. He ordered herto undergo a month of in-patient treatment.
Byrd, who died in April 2011 at the age of 42, is among the rising number of people in the United States who have been killed by alcohol in the last decade.
It’s an increase that has been obscured by the opioid epidemic. But alcohol kills more people each year than overdoses – through cancer, liver cirrhosis, pancreatitis and suicide, among other ways.
From 2007 to 2017, the number of deaths attributable to alcohol increased 35 percent, according to a new analysis by the Institute for Health Metrics and Evaluation at the University of Washington. The death rate rose 24 percent.
One alarming statistic: Deaths among women rose 67 percent. Women once drank far less than men, and their more moderate drinking helped prevent heart disease, offsetting some of the harm.
Deaths among men rose 29 percent.
While teen deaths from drinking were down about 16 percent during the same period, deaths among people aged 45 to 64 rose by about a quarter.
People’s risk of dying, of course, increases as they age. What’s new is that alcohol is increasingly the cause.
“The story is that no one has noticed this,” says Max Griswold, who helped develop the alcohol estimates for the institute. “It hasn’t really been researched before.”
The District of Columbia, less than 10 miles away from the Venable law office where Byrd was a partner, had the highest rate of death from alcohol in the country, according to the institute’s analysis. Georgia and Alabama came in second and third.
Alabama, in fact, ranked third among states with the strongest alcohol control policies, as rated by medical researchers in a 2014 report published in the American Journal of Preventive Medicine.
States can influence drinking – especially dangerous binge drinking – with policies such as taxes on alcohol and restrictions on where and when it can be sold.
Psychologist Benjamin Miller, chief strategy officer at the nonprofit Well Being Trust, says the larger health challenges in the South are to blame for high alcohol death rates. Southern states typically rank near the bottom in national rankings in cancer, cardiovascular disease and overall health.
Oklahoma, Utah, Kansas and Tennessee rounded out the five states with the strongest alcohol control policies, the researchers reported. States with more stringent alcohol control policies had lower rates of binge drinking, they found.
Nevada, South Dakota, Iowa, Wyoming and Wisconsin had the weakest alcohol control policies.
David Jernigan, a professor at Boston University’s school of public health who has specialized in alcohol research for 30 years, notes that the beer industry holds considerable sway in Wisconsin.
Binge drinking is sending far more people to the emergency room, a separate team of researchers reported in the February 2018 issue of the journal Alcoholism: Clinical and Experimental Research.
The researchers, who looked at ER visits from 2006 to 2014,found the largest increases were among the middle aged – especially women. The number of teenage binge drinkers landing in the ER during that time actually declined.
Older, often lifelong drinkers don’t need only to have their stomachs pumped. They frequently have multiple complications from their drinking.
Their often bulbous bellies need to be drained of fluid, which builds up from liver cirrhosis, and their lungs cleared of aspirated vomit, says Dr. Anthony Marchetti, an emergency room doctor at Upson Regional Medical Center in Thomaston, Georgia.
They might also have brain hemorrhages or internal bleeding, because booze prevents their blood from clotting properly.
By middle age, Marchetti says, long-term drinking can also lead to heart failure, infections due to immune suppression, a type of dementia from alcohol-induced brain damage, stomach ulcers and a much higher risk of cancer.
As opioid overdoses, which kill about 72,000 people a year, grabbed America’s attention, the slower moving epidemic of alcohol accelerated, especially in Southern states and the nation’s capital. About 88,000 people die each year from alcohol.
Making matters worse, alcoholism is trickier to treat – and criticize – than opioid addiction.
“Culturally, we’ve made it acceptable to drink but not to go out and shoot up heroin,” Miller says. “A lot of people will read this and say ‘What’s the problem?’ “
It might be a more socially acceptable addiction, but alcoholism is at least three times costlier to treat than opioid addiction, according to the Centers for Disease Control and Prevention. And it’s a far more complicated midlife crisis to address.
The proven approaches – taxes on alcohol and limits on where and when alcohol is sold – are often rejected because the liquor industry has considerable clout with policymakers.
Ron Byrd says his daughter Erika was “beautiful inside and out.”
To him, there’s no question about what caused her death.
That’s despite the fact there was no alcohol in her system when she was found dead at home. She was so sick, Byrd says, she hadn’t been able to eat or drink for days.
“The death certificate never says alcoholism,” he says. “It said heart arrhythmia and heart valve disease. But nobody in our family had heart problems.”
Attorney Lisa Smith has been in recovery from alcohol and cocaine addiction for a decade. The New York City woman wrote the memoir “Girl Walks Out of a Bar” and co-hosts the podcast Recovery Rocks.
Smithspeaks at legal conferences and law firms such as Byrd’s about the hazards of lawyers’ high-stress days and booze-fueled dinners with clients. But she’s fighting forces far larger than her profession.
“It is poison, and we’re treating it like it’s something other than that because there‘s big corporate money behind it,” she says. “A lot of people are getting really rich on something that is toxic to us.”
Deaths of despair
In its Pain in the Nation report this year, the Well Being Trust called losses from drugs, alcohol and suicide “despair deaths.”
The three are closely related. Suicide is the third leading cause of death from alcohol, after cancers anddigestive diseases. One in five individuals who die from opioid overdoses have alcohol in their system at the time of their death.
Drinking can lead to cancers all along the digestive tract, from the mouth to the colon. About 15 percent of U.S. breast cancer cases are considered to be caused by alcohol. A third of those cases affected women who drank 1.5 drinks or less a week, according to a 2013 report in the American Journal of Public Health.
The “direct toxicity” of alcohol damages the nervous system from the brain down to the spinal cord and to peripheral nerves, says Marchetti, the Georgia emergency physician. It’s common for people in the late stages of alcoholism to have numbness in their feet and legs, which makes walking difficult even when they aren’t impaired.
Emergency rooms are the most expensive place to treat problems. Between 2008 and 2014, the rate of ER visits involving acute alcohol consumption rose nearly 40 percent, according to the study in the journal Alcoholism: Clinical and Experimental Research. For chronic alcohol use, the rate rose nearly 60 percent.
The increases for acute and chronic alcohol use were larger for women.
People who drink throughout their lifetime develop a tolerance for alcohol. But as they age, they lose muscle and gain fat and become less tolerant.
That leads to increased injuries and illnesses, says Rick Grucza, an associate professor of psychiatry at Washington University in St. Louis and lead author of the Alcoholism study.
But why are so many people drowning so many sorrows?
Brenda Padgett believes it was postpartum depression that led her daughter to take up the heavy drinking that ultimately killed her last year.
Ashley Hartshorn, who lived in Hendersonville, North Carolina, had already suffered the trauma of hearing her stepfather kill his girlfriend while she was on the phone.
Then Hartshorn testified against him in court, which helped send him to prison for life.
The depression came after the birth of her third child in February 2012.
“She wanted so badly to quit drinking, but the shame and the fear kept her from being able to allow herself to reach out for help,” Padgett says. “Like many, we were ignorant to the effects that alcohol has on the body. I thought she had time, time to hit rock bottom and time to seek help.
“I never knew that only five years of alcohol abuse could take the life of someone so young.”
Neither did Nancy Juracka. Her son Lance died in 2006 after just three years of heavy drinking. He was 36.
Lance Juracka, who grew up in Hermosa Beach, California, was intimately familiar with the scourge of alcoholism: He knew an uncle and aunt had drunk themselves to death before he was born. He even produced a short documentary about alcohol abuse while at New York University’s Tisch School of the Arts.
He started drinking when he got a job in Las Vegas reviewing shows – and was continually offered free drinks.
“Once he got a taste for alcohol, it really did him in fast,” his mother says. “I don’t understand how Lance’s liver went so quick.”
He headed back to California and ultimately moved back in with his mother.
He started a painting business. But his workers told Juracka he would just drink vodka or sleep.
“I thought I was going to lose my mind, I was so frantic,” she says. “I would sit up all night with him so he wouldn’t choke on this vomit.”
Joseph Garbely, an internal and addiction medicine physician at Caron Treatment Centers in Wernersville, Pennsylvania, says research shows that 10 percent of parents think having two or more alcoholic drinks a day is reasonable to reduce their stress.
But why? It’s not as if liquor is becoming more accepted.
Consider, however, the lack of public service announcements about the effect excessive alcohol has on health or families.
Ali Mokdad is a professor at the Institute for Health Metrics and Evaluation. He notes that alcohol-related education focuses on drunk driving.
Miller and others point to the high level of workplace stress that began accelerating during the recession, loneliness linked to social media and increasing pressures on working mothers.
In fact, social isolation can be both a cause and the result of excessive drinking. Parents whose children drank themselves to death in their 20s and 30s often describe the drinking in isolation seen in elderly alcoholics.
Few who drink excessively while young will become alcoholics, much less drink themselves to death. Those who are in recovery for alcoholism say people who turn high school or college binge drinking into a nightly coping ritual are at the most risk.
Amy Durham came close to dying from alcohol six years ago, when she was 40. And she barely drank until she was in her 30s.
The child of an alcoholic father, Durham never thought she could or would lose control.
“I didn’t even know what was happening to me,” she says.
She attributes her plunge into alcoholism to unresolved trauma from growing up in an alcoholic home, the stress of her work as a school principal, a “toxic” romantic relationship and grief over an inability to get pregnant.
“I just needed to be numb,” she says.
Ron Byrd says Erika, too, dreamed of having children. After two divorces and stage 3b breast cancer, however, the chance was slipping away.
“She wanted so desperately to have a baby,” Byrd says.
Durham is now corporate director of alumni relations at Pennsylvania-based Caron Treatment Centers, where she was treated.
“I wasn’t able to see that my drinking was a problem until it was almost too late,” she says. “I put limits on myself and would say that i’d only drink two glasses of wine in a social setting and then go home and drink a lot in isolation.”
When her father died in July 2012 of esophageal cancer, Durham says, she began a “very bad downward spiral.”
She remembers his funeral.
“i was trying to be nothing like my father, but I couldn’t wait to get out of that church and drink,” she says. “The shame of what was happening to me was more than I could bear.”
Like Hartshorn and Byrd, Durham started with white wine. But she ended up drinking copious amounts of vodka.
By the time her family got her to a hospital, Durham was in triple organ failure and wound up in a coma for 10 days.
That was followed by six weeks of dialysis.
When she arrived at in-patient rehab after the dialysis, Durham says, her body and eyes were still yellow and she was carrying 100 extra pounds of fluid – half of it in her legs.
She says fellow rehab residents – no strangers to the telltale signs of addiction – quickly looked away as she passed.
Men vs. women drinkers
When men crash and burn from alcohol, Mokdad says, the spectacle is often public. They get into bar fights, get cited by police for drunk driving or lose heir jobs.
A more typical trajectory for women starts with evening wine as a way to de-stress from the work day – either in a professional setting, or home with young children.
Author and podcast co-host Stefanie Wilder-Taylor, writer of “Sippy Cups Are Not for Chardonnay,” believes this stems from stubborn gender roles and norms surrounding stress.
“Moms just aren’t going to call home and say they’re stopping for a couple drinks after work with friends or going to the gym to unwind,” the Los Angeles woman says
Otherwise, they might feel like parenting failures as they compare themselves to other moms. So they drink wine while they make dinner, which can lead to a nightly pattern of excessive drinking.
That describes nurse practitioner Eileen O’Grady, who quit drinking 12 years ago.
O’Grady, who lives in McLean, Virginia, says her two sons, now in college, never really saw her drunk. But she couldn’t bear the thought of continuing her destructive double life. She would drink continually from dinner until she went to sleep, she says, and then start again the next evening.
For O’Grady, the last straw came after a night of especially hard drinking with another mom in her neighborhood.
The other woman, a schoolteacher, vomited in O’Grady’s car. She returned the next day to clean it up.
O’Grady hasn’t taken another drink.
“I could see my life if I kept going,” O’Grady says. She is now active in her local recovery community and working as a wellness coach.
Her schoolteacher friend taught classes until last fall. Within days of leaving the classroom, she was in a hospital with end-stage liver disease.
She died in hospice on Jan. 3.
At least 15 people at the woman’s memorial service asked O’Grady how her friend had died. They were stunned to learn alcohol was the cause.
The woman was poisoning herself with a half-gallon of vodka a day, O’Grady says, yet no one knew beyond her immediate family, O’Grady and a mutual friend in the neighborhood.
“We’re closeted,” O’Grady says. “We’re not in bars getting in fights.”
As for Durham, she was on a liver transplant list for about five months in 2011 and 2012. Then she learned she no longer needed a new liver.
“Livers have a great capacity for recovery,” says Dr. Michael Lucey, a professor and head of the division of gastroenterology and hepatology at the University of Wisconsin medical school.
Durham was once in a sorority at University of Mississippi, where beauty was competitive and a popular saying was “pretty is as pretty does.”
“But there was nothing pretty about my drinking,” she says.
If she had been diagnosed with breast cancer, Durham says, she wouldn’t think twice about getting treatment and talking about it.
Durham stopped drinking six years ago Thursday. She says she surprises people with how openly she shares the gritty details of her near-death experience.
“I want to show the world what recovery looks like, especially for women where stigma is still the way it is,” Durham says. “I want people to know there is hope.”
Erika Byrd called her father in hysterics on April 9, 2011. She had been fired after failing to turn in paperwork to continue getting disability coverage through her law firm.
“I don’t want to want it, but I want it,” Byrd recalls her saying, sobbing.
“I said, ‘If you can stop drinking you can do anything,’ ” Byrd says. “I told her, ‘We love you, Erika,’ and she hung up.”
Byrd and his wife were getting ready to go to church the next day when there was a knock on the door. A pastor stood with a police officer. Erika was dead.
A doctor from the National Institute for Mental Health called to ask if the Byrds would consider donating Erika’s brain for research.
They said yes.
“She had done everything she knew how to to beat this terrible disease,” Ron Byrd says. “I would think she would want it.”
The post Alcohol Is Killing More People, And Younger appeared first on Reach Out Recovery.
Should US Doctors Screen For Alcohol Disorder
It’s no secret. Alcohol is still the kind of addictions, advertised as the only way to have fun and celebrate no matter where you are or what you’re doing. The consequence is many Americans have a problem regulating how much alcohol they drink. While not everyone is an avid offender, it’s not uncommon for drinkers to engage in risky behavior either.
The U.S. Preventive Services Task Force (USPSTF) is highlighting a new recommendation in hopes of curbing that trend. Their review, published in the JAMA Network, found that general care physician screening can help.
They’re recommending that these doctors conduct screening for alcohol misuse in adults over 18. If patients are found to be drinking too much, “brief counseling” should follow.
“The net benefit of screening and brief behavioral counseling interventions for unhealthy alcohol use in adults, including pregnant women, is moderate,” states the paper.
Yes, it’s true. Overusing alcohol has turned into a nationwide problem.
The review attests that nearly 90,000 deaths from 2006-2010 were related to alcohol. That included both injuries from car accidents and alcohol overuse.
Many professionals agree that something must be done. That’s why the USPSTF committed to their investigation in the first place.
However, the evidence behind their recommendation appears limited.
The USPSTF came to their conclusion based on evidence with physicians who already provide some screening. But no studies actually evaluated the effectiveness of alcohol screening directly.
Perhaps this new recommendation warrants a formal study.
At the same time, evidence also proved inconclusive as to the benefits of screening adolescents (those between ages 12 and 17).
Furthermore, other hurdles for the USPSTF recommendation include how much burden it could place on doctors’ already weighty responsibilities.
Yes, a simple screening question like “How much alcohol do you drink?” might provide some accountability.
But if patients answer yes, how much time and effort should doctors spend on the “brief counseling?” Likewise, how will they evaluate whether their efforts are successful?
There are no current standards for alcohol recovery as it is.
In addition, such screening could place the burden of responsibility on doctors rather than alcohol users.
Perhaps screening by general care doctors is a good idea. However, the evidence may not be strong enough to implement rigorous change.
Researchers should look into other means of catching and treating alcohol misuse. In the meantime, at least general care doctors can choose whether they will conduct screening in their own practices.
What is Alcohol Misuse?
According to the National Institute on Alcohol Abuse and Alcoholism, moderate drinking is defined as no more than one drink per day for women and twp per day for men.
Anything above four drinks per day for men (or three for women) is considered alcohol misuse. Binge drinking isn’t far beyond that level either.
The point is that alcohol users have to be careful. It’s easy to go past the recommended amounts, especially with holiday celebrations coming up.
Whether or not general care doctors decide to screen, alcohol users should take responsibility. They should not exceed recommended alcohol amounts, and that includes carefully monitoring the type of alcohol too.
According to the CDC, one drink is defined as:
12 ounces of beer
8 ounces of malt liquor
5 ounces of wine
1.5 ounces of distilled spirits or hard liquor (3)
Alcohol users should do their best to stay educated on and aware of their drinking habits. If people find themselves taking risks or binge drinking, they should seek help and accountability from friends, family and notable recovery centers.
Content Originally published by Fox News
The post Should US Doctors Screen For Alcohol Disorder appeared first on Reach Out Recovery.
November 16, 2018
Kevin Love Explains What It Feels Like To Deal With Anxiety
From Men’s Health:
As a five-time NBA All Star and Olympic Gold Medal Winner, it’s safe to say that Kevin Love is doing something right. But the 30-year-old Cleveland Cavaliers player has insecurities like anyone else. For Love, these doubts are a source of anxiety.
“I [always] had this sense that I was doing something wrong,” he explains to MensHealth.com. “I never was. I just had that feeling for no reason.”
Earlier this year, Love discussed his anxiety in an open letter published in The Players Tribune. Love’s brave essay got a lot of positive attention. After all, it’s unfortunately rare that men—let alone professional athletes—speak so openly about their mental health.
“For 29 years, I thought about mental health as someone else’s problem,” he wrote. “To me, it was a form of weakness that could derail my success in sports or make me seem weird or different.”
When he was younger, Love’s anxiety “manifested in so many different ways,” he explains. “The only thing I knew was to go somewhere and have a rage-type fit.”
Love finally prioritized his mental health after a panic attack sidelined him during the middle of a game.
“I thought I was dying,” he says. “It was just an out-of-body crazy experience that I’d never had before.”
Now, the NBA star wants other guys to know their masculinity isn’t threatened by mental health issues. Love partnered with Schick Hydro and the Movember Foundation to create a series of “Locker Room Talk” videos about men’s health. In one episode, Love speaks with decorated Olympian Michael Phelps about his struggle with depression. Fans can donate to the campaign, which will fund various mental and physical health programs, and win the chance to meet Love before a game.
As for his own experience with anxiety, Love describes it as a “never-ending feeling in the pit of my stomach.”
“I just have this thing sitting here that just will not go away,” he says. “For better or worse, I think it will always be there.”
Through therapy, Love has found ways to manage this unease. The athlete finds relief by working out, playing basketball and meditating.
“I use Headspace quite a bit,” he says. According to Love, the app is easy to use and offers meditations that take less than five minutes.
Love also performs a technique where he tenses every part of his body and assesses how he’s feeling. Stress and anxiety build up in his extremities, particularly the feet, and he finds that breathing into those areas is relaxing.
“I’ve really learned to breathe into my body,” he says. “It sounds funny.”
Even those who don’t experience anxiety can benefit from one of Love’s strategies: He takes a couple of minutes each day to think about how he’s feeling.
“Just do a self check,” he says. “I try to do that daily.”
And if you do experience anxiety, Love encourages professional treatment.
“It’s always worth a shot,” he says. “You have to look at it like you’re investing in yourself and your happiness.”
The post Kevin Love Explains What It Feels Like To Deal With Anxiety appeared first on Reach Out Recovery.
The Fourth C In Addiction Is Really Enabling
When I first heard the three C’s, “I didn’t cause it. I can’t cure it, and I can’t control it,” I was so relieved, but did you know there is a fourth C? I can contribute to it by enabling addiction.
How My Mom Contributes
Hearing this at my meeting Saturday was a light bulb moment. Before I knew about the three C’s, I blamed my mom for my brother’s disease. She should’ve been tougher and that should’ve stopped it. After learning about the three C’s, I knew my blame was misplaced, but something was still off. I didn’t want her to keep:
Balancing his checkbook
Lending him money
Believing his outrageous lies
Mediating arguments with girlfriends
Filing his taxes for him
I was furious because her enabling allowed my brother to stay sicker longer, and being angry with her is easier than facing my fear of losing my brother.
The Apple Doesn’t Fall Far From The Tree
In case you missed it, nothing in the above scenario is any of my business. This often happens in families with alcohol use disorder. In an effort to keep everyone alive, responsibilities get shifted. Without realizing it, my mother showed me that anger, controlling, and manipulation were just part of the wife’s or mom’s job. Looking at the my brother’s addiction, analyzing what went wrong, and blaming my mom takes the focus off of me and my life. I was an enabler, just like my mom. I was still cutting my son’s food for him when he was 10 years old.
I’m Getting Better
My son has special needs, including severe ADHD. Fear and denial kept me from seeing what he could do. One day when I picked him up from school his teacher was waiting to see me. My son had refused to do any school work because:
The work was too hard
The lights were too bright
Some other kid was too loud
The assignment was too long
I knew the list well. It was the same list of excuses I gave his teachers when he was younger. Back then, he couldn’t keep up with his classmates because of his medical condition. Now he is attending a private school which specializes in accommodating his needs. Now he’s given work he can do; he just didn’t want to do it. Now I have recovery, and my top priority is making sure he’s able to take care of himself. While the teacher replayed the day’s drama, I didn’t defend or coddle. I just listened. It felt awkward and not rescuing him was hard, but I learned that would have been enabling. I was scared but proud.
The Experts Weigh In On Enabling
In their book Boundaries, Drs. Cloud and Townsend explain how contributing to the disease of alcohol use disorder interferes with the first law of boundaries – sowing and reaping. “Sometimes, however, people don’t reap what they sow, because someone else steps in and reaps the consequences for them…Rescuing a person from the natural consequences of his behavior enables him to continue in irresponsible behavior.” My goal is to not contribute to anyone else’s unhealthy behaviors. To reach that goal, I use these recovery tools:
KYMSI – Keep your mouth shut indefinitely
MYOB – Mind my own business
Smile, pause, and walk away
Stay in my yard and stay in my day
Keep the focus on me
When someone you love is losing his/her life to this horrible disease, it’s easy to act out of desperation. On days like these, the best I can do is trust my Higher Power and take one day at a time.
The post The Fourth C In Addiction Is Really Enabling appeared first on Reach Out Recovery.
Meditation Helps Vets With Post-Traumatic Stress Disorder
From The Washington Post:
Meditation worked as well as traditional therapy for military veterans with post-traumatic stress disorder in a small experiment sponsored by the Department of Defense.
One method preferred by the Department of Veterans Affairs is exposure therapy, but it doesn’t work for everyone and many can’t handle what it requires: purposely recalling traumatic events and confronting emotions.
Meditation could be a better choice for some, the researchers said.
The experiment tested meditation against exposure therapy, which involves working with a therapist and gradually letting go of fears triggered by painful memories.
Many vets won’t try exposure therapy or drop out because it’s too difficult, said Thomas Rutledge, the study’s senior author and a Veterans Affairs psychologist in San Diego.
Evidence for meditation “allows us to put more options on the table” with confidence they work, Rutledge said.
The study was published Thursday in the journal Lancet Psychiatry.
About 400,000 veterans had a PTSD diagnosis in 2013, according to the VA health system. The VA already is using meditation, yoga and similar approaches to supplement traditional therapy with PTSD, said Paula Schnurr, executive director of the VA’s National Center for PTSD.
While the three-month study adds to evidence supporting these lifestyle practices, Schnurr said, more research is needed to learn how long meditation’s benefits last.
“There’s no follow-up in this study,” Schnurr noted, and one therapist did 80 percent of the exposure therapy so the findings hinge largely on one therapist’s skills.
Researchers measured symptoms in about 200 San Diego area veterans randomly assigned to one of three groups. Some learned to meditate. Others got exposure therapy. The third group attended classes where they learned about nutrition and exercise.
All sessions were once a week for 90 minutes.
After three months, 61 percent of the meditation group improved on a standard PTSD assessment, compared to 42 percent of those who got exposure therapy and 32 percent of those who went to classes. When researchers accounted for other factors, meditation was better than the classes and equally effective as exposure therapy.
The researchers defined success as at least a 10-point improvement in scores on a standard symptoms test, given to participants by people who did not know which kind of treatment they’d received. The test measures symptoms such as flashbacks, nightmares and insomnia.
PTSD also can be treated with medications or other types of talk therapy. Many of the participants were taking prescribed medicine for PTSD.
Most of the vets were men with combat-related trauma, so it’s not clear whether meditation would be equally effective in women or with other types of trauma.
There’s growing interest in meditation in the United States. A government survey last year found 14 percent of adults said they had recently meditated, up from 4 percent from a similar survey five years earlier.
There are many styles of meditation. The type taught to vets in the study was transcendental meditation, or TM, which involves thinking of a mantra or sound to settle the mind.
TM was developed by Maharishi Mahesh Yogi, a guru to the Beatles in the late 1960s. Some of the study authors are affiliated with a university in Fairfield, Iowa, founded by Maharishi. Their role was to oversee the meditation training.
Rutledge, who was the principal researcher, said he does not practice meditation himself.
Meditation could be more acceptable to veterans who might associate mental health treatment with weakness, Rutledge said.
“It’s probably less threatening,” he said. “It may be easier to talk to veterans about participating in something like meditation.”
The post Meditation Helps Vets With Post-Traumatic Stress Disorder appeared first on Reach Out Recovery.
Is It Adolescence Or Addiction
In August, my tweenage son, Keith, found the seedy underbelly of the internet. At 40, I’m still too young to see the graphic images he saw. Here’s why I’m treating his obsession like an addiction.
My first line of defense was an awkward conversation about what sex is and is not. He promised to never look at those videos again. I believed him. After all, some curiosity is normal, right?
In September, I again found trashy images in his browser history. I lectured. He promised. This pattern repeated more times than it should have. I changed passwords. We then developed a written contract.
When he violated our written contract, I took his device away and hid it in my bedroom. Later that night, when Keith thought I was asleep, I heard bare feet running through the house. Keith was in the office digging through my desk drawers. He padded back through the house and stood over my bed. I pretended to be asleep. He opened my nightstand drawer, but didn’t find his device. Next, he went through my purse. From there, he went to the garage to search my car.
I crept down the dark hall. In silence, I locked the garage door, trapping my son inside. Then I waited for him to realize he was caught. He screamed and yelled at being found out. He didn’t show any remorse at being caught.
My Son’s Drive Deepens
For the month of October, Keith had no technology. Over Thanksgiving break, I let Keith try to re-establish trust with me by giving him limited use of his device without any wifi privileges. I was still hoping this was a passing phase.
This week, Keith tried to take his phone into the youth service. When I noticed this breach, I told him to put his phone in my purse. He did and we both went on to our separate services. Later during the service, I noticed his phone was not in my purse. My stomach was sick, and I was overcome with dread. I walked down to the youth auditorium. Keith was using the internet on his phone. I was devastated. I returned to my service, too heartbroken to listen.
Keith’s drive for this device reaches beyond natural curiosity. I know addiction. I’ve lived with addiction. Keith’s lying is all too familiar. So is the sadness of being less important than the drug of choice. I don’t want this for me or my kid. Worse than that, he is so driven to get what he wants. I am afraid that this is only his drug of the day. What will happen when he tries his first beer or joint?
How Keith’s Addiction Harms Me
Addiction steals peace and harmony. Addiction pulls me to live in the future. My mind races with thoughts, “What if he is arrested?” Addiction lies to me and says “You’re only O.K. if Keith is O.K.” Keith’s illness shines a light on my own illness.
I love Step 12. It says, “Having had a spiritual experience as the result of these steps, we try to carry this message to others and practice these principles in all our affairs.” I practice my recovery in all of my affairs because my illness has affected ALL of my affairs.
My Go To Recovery Tools
Keith’s dishonesty sent me back to the basics:
Live one day at a time. I had plans to do some grocery shopping after church, so I refused to let my mood change my plans.
Keep my mouth shut. I didn’t say anything when I took the phone, and I didn’t say anything in the car after the church. Before I even made a decision, I talked it over with my sponsor and my therapist. Keith is old enough to understand a delayed consequence.
Finally, I put the focus back on me. To recover from the set back, I cleaned my bedroom and gave it a mini-spa makeover. I also gave myself a pedicure and watched a movie. I took the time to eat healthy, protein rich meals, and I did yoga. I’m determined to enjoy my life whether Keith ends up in prison or not. The disease may end up taking my son, but it will not have two victims.
I decided the best way to handle Keith’s complete lack of respect was to take away every single belonging in his bedroom. He can earn them back, but for now they are all in the storage unit and he is sleeping in a room with nothing, but his bed.
Even though I am his parent, I can’t make Keith obey my commands. The only person I can change is me.
The post Is It Adolescence Or Addiction appeared first on Reach Out Recovery.
You Cannot Talk Butterfly Language With Caterpillars
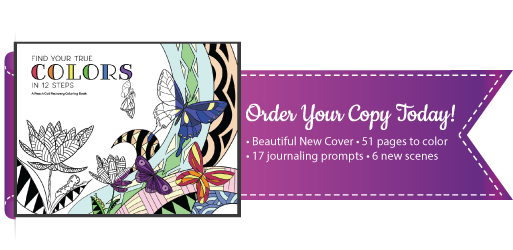
Entering recovery is an incredible metamorphosis. Those in recovery learn a new way to think. They’re immersed in unfamiliar terms, slogans, and acronyms. As a result, friends and family often struggle with an unexpected kind of illiteracy. Our new book, Find Your True Colors In 12 Steps, reinforces early recovery lessons and translates these lessons so friends and family can join their loved ones in this empowering new world.
Recovery Is For Everyone
It only takes one person in recovery to change the whole family. Addiction is a family disease that affects generations, and everyone in the family needs to heal. Sometimes, the person who struggles with addiction isn’t the first who seeks recovery. Parents, partners, and children find support and healing in programs like Al-Anon, CoDA, Nar-Anon, and Celebrate Recovery.
Each of these family support programs follow the same 12 Steps of AA and NA. Why? Because they have helped millions. When families all work the same program, they can all speak the new language of recovery. Even if your loved one doesn’t quickly follow you into a program, your recovery will help you navigate the heartbreaking challenges of addiction.
This coloring book supplements a 12 Step recovery program with a twist. Many hurt by addiction live in constant fear. Will she get fired today? Will he get arrested? Or what if she drives home drunk again? We can’t sleep, and our thoughts race to plan for our worst fears: court dates, overdoses, and funerals. Our minds can only focus on one thought at a time.
This coloring book gives hurting minds 51 scenes to color and hours of distractions on which to focus.
Journaling is another key element to recovery, but it’s an intimidating habit to start. This book features 17 writing prompts to help you ease into this strange new therapy.
More Than Just A Coloring Book
We took the relaxing concept of adult coloring books and infused it with tools and slogans. Our book has 12 chapters, one for each step. Here’s an inside look at Step 12.
Order Your Families’ Books Today
Embarking on the brave new journey to recovery means you’ll learn a new language too: the language of hope. You’ll learn to communicate without fear and blame. You’re basically learning to talk butterfly language. Order your books today, so every caterpillar in your family can learn the incredible new language of recovery.
The post You Cannot Talk Butterfly Language With Caterpillars appeared first on Reach Out Recovery.
Holiday Boundaries Keep Traditions Safe
Holiday boundaries can conflict with traditions now that holiday gatherings are upon us again. Hallmark cards depict mom and dad and a couple of cherub-cheeked children warming themselves by a fire. Or sledding, shopping, baking cookies, visiting Santa or … any traditions that go along with the holidays. When seasonal images of togetherness don’t match up with boundaries to limit toxic family interactions, then what?
Holiday Boundaries Are Needed Because Some Emotions Can’t Be Ignored
Trauma, grief and addiction aren’t feelings that can be neatly tucked away during times of festivity. When a family member’s behavior requires detachment in families whose holiday traditions are steeped in … well…traditions..how can we honor the traditions while still maintaining our boundaries?
Creating new traditions around loss (either a family member who has passed away, or is currently banished) can be healthy and help us move forward. Some family members are not safe to be around, accepting that reality works better than trying to force everyone to get together for the sake of the holiday,
Creating detachment from family members is no easy task. Vacillating, second guessing and giving more chances often sabotages even the most resolute among us. Add to that the pressures of holiday family gatherings and all the happy memories, and the boundaries that took so long to put in place begin to crumble like cookies.
Avoid The Tradition Of Turning A Blind Eye
However, if we realize that the tradition of turning a blind eye because of the holidays has been a choice, we understand that we can choose differently while still maintaining the boundary and the tradition. Smudging boundaries leaves family traditions in ruins because we want the holiday to be the way it was and the person to be the way they were before whatever happened that caused the need for space and detachment. It serves no one to create resentment around festivities meant to draw people together.
Family members can be honored and remembered in many ways throughout the season, even while maintaining healthy holiday boundaries.
Make a place setting at the table for your loved one who is absent.
Donate to a favorite charity in their honor.
Support their choices from a distance and without voicing your opinion.
Doing whatever it takes. Being present without directing sometimes means not being physically in their presence.
Standing back and giving someone else the space to figure things out for themselves is a way of letting the other person know that you trust them. Trust is a big gift.
Remember the way it used to be, but choose the way it is now. Choice doesn’t victimize – it empowers.
When we empower others by leaning back with our support, instead of leaning in and being the director, we are gifting them with our respect and our unconditional love. And isn’t love the basis of family traditions, after all?
The post Holiday Boundaries Keep Traditions Safe appeared first on Reach Out Recovery.
November 15, 2018
Forgiveness: The Path to Healing And Emotional Freedom
Forgiveness is a crucial element in leading a healthy, fulfilling life after experiencing abuse, hurt, or trauma. For many, the process of forgiveness can feel confusing and overwhelming.
Here’s some insight into the concept of forgiveness to help you along your journey.
What is Forgiveness?
A good first step is to say what it is not. Forgiveness is NOT:
Condoning behavior that is unacceptable and hurtful.
“Forgetting” (or attempting to forget) behavior and/or events that happened.
Letting someone “off the hook” for their behavior.
Absolving the perpetrator of sin with no earthly consequences.
Superficially deciding that all is done and forgiven. This actually bypasses the work that is required in the forgiveness process.
An obligation.
I have searched far and wide for my own definition. I explored concepts, philosophies, and theories from different cultures and religions before I came to the following: Forgiveness is a process of feeling, understanding, and letting go that is a gift to one’s self. Again, I emphasize that forgiveness is a process, not an event. Additionally, forgiveness has little – almost nothing – to do with the other person.
Do I have to forgive in order to be free from hurts and/or abuse?
The answer to this question is a simple, but not simplistic, “yes.” As adults, we must forgive in order to be truly free of seeing ourselves as victims. Victim identification keeps us bound to the person, situation, or institution that hurt us. Additionally, it keeps us in a loop of blame, shame, self-perpetration (such as addictive behaviors and self-abandonment), dishonesty with ourselves and others, and the unconscious seeking of destructive relationships. The process of moving from victim, to survivor, to thriver allows us to move forward and live our lives to the fullest.
I have witnessed many clients freed from the bitterness, shame, guilt, hurt, and loneliness they had carried for ages because of their engagement in the forgiveness process. They now have healthy relationships with themselves and others. You can’t bypass or skip over the process. As poet Robert Frost wrote in his 1915 poem A Servant to Servants, “The best way out is always through.”
How do I actually forgive? What is expected of me in this process?
It is important to remember that the process of forgiveness will look and feel different for everyone. You have the right to make choices, set limits, and create boundaries that titrate your experience. You get to do this at your own pace. Here are some key actions to consider as you work on forgiving those who have hurt you.
Strive to gain an objective understanding of the hurtful behavior/situation, and remember that you can do things differently right now.
Truly know yourself and what makes you tick—your motives, beliefs, behaviors, dreams, and feelings.
Identify, label, and express your feelings. It is important to do this in a safe way and in a safe place so that you do not—perhaps unintentionally—further hurt yourself or someone else. I also strongly recommend you work with a guide, such as a mental health professional.
Name painful beliefs about yourself, others, the world, and maybe even God (or whatever spiritual concept you choose).
Acknowledge emotions, ride their waves, and let them pass. Emotions last about 30-90 seconds and come in waves. You can do almost anything for 30-90 seconds!
Allow yourself to grieve losses, such as those of your innocence, hopes, dreams, and significant relationships. Grieving is painful, but it takes us to the place of acceptance.
Create a “payoff and cost” list to identify what you get out of and what consequences you experience from the beliefs, feelings, and behaviors that cause pain.
Decide to let go. When emotions come up, it can be easy and almost natural to get “stuck” and languish in them. Somewhere in the process, making the conscious decision to let go will be crucial to moving forward.
Set limits that are self-care directed, not meant for punishment or revenge. This includes if, how, and when you have contact with those who have harmed you.
Practice being gentle and kind to yourself and others.
Share your experience, strength, and hope with others who have experienced similar hurts and pain.
In order to make the most of your experience, check in with yourself regularly to remain in tune with your emotions. Recognize when you have made progress and continue on the path diligently and at the pace that works best for you.
From Psychology Today
The post Forgiveness: The Path to Healing And Emotional Freedom appeared first on Reach Out Recovery.
How Exercise Could Help Fight Drug Addiction
From Science Daily:
The siren call of addictive drugs can be hard to resist, and returning to the environment where drugs were previously taken can make resistance that much harder. However, addicts who exercise appear to be less vulnerable to the impact of these environmental cues. Now, research with mice suggests that exercise might strengthen a drug user’s resolve by altering the production of peptides in the brain, according to a study in the journal ACS Omega.
Re-exposure to drug-related cues, such as the location where drugs were taken, the people with whom they were taken or drug paraphernalia, can cause even recovered drug abusers to relapse. Prior studies have shown that exercise can reduce craving and relapse in addicts, as well as mice. Although the mechanism was unknown, exercise was thought to alter the learned association between drug-related cues and the rewarding sensations of taking a drug, possibly by changing the levels of peptides in the brain. Jonathan Sweedler, Justin Rhodes and colleagues at University of Illinois at Urbana-Champaign decided to explore this theory by quantifying these peptide changes in mice.
Mice were given cocaine injections over four days in special chambers with a distinctive floor texture to produce a drug association with that environment. The animals were then housed for 30 days in cages, some of which included a running wheel. The researchers found that mice that exercised on these wheels had lower levels of brain peptides related to myelin, a substance that is thought to help fix memories in place. Re-exposure to the cocaine-associated environment affected running and sedentary mice differently: Compared with sedentary mice, the animals with running wheels showed a reduced preference for the cocaine-associated environment. In addition, the brains of re-exposed runners contained higher levels of hemoglobin-derived peptides, some of which are involved in cell signaling in the brain. Meanwhile, peptides derived from actin decreased in the brains of re-exposed sedentary mice. Actin is involved in learning and memory and is implicated in drug seeking. The researchers say these findings related to peptide changes will help to identify biomarkers for drug dependence and relapse.
The post How Exercise Could Help Fight Drug Addiction appeared first on Reach Out Recovery.