Leslie Glass's Blog, page 281
March 30, 2019
25 Tips To Help Teens Coping With Grief
Most teens know someone who passed away do to drug or alcohol use. The loss may be the friend, or sibling, who is no longer able to attend school or be part of your life because of his or her lifestyle. Or it may be someone who died in an accident resulting from alcohol use, or by overdose, or suicide. Any death of this kind is devastating and traumatic. The closer you were to the person who’s gone, the more painful it is. Know that you are not alone in your grief, and that thousands of others are suffering just like you.
Managing Grief In A Healthy Way
We’re going to give you a list of the things you can do to help you, but it’s important to know that you have the power to help yourself. Asking others for help is the most important thing you can do for yourself, plus, it helps them as much as it helps you. People around you want to help–friends your own age, relatives, teachers, counselors, your spiritual leaders all find hope and comfort in comforting you. That’s important to know.
It IS A Big Deal While Your Heart Is Broken
The trauma of losing a loved one at this age in this way is something that can cause lasting hurt. While coping skills are often similar to how adults cope with grief and loss, you also may find some healing techniques to be unique to being an adolescent. Let’s explore these techniques.
25 Coping Skills For Grief
It’s healthier to admit your heart is broken – let yourself feel the grief.
There’s no right or wrong way to grieve. Your feelings, anger, sadness, and hurt are all normal. You’ll have many feelings, some of which may be disturbing. Those are the ones you need tools to deal with.
Some deaths are more difficult to cope with than others, no question about that. Avoidable deaths can hurt even more.
Grief is a rollercoaster. Sometimes you’ll be calm and sad. Other times you overwhelmed by what went wrong and feel as though you can’t cope.
You may feel guilty, especially if the friend died from an overdose and you were there. If you had given up on them and were not there to help, know that they chose to use and it’s not your fault.
Hormones may contribute to overwhelming feelings such as despondency, despair, depression, and because of this, you may have thoughts of suicide.
If you feel suicidal, immediately talk to someone you trust such as a parent, a teacher, or a counselor call the teen suicide hotline.
Your thoughts and feelings are nothing to be ashamed of. You don’t need to feel embarrassed.
Be open and honest with friends about how you feel.
Thoughts and feelings aren’t facts – if you feel suicidal, it doesn’t mean you have to attempt suicide, or you will attempt suicide. It means that you are in significant pain and you need help. Tell someone.
It’s common to feel angry, hurt, or abandoned because someone died and left you, or chose using over you.
Don’t develop unhealthy ways to try to cope with the loss – using substances, skipping school, or cutting yourself. Again this is the time to find someone who can help you.
There are many to cope with your feelings that don’t involve talking about it over and over or hurting yourself. You can write in a journal, draw, exercise, create a memory book of the loved one, put flowers on a grave. You can attend the funeral.
It’s perfectly possible to grieve, laugh, do well at school, and have fun at the same time. You’re one person, but have lots of different parts that can be nourished in so many ways.
Yes, there will be plenty of gossip about the person who has died. This can be especially painful if it’s your closest friend, a sibling, or a parent. Try to let it go. Gossip is just that.
You may feel that the world is now an unsafe place or that your belief system has been damaged – explore ways to feel safe and to think about life’s meaning.
Watch out for numbing yourself from the pain in order to try to feel better – numbing doesn’t work in the long run.
Be careful not to just throw yourself into school or work as a way to cope. Everything in moderation.
Use social media to help you as there are numerous ways to learn, cope, and heal through grief, including online grief support groups.
Make sure you are doing the basics in life – eating healthy, resting and sleeping, exercising.
Ask others questions regarding life and death.
Seek a spiritual mentor if religion and spirituality are important to you. Or do spiritual activities such as praying, having fun, playing in nature, being creative, meditating, discussing spiritual questions.
Be kind to yourself and others.
Consider counseling at school or outside individual or group therapy.
Understand that by working through the pain, while it won’t totally go away, you can grow and heal and also help others.
While grief is heart-wrenching, you can go beyond surviving the sorrow to once again, being able to thrive and enjoy life’s ups and downs.
The post 25 Tips To Help Teens Coping With Grief appeared first on Reach Out Recovery.
March 29, 2019
Lindsay Lohan’s Beach Club Recovery
From Psychology Today:
What is recovery and has Lindsay Lohan achieved it?
Lindsay Lohan is back. After a youthful superstar career when—between 1998 and 2007—Lohan’s films earned an estimated half billion dollars, she entered a period of drunken misbehavior, arrests, rehabs, and failed efforts at sobriety—meaning abstinence.
In a disturbing 2014 series with Oprah, Lindsay, Lohan still appeared to be at loose ends—and drinking. This, after Oprah elicited from Lohan a hesitant concession that, as she learned in rehab, she was an “addict.” Ultimately, even Oprah was forced to conclude that Lohan had failed.
But in 2019, the 32-year old Lohan is no longer trying to be a movie ingenue. Instead, she is trying to pass as a mature adult who manages a Greek beach club she co-owns. And, yes, the club serves alcohol.
How’s she doing? Whatever the merits of the MTV series, Lindsay Lohan’sBeach Club, as TV, Lohan does seem to be a hands-on, demanding manager:
“‘She’s really strict. But that’s being a boss—you have to be a hard a** sometimes. She’s very personable so you get to know her as a person. She’s been through a lot too.’ Said employee Sarah Tariq.
When the interviewer asked if she would be the new Lisa Vanderpump, Sara responded: “Um…I think Lisa Vanderpump might be nicer.”
Lindsay might agree. She’s already made headlines for telling one of her employees on social media to change her shoes to match her uniform. It was later revealed that the worker was fired.”
The rumors have already emerged that Lindsay has been seen drinking. “Uh-oh,” those knowledgeable about recovery declare, “she’s living out her life-long identity as an addict.”
So, can Lohan really be in recovery if she is no longer in AA, long past rehab, and possibly continuing, in her thirties, to drink?
Well, yes. In fact, contrary to the standard view of addiction and recovery, as I outlined in Psychology Today and PT blogs, hers is the actual route to recovery achieved by most adults. As people age, acquire new responsibilities, and assume age-appropriate maturity, whether they drink or not is irrelevant to their sobriety.
While writing such things (particularly in Psychology Today) has gotten me into a great deal of trouble, times have changed. The term “harm reduction” has come to stand for the idea that people can still use substances (as after all, in one form or another, virtually all of us do) and fulfill their adult obligations, as it seems Lohan is doing:
“Everybody has this idea that Lindsay goes out all the time,” Panos (her business partner), who clearly adores Lohan, told me. “That’s not her. Her normal life standard is staying at home. She cooks this recipe called borscht that is delicious. She introduced the series Pose to me and we watched the whole thing in two days. We’re like family.” But when it comes to business, Panos said, Lohan is still appropriately wary: “It’s true she trusts me, but that doesn’t mean that she doesn’t keep her eyes on me all the time.” Of course, Panos also added, “And I have my eyes on her all the time.”
Yes, keeping your eyes on your business partner when your money and reputation are on the line is a necessary part of being an adult. So be it.
And, while we’re at it, Lindsay looks fabulous.
P.S. I laid this all out ten years ago in WSJ


The post Lindsay Lohan’s Beach Club Recovery appeared first on Reach Out Recovery.
Here’s What Happened When I Tried Mantra Meditation During The Hardest Month of My Life
From Yoga Journal:
Hint: It helped. A lot.
If someone would’ve told me back in December that the first month of 2019 would be the hardest of my life, I probably would’ve thought twice before signing up for Yoga Journal’s 30-day meditation challenge. Because let’s be honest: Meditation is the exact opposite of running away from your problems. Instead, it inspires you to sit your butt down right in the middle of those problems and face your resulting emotions head on.
In January, all I wanted to do was run away from my ongoing relationship problems, self smack-talk, and most significantly, the immense sadness from the death of my beloved aunt.
Yet even though there were many days that stared at my cushion with pure, unadulterated resentment, or put off my practice until the end of the day, I can honestly say that the practice completely transformed how I handled some of the most challenging times I’ve ever faced. It not only gave me the space to confront my feelings, but it also helped me learn how to take care of myself along the way.
Introducing Myself to Mantra Meditation
I’ve been consistently meditating for a little over a year now, practicing everything from guided 10-minute meditations on the Calm app to classes at MNDFL meditation studio in New York City. However, I would say my relationship with meditation didn’t become a real commitment until I got a meditation cushion for my apartment about five months ago. It’s dramatically changed my practice, which used to happen in my bed. (You can imagine how that went on the days I was tired.)
Even though I had heard positive things about mantra meditation—a practice where you silently repeat a mantra, which you either choose for yourself or is given to you during an initiation—I was pretty intimidated by it. However, when I spoke with Alan Finger, meditation teacher and author of Tantra of the Yoga Sutras: Essential Wisdom for Living with Awareness and Grace, he told me that mantra, just like asana or pranayama, is simply a tool used to alter the consciousness. “When practicing with a mantra, it’s important to say the mantra aloud first, so that you can feel the sound vibrations in the body,” he told me.
As a somewhat experienced meditator, mantra meditation was still very new to me. I didn’t really have a plan to choose a mantra, but after practicing alongside Hilary Jackendoff in a guided meditation video, she helped me discover “So Hum,” which means “I am that.” Finger mentioned that different mantras can be used for different feelings, such as sleeplessness, anxiety, depression, and more, but this mantra felt pretty versatile, so I stuck with it.
Jackendoff taught us to meditate with the mantra, using the breath. On every inhalation, I would silently say the word “So.” On every exhalation, I would silently say the word “Hum.” I’m used to meditating with my breath, so this seemed doable.
Week 1: When Sh!t Hits the Fan, It’s Time to Sit
Disclaimer: I didn’t meditate at all the first two days of January. I also didn’t work out or eat healthy (some of the habits I stick with regularly). I was feeling really down on myself, because January is supposed to be a time to start new habits, eat clean, and get fit—and I felt like I blew it already. It sounds ridiculous, but that is my thought process sometimes. When my good habits don’t happen, I tend to beat myself up.
Then, as I was working at my laptop on the third day of January, I had a thought and told myself: You can sit here, work, and feel miserable—or you can take a 20-minute break, step away from your laptop, and meditate.
It took everything in me to walk upstairs and grab my cushion, but I was desperate to feel better, so that’s exactly what I did.
Week 2: When “I am that” becomes “I am love”
After my first week of mantra meditation, I felt like a weight had been lifted off of my shoulders. Suddenly, my goals for the new year weren’t tied to perfecting myself through diet and exercise, but instead, doing something every day that made me feel loved—and meditation became that thing. I switched my mantra. Instead of silently repeating So Hum, I started repeating “I am” on every inhalation and “love” on every exhalation. I found myself looking forward to making a cup of tea, plopping down on my cushion, and sitting for 20 to 30 minutes every day.
Having a week of solid practice under my belt really helped me for what was to come. Because my theme for 2019 is self-love, I became hyper aware of my relationships—with myself and with others. My boyfriend and I got into an argument in the beginning of the month and I wasn’t able to let it go. Every time we tried to talk about it, we couldn’t come to a fair conclusion.
During the second week of my meditation, the lingering argument kept coming up in my meditation. I would sit on the cushion, silently repeat my mantra, and cry. How could I practice “I am love” if I didn’t feel loved? How could I love him if I kept beating myself up?
So, what did I do? I continued to sit, to cry, and to come back to my breath. Giving myself that space during meditation allowed me to tap into what I was really feeling. It also gave me the space to go to my boyfriend later that week with a calm heart. Instead of arguing, we were able to have a productive conversation. I truly believe that if I didn’t give myself that space, we would still be arguing today about the same thing.
Weeks 3 and 4: Sitting with Sadness
For the past eight months, my beloved aunt had been living with metastatic breast cancer—the terminal kind. On January 21, she passed away.
A few days before her death, I my mom called me to let me know it was time to come home. I took a bus from New York City to Maryland on the morning of January 21 and repeated my mantra for about 25 minutes. An hour into my journey, my brother texted me to tell me that my aunt had passed away.
In the days following my aunt’s death, I felt so much hurt I didn’t even realize was possible. Every time I came to my meditation cushion, I would cry, breathe, and simply sit in a feeling of numbness. The cushion gave me space—to feel sad, to mourn, to feel angry, and sometimes, to do nothing. Every time I came back to my mantra—“I am love”—I remembered that my aunt wouldn’t want me to live in grief and sadness. It was inevitable to feel these emotions, sure. But I realized the only way these feelings would pass is if I really felt them.
The difference I noticed thanks to my new mantra meditation practice happened when I wasn’t on my cushion. Every single day after my aunt passed, I would ask myself how I could bring a little more love into my day. Some days that meant resting and watching movies with my mom. Other days that meant working out, going for a long walk, or spending time with friends.
Moving Forward with Mantra
Now that it’s February, I still hold my mantra in my heart. I still ask myself every day, “How can you bring more love into your day?” or “What will make you feel more loved?” I think I will continue to keep my mantra in my practice until something else seems like a better fit. Just as Finger told me, there’s a mantra for everything—and I look forward to discovering more mantras as my life’s journey, and all its ups and downs, unfolds.


The post Here’s What Happened When I Tried Mantra Meditation During The Hardest Month of My Life appeared first on Reach Out Recovery.
Equine Assisted Therapy: A Unique and Effective Intervention
From Psychology Today:
Equine therapy alleviates multiple emotional and behavioral struggles.
There is increasing recognition and integration of Equine Assisted Therapy in the traditional mental health field. Growing evidence supports the effectiveness of treatment with horses in a therapeutic environment. Studies have resulted in a body of literature supporting the therapeutic value of the human-animal interaction. Equine Assisted Therapy can help clients with depression, anxiety, ADHD, conduct disorders, addiction, trauma, eating disorders, spectrum and health difficulties, dissociative disorders, Alzheimer’s disease, dementia, and other mental health difficulties.
What is Equine Assisted Psychotherapy?
Equine Assisted Therapy is a form of experiential therapy that includes horses and a specialist psychologist or counselor working together with a client to create positive change. The therapist is specifically trained in Equine Assisted Therapy in conjunction with traditional training in the mental health field. Equine Assisted Therapy often includes a number of beneficial equine activities such as observing, handling, grooming, groundwork, and structured challenging exercises focused on the child’s or adolescent’s needs and goals. Equine Assisted Therapy provides unique non-verbal opportunities for the client to enhance self-awareness, recognize maladaptive behaviors, identify negative feelings, and face self-defeating cognitions. It may be used for clients with psycho-social difficulties and mental health needs that can result in significant changes in cognition, mood, judgment, insight, perception, social skills, communication, behavior, and learning.
Benefits of Equine Assisted Therapy
In light of research and observational findings, experts suggest that Equine Therapy—a common form of animal-assisted therapy–may yield a variety of psychotherapeutic benefits in the following domains:
Trust: The first step in Equine Assisted Therapy is to trust the horse, the therapist, and yourself. This is a profound step towards growth in interpersonal relationships and healing. Learning to trust an animal such as a horse is very powerful in the development and restoration of trust for those whose ability to trust has been violated by difficult life experiences.Anxiety Reduction: Research on the human-animal interaction indicate that contact with animals and horses significantly reduces physiological anxiety levels. Some children and teens are initially afraid of horses. With the support of an expert therapist and a trained therapy horse whose genuineness and affection help allay these fears, children are empowered to embrace therapy to diminish anxiety.Depression and decreasing Isolation: Depression is frequently associated with feeling rejected by peers, feeling different from peers, and feeling left out. Depression is an intrinsically isolating experience. The horse’s unconditional acceptance non-verbally encourages children and adolescents back into the camaraderie of life to engage in positive social interactions that decrease depression and isolation.Mindfulness: Equine Assisted Therapy integrates mindfulness at almost every step as the child learns to be present, in the moment, calm, centered, focused, and fully engaged. Horses are very sensitive and pick up on others’ emotions quickly, and accurately reflect these feelings in mirroring ways to the child. One can almost experience it as bio-feedback, but it the dynamic between the child and the horse that is creating the feedback loop. With mindfulness, the child is able to learn new, positive ways of being, which has a significant impact on cognition, feelings, and behaviors associated depression, anxiety, trauma, obsessions, impulsivity, emotional regulation, and other mental health issues.Self-Esteem: Children’s confidence is enhanced as they challenge themselves to learn and master new skills. They improve their ability to tackle new projects and challenges in a natural, non-competitive, and non-judgmental environment, which leads to improved confidence, self-assurance, and self-esteem.Impulse Regulation: Children and teens who struggle with impulse control and emotional regulation can benefit tremendously from Equine-Assisted Therapy. The need to communicate with a horse calmly and non-reactively promotes the skills of emotional awareness, emotion regulation, self-control, and impulse modulation. Equine-Assisted Therapy is effective in reducing children’s irritability, agitation, and impulsivity, and increases cooperation, emotional regulation, capacity for delay, and behavioral control.Self-Efficacy: Experiencing success with challenging exercises and goal focused activities in non-verbal ways fosters initiative, problem-solving, and renewed internal feelings of self-efficacy. Experiences of “I did it!” replace feelings of helplessness and lack of motivation, empowering the child and adolescent to take on challenges in many areas of coping and healing.Positive Identity: As the horse and therapist work in close alliance with the child and adolescent, a gradual sense of acceptance and feeling ‘liked’ emerges to enhance the child’s positive self-concept and identity. The child bonds with the horse to create a positive and healthy relationship that fosters the child’s identity and self-definition. Communication: Learning to communicate and achieve harmony with a large animal promotes intuition, stepping outside of one’s comfort zone, and patience. Horses’ sensitivity to non-verbal communication assists children to develop greater awareness of their emotions, the non-verbal cues that they may be communicating, and the critical role of non-verbal communication in relationships.Growth With Nature: Through Equine Assisted Therapy children and adolescents have a unique opportunity to encounter the outdoors from a new perspective. Feelings of joy and connection are often discovered or revived as children experience nature’s beauty in a renewed way. Especially for children and teenagers, engaging in therapy in a more natural, peaceful, outdoor environment greatly enhances the benefits of therapy.Self-Acceptance: Many children are initially concerned that they will do something embarrassing while learning about and interacting with the horses. Yet children quickly learn that every individual has their own equine experience, and they learn to focus inwardly on their comfort level in their own skin as opposed to making comparisons. Fears of embarrassment in public are thereby often reduced and self-acceptance increased. Children and adolescents also learn that progress is a journey, and self-acceptance for every phase of that journey is critical to resilience.Social Skills: Equine Assisted Therapy supports children in learning appropriate non-verbal and verbal communication, receiving and understanding positive and negative feedback, reciprocity in relationships, assertiveness, initiative, and engagement. It is very powerful in moving children who are socially isolated or withdrawn to a more open, positive, and appropriate social platform. A positive relationship with a horse is often the first, safe step toward practicing the social skills needed to initiate closer relationships with people, learn trust, and engage in social reciprocity.Assertiveness: Working effectively with a large animal can be intimidating and Equine Assisted Therapy provides the foundation for children to learn how to be more assertive, clear, and directive. Communicating effectively with a horse and engaging in challenging exercises that include the horse foster the child to demonstrate initiation, assertiveness, and direction; all important skills that enable them to express their needs and feelings more effectively in relationships.Boundaries: Many children and adolescents have experienced prior relationships as controlling, traumatic, conflictual, or untrustworthy. Healing takes place as they discover that the relationship with horses occurs within the context of a healthy, safe, and mutually respectful relationship between themselves and the horse. Children quickly learn that although physically bigger and more powerful, the horse typically mirrors the child’s emotions and operates within the boundaries of this safe and mutually caring relationship.Creativity and Spontaneity: Many children with socio-emotional difficulties may be emotionally inhibited, rigid, or despondent, and are likely to have lost some sense of spontaneity. The creativity, spontaneity, and playful aspects of Equine Assisted Therapy and equine activities can help restore spontaneity, creativity, and ability for healthy recreation and play.Perspective and Giving: By developing a caring and nurturing a relationship with a specific horse, the child develops a positive attachment outside of their home and school. Through grooming activities and caring for the horse, children are able to learn to give, nurture, connect, and put aside the absorbing focus of their struggles, self-defeating thoughts, negative, sad emotions, and anxious ruminations, and instead direct their attention and thoughts externally toward safe and caring interactions.
Equine Assisted Therapy can be a powerful and magical way to assist our children and adolescents in multiple social, emotional, physical, cognitive, and behavioral domains. Equine Assisted Therapy is being recognized as a more integral part of psychotherapy and mental health and can serve as a unique and effective intervention that should be considered as a resource by parents and professionals.


The post Equine Assisted Therapy: A Unique and Effective Intervention appeared first on Reach Out Recovery.
Second Man Found Dead In Democratic Donor Ed Buck’s Apartment Also OD’d On Meth
From NBC News:
Timothy Dean, 55, was found dead in Buck’s apartment after Gemmel Moore, 26, died there in July 2017.
The second man found dead in the span of two years in political activist and prominent Democratic donor Ed Buck’s West Hollywood apartment died of a methamphetamine overdose, the Los Angeles Sheriff’s Department said Monday.
Timothy Dean’s death Jan. 7 was ruled accidental by the coroner’s office, the sheriff’s department said.
Dean, 55, was found dead in Buck’s apartment after Gemmel Moore, 26, died there in July 2017. Moore’s death was also ruled as an accidental overdose of crystal methamphetamine.
Police did not charge Buck with any crime, but last month, Moore’s mother, LaTisha Nixon, filed a wrongful death lawsuit against Buck, Los Angeles District Attorney Jackie Lacey, the assistant district attorney and others.
Nixon said she had found Moore’s personal journal in which Moore wrote that Buck had made him hooked on crystal meth by injecting him with the dangerous drug.
The 24-page lawsuitaccuses Buck of wrongful death, sexual battery, assault, battery, negligence, civil rights violation, hate violence and drug dealer liability.
Many of the lawsuit’s claims against Buck had previously been alleged by journalist and activist Jasmyne Cannick, who, along with other activists, publicized Moore’s journal and delivered a 30,000-signature petition demanding local authorities reinvestigate and indict Buck.
“This lawsuit helps to protect a very vulnerable population of gay black men by exposing details of Buck’s predatory and racially-discriminatory actions against gay black men,” said Nana Gymafi, human rights and criminal defense attorney and co-counsel for Nixon.
A year after Moore died, Cannick had posted a warning to Twitterthat another black man was likely to die in Buck’s apartment.
In a statement provided to NBC News at the time, Seymour Amster, Buck’s attorney, said, “On behalf of Mr. Buck, we categorically deny all allegations of wrongdoing and look forward to litigating this matter in a court of law.”
A call to Buck’s lawyer for comment was not immediately returned.
The district attorney’ office declined to comment on the lawsuit.


The post Second Man Found Dead In Democratic Donor Ed Buck’s Apartment Also OD’d On Meth appeared first on Reach Out Recovery.
Can What We Eat Affect How We Feel?
From The New York Times:
Nutritional psychiatrists counsel patients on how better eating may be another tool in helping to ease depression and anxiety and may lead to better mental health.
The patient, a 48-year-old real estate professional in treatment for anxiety and mild depression, revealed that he had eaten three dozen oysters over the weekend.
His psychiatrist, Dr. Drew Ramsey, an assistant clinical professor of psychiatry at Columbia University, was impressed: “You’re the only person I’ve prescribed them to who came back and said he ate 36!”
Dr. Ramsey, the author of several books that address food and mental health, is a big fan of oysters. They are rich in vitamin B12, he said, which studies suggest may help to reduce brain shrinkage. They are also well stocked with long chain omega-3 fatty acids, deficiencies of which have been linked to higher risk for suicide and depression.
But shellfish are not the only food he is enthusiastic about. Dr. Ramsey is a pioneer in the field of nutritional psychiatry, which attempts to apply what science is learning about the impact of nutrition on the brain and mental health.
Dr. Ramsey argues that a poor diet is a major factor contributing to the epidemic of depression, which is the top driver of disability for Americans aged 15 to 44, according to a report by the World Health Organization. Together with Samantha Elkrief, a chef and food coach who sits in on many of his patient sessions, he often counsels patients on how better eating may lead to better mental health.
The irony, he says, is that most Americans are overfed in calories yet starved of the vital array of micronutrients that our brains need, many of which are found in common plant foods. A survey published in 2017 by the Centers for Disease Control and Prevention reported that only one in 10 adults meets the minimal daily federal recommendations for fruit and vegetables — at least one-and-a-half to two cups per day of fruit and two to three cups per day of vegetables.
Nutritional psychiatrists like Dr. Ramsey prescribe antidepressants and other medications, where appropriate, and engage in talk therapy and other traditional forms of counseling. But they argue that fresh and nutritious food can be a potent addition to the mix of available therapies.
Americans routinely change what they eat in order to lose weight, control their blood sugar levels and lower artery-clogging cholesterol. But Dr. Ramsey says that it is still rare for people to pay attention to the food needs of the most complex and energy-consuming organ in the body, the human brain.
The patient Dr. Ramsey was seeing that day credits the nutritional guidance, including cutting down on many of the processed and fried foods and fatty meats that used to be part of his diet, with improving his mood and helping him overcome a long-term addiction to alcohol.
“It’s one part of the whole package that helps alleviate my depression and helps me to feel better,” he said.
Research on the impact of diet on mental functioning is relatively new, and food studies can be difficult to perform and hard to interpret, since so many factors go into what we eat and our general well-being. But a study of more than 12,000 Australians published in the American Journal of Public Health in 2016 found that individuals who increased the number of servings of fruits and vegetables that they ate reported that they were happier and more satisfied with their life than those whose diets remained the same.
Another study of 422 young adults from New Zealand and the United States showed higher levels of mental health and well-being for those who ate more fresh fruits and vegetables. Interestingly, the same benefits did not accrue to those who ate canned fruits and vegetables. “We think this is due to the higher nutrient content of raw fruits and vegetables, particularly B vitamins and vitamin C, which are vulnerable to heat degradation,” said Tamlin Conner, a study author and senior lecturer at the University of Ota.
One of the first randomized controlled trials to test whether dietary change may be effective in helping to treat depression was published in 2017. In the study, led by Felice Jacka, a psychiatric epidemiologist in Australia, participants who were coached to follow a Mediterranean diet for 12 weeks reported improvements in mood and lower anxiety levels. Those who received general coaching showed no such benefits.
A Mediterranean diet, rich in whole grains, legumes and seafood as well as nutrient-dense leafy vegetables that are high in the fiber, promotes a diverse population of helpful bacteria in the gut. Research suggests that a healthy gut microbiome may be important in the processing of neurotransmitters like serotonin that regulate mood.
“Our imaging studies show that the brains of people who follow a Mediterranean-style diet typically look younger, have larger volumes and are more metabolically active than people who eat a more typical Western diet,” said Dr. Lisa Mosconi, the director of the Women’s Brain Initiative at the Weill Cornell Medical Center in New York. Such brain benefits may be protective against the onset of dementia, she said.
Dr. Mosconi noted that “there is no one diet that fits all” but advises patients to cut out processed foods, minimize meat and dairy and eat more whole foods like fatty fish, vegetables and whole grains and legumes to cut the risk of developing degenerative brain diseases associated with aging.
She and Dr. Ramsey both recommend “eating the rainbow,” that is, consuming a wide array of colorful fruits and vegetables like peppers, blueberries, sweet potatoes, kale and tomatoes. Such foods are high in phytonutrients that may help to reduce harmful inflammation throughout the body, including the brain, and promote the growth of new brain cells throughout our adult years, they say.
Dr. Emily Deans, a clinical instructor in psychiatry at Harvard Medical School, cautions that a plant-only diet may carry some risks. Some large observational studies suggest, for example, that strict vegetarians and vegans may have somewhat higher rates of depression and eating disorders than those who eat a more varied diet. Those on a meat-free diet may also need to take supplements to provide missing nutrients. “Some of the key nutrients for the brain, like long chain omega 3 fatty acids and vitamin B12, are simply not found in vegetable only diets,” says Dr. Deans.
Samantha Elkrief, the food coach who assists Dr. Ramsey, adds that it’s not just what we eat but the attitudes that we bring to our food that contribute to mental well-being. “I want to help people find the foods that give them joy, that make them feel good,” she says. “It’s about slowing down and becoming more mindful, noticing your body, noticing how you feel when you eat certain foods.”


The post Can What We Eat Affect How We Feel? appeared first on Reach Out Recovery.
How A Scottish Woman Endured Burns, Broken Bones, Childbirth And Surgeries Without Ever Feeling Pain
A newly discovered genetic mutation caused a Scottish woman to endure cuts, burns, broken bones, childbirth and surgery without feeling any pain, according to a case study published in the British Journal of Anaesthesia.
About five years ago, Joanne Cameron, now 71, had what should have been a painful hand surgery at Scotland’s Raigmore Hospital, says Dr. Devjit Srivastava, a consultant in anesthesia and pain medicine at the hospital.
“She mentioned that she does not feel pain and she did not need any anesthesia, which was not a usual day in the office for me,” Srivastava tells TIME. “I disregarded her, actually. I couldn’t believe her.”
Srivastava gave Cameron anesthesia as usual, but decided to check in with her after the operation. When he did, he found that she reported no pain, and didn’t take any painkillers beyond an over-the-counter drug recommended by her doctors.
In talking to her further, Srivastava learned that Cameron also hadn’t experienced pain from a previous arthritis diagnosis or a hip replacement surgery. When giving birth to her two children, she told Srivastava, she experienced only “a bit of uncomfortableness.” In some cases, she didn’t even notice injuries — she reported “often smelling her burning flesh before noticing any [burn] injury,” according to the case study, and remembered breaking her arm as a child and not noticing until her mother caught sight of it.
Perplexed, “I felt it was a responsibility that I shouldn’t let her go without investigating,” Srivastava says.
He referred her to pain genetics experts at the University College London and the University of Oxford, who completed genetic sequencing on her as well as her mother and two children, according to the case study. They found that Cameron had a handful of genetic mutations, including one on the chromosome that codes for an enzyme called FAAH. Cameron’s FAAH gene was making a modified type of the enzyme, which had been shown in previous research to lessen pain perception.
From there, doctors uncovered another genetic mutation near the FAAH gene. And through blood tests, they confirmed that her genetic defect was “translating into a biochemical defect which increases a brain chemical, due to which she does not feel pain, she is forgetful and she is incredibly happy,” Srivastava explains.
The discovery highlights the delicate role of pain in the body, Srivastava adds.
Some pain is a good thing, as it serves as a warning sign when something is amiss, he says. (Even without such warning signs, Cameron is today in “absolutely good health,” Srivastava says.) But at the same time, millions of people — including more than 50 million in the U.S. alone — suffer from chronic pain, which can significantly hamper quality of life, lead to reliance on addictive painkillers such as opioids and even change the way the brain works.
Cameron’s case may someday lead to a breakthrough for these people, Srivastava says. He hopes that, if researchers can identify the molecular pathways behind Cameron’s pain tolerance, they can someday use that information to develop new pain relief therapies — ideally that come with fewer risks than opioids.
That reality is a long way off — research is only at the conceptual stages for now, Srivastava says — but he says it’s not impossible to imagine.
“When pain lingers on for months or years, it serves no useful purpose,” he says. “We are trying to [target] those millions of patients and provide help to them.”


The post How A Scottish Woman Endured Burns, Broken Bones, Childbirth And Surgeries Without Ever Feeling Pain appeared first on Reach Out Recovery.
March 28, 2019
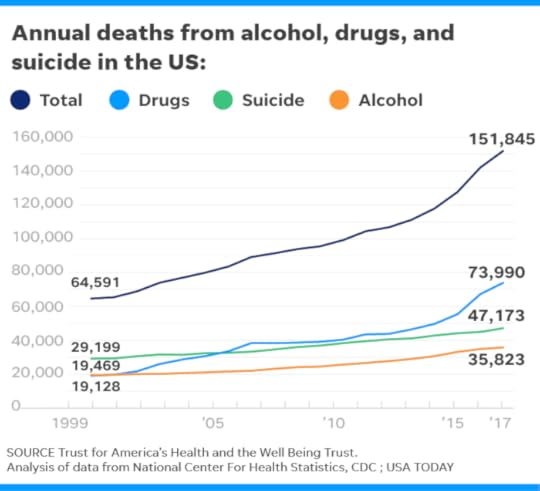
Highest Drug/Alcohol Deaths In History
From USA Today A study shows that more Americans are dying from drug and alcohol abuse and suicides than at any point in roughly the past 20 years. Veuer’s Justin Kircher has more.
The number of deaths from alcohol, drugs and suicide in 2017 hit the highest level since federal data collection started in 1999, according to an analysis of Centers for Disease Control and Prevention data by two public health nonprofits.
The national rate for deaths from alcohol, drugs and suicide rose from 43.9 to 46.6 deaths per 100,000 people in 2017, a 6 percent increase, the Trust for America’s Health and the Well Being Trust reported Tuesday. That was a slower increase than in the previous two years, but it was greater than the 4 percent average annual increase since 1999.
Deaths from suicides rose from 13.9 to 14.5 deaths per 100,000, a 4 percent increase. That was double the average annual pace over the previous decade.
Suicide by suffocation increased 42 percent from 2008 to 2017. Suicide by firearm increased 22 percent in that time.
Psychologist Benjamin Miller, chief strategy officer of the Well Being Trust, says broader efforts are needed to address the underlying causes of alcohol and drug use and suicide.
“It’s almost a joke how simple we’re trying to make these issues,” he says. “We’re not changing direction, and it’s getting worse.”
The health and well-being trusts propose approaches including:
► More funding and support for programs that reduce risk factors and promote resilience in children, families and communities. Trauma and adverse childhood experiences such as incarcerated parents or exposure to domestic violence increase the risk of drug and alcohol abuse and suicide.
► Policies that limit people’s access to the means of suicide, such as the safe storage of medications and firearms, and responsible opioid prescribing practices.
► More resources for programs that reduce the risk of addiction and overdose, especially in areas and among people most affected, and equal access to such services.

Psychologist Ben Miller is chief strategy officer at the Well Being Trust. (Photo: Well Being Trust)
While overdose antidotes and treatment for opioid use disorder are needed, Miller says, “it’s not going to fix” the underlying problems that lead people to end their lives, whether or not it’s intentional.
In most states, deaths from alcohol, drugs and suicides increased in 2017. In five – Massachusetts, Oklahoma, Rhode Island, Utah and Wyoming – those deaths fell.
Deaths from synthetic opioids, including the narcotic pain reliever fentanyl, rose 45 percent. Such deaths have increased tenfold in the past five years.
Loribeth Bowman Stein says the lack of social connection fuels hopelessness: “We don’t really see each other anymore.”
“We don’t share our hopes and joys in the same way, and we aren’t as available to one another, physically and emotionally, as we need to be,” says Stein, of Milford, Connecticut. “The world got smaller, but lonelier.”

LoriBeth Bowman Stein of Milford, Conn. says people aren’t connected as much as they used to be. (Photo: Family photo)
Miller agrees. When people feel a “lack of belonging,” he says, “they seek meaning in other places.”
That can lead them to withdraw into addiction. The new report emphasizes what should be done differently.
Kimberly McDonald is a licensed clinical social worker who has worked in a hospital, for county government and in private practice. She lost her father to suicide in 2010.
“We are a society that criticizes and lacks compassion, integrity, and empathy,” the Richmond, Wisconsin, woman says. “I work daily with individuals who each have their own demons.”
McDonald’s father took his own life after diagnoses of Lewy body dementia and Parkinson’s disease.
“He knew the trajectory of where the disease would take him,” she says.
John Auerbach, the former Massachusetts state health secretary who heads Trust for America’s Health, says the country needs to better understand and address what drives “these devastating deaths of despair.”
If you are interested in connecting with people online who have overcome or are struggling with issues mentioned in this story, join USA TODAY’s “I Survived It” Facebook support group.
Booze isn’t just featured in commercials, it’s pretty much gotten to the point where it’s featured in your favorite TV show or movie. Here’s how alcohol advertising affects minors. USA TODAY
The post Highest Drug/Alcohol Deaths In History appeared first on Reach Out Recovery.
What Is Unresolved Grief
Unresolved grief is more common that we think. Grief for someone we lost is only one cause of lingering sadness. I grieved for my mother for 30 years. I looked for her on the street, sobbed when I saw other mothers and daughters having fun. Even shopping for clothes made me tearful because it was something we used to do together. My decades long reaction was beyond typical sadness, I had unresolved grief.
My First Experience In Grieving
My mom died of cancer a few years after I married, and three weeks before my son was born. A few months later my husband quit his job and didn’t find another for nine months. All four events, marriage, death of a loved one, birth of a baby, and loss of a job are high stress. My coping skills always kick in when times get tough, but I didn’t stop active suffering about my mom regardless of the other changes in my life.
What Causes Unresolved Grief
People do get stuck in their losses and it isn’t always a death. It can be a change of circumstance, or even marriage itself. It’s important to recognize what you’re feeling so you can take steps to lift the burden.
For me and the loss of my mom one problem was I did not have the opportunity of a proper “goodbye.” Even though I had sat with my mom throughout her illness and was pregnant for nine months of it, she never gave me her blessing or wished me well with my baby. She was not able to say goodbye. Doubly painful was the fact that my children grew up without a grandmother. This was cause for my grieving on their behalf, too. Grief is often about much more than just the passing because of the many extra feelings associated with it. This is also true for job loss, change of circumstances, moving, etc. There are some 40 life experiences that can cause grief.
Although sorrow is a normal reaction, unresolved grief has a more traumatic impact. As a result it can have a negative effect on one’s life. You may be asking yourself, “How do I know if I have unresolved grief?”
Signs of Unresolved Grief
Although many of sufferers try to pretend that they are “over it” for various reasons, the following are some of the tell-tale signs that someone is grieving:
Preoccupation with sad or painful memories
Refusal to talk about the loss at all
Increase in alcohol, food, drug, or cigarette usage.Antisocial behavior
Overindulge in hobbies, work, or exercise activities
Lack of energy
Difficulty concentrating
Isolation from friends and family
How Children Express Unresolved Grief
Develop behavior problems
Have Fear of being alone
Become more aggressive
Perform worse at school
How Teens Express Unresolved Grief
Using drugs
Drinking Alcohol
Stealing
Have unprotected sex
Become accident prone
Withdraw from friends
Have difficulty completing schoolwork
Young children may show unresolved grief by developing behavior problems or expressing fears about being alone, especially at night.
If left untreated, the long term effects can be devastating to future relationships and every day activities, such as work and what used to be enjoyable hobbies. Here are some things that can be done to help resolve the unsettled feelings.
Validate Feelings
Everyone has a right to sad feelings. Even though others may not understand your feelings or fail to empathize with you, it is important for you to empathize with yourself. It is also important for you to empathize with children and teens who are suffering. Give everyone permission to process, naturally, the loss they have experienced.
Reach Out
No matter how small it may be, build a support network. Whether it is that one special friend who can listen without judgement, or an online group on social media. It’s important to have someone to turn to if you need a shoulder to cry on or a new outlook in order to get you through a rough moment.
Some Causes Of Unresolved Grief
Unresolved grief can be caused by pretty much anything big or small. If something, someone, or an event was important to you. You may not even think something that happened long ago may continue to nag at you now. There are some 40 life events that can cause unresolved grief. Here are some:
Death of a spouse
Divorce
Marital separation
Imprisonment
Death of a close family member
Personal injury or illness
Marriage
Dismissal from work
Marital reconciliation
Retirement
Change in health of family member
Pregnancy
Sexual difficulties
Gain a new family member
Business readjustment
Change in financial state
Death of a close friend
Change to different line of work
Change in frequency of arguments
Major mortgage
Foreclosure of mortgage or loan
Change in responsibilities at work
Child leaving home
Trouble with in-laws
Outstanding personal achievement
Spouse starts or stops work
Begin or end school
Change in living conditions
Revision of personal habits
Trouble with boss
New working hours or conditions
Change in residence
New schools
Change in recreation
Beginning or ending church activities
Change in social activities
Minor mortgage or loan
Change in sleeping habits
Change in number of family reunions
Starting a new eating habit
Vacation>
Christmas
Minor violation of law
Loss of Trust, Approval, Safety and Control of one’s body
There is no definite point in time or a list of symptoms that define unresolved grief. Unresolved grief lasts longer than usual for a person’s social circle or cultural background. It may also be used to describe grief that does not go away or interferes with the person’s ability to take care of daily responsibilities. People with unresolved grief who do not seek treatment are more likely to develop other mental health and physical problems.
The post What Is Unresolved Grief appeared first on Reach Out Recovery.
Does Smoking Marijuana Impact Male Fertility
From Medical News Today by Maria Cohut With the increased legalization of cannabis, especially medical marijuana, researchers are interested in finding out more about its effects on health. One area that is currently under exploration is that of marijuana’s effect on fertility.

Researchers are investigating the potential effects of smoking marijuana on male fertility.
As recent research shows, men in Western countries are facing a fertility crisis. Sperm count in males of reproductive age more than halvedbetween 1973 and 2011.
According to the Eunice Kennedy Shriver National Institute of Child Health and Human Development, approximately 9 percent of men in the United States have faced infertility.
For this reason, researchers have been looking at how different modifiable factors, such as lifestyle choices, might affect male fertility.
In a new study, a team of investigators from the Harvard T. H. Chan School of Public Health in Boston, MA, has focused on the effects that smoking marijuana has on markers of male fertility.
The researchers’ findings, which they report in a study paper that features in the journal Human Reproduction, ran counter to the hypothesis that they established at the beginning of the study.
“[The] unexpected findings highlight how little we know about the reproductive health effects of marijuana and, in fact, of the health effects of marijuana in general,” notes study author Jorge Chavarro.
“Our results need to be interpreted with caution, and they highlight the need to further study the health effects of marijuana use,” he emphasizes.
Higher sperm concentration among users
To begin with, the research team speculated that men who either smoked or had smoked marijuana would have poor sperm quality. However, that is not the conclusion that this study reached.
In their research, the investigators recruited 662 men who attended the Fertility Clinic at Massachusetts General Hospital in Boston between 2000 and 2017. The average participant was 36 years old, white, and had a college degree.
To assess sperm quality, the researchers collected and analyzed 1,143 semen samples from the study participants. They also took blood samples from 317 of the men. The team used the blood samples to test for reproductive hormones.
Additionally, the researchers asked the men to fill in questionnaires asking them about their use of marijuana, including whether they had ever smoked more than two joints and whether they still used marijuana.Does a nut-rich diet lead to better sperm quality?Could eating more nuts help improve male fertility?READ NOW
The team found that 365 (or 55 percent) of the participants had smoked marijuana at some point in their lives. Of these people, 44 percent no longer used this substance, while 11 percent self-identified as current smokers.
In looking at the semen samples, the researchers noticed that men who had used marijuana had higher average sperm concentrations than nonsmokers.
More specifically, marijuana users had an average sperm concentration of 62.7 million sperm per milliliter of ejaculate, whereas their peers who had never smoked marijuana had 45.4 million sperm per milliliter of ejaculate.
The investigators also observed that among marijuana smokers, only 5 percent had sperm concentrations below 15 million sperm per milliliter of ejaculate — the threshold for “normal” sperm concentration levels — while 12 percent of never-smokers had sperm concentrations below this level.
Findings consistent with interpretations
Another finding reported in the study indicates that marijuana smokers who used the substance more frequently also tended to have higher blood testosterone levels.
Still, the researchers warn that their results may not apply to the general male population since the study focused specifically on men seeking treatment at a fertility clinic.
Even though they were unexpected, the authors suggest that their findings do make logical sense in the context of marijuana’s effect on the human endocannabinoid system, which responds to the active compounds present in this substance.
“Our findings were contrary to what we initially hypothesized. However, they are consistent with two different interpretations, the first being that low levels of marijuana use could benefit sperm production because of its effect on the endocannabinoid system, which is known to play a role in fertility, but those benefits are lost with higher levels of marijuana consumption.”
Lead author Feiby Nassan
“An equally plausible interpretation is that our findings could reflect the fact that men with higher testosterone levels are more likely to engage in risk-seeking behaviors, including smoking marijuana,” Nassan adds.


The post Does Smoking Marijuana Impact Male Fertility appeared first on Reach Out Recovery.



