Leslie Glass's Blog, page 284
March 21, 2019
Vitamins & Supplements For Alcohol Recovery
From Jerry Shaw @ Livestrong: Vitamins play a major role in alcohol recovery in foods and supplements. Recovering alcoholics suffer from depleted nutrients from heavy drinking that can cause irregular eating habits.
Alcoholics neglect healthy diets and often get their calories from fatty or sugary foods. Recovering alcoholics may confuse feelings of hunger for alcoholic cravings and need encouragement to return to normal dietary patterns. A healthy diet for recovery includes vitamin-rich protein, complex carbohydrate and high-fiber foods. Vitamin supplements aid in restoring proper nourishment.
Vitamin B Depletion
The most common deficiencies from alcoholism include thiamine, pyridoxine and folic acid, according to the University of Maryland Medical Center. Thiamine, a B vitamin found in meat, grains and yeast, helps metabolize carbohydrates. Fish, liver, cereals and yeast contain pyridoxine, or vitamin B-6. Green vegetables, fruit and liver contain folic acid, also a B vitamin. B vitamin foods also include poultry, nuts, brown rice and dairy products. Broccoli, asparagus, potatoes, bananas, apricots and figs contain B vitamins.
Deficiency Problems
Deficiencies in the B vitamins can result in anemia or neurological problems. In the late stages of alcoholism, the deficiencies may lead to Korsakoff’s syndrome, also known as “wet brain,” which prevents the proper absorption of nutrients and causes serious mental impairment and brain disorders.
Supplement Potential
Doctors may prescribe supplements to replenish the deficiencies as the alcoholic begins a recovery diet. Alcoholics often have difficulty eating after they end long-term drinking. The supplements help return lost nutrients until regular eating habits return. Supplements during recovery may include minerals, such as selenium, magnesium and zinc.
Vitamin A Caution
Alcoholics may also have vitamin A deficiencies. However, excess amounts of vitamin A can damage the liver. Recovering alcoholics need to follow the advice of a doctor for dietary or supplemental intake of these vitamins. Dairy products, green and yellow vegetables, chicken, liver, mackerel and herring contain high amounts of vitamin A.
Anxiety Remedy
Research shows a combination of vitamin C, vitamin E, vitamin B-6 and niacin, a B vitamin, reduces anxiety for alcoholics in the early stages of recovery, according to the University of Michigan Health System. Anxiety often occurs for alcoholics after they quit drinking and increases the risk of relapse. Strawberries, oranges, broccoli and peas contain vitamin C. Vitamin E foods include mackerel, salmon, whole grains, spinach, tomatoes, sweet potatoes, nuts and olive and corn oils.
Support Benefits
While restoration of vitamins to the body helps alcoholics during recovery, they also benefit from counseling or support groups for help in continuing their sobriety. Doctors and other recovering alcoholics can provide advice on their feelings, including anxiety and point out the importance of a healthy diet.
The post Vitamins & Supplements For Alcohol Recovery appeared first on Reach Out Recovery.
Fentanyl: The Opioid Epidemic’s Third Wave
From Martha Bebinger @ NPR: Men are dying after opioid overdoses at nearly three times the rate of women in the United States. Overdose deaths are increasing faster among black and Latino Americans than among whites. And there’s an especially steep rise in the number of young adults ages 25 to 34 whose death certificates include some version of the drug fentanyl.
These findings, published Thursday in a report by the Centers for Disease Control and Prevention, highlight the start of the third wave of the nation’s opioid epidemic. The first was prescription pain medications, such as OxyContin; then heroin, which replaced pills when they became too expensive; and now fentanyl.
Fentanyl is a powerful synthetic opioid that can shut down breathing in less than a minute, and its popularity in the U.S. began to surge at the end of 2013. For each of the next three years, fatal overdoses involving fentanyl doubled, “rising at an exponential rate,” says Merianne Rose Spencer, a statistician at the CDC and one of the study’s authors.
Spencer’s research shows a 113 percent average annual increase from 2013 to 2016 (when adjusted for age). That total was first reported late in 2018, but Spencer looked deeper with this report into the demographic characteristics of those people dying from fentanyl overdoses.
Increased trafficking of the drug and increased use are both fueling the spike in fentanyl deaths. For drug dealers, fentanyl is easier to produce than some other opioids. Unlike the poppies needed for heroin, which can be spoiled by weather or a bad harvest, fentanyl’s ingredients are easily supplied; it’s a synthetic combination of chemicals, often produced in China and packaged in Mexico, according to the U.S. Drug Enforcement Administration. And because fentanyl can be 50 times more powerful than heroin, smaller amounts translate to bigger profits.
Jon DeLena, assistant special agent in charge of the DEA’s New England Field Division, says one kilogram of fentanyl, driven across the southern U.S. border, can be mixed with fillers or other drugs to create six or eight kilograms for sale.
“I mean, imagine that business model,” DeLena says. “If you went to any small-business owner and said, ‘Hey, I have a way to make your product eight times the product that you have now,’ there’s a tremendous windfall in there.”
For drug users, fentanyl is more likely to cause an overdose than heroin because it is so potent and because the high fades more quickly than with heroin. Drug users say they inject more frequently with fentanyl because the high doesn’t last as long — and more frequent injecting adds to their risk of overdose.
Fentanyl-Laced Cocaine Becoming A Deadly Problem Among Drug Users
Fentanyl is also showing up in some supplies of cocaine and methamphetamines, which means that some people who don’t even know they need to worry about a fentanyl overdose are dying.
There are several ways fentanyl can wind up in a dose of some other drug. The mixing may be intentional, as a person seeks a more intense or different kind of high. It may happen as an accidental contamination, as dealers package their fentanyl and other drugs in the same place.
Or dealers may be adding fentanyl to cocaine and meth on purpose, in an effort to expand their clientele of users hooked on fentanyl.
“That’s something we have to consider,” says David Kelley, referring to the intentional addition of fentanyl to cocaine, heroin or other drugs by dealers. Kelley is deputy director of the New England High Intensity Drug Trafficking Area. “The fact that we’ve had instances where it’s been present with different drugs leads one to believe that could be a possibility.”
The picture gets more complicated, says Kelley, as dealers develop new forms of fentanyl that are even more deadly. The new CDC report shows dozens of varieties of the drug now on the streets.
The highest rates of fentanyl-involved overdose deaths were found in New England, according to the study, followed by states in the Mid-Atlantic and Upper Midwest. But fentanyl deaths had barely increased in the West — including in Hawaii and Alaska — as of the end of 2016.
Researchers have no firm explanations for these geographic differences, but some people watching the trends have theories. One is that it’s easier to mix a few white fentanyl crystals into the powdered form of heroin that is more common in eastern states than into the black tar heroin that is sold more routinely in the West. Another hypothesis holds that drug cartels used New England as a test market for fentanyl because the region has a strong, long-standing market for opioids.
Spencer, the study’s main author, hopes that some of the other characteristics of the wave of fentanyl highlighted in this report will help shape the public response. Why, for example, did the influx of fentanyl increase the overdose death rate among men to nearly three times the rate of overdose deaths among women?
Some research points to one particular factor: Men are more likely to use drugs alone. In the era of fentanyl, that increases a man’s chances of an overdose and death, says Ricky Bluthenthal, a professor of preventive medicine at the University of Southern California’s Keck School of Medicine.
“You have stigma around your drug use, so you hide it,” Bluthenthal says. “You use by yourself in an unsupervised setting. [If] there’s fentanyl in it, then you die.”
Traci Green, deputy director of Boston Medical Center’s Injury Prevention Center, offers some other reasons. Women are more likely to buy and use drugs with a partner, Green says. And women are more likely to call for help — including 911 — and to seek help, including treatment.
“Women go to the doctor more,” she says. “We have health issues that take us to the doctor more. So we have more opportunities to help.”
Green notes that every interaction with a health care provider is a chance to bring someone into treatment. So this finding should encourage more outreach, she says, and encourage health care providers to find more ways to connect with active drug users.
As to why fentanyl seems to be hitting blacks and Latinos disproportionately as compared with whites, Green mentions the higher incarceration rates for blacks and Latinos. Those who formerly used opioids heavily face a particularly high risk of overdose when they leave jail or prison and inject fentanyl, she notes; they’ve lost their tolerance to high levels of the drugs.
There are also reports that African-Americans and Latinos are less likely to call 911 because they don’t trust first responders, and medication-based treatment may not be as available to racial minorities. Many Latinos say bilingual treatment programs are hard to find.
Spencer says the deaths attributed to fentanyl in her study should be seen as a minimum number — there are likely more that weren’t counted. Coroners in some states don’t test for the drug or don’t have equipment that can detect one of the dozens of new variations of fentanyl that would appear if sophisticated tests were more widely available.
There are signs the fentanyl surge continues. Kelley, with the New England High Intensity Drug Trafficking Area, notes that fentanyl seizures are rising. And in Massachusetts, one of the hardest-hit areas, state data show fentanyl present in more than 89 percent of fatal overdoses through October 2018.
Still, in one glimmer of hope, even as the number of overdoses in Massachusetts continues to rise, associated deaths dropped 4 percent last year. Many public health specialists attribute the decrease in deaths to the spreading availability of naloxone, a drug that can reverse an opioid overdose.
This story is part of NPR’s reporting partnership with WBUR and Kaiser Health News.
The post Fentanyl: The Opioid Epidemic’s Third Wave appeared first on Reach Out Recovery.
Joe Walsh & Ringo Starr’s Mission To End Addiction
From Sarah Grant @ Rolling Stone: It was a foggy autumn night in New York’s Rainbow Room when Joe Walsh took center stage — no guitar in sight. So he addressed the elephant in the room: “I’m Joe, and I’m an alcoholic.” It’s a half-joke, meant to set the audience at ease while gently reminding the tables of suits and sequined dresses that addiction is not some distant, dark memory; but on the contrary it’s a specter that hangs over 45 million American families. Even the ones who sell out Madison Square Garden.
That night the 71-year-old old Eagles guitarist, 25 years a “sober alcoholic,” received the highest humanitarian award for activism in the addiction recovery community, jointly awarded by the nonprofit Facing Addiction and the National Council on Alcoholism and Drug Dependence (NCADD). His wife, the elegant Marjorie Bach, was also honored and she stood behind him, wiping tears from her eyes with a napkin even when he cracked jokes. Bach is 27 years sober. Earlier, she spoke with unflinching gravitas about fearing at one point her husband would die. Walsh’s in-laws, Ringo Starr and Barbara Bach, presented them with the award. Between the four of them, they have over a century of sobriety.
The evening was full of humbling stories where glamorous, talented people admitted the insidiousness of their addiction battles. The floor turned over to an all-star tribute led by country singer-songwriter Vince Gill, the Doobie Brothers’ Michael McDonald and Butch Walker. They rocked to Walsh’s classic riffs from “Take It To the Limit” to “Life’s Been Good.” Gill, 61, spoke in the breaks about the surreal joy of getting to play with the Eagles, but also, of the pain he felt watching his older brother succumb to alcoholism at a young age. That was over 25 years ago, Gill said. But as he began “Rocky Mountain Way,” it was clear that playing with Walsh in the Eagles was not just about childhood-dream fulfillment but about soothing a long open wound.
Walsh Goes To Rehab
After checking into rehab for the final time in 1995, Walsh had to put his guitar down — possibly for good — in order to put his life back together. He didn’t think he’d ever play again. Over the course of 20 years, Walsh got married and eventually found his way back to music with the help of Ringo Starr, his actual brother-in-law and brother in sobriety. In 2012, Walsh released Analog Man, his first solo album as a sober musician. “People tell me I play better now sober than I did before,” he said. “But the only thing that matters to me now is that I can say I haven’t had a drink today.”
Sitting side by side backstage, Starr and Walsh are an odd pair: one a voluble English drummer in violet-tinted spectacles, the other steely, platinum-haired guitar god. Although the Liverpudlian is only nine years older than Walsh, he has a sweet, avuncular way of leaping to answer questions as if moving the target away from his withdrawn brother-in-law. Walsh sits silently, turning the words over in his mind. But like a pitcher with a long windup, when Walsh speaks, it’s with surprising power.
Rolling Stone: You’ve both spoken at length about your alcohol and drug addictions. What was it like to become a public figure for something you tried for years to keep hidden?
Starr: Well I didn’t really come out publicly. They had helicopters flying over the arena, so that was how I came out. [Laughs.]
Walsh: I always tried to hide it. I had my vodka in a bag. Nobody knew. When really, half the world knew I was a mess. So, anonymity didn’t exist for me.
What changed your mind?
Walsh: I got sober because of a fellowship of men and women who were sober alcoholics. That’s how I got sober. After a couple years, I talked about [my sobriety] with other alcoholics and tried to help them. The only person who can get somebody else sober is somebody who’s been there and done that.
When did you make the decision though to become a public advocate?
Walsh: I realized that I do more good showing people that there’s life after addiction. So I decided it’s okay to go public because everybody knew anyway, and if I save one life showing that there’s life after addiction I feel good about it. I believe that’s part of why I lived.
Ringo, before you got sober, was there a fear that choosing sobriety would end your artistic life?
Starr: I was afraid at the beginning. [I thought] I don’t know how you do anything if you’re not drunk. That’s where I ended up. I couldn’t play sober, but I also couldn’t play as a drunk. So when I did end up in this rehab, it was like a light went on and said you’re a musician, you play good.
After rehab, that’s when you put together the First All-Starr band in 1989?
Starr: Yes, but it was weird. My lawyer in Los Angeles called me that they wanted to back me on a tour. I’ve never toured [solo]. But I put a band together. He [pointing to Walsh] was in it. It was practically an orchestra.
Walsh: He didn’t think everybody would come.
Starr: I didn’t think anybody would come. I only knew three drummers and I was one of them. But you know, a lot of people in that band weren’t sober. They were all sort of on something. But we pulled it together. For me personally, that’s all it’s about. I got over the mad first, second year, and now, this is how I live. It’s a normal way of living now, and I have a lot of fun.
Walsh: And now most of those guys [Levon Helm, Clarence Clemons, Billy Preston and Rick Danko] are dead.
Starr: Yeah. All the band’s dead.
What are your thoughts on the opioid crisis?
Walsh: Well, I don’t think America’s aware of how bad it is out there. And I’m talking about addiction across the board. Opiate addiction, it’s killing young kids by the hundreds – by the thousands.
A lot of young musicians, in particular, are overdosing. Do you think the pressure to constantly be on tour, to always be “on,” is connected to this trend?
Starr: Well in my case, early on, the pressures were just there. You’d have a drink and later on, it got to be cocaine or whatever.
What about for older musicians, who may push themselves with painkillers to keep up unsustainably rigorous schedules?
Walsh: We need to have a look at this, yes. The problem is if you hurt physically, you can get prescription pills for that. If you hurt mentally, you can drink – drink your way through it, you know? The problem is that after that pain is gone, whatever substance you used very subtly convinces you that you can’t do anything without it and then you have to deal with that. And people don’t know that.
Starr: The good news is, though, a lot of new artists are sober people. The part of it where musician felt it was their right to get crazy has changed. And we lost a lot of really good [musicians] because of that. Why we’re [gestures to Walsh] still here, I don’t know. That’s just how it is. But I think now in the new music age, it’s getting a bit cleaner. I think their rebellion is to stay clean. Like they’re going back to vinyl [smiles].
At this point, if you see or suspect a musician, with whom you’re close, is struggling with addiction, do you say something to them privately?
Starr: I don’t say a lot.
Walsh: That’s very frustrating because you can’t help somebody unless they’re ready. You can point it out to them. They might listen, they might get angry. You can be there for them and if they bring it up, talk to them. You can set an example and show them how much better it is to be sober. But no, we don’t drive around in cars looking for people and yanking them off the streets.
When you first got sober, was music ever the enemy?
Walsh: I was terrified. I was absolutely terrified to go in front of people sober and not have a really good buzz going.
Starr: We didn’t know how to do it.
Walsh: I was really uncomfortable maybe the first 10 times.
What about playing by yourself, just seeing if you could do it?
Walsh: I didn’t write for a year. I couldn’t write for a year because I’d sit down and try and write something and get frustrated, and my mind would say, “well you know what works…”
Starr: Yeah.
Walsh: And that wasn’t an option.
So you couldn’t write?
Walsh: Sobriety came first. And I thought well, maybe I will never write a song again, and that’s gotta be okay. It was the same thing with playing live. I was uncomfortable, but then other musicians would start coming up to me, saying, “Joe, you used to be really good, but there’s a profound difference in the way you’re playing now.”
What did they say?
Walsh: They said it made them want to get sober. And I have been able to get some people sober that way. But I was just in my own way. I was all about me. I was uncomfortable, and then one day I realized I could do it. I can do this. And after that, I can’t imagine doing any substance that would affect my playing sober now. I don’t even think about it.
What was playing sober first like for you, Ringo?
Starr: What happened to me is that playing was all right and being onstage and being in the front, but afterwards, my whole body screaming: let’s get crazy. [Alcohol] had always been the prize, do a gig and then you get crazy.
Walsh: It was your reward.
Starr: I used to have to sit on the [drum] seat and just hold [still]. Barbara couldn’t talk to me. People around me couldn’t talk to me. I’m just holding on because all my sinews and veins and brains were like, “Let’s get fucked up.” But I didn’t. That’s how it works. If [sobriety] is something you want, you can get it. Here it is. Come and get it.
Joe, can you tell me about the epiphany you had in New Zealand?
You said that you’d had a bunch of relapses and nothing had been working until that moment in the hills.
Walsh: It was in Hawke’s Bay, the ancient capital of the Maori nation, the indigenous people there. I befriended them in New Zealand and they took me to the capital fortress that is abandoned and in ruins now, but it’s a very holy place. I stood on top of that hill. I looked at the ocean and I looked at all this farmland. New Zealand is beautiful. I had a moment of clarity, which was you can either die or you can stop.
How old were you roughly then that happened?
Walsh: About 45.
Have you had other spiritual experiences like that in your life?
Walsh: I have had moments before, like “I’ve gotta do something about this,” but by noon I was drunk again. This time, I believe it was God saying, “Hey, why don’t you try me?”
So you literally walked down the mountain, determined to go back to rehab, and that time it took?
Walsh: Yes. I went back to the United States. I made arrangements to go in. It terrified me. Terrified me.
Why?
Walsh: Because I didn’t know what sober was. I thought I was going to have to wear a tie and have a job and go to work every day, and that’s not the case. No, I can do what I always do really well. I just had to learn how. When you get sober, you learn how to do everything one day at a time, and when you get enough things that you know how to do sober, you’re good to go.
Ringo, you once said in reference to the Beatles: “The world made us mean something.”
You seemed to be hinting at the objectification wrapped into being a so-called “legend.”
Starr: I think in my case, the blessing was I was in a band and we had each other. Yeah, after a couple months, one of us would be going off the rails whether someone was having to drag me back or drag George back or John. One of the saddest moments, nothing to do with drinking, was when we went to see Elvis. I felt really sad because he had 12 guys with him, only doing his bidding. He’d say something like, ‘Let’s play football.’ They’d all run out and play ball with him. Being a solo artist, it’s gotta be really hard.
Walsh: Yeah, and lonely.
Starr: I’m afraid I never had that in my life. I’ve always been with a couple of good bands and now still always in band. So I’ve had friends around. I think that’s very important.
Walsh: Well you can’t confuse success with validity. I just want to say when we — I mean folks like me — when we go onstage for two-and-a-half hours, we look really cool. We’re cool, you know? The rest of the day, people make the assumption that we’re cool then too, and we’re not. We’re just people with all the problems that everybody else has. It’s not as extravagant a lifestyle as it appears when we’re onstage. So don’t think being a rock star is the answer to all your problems. It’s the beginning of all your problems.
Starr: The discussion is very difficult, because we did as much as anybody did and we’re still here and we’re sober, and there’s no telling when that day is when you leave. I don’t know why Tom [Petty]’s gone and I’m here. It’s unanswerable. But I know in the bands I hang out with, there’s a pretty — not absolutely — but a pretty large sober mentality going on now.
The post Joe Walsh & Ringo Starr’s Mission To End Addiction appeared first on Reach Out Recovery.
March 20, 2019
Wendy Williams In Recovery
(CNN)Wendy Williams got incredibly candid during her show Tuesday about her struggle with addiction.The host of “The Wendy Williams Show” told viewers she is living in a sober house and talked about her past struggles with cocaine.”I have been living in a sober house,” she said tearfully. “You know, I’ve had a struggle with cocaine in the past. I never went to a place to get treatment. There are people in your family; it might be you. I want you to know more of the story.”Wendy Williams announces show hiatus due to Graves’ disease (2018)

Wendy Williams explains why she fainted on-air (2017)Williams returned to her hosting duties March 4 after more than two months on hiatus. She originally said she was stepping away to focus on health issues stemming from Graves’ disease, an autoimmune disorder that causes overstimulation of the thyroid. It can lead to eye inflammation, racing heartbeat, hand tremors, trouble sleeping, weight loss, muscle weakness and neuropsychiatric symptoms, according to the American Thyroid Association.But during her show, Williams revealed Tuesday that her absence has involved more than Graves’ disease.”Only (one person) knows about this — not my parents, nobody,” she said. “Nobody knew because I look so glamorous out here. After I finish my appointments, I am driven by my 24-hour sober coach back to a home that I live in the tri-state (area) with a bunch of smelly boys who have become my family.”We talk and read and talk and read and then I get bored with them,” she said. “Doors locked by 10 p.m., lights out by 10 p.m., so I go to my room and stare at the ceiling and fall asleep to come here and see you. So, that is my truth.”Williams’ fans initially became concerned in November 2017, after she fainted on air. Then in December 2018, Williams made headlines again when she slurred her speech on air.
The post Wendy Williams In Recovery appeared first on Reach Out Recovery.
Just 10 Minutes Of Exercise A Week May Be Enough To Extend Your Life
Exercising for just 10 minutes a week is linked to a longer life, according to a new study published in the British Journal of Sports Medicine.
Several recent studies have found that even low-intensity exercise, done for a short amount of time, can have a meaningful impact on health. Still, the idea that exercising for 10 minutes a week — less time than it takes to watch a TV show, do a load of laundry or make a pot of pasta — may be enough to increase your lifespan is novel. It’s also somewhat controversial since the federal physical activity guidelines recommend getting at least 75 minutes of vigorous aerobic exercise or 150 minutes of moderate aerobic exercise each week.
“Any dose of physical activity will be beneficial to human health,” study co-author Bo Xi, a professor and epidemiologist at the Shandong University School of Public Health in China, wrote in an email to TIME.
The study was based on data from more than 88,000 U.S. adults who participated in the National Health Interview Survey between 1997 and 2008. All of the participants were ages 40 to 85 and did not have any chronic diseases when they took the survey. They also provided demographic and health information, and were tracked by researchers for about nine years.
About 8,000 people died during the follow-up period, and the researchers found that virtually any amount of exercise reduced the risks of dying of cardiovascular disease, cancer or any other cause. These reductions in risk increased the more people exercised. Exercise has long been shown to improve cardiovascular health, and physical activity can help prevent obesity, which is linked to cancer.
What was interesting was how little physical activity it took to see benefits. People who got just 10 to 59 minutes of light-to-moderate intensity physical activity during their free time each week had an 18% lower risk of early death than people who were sedentary. They also had a 12% lower risk of dying from cardiovascular issues during the study and a 14% lower risk of dying from cancer, the data showed.
After that, the benefits accumulated. People who got 60 to 149 minutes of light-to-moderate exercise per week had a 22% lower risk of early death than sedentary people, and those who got 150 to 299 minutes had a 31% reduced risk. Getting 300 to 449 minutes of light-to-moderate physical activity per week was linked to a 33% lower risk of dying during the study period.
Contrary to some research that has found an upper limit to the amount of exercise that is healthy, the researchers found that there was seemingly no limit to the longevity benefits of exercise. Even the small group of people who got 10 times the amount of exercise recommended by the federal government — 1,500 minutes of exercise a week, or more than three hours a day — had a 46% lower risk of death than the least active group, the researchers found.
Still, observational studies like this one cannot prove cause and effect; they can only find patterns. The researchers also were not able to adjust for certain lifestyle factors that could affect mortality risk, including dietary habits and changes in physical activity over time. Despite these limitations, the study’s results are yet another endorsement of the power of physical activity, even in small amounts.
“To meet the minimum recommendations of the physical activity guidelines may be difficult,” Xi says, “but even low doses of physical activity will be useful, and more will be better.”
The post Just 10 Minutes Of Exercise A Week May Be Enough To Extend Your Life appeared first on Reach Out Recovery.
People Who Don’t Drink May Still Suffer Harms From Alcohol
From Science Daily:
Harms to people resulting from alcohol consumption by others in Germany in 2014 are assessed in a study published in the open access journal BMC Medicine.
Much of the research into alcohol-associated harms investigates harm to the drinker, not to other individuals. Researchers at Institute for Therapy Research in Bayern, Germany, estimated the harms caused to others by alcohol during pregnancy, in road traffic accidents, and as a result of interpersonal violence. The authors conclude that the harmful effects of alcohol on people other than the drinker need to be recognized as a public health problem, and effective ways of preventing such harms are required.
Dr Ludwig Kraus, the corresponding author, said: “This study estimates some of the most severe harms that alcohol use may cause to other people than the drinker, namely fetal alcohol syndrome (FAS), fetal alcohol spectrum disorders (FASD), road traffic fatalities caused by drunk drivers, and deaths resulting from alcohol-attributable interpersonal violence.”
The authors found that alcohol was responsible for 1,214 (45.1%) third-party road traffic deaths and 55 (14.9%) interpersonal violence deaths, and was implicated in 2,930 incidents of FAS and 12,650 cases of FASD. The authors note that FAS and FASD are not the only potential consequences of drinking alcohol during pregnancy. Overall, these results indicate that alcohol may not only cause harm to the drinker, but also substantial harm to third parties.
Dr Kraus said: “Although the estimates across the three harm domains are not directly comparable, the results suggest that alcohol use in pregnancy followed by road traffic fatalities account for significantly more harm to others than alcohol-related violence.”
To investigate the potential harm caused by alcohol to third parties, the authors examined survey data on the prevalence of alcohol use during pregnancy to estimate incidents of FAS and FASD in Germany. Cause-of-death statistics provided estimates of third party traffic deaths and interpersonal violence deaths thought to be caused by alcohol.
The authors caution that accurately assessing the prevalence and extent of alcohol use during pregnancy in Germany is challenging as the data are self-reported and so may be vulnerable to bias or misremembering.
Dr Kraus said: “Although measures such as pricing policies or limiting the marketing of alcoholic beverages are unpopular, targeted measures addressing particular populations at risk, such as women of childbearing age or road users, may help to reduce harms to others as well as harms to the drinker.”
The post People Who Don’t Drink May Still Suffer Harms From Alcohol appeared first on Reach Out Recovery.
When Does Social Drinking Become A Problem?
It’s a question many want to avoid. Where is the line that separates casual drinking and a medical disorder? Some say if you want a drink you’re not an alcoholic, but if you need a drink then you are (an alcoholic). Others say, at first the man has a drink, and then the drink has a drink, and then the drink has the man.” However, those definitions are open to many interpretations. How can we subjectively quantify alcohol consumption?
Alcohol Becomes A Disorder In Stages
Alcohol affects each person differently, and not every person who has one drink wants another drink. We’ve all known people who have a drink on celebrations and never want one otherwise. Many people define themselves as social drinkers but that is a description that’s hard to define. When I took a history from a patient in my office I would spend a fair amount of time on the social history. This includes:
Family history
Work and military history
Behavior history (what I call the drugs, sex and rock and roll history).
How much do they smoke and drink?
Do they use illegal drugs, etc.?
When a patient told me that they were a “social drinker” I would always follow with this question: well, how social are you? Some consider the yearly family celebrations (wedding, funerals, graduations, etc.) to be social while others consider every Friday night at the neighborhood watering hole to be social. Or every night.
A chemical addiction separates a drinker from an alcoholic, as do the reasons for drinking. According to the Journal of the American Medical Association roughly 50% of individuals with severe mental disorders are affected by substance abuse and 37 % of alcohol abusers and 53% of drug abusers also have at least one serious mental illness. Of all the people diagnosed as mentally ill, 29% abuse either alcohol or drugs.
Many get-togethers, both business and general social events, have the use of alcohol as part of the function. And there are a number of benefits that people obtain from social drinking.* First, alcohol is often described as a “social lubricant”. People tend to relax and open up as the alcohol helps them to feel less self-conscious. It also helps people unwind and forget responsibilities for a while.
One Sign Of A Disorder Is When Cutting Down Doesn’t Work
Often people have some awareness that they are drinking too much. They may have faced:
DUIs
Blackouts
Risky behaviors
They resolve to drink less, but can’t cut down. Getting help can mean starting a 12 Step program, having an addiction professional provide treatment in patient or outpatient setting. A continuum of care can also include daily alcohol testing to make sure the disorder is in remission and to insure accountability.
Whatever the outcome, it’s best to know what you are facing. Any situation can be improved by recovery, so be brave and take this self-assessment written by the NCADD (National Council on Alcohol and Drug Dependence). Here are a sampling of the questions:
Are you having black-outs?
Are you avoiding others who aren’t drinkers?
Have you tried to quit but find that you can’t?
Are you drinking to cheer up (and avoid obvious depression)?
Are you hiding your drinking? Putting it in your orange juice, or hiding it in your closet, etc.
Do you have skin changes on your face such as a flushed appearance and broken capillaries around your nose?
Do your hands tremble?
Are you having problems with loved ones because of your drinking?
If you don’t have a drink do you find yourself anxious, nauseated or have trouble going to sleep?
Do you have a drink in the morning? “The hair of the dog.”
* Information sourced by: http://alcoholrehab.com/alcoholism/so...
The good news is: Recovery is possible. Visit www.recoveryguidance.com to find treatment options near you. Recovery Guidance is a safe, commitment-free resource for patients.
The post When Does Social Drinking Become A Problem? appeared first on Reach Out Recovery.
Addictive Substances Trick The Brain
The brain can experience pleasure from all sorts of things we like to do in life; eat a piece of cake, have a sexual encounter, play a video game. The way the brain signals pleasure is through the release of a neurotransmitter (a chemical messenger) called dopamine into the nucleus accumbens, the brains pleasure center.
This is generally a good thing; it ensures that people will seek out things needed for survival. But, drugs of misuse such as nicotine, alcohol, and heroin also cause the release of dopamine in the nucleus accumbens, and in some cases, these drugs cause much more dopamine release than natural, non-drug rewards.

Substances Trick The Brain’s Reward System
Addictive drugs can provide a shortcut to the brains reward system by flooding the nucleus accumbens with dopamine. And, addictive drugs can release two to 10 times the amount of dopamine that natural rewards do, and they do it more quickly and more reliably (helpguide.org).
When Tolerance Develops People Need More
Over time, drugs become less rewarding, and craving for the drug takes over. The brain adapts to the effects of the drug (an effect known as tolerance), and because of these brain adaptations, dopamine has less impact. People who develop an addiction find that the drug no longer gives them as much pleasure as it used to, and that they have to take greater amounts of the drug more frequently to feel high.
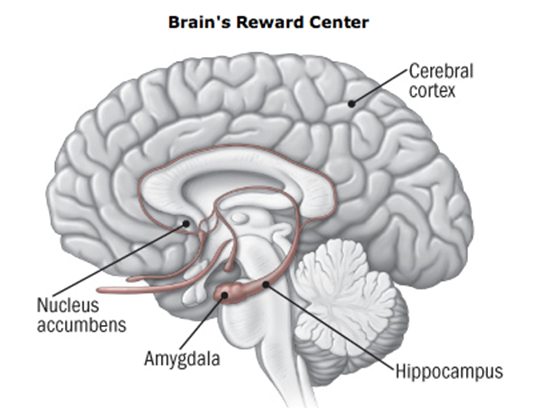
Below is a picture (helpguide.org) of the brain and the nucleus accumbens, in addition to some other brain regions that are affected by addition.
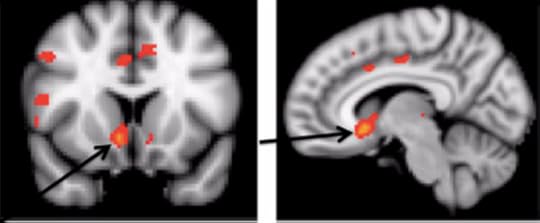
And, here is a picture from Recovery Research Institute’s own research of the brain activated by alcohol (Gilman et al., 2008). The nucleus accumbens is activated.
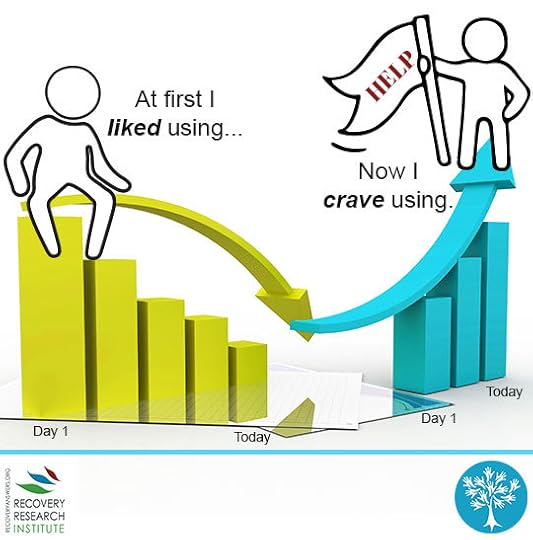
There is a distinction between liking and wanting the drug; as over time, the liking decreases and the wanting increases. Individuals with a substance use disorder continue to seek and use the substance despite the negative consequences and tremendous problems caused for themselves and for their loved ones, because the substance allows them to simply feel normal.
The post Addictive Substances Trick The Brain appeared first on Reach Out Recovery.
March 19, 2019
4 Empowering Changes To Make In Recovery
Understanding and accepting the factors that contribute to our thoughts, feelings, and actions can not only be useful, but very empowering when you’re on the road to recovery.
Once you are familiar with the environmental factors that are relevant to YOUR life, then you can take action to create change and improve the odds that you’re the one with the control—not the addiction. You’ll also find helpful tips for partners and family members who want to support a loved one in addiction recovery—since they make up a substantial portion of the environmental influence.
Four Environmental Domains That Contribute To Addiction
The way I see it, four environmental sub-domains that play a role in the development of addiction.
1. The Family Domain
There’s no denying that our early life experiences and familial interactions play an important role in the development of our mental health. You may not realize, however, just how critical those interactions and parenting styles can be and how they can contribute to later addiction.
Identify The Factors
Parents who have favorable attitudes toward drug use or use drugs themselves often have children who are more likely to use and drugs, and with the increased probability of use comes an increase in the probability of problems.
Additionally, parenting styles identified as authoritarian (highly demanding, little positive feedback, harsh punishments) or avoidant (difficulties responding to emotional needs of child and child learns to hide their emotions) also lead to increased substance use problems when compared to an authoritative (high responsiveness and high demand) parenting style. Better work on those boundaries early!
A NIDA funded study also found that addiction was more likely in individuals who had a sibling or spouse who had an alcohol or substance addiction. The closer the siblings were in age, the greater the relationship.2 While some may want to attribute the sibling connection primarily to biology, there is a substantial environmental influence for shared childhood households and it is obvious that the spousal relationship is largely environmental. Although, as we’ll discuss later, these factors are not truly independent at all.
If you can relate to these experiences, then you may begin to form a picture of the critical influence of family and why you have an addiction.
Opportunities For Change
I’ve mentioned the risk factors in the family domain which contribute to addictions, but family can also play a protective role. Research suggests that family support (and psychoeducation provided to family members) during the recovery process leads to higher recovery success in people with addictions.
If you have a family member with an alcohol or substance use disorder, then your support (both practically and emotionally) can go a long way in aiding the recovery of your loved one’s addiction.
2. The Peer Domain
It will come as no surprise that the people we surround ourselves with do have an impact on the choices we make and the way we behave. While you may associate “peer-pressure” with adolescence, the same factors that underlie this phenomenon can persist well into the adult years (I mean, who doesn’t still get affected by friends when it comes to fashion style, car-choice, and so many more factors?)
Identify The Factors
Stress in the workplace can lead to addiction. When under pressure, people draw on their default coping strategies—whether helpful or unhelpful—to help them manage how they are feeling. For those in the retail and food industries, the stress levels are incredibly high, and so too is the risk of alcohol and substance addiction.
According to a 2015 study by the Substance Abuse and Mental Health Services Administration, the food service and hospitality industry have the highest rates of substance use disorders and third-highest rates of heavy-alcohol use of all employment sectors.
In the school environment, a student’s performance, participation, and commitment to school can be a major risk factor in addiction. A lack of social structure can also contribute while some structures, like the Greek system, can exacerbate substance use struggles.5
Opportunities For Change
Research has shown programs addressing alcohol and other drug use in the workplace to be cost-effective, contributing to the health and well-being of the employee and organization.
When you study or work in an environment that actively promotes good mental health and a healthy lifestyle, then you are more likely to absorb these messages, feel safe to ask for help, and have the confidence to overcome an addiction. If you find that your work/school environments do not promote healthy habits, it is often possible to change these patterns through active engagement and discussion with decision makers. After all, this is your life!
3. The Community Domain
Your connection, or lack thereof, to the community in which you live plays a big part in the likelihood of developing an addiction. Additionally, social norms in a given context, culture and time define what is even identified as a problem.
Identify The Factors
Research shows that if an individual’s community has favorable attitudes toward alcohol and drug use, then their risk of developing a problem is increased.
Still, drinking averages have changed dramatically over the years. As mentioned above, the average amount of alcohol consumption in the U.S. has dropped to only 1/5th of what it used to be in colonial times! Now, if everyone was drinking five times more alcohol 200 years ago (on average), it is safe to assume that the threshold for calling someone a problem drinker, or “alcoholic,” was also higher. We don’t have great records from this time, so documentation is difficult, but moderate drinking standards have changed, meaning what used to be normal drinking is now considered deviant or excessive. Society’s rules and standards define the way we measure “addiction” and also create the perception of those who struggle and what is or isn’t OK (this is where shame and stigma come from).
Opportunities For Change
Funded by the National Institutes of Health’s National Institute on Alcohol Abuse and Alcoholism (NIAAA), a new report concluded that individuals with substance abuse problems who are living in a collaborative housing setting would have their addiction treated more effectively than abusers not residing in a community-based facility.
This means that people who reside with other people in similar circumstances who are in treatment are less likely to feel stigmatized and shamed.
But it goes much deeper than that: if social norms play such a crucial role in what addiction is, then it has to be obvious that biology alone (or psychology alone) cannot be the primary culprits in its development. And if we can understand that the lens through which we see “addicts” can have an incredible influence on their success and quality of life then we have to adjust our way of talking about addiction wholesale.
4. Other Factors To Consider
We have looked at the four big environmental domains, but there are a couple more factors worth mentioning that can also increase drug use and addictive behavior. These include:
Media consumption: Children and adolescents who are frequently exposed to media (advertisements, TV shows, and movies) containing alcohol and substance use can lead to addiction. The portrayal of alcohol and drugs in a favorable light can influence child and adolescent attitudes and behaviors around alcohol and drugs.
Proximity to drugs: Access to alcohol and drugs is one of the biggest contributors to first use (and ongoing use) of alcohol and drugs by children and young people.
Take Home Message
While environmental factors can contribute to a substance use problem, they can also help during the recovery process. If you’re seeking treatment for addiction, then you want to be aware of all the factors that contribute to your problem and not “box yourself in” by only focusing on the factors others believe to be important.
While we may think we have little control over biological factors (there is actually quite a bit we can do there too), and psychological factors can take time to resolve, the environmental domain is something you CAN make changes in with substantial payoff and relative ease. Whether it’s enlisting the help of your family, connecting with other people in your circumstances (who are motivated towards recovery), and ensuring the environments you work or study in are conducive to recovery, there is much you can do.
Here’s a little trick I recommend for everyone I work with that can help if there is a specific room or place that you tend to drink/use in more frequently. This room, or location, in your environment has become a trigger for your behavior. When you enter it or get near it, you likely begin craving or thinking about your drinking, using, or engaging in your addictive/compulsive behavior. But here is where biology and environment can meet. Since your brain recognizes specific aspects of this place in order to create the overall picture and therefore the connection with the behavior, there’s an opportunity to intervene! Change the look of the room as completely as possible—move furniture around, paint the walls or add wallpaper or art, change the scent and the lighting. If you do this, you’ll notice that much of the power of the trigger has dissipated because your brain now thinks of this location as different. It’s a quick and easy fix for the vexing problem of bedroom/living-room/kitchen drinking that, while not a silver bullet, should give you a little relief. Here’s what’s important though—if you simply continue using in that room moving forward you’ll create the exact same old relationship with the new environment… So beware.
If you have a family member with an addiction and you’ve begun to lose hope, then you’ll find that what you say and do will make an impact on your loved one. Learn about the multitude of factors relevant to your loved one and try to have inclusive and supportive conversations with them about what you learn. Your support and understanding could go a long way.
I find environmental factors the most helpful in leading clients to see how powerful their surroundings, community, relationships, and home can lead toward health or relapse. Our environment has an incredibly strong influence on our behavior and the way we see the world.
Content originally published by Psychology Today:
The post 4 Empowering Changes To Make In Recovery appeared first on Reach Out Recovery.
Grieving A Loss That Shouldn’t Have Been
From Alexis Coleman @ Nicholson Student Media: Natalie Madruga, 24, stares endearingly at a photo of her and her father, Manny, taken before his death.
Like many people who have dealt with the loss of a parent, UCF graduate student Natalie Madruga handled her father’s death by staying busy. She worked extra hours, did volunteer work and said she never gave herself time to breathe.
Madruga, 24-year-old rhetoric and composition student, was devastated when her father, Manny, a criminal prosecutor in their hometown of Key West, Florida, died by suicide in 2016.
In the weeks and months that followed, Madruga said she stayed preoccupied by making empty promises and obligations to friends and school events — anything to avoid the topic or the reality of her father’s death.
“I kept myself really busy,” Madruga said. “I said ‘yes’ to everything, [and] I made millions of empty promises. I tried to be around people at all times just because I was avoiding it. I thought that meant that I was doing okay. It did not mean I was doing okay.”
UCF’s Counseling and Psychological Services writes that doing excessive work or going to extremes to avoid thinking about loss are signs someone is facing the death of a loved one and needs support.
In March 2017, four months after her father’s death, Madruga began attending the support group Healing After a Loved One’s Suicide, or HALOS, in Orlando. From there, she said she started her grieving process and began to cope.
According to the Centers for Disease Control and Prevention, suicide increased by 30 percent in the U.S. from 2000 to 2016.
While in HALOS, Madruga said a phrase that helped her begin to accept her father’s death was, ‘Grief is not your enemy — it’s your companion.'”
Now, she said she leaves photos of her father around her apartment to help her cope, and she listens to a CD he made for her featuring a song called “Never Alone” by Jim Brickman.
Madruga also attends an event in Key West dedicated to her father called the Manny Madruga Domino Tournament. There have been three domino tournaments, and she’s been to two. The event, which is hosted by the the Rotary Club of Sunset Key West, originated from one of her father’s ideas to raise scholarship money for Key West High School seniors interested in law.
In addition to raising scholarship money, the tournament also donates funds to suicide awareness and prevention programs, according to a Facebook post by the Rotary Club of Sunset Key West. The annual event started January 2017.
Occasionally, at the end of the event, Madruga said she leaves her father’s favorite drink — a Long Island Iced Tea — on a table with his name, birth date and the date of his death.
“I want him to be remembered more for what he did when he lived than how he died,” Madruga said. “But I don’t want people to forget how he died either. I don’t want it to be the only thing in the picture, but I also don’t want it to be erased.”
Sarah Mouradian is another member of the community of UCF students who has faced coping with grief after the death of a parent. Mouradian graduated from UCF with a bachelor’s degree in writing and rhetoric in 2018 — only months after her mother, Linda, died of a stroke stemming from sepsis. Mouradian had already lost her father, Greg, at the age of 5 in 2002 due to complications from multiple sclerosis.
Even after her father’s death during her childhood, Mouradian said she had family members around her to provide memories and remind her of her father’s love. Mouradian said while it was tough adjusting to everyday life after her mother’s death, she was able to accept it in time. After losing her mom, she said it helped to have people surrounding her who encouraged her to talk about it.
“Thankfully, I have my friend [Emily Auschwitz] and her parents,” Mouradian said. “They were really supportive, and even though I don’t have any family down here [because] all my family is still in Michigan, they’re like my family.”
According to the CAPS website, receiving support from those in your life such as family, friends or a religious group can help with the healing process.
CAPS Associate Director Teresa Michaelson-Chmelir said connecting with a friend or doing activities that can bring happiness are forms of self-care, which she said she encourages during the grieving process.
“It could be anything from being involved in some physical activities to someone who’s more of an artist,” Michaelson-Chmelir said. “Maybe it could be creative expression through art and music, movement even, so I would encourage the person as they are processing their grief and loss to engage in self-care and whatever that self-care might look like to them.”
To cope, Mouradian said she keeps items of sentimental value from her mother, such as a box of soaps and perfumes and a Minnie Mouse T-shirt.
Walt Disney World itself is home to a special memorial for Mouradian’s mother that Mouradian visits every month. She and her mother had a photo of them together etched onto the Leave a Legacy monument at Epcot in 2006. While the Leave a Legacy program was discontinued in 2007, Mouradian’s photo with her mother remains on display as a reminder of happy times.
Mouradian also credits her Catholic faith — which she said her mother instilled in her — with helping during moments of sadness.
“One thing that I’m really grateful for to her is her faith that she had,” Mouradian said. “She set a really good example for me. Even though I’ll feel sad right away, I know I’ll see her again, and I can still talk to her because I know she’ll still hear me … so that kind of helps, too. Knowing that that’s not the end of her. There’s hope to be reunited again.”
For students coping with death, CAPS offers a counseling group called Grief and Loss. According to the CAPS website, students within the Grief and Loss group are given a safe and supportive space to talk about their loved ones and learn ways of responding to loss while going through the grieving process.
According to a document from CAPS about how to cope with grief, it’s important for people coping with loss to grieve at own their pace, while others should understand that everyone’s unique type of grief deserves respect. A person is free to express their emotions by doing anything from talking to journaling to crying.
“A person has their own unique and individualized way of processing grief,” Michaelson-Chmelir said. “No two people are alike. Each person will have their own journey.”
Within the healing journey, Michaelson-Chmelir said that it’s encouraged for individuals to remember their loved ones however they choose to do so.
“If they want to remember the good thoughts [they can]” she said. “Sometimes even the sad memories are part of the story [and] part of the relationship they had.”
Michaelson-Chmelir also said although the pain of losing a loved one can lighten over time, loss is a feeling that never really fades.
“The person will continue to experience the loss throughout their life, but the pain will lessen over time,” Michaelson-Chmelir said. “There’s no way that person will ever fully get over that, but they will as the years pass.”
The post Grieving A Loss That Shouldn’t Have Been appeared first on Reach Out Recovery.





