Leslie Glass's Blog, page 252
July 29, 2019
6 Steps To Getting What You Want
Getting what you want requires more than wishing, hoping, and praying. People say that recovery operates by some universal law. Just when you become ready for that something you desperately need, it shows up. Readiness and being able to redefine what you want are an important components to moving forward in recovery. Here are six steps to achieving a better you and a better future.
Honesty is the first Step in getting what you want
Be brutally honest with yourself. Start right where you are. Are you an angry and judgmental person and want to change that? Start by admitting that you are angry. You can’t fix what you are in denial about. It is the starting gate and not a point of shame.
Journal (Write It Down)
Get it on paper. Describe what you are feeling and the situation that is triggering your responses. Acknowledge what you were thinking at the time. I was angry, sad, mad glad, etc. Make journaling convenient so you will be consistent. You will find journaling to be quite cathartic and revealing. It might be your best mentor.
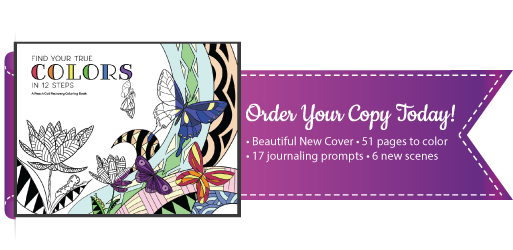
Get 100 Tips For Growing Up In Recovery To Be Your Best Self
Think Reflectively
Are you always reacting to one drama to another? Are you creating drama by overreacting to every little thing? Over reacting to a perceived emergency is like having our brains hijacked. Do it enough and it becomes a lifestyle of overdramatizing and using our D.O.C.’s to soothe our psyche. When you feel yourself spinning into a frenzy, stop. Use your energy to step and really think about what’s happening and how you want to act. You can become more intentional with your thoughts and behavior. This is what makes us all powerful as humans. We have the authority to observe, think, and respond with our best foot forward.
Be In Community (Opposite of Isolating)
We heal in communities. Find a sponsor, a healing group, a recovery coach, something or everything. Show up and listen. Learn who you can trust with what you are dealing with. Show humility and ask for help. Choose consistency and accountability. We have already proven we can’t do it alone nor were we meant to be isolated. We aren’t designed to be self-sufficient islands so be intentional about building a positive and affirming group that you are active in.
Rehearse Affirmations
We will always return to and act out of our dominant beliefs. We don’t have to live with what others have handed to us. We have the ability to reshape heart held principles and rebuild our core identity. Create a list of positive affirmations and rehearse them daily. This is a gift we can speak over our lives. My good friend calls this his “pre-flight” list. Every pilot has a check list they go through before lift-off. This is how we can start our days. Rehearsing our intrinsic value as human beings.
Need A Recovery Activity Book For Support and Fun? Get It Now
Take Action
It is in taking that first step that the power to accomplish, create, sustain will meet us. This is the same principle as when you are ready what you need will show up. But you have to take the action. Accomplishment of goals does not meet us while we sit pondering our next move feeling apprehensive. Accept the risk and take the steps to become your very best.
The post 6 Steps To Getting What You Want appeared first on Reach Out Recovery.
Not Prepared For Son’s Life After Overdose
Life after overdose is trauma beyond imagining for loved ones. My son Josh lay there in the trauma room comatose and hooked up to a ventilator and everything else that could be. As a physician, I was used to taking care of others in that situation; now the shoe was on the other foot. Straddling being a mother and a physician was difficult at best. At worst I was annoying to the staff as my mother brain and doctor brain dealt with the situation.
After overdose the damage was major
Josh’s overdose that landed him here had stroked out his entire brain except the brainstem. He had a heart attack, was in kidney failure, and his enzymes that should have been single digit were nearly 60,000. He was in Rhabdomyolysis. He had a huge open wound on the back of his scalp approximately 8 inches in diameter.
A lifetime of drug use ended with another overdose
The vigil I had been dreading for nearly 20 years began. The doctors told me he would die. The neurologist told me that the addiction area of his brain had been affected by the stroke. I remember thinking “Great. If he doesn’t die he’ll be in a PVS (persistent vegetative state) without addiction problems.” After seven days I was able to help the hospital understand that even though Josh was young, he would not want to live in a coma. We decided to take the ventilator out. The neurologist and I were standing on opposite sides of Josh’s bed talking about the fact that he would not live through this. I looked over at Josh and his lower lip was quivering (around the ventilator tubing) the way it had when he was young and in trouble. I wondered if he could hear us.
Josh started breathing on his own
Three days after we took the ventilator out, Josh had not died. He opened his eyes on day 10 after being admitted. I could tell he knew who I was. I told him then, “You flunked dying and now you must learn why God has kept you alive.” He smiled.
The overdose did not end with death
Josh walked out of the nursing home four months later on a cane. He had a traumatic brain injury that would develop early onset dementia. He had lost his hearing (eventually he obtained hearing aids) and could no longer work as a chef, but he was alive. Was that a good thing?
I was not prepared for his life after overdose
So many parents are losing their children this way. Let me say that the aftermath has not been easy for me. While I am happy that my son is alive, I couldn’t help being angry with him most of the time, and I couldn’t seem to get over it. Josh still has addiction problems, and now problems with mood swings due to the brain injury. I felt I should have been able to deal with these issues, especially when he pushed my buttons. Surprisingly, he remembered where they were! I now felt I couldn’t deal with the smallest of issues with him. It was as if I was completely out of fuel. I had no reserve left.
The Answer to life after overdose came to me
Finally, one day while meditating, the answer came to me. I had been prepared to lose my son, but I didn’t. I wasn’t prepared for life like this. I had no emotional tools to cope with his life after a catastrophic overdose. It sounds strange but it was indeed an epiphany. At least now I knew why I was angry all the time. Angry at him and also at myself.
A counselor helped me understand
I am constantly working on my feelings about Josh’s living when he was supposed to die. And the fact that he still has problems with addiction. These don’t have to be my issues. They are his. I can’t make him well again.
A parent’s secret feeling revealed
It’s wonderful that my son is still on this side of the curtain, and I love him more than life. I understand this. I also understand what a good friend told me: “You’re still watching him die every day. At least my son went in one day.” While that is all true, in my Mother’s heart there always resides a spark of hope.
Watching loved ones suffer is one of the most cruel aspects of addiction. Recovery is also available for the families of. Find family support groups and therapists near you at Recovery Guidance.
The post Not Prepared For Son’s Life After Overdose appeared first on Reach Out Recovery.
10 Things To Not Say To A Depressed Friend –
Remember the game telephone we played as kids? One child whispered a secret to the next, then that child whispered what he or she heard to the next. By the end of the game, the original secret was hilariously distorted. Often, this same thing happens when we try to cheer up a loved one struggling with depression. The message of help and hope is distorted into shame and condemnation.
We all want to be helpful to our family, friends, coworkers, and acquaintances, but sometimes we don’t know what to say. We either:
Say and do helpful things
Ignore the person, the problem, or both
Try to help but end up saying and doing hurtful things
10 Things Not To Say To A Depressed Friend
Remember that while you want to help, there are things to do and say that can be beneficial to one who is depressed, but the following statements are usually disheartening. Here are the most commonly offered good intentions:
“It can’t be that bad.”
“You’re just having a bad day.”
“Stop feeling sorry for yourself.”
“Pull yourself up by your bootstraps.” OR “Snap out of it.” OR “Get over it.”
“You don’t look (or seem) depressed.”
“Think about all the people that are worse off than you…” OR “You think you have problems, let me tell you about….”
“Why are seeing a psychiatrist (or social worker, counselor, psychologist)? They’re a bunch of quacks.
“Why are you taking meds? They can’t be good for you. And the BIG Book (AA) says you shouldn’t take drugs.
“What doesn’t kill you will make you stronger.”
“Have you tried…”
What The Depressed Friend Is Likely To Hear
Depression often comes with feelings of shame, overwhelm, exhaustion, and worry. When those feelings are present, they transcribe the well-intended message of hope and generate these types of responses:
Here is my list of everything that is going wrong in my life…
Well, perhaps this will kill me.
I’d love to look at the bright side, but all I can think about is sleeping, or worse yet dying…
Yep, it would be great if I could get myself out of bed.
Of course I’ve never thought about this. (Add sarcasm)
How could you be so cold and compassionless?
I’m so depressed that I really don’t care.
All of the above offered good intentions either minimize the person’s pain or try to solve the person’s problem. They border on being controlling and unkind. Comparative pain almost never cheers someone up, and doctors have yet to find any combination of words that can magically cure depression.
To help a depressed friend or relative, instead try:
Listening without judging or giving advice
Validating your friend’s feelings
Letting your friend find his or her own solutions
Unless your depressed friend specifically asks for your opinion, keep your opinions to yourself. (This is so important that we said it twice.)
For more helpful ideas on how to support a depressed friend, read our article, 10 Things To Say To Someone Who’s Depressed.
The post 10 Things To Not Say To A Depressed Friend – appeared first on Reach Out Recovery.
Alcohol: It Really Is Everywhere
From Psychology Today:
Could there be more alcohol commercials on TV?
Wow, there is a lot of alcohol being advertised on TV these days. I never really thought about this until the last few years, when addiction treatment came under my direction at the AMITA Health Foglia Family Foundation Residential Treatment Center.
In addition to anxiety and stress, I now help to manage addiction cases, so to see all of the commercials on TV about all of the new ways that we can get alcohol into our system gives me pause.
I get the whole need to advertise, but I also feel for those who see these commercials and get triggered with a craving or an urge to drink again. It is so difficult for the patients that I have treated, who have put so much effort into getting sober, to just be pelted constantly by taunts to drink all over again.
If you have a friend or loved one who has been a substance user, I wonder if you would consider doing something to honor their journey to sobriety. Would you consider hosting a sober party at your home? Would you be willing to join them on an outing to a sporting event or concert and be a model for them that those events can be enjoyable even without drinking? And, would you be willing to be a person that they can check in with now and then if they are having a tough day?
This summer, when it is tempting to be out on the deck with a summer cocktail, would you be willing to have a person who is trying to be sober over to your deck and serving some lovely iced teas instead?
It would mean a lot to your friends or family who are trying to remain sober and really show them that there are people out there who support them on their journey.
Have a safe summer and, if needed, a sober one as well.


The post Alcohol: It Really Is Everywhere appeared first on Reach Out Recovery.
July 28, 2019
The Toxic Past: A Survival Guide
The toxic past returns to haunt us all. I started crying the other day while I was hiking. It just happened, and before I knew it, tears were rolling down my face. I finally stopped and took off my glasses to wipe my face just as this nice-looking guy passed me. Both of us with our dogs, dressed all sporty, in shape, and on top of a mountain on a brilliant morning in Southern California. But there I stood, with the pain in my heart written all over me. He looked at me with concern but also curiosity; and I felt caught, exposed, and embarrassed, so I knelt down next to my dog and pretended to do something. He passed, and I stood up and pulled myself together. Sort of.
“What happened to her?” he must have thought. “Did someone die? Is she sick? What could have caused her to crumble like that in such a beautiful setting on such a beautiful day?”
How could I have possibly explained that it wasn’t anything, in particular, that day that made my soul ache? It was just my toxic past.
It was the decades of stuff that occasionally surfaces, particularly at this time of year. I never talk about the specifics of my story anymore because it doesn’t matter and continuing to retell those stories only gives them power when they don’t have a hold over me anymore. But, I did have a therapist at one particularly dark time in my life who told me, “There will be some days you will cry for the rest of your life. That’s just how it’s going to be, and you’ll have to learn how to take care of yourself when those moments come up.”
Need 100 Tips For Growing Up? Get It Now!
Because I’m a survivor of trauma, addiction, deaths of beloved friends and boyfriends, and sometimes it still hurts.
Some days there are people I miss and relationships I mourn. Rage and sadness spills out, but I don’t need to use over it anymore. That’s the good news. It passes pretty quickly. That’s the other good news, but I do need an action plan.
In moments of despair I do these five things to stay centered:
Talk about my feelings with someone. Anyone I feel safe with will do, but I don’t keep the feeling locked up inside.
I keep active. There’s a reason I’m on top of that mountain, or in boot camp, as many times a week as my schedule and body permit.
Eat well. My brain needs nutrition to function well. This is not a joke. I used to get so annoyed when people would bitch at me to eat regularly and well. Now I know I feel awful when I don’t. Anxious, hangry, stressed are not good for me.
Take a break. If I feel overwhelmed I turn everything off for an hour, a day, a week, as long I can/need.
Care for others, animals, be of service, whatever I can do to get out of myself and my head for an hour a day.
Get The Recovery Activity Book For Serenity Today!
For me, the recovery plan has to account for the fact that there will be bad days.
It’s not enough to have smart feet that take me to the right places. I need to know how to mend my heart and nourish my soul at a moment’s notice. These are just some of the tools I use. Find the ones that work for you—nature, animals, cooking, meditation—all of these things make me happy. Start by using the ones above and making a list of the things you like to do. With practice, it becomes second nature 
July 27, 2019
What’s More Addicting Than Chocolate? You Might Be Surprised
From Psychology Today:
Did you ever wonder which foods are most addicting, and what psychological traits are associated with people who say they can’t stop eating them? For me, this curiosity began 20 years ago when I conducted my own informal survey with thousands of visitors on my website. A few intriguing trends emerged:
People who struggled with chocolate tended to be more lonely, brokenhearted, or depressed. People who struggled with crunchy, salty snacks tended to be more stressed at work.And people who struggled with soft, starchy things like bread and bagels tended to be more stressed at home.
That was all very intriguing, but the survey had several serious methodological flaws and the data-set was no longer available to review. So, more recently, I commissioned a professional survey with 500 people. We recruited a stratified random sample of the population, and I had the data weighted to be demographically representative of the United States as a whole. We asked what foods people had trouble stopping once they started, how satisfied they were with their life overall, and how close they were to their ideal weight.
The order of addiction in the results really surprised me. From the way people talk about chocolate, you’d think it would’ve come up as the most addicting food treat of all. After all “just hand over the chocolate and nobody gets hurt” has to have come from somewhere, right? But chocolate was far from the most addictive food reported:
Salty snacks, chips, pretzels, popcorn, etc. turned out to be almost twice as addictive as chocolate. 32.9% of respondents indicated they were out of control with these kinds of snacks as compared to only 18.6% who struggled with chocolate. Life satisfaction also played a strong role in the salty snack category. You might expect people more satisfied with their lives to be less likely to struggle, but the opposite proved true. Those at least somewhat satisfied were 50%+ more likely to say they couldn’t stop eating salty snacks. Demographically, those aged 65+ had more trouble with salty snacks than the rest of the population (43.6% vs. 32.9%) Non-chocolate sugary treats (sweets, candy, cake, cookies, etc.) were also reported to be more addictive than chocolate at 24.3%. And intriguingly, those who said they were very satisfied with life were 33% less likely to struggle with sweets than everyone else. Does life satisfaction move us away from sweets and towards salty, crunchy snacks? Or is there something about indulging in the salty-crunchy stuff that makes us feel more satisfied? We can only hypothesize. Large food manufacturers certainly spend a fortune attempting to maximize satisfaction from salty snacks, perhaps this effect is part of what we’re seeing. There was also a trend towards women having just slightly more difficulty with sweets than men (28.5% vs. 24.3%).Flour (bread, pasta, etc) came in at 14.2%. There was no significant impact of life satisfaction, weight, gender, or age on difficulty controlling oneself with flour. In last place were fatty snacks (nuts, cheese, and fried food) at only 10.2%. It’s noteworthy that people who were forty or more pounds overweight were more than twice as likely to have trouble with fatty snacks vs. those closer to their ideal weight (14.1% vs. 6.2%). Notwithstanding this difference, fatty snacks were still not a primary concern for most people
How can we leverage this data? Take note of the pattern, and become both more aware of and more careful with the more addictive food categories. Of course, the most addictive food in the world for you personally is whichever one you can’t stop eating! Still, the pattern is clear, and in my experience, more awareness, sensitivity, and planning can lead to substantially more control.
When people tell me they can’t control themselves with certain foods, I ask them what role they’d like that food to play in their lives. Sometimes they say something very specific like “I wish I could eat it just once per week in a very specific amount.” Other times they say “I think I need to quit it entirely. It’s the kind of thing I can’t give an inch without giving a mile!”
If you think it’s wiser to have very specific amounts, then the next step is to articulate the conditions and amounts very cogently and clearly. For example “I will allow myself one 8 oz. bag of _____ (insert favorite salty snack here) on Saturday or Sunday but not both.” Or “I will allow myself one dessert when I’m out at a restaurant, but no more than twice per calendar week.” On the other hand, if you think you need to quit, then quit! For some people, none is a lot easier than some.
For more a practical, step by step method to organize your mind to either quit or control any of the foods in the categories above, please see “How to Stop Binge Eating in Three Unusual Steps.”


The post What’s More Addicting Than Chocolate? You Might Be Surprised appeared first on Reach Out Recovery.
What To Know About Waking Up With Anxiety
From Medical News Today:
There are many possible causes of a person waking up with anxiety, including stress from work, school, or relationships issues. Although it is common to wake up feeling anxious from time to time, if a person experiences it frequently, they may have generalized anxiety disorder.
Generalized anxiety disorder (GAD) is a condition that causes uncontrollable and excessive worrying that affects a person’s everyday life. GAD may cause a person to wake up due to anxiety or have difficulty falling or staying asleep.
Common symptoms of GAD include:
nervousness or worryfeeling restless, on edge, or wound upfinding it difficult to concentratefatiguefrequent panic attacksirritability
GAD and other anxiety disorders can develop over time. In most cases, several ongoing circumstances lead to a person developing a form of anxiety. People with a history or family history of anxiety may be more at risk than others, but it is possible for anyone to develop anxiety.
Possible triggers for morning anxiety include the following:
1. Stress at work, home, or school
Stress is the body’s natural response to unpleasant stimuli. The body releases cortisol, which people often refer to as the stress hormone, when a person feels worried or stressed.
According to one study, the body releases an abundance of cortisol in the morning when a person is under a lot of stress. When cortisol wakes a person, medical professionals refer to this as the cortisol awakening response (CAR).
CAR is the most likely cause of people with or without GAD waking up feeling anxious. For most people, the feeling should pass once the stressor is gone. If it does not pass, a person may wish to consider speaking to a healthcare professional about their continued anxiety. Doing this may also be beneficial for people who regularly feel anxious but cannot identify a cause.
2. Substance or alcohol use
People already dealing with anxiety should avoid alcohol and recreational drug use.
Although substance use and alcohol use do not have direct links to anxiety, they can make symptoms of anxiety worse.
As a result, alcohol or other substances can affect how a person sleeps or how they feel when they wake up.
3. Relationship troubles
There is evidence that how happy a person is in their relationship can directly affect aspects of their health. These include illness recovery and sleep patterns.
In a small-scale study, researchers asked 29 couples to record their relationship experiences during the day and how they slept at night. The results indicated that when females reported having positive interactions with their partner during the day, both they and their partner slept better than when the interactions were negative.
In a similar way, relationship status may cause a person to wake up feeling anxious.
4. Life events
GAD and other anxiety disorders may develop due to ongoing or acute stressful life events. Some life events that might trigger anxiety on waking include:
changes in living arrangements, for example, moving to a new area or someone else moving outchanges in employment, such as switching jobs or losing a jobexperiencing physical, mental, or sexual abusethe separation from or death of a loved oneemotional shock after a traumatic event
5. Financial issues
Finances affect nearly every adult, and many people worry about them. A person may have concerns about how they will pay for groceries, cover the mortgage or rent, or travel to work.
However, for some, thinking and worrying about finances can become an overwhelming problem.
When a person worries about finances excessively, they can develop anxiety that may affect their sleep and how they feel when they wake up in the morning.
6. Physical health issues
Chronic physical illness can contribute to a person feeling more anxious.
Although everyone will respond to health conditions differently, a person who has an ongoing medical issue may develop anxiety.
Some common health conditions that may trigger anxiety include:
diabetesheart diseasehypertensionasthmapsoriasisdepressioncancer
7. Other mental health disorders
A person living with GAD may or may not have additional mental health disorders.
If they do have another disorder, such as depression or bipolar disorder, their symptoms of anxiety may get worse.
This exacerbation can lead to a person waking up with anxiety in the morning.
Diagnosis
It will generally be a doctor, psychiatrist, or psychologist who diagnoses anxiety. A person will typically visit them to discuss persistent anxiety, a feeling of being overwhelmed, or sleeping difficulties.
The healthcare professional will usually perform a basic examination and ask questions about the person’s health — including any other mental health disorders — and what symptoms they are experiencing.
Before confirming a diagnosis of anxiety, the healthcare professional is likely to perform tests to help rule out other conditions, depending on what symptoms a person is experiencing.
Finally, they may ask the individual to complete a self-assessment. There are many different types of self-assessment, but they will use the one that they believe will best determine whether the person has an anxiety disorder or another disorder that is causing symptoms of anxiety.
Treatment and coping
If a person has GAD or another form of anxiety, their doctor may prescribe an antidepressant. In addition, they may recommend counseling, support groups, or other forms of therapy to help a person feel less anxious.
A person can also take steps at home to reduce their anxiety. These include:
doing regular exerciseavoiding alcohol and other drugsusing deep breathing techniquespracticing meditationpracticing yogaeating a healthful diettrying to avoid stressful situations
Outlook
A person who consistently wakes up feeling anxious may have GAD or another form of anxiety. Many potential triggers can cause a person to wake up feeling anxious.
If these feelings persist, a person should talk to their doctor about their anxiety symptoms and the treatment options.


The post What To Know About Waking Up With Anxiety appeared first on Reach Out Recovery.
Recovery Journey At 10 Years
I am alive and thriving today because no matter what happened, I was determined to stay the course of my recovery and do more than just survive.
It wasn’t easy. I have now been in and out of recovery for half my life. If you want to get technical, I’ve been working on recovery my entire adult life, 20 years, in fact. I entered an addiction recovery treatment program at the tender age of 21, but it didn’t stick the first time. Or the second. Or the third. I’m not a one-chip wonder, meaning I didn’t get sober once and stay clean the entire time. I did, however, make a serious decision to change my life ten years ago, and while it hasn’t been all smooth seas since, I have not strayed from that mindset. I am now 40 and healthy. I repeat, it wasn’t easy.
The recovery journey is more challenging when anxiety and trauma are involved
Recovery from addiction is a complicated process when there are no bumps in the road. When you’re dealing with more than one behavioral issue, or have trauma in your story, or a “generalized anxiety” diagnosis, or have ANY family dysfunction whatsoever, it becomes even more complex.
In my experience, I pulled back one layer of the onion only to discover there were more underneath. I had a cellar in my basement where a vault lived, and locked in there hidden away were most of my feelings. This phenomenon made my recovery a long process where sometimes I took a step forward only to take two steps back. The path to success is no straight line, especially when it comes to mental health and health and wellness.
Recovery took time but it was worth the effort
Life is bright and shiny at 40. It doesn’t look the way I expected it to, but it feels better than I ever imagined. Since we’re all still learning about what modern recovery looks like, and I’ve been writing about mine since I started, I compiled two lists that help consolidate the way I feel about all this. Here’s the first list of what I’ve learned:
1. There will be good years and bad ones on your recovery journey
That’s just life. I had this sense that if I made it five years, my life would be merry. It doesn’t work that way. Business is up and down, relationships come and go, and then as you get older, you start to lose people. However, if you’re prepared and armed with a toolbox to help, you can survive disappointments and heartbreak.
2. Getting sober is just the first step
I needed enlightenment in many areas. Learning healthy boundaries was an unexpected adventure, as was sober dating. Both caused me as much discomfort as getting sober did. Seriously, detaching from enmeshed relationships felt physically painful to me at times. Learning to use food as fuel, not comfort, and becoming financially responsible was also difficult and stressful. There were years it felt like I was training for a recovery Olympics that I wanted no part in. But, somewhere along the way, I built a well-rounded recovery lifestyle. I’m almost to the point where I have every aspect of my life organized. Almost.
3. Relationships are hard you have to think of others
I thought I’d master and get relationships sorted out by now. Insert laughter here. While I find they are far less dramatic than they once were, I’m certainly no professional in this matter. I do believe I’ve become aware and considerate of other people’s feelings. It’s no longer all about me. I don’t believe I can change anyone and I would no longer dare to try. I also now know no one can change me. There is no magic pill, and there is no magic person. It’s all hard work. However, with age, I’ve come to enjoy the work and derive great satisfaction from my improvement.
4. Self care is more than bubble baths and manicures
I recently read an article about self-care being really hard. It said self-care is not all baths and mani-pedis. The article is correct. Real self-care is financial responsibility, emotional accountability, impulse control. Basically, adulting really hard. It took a lot of practice for me to intuitively practice self-care and do things like grocery shop and plan out my whole week of meals, pay ALL my bills EVERY month, and stay gainfully employed.
Need 100 Tips For Growing Up? Get It Now!
Making sure all areas of your life are organized and well cared for is almost impossible for anyone coming out of addiction. I didn’t open my mail for years. I didn’t understand financial “stuff,” and I had the emotional capacity of a 12-year-old. Caring about those things did not come naturally to me. I had to learn how to do them years into my recovery; then I had to be disciplined in practicing them until they became habit. Trust me, it’s easier to get addicted to drugs than paying your taxes.
5. Patience and gratitude are everything
What I was writing about above – The learning self-care? Sometimes I wonder what would have happened if I stopped trying years ago because it all seemed too hard and progress was slow. Trudging from program to program, painfully learning how to manage my emotions and relationships wasn’t fun. But, it was rewarding, and it worked. I can find gratitude daily. I try to live in gratitude most of the time, and it’s a beautiful thing. I’m also patient with myself, and other people. Man, do things go better when you can just calm down and wait.
Need the Recovery Activity Book to calm down? Get it now!
The moral of the story is, while this may sound like it’s too much work, like it’ll take too long, and the pain along the way will make it impossible to get through—it wasn’t. The markers along the way become too important, the progress becomes too gratifying, and then when you realize you’re no longer in pain or anxious anymore, it’s all worth it, and you never look back.
The post Recovery Journey At 10 Years appeared first on Reach Out Recovery.
July 26, 2019
3 Truths About Anxiety That Will Help You Feel Better, Fast –
From Yoga Journal:
There are many words we might use to describe how anxiety makes us feel: uncomfortable, scared, unsettled, conflicted, anxious, antsy, nervous, attacked, unsafe, and out of control. But there is one thing that almost everyone can agree on: It feels bad. In fact, anxiety is often described to me as a deep-seated feeling that something bad is happening or is about to happen.
But anxiety may not be what you think. Which can make it really hard to heal.
Despite popular belief, anxiety is not “just fear” that can be worked through with enough therapy. And while anxiety can be linked to certain medical and psychiatric conditions, many people who struggle with anxiety have seen doctor after doctor with no relief.
Is it time to look at anxiety in a new way?
The feeling of something bad happening, even if there is no medical condition, is actually quite accurate because something bad is happening inside of you. Your body is feeling unresolved emotional energy, or baggage, that’s stuck in your system.
Anxiety comes from your body being in freak-out mode, not because of what’s happening outside of you but because of what’s stuck inside of you. While external circumstances outside of your control certainly may trigger you, that is not the actual origin of anxiety.
The feeling of anxiety arises because your body is trying so hard to keep old emotional baggage contained, and it’s just too much for anyone to hold. Anxiety manifests when stored emotional energy is trying to bubble up and out. Anxiety can be caused by any emotional baggage that you have not dealt with. I’ve seen as many people with anxiety due to suppressed anger and frustration as due to fear.
To heal anxiety, you first need to understand it. Here’s 3 truths that will help you do just that.
1. Anxiety Shows Up In Sneaky Ways
Many people have anxiety and yet have absolutely none of the typical symptoms you might imagine. Knowing how anxiety is showing up in your life can help you be more aware of how it’s affecting you.
Anxiety can manifest in ways you may not even be aware of, including:
• Negative, compulsive, or obsessive thoughts
• Needing to be in control of life and others
• Inability to relax
• Difficulty making decisions
• Being too hard on yourself
• Resistance to accepting help from others
• Feeling shaky or unstable
• Feeling sad, angry, or pretty much any other difficult emotion
• Being moody
• Inability to concentrate
• Digestive upset
• Heartburn
• Fatigue
2. Anyone Can Be Affected by Anxiety
Many believe that only weak or highly emotional people get anxiety. People who experience anxiety often feel bad about themselves, feeling delicate and unable to handle life in the way that others can. Sometimes these perceptions do actually become beliefs that perpetuate anxiety. Imagine subconsciously telling yourself all day, “I can’t handle life” or “I’m so delicate.” Nothing could be further from the truth.
Many people who experience anxiety have a constitutional makeup or personality traits that actually tend toward anxiety, such as being highly empathic, overachieving, self-sacrificing, self-critical, or always being the “strong” one or a Type-A perfectionist who prides themselves on keeping everything under control.
Anxiety sufferers are often in leadership and caretaking roles and are able to “do or conquer anything.” These are awesome personality traits. However, these people may also take on the world at the expense of themselves.
3. One Reason You Can’t “Just Get Over It”
Many anxiety sufferers are told that it’s all in their head and they should just get over it, take deep breaths, or don’t stress so much. It’s not hard to end up feeling like anxiety is your fault—that if only you had more willpower or discipline you could fix this. But, of course, it’s not nearly that easy. One of the reasons it’s impossible to take that approach is because your body is stuck in freak-out mode.
When your body is stuck in fight, flight, or freeze—or what I call freak-out mode—it’s very difficult to heal. This freak-out mode is linked to the triple warmer meridian (an energy pathway in your body’s energy system), which governs the fight, flight, or freeze response in the body. It affects the nervous system, immune system, and so much more. This freak-out response essentially creates a feeling of danger in your whole system. Anxiety is not just in your head; it’s in your entire body. In order to fully heal, you need to train your body to be relaxed and calm. In other words, you need to get your body out of freak-out mode and into healing mode.
Emotions that you felt in the past can get lodged in the body and contribute to this freak-out mode. When they become stuck, you are essentially feeling each of those emotions (which can number in the hundreds or thousands) at a low level all the time. So it’s no surprise now why you’re feeling so uncomfortable, right? In addition, the sheer force of having to “hold” all of these unexpressed emotions can create a sense of anxiety.
How to Heal Anxiety
There are many ways to deal with stuck emotions that contribute to anxiety. Thymus tapping is one of them.
The thymus gland is the master gland of the body’s immune system and is located in the upper part of the chest, behind the breastbone. It sits right over the heart. The thymus is vital to the healthy functioning of the immune system and is connected to the entire energy system and is so powerful that it can work as a stress modulator when stimulated.
A lot of people are naturally drawn to the thymus area when they are feeling anxious and don’t even realize that their body is trying to help them tend to this special gland.
How to Use Thymus Tapping: First, try to tune into the anxiety and ask yourself: “If there was an emotion under this anxiety, what would it be?” Remember, anxiety happens from suppressing emotions. That’s why identifying the true emotion your body is very helpful. Next, tap the thymus gland using your fingertips to help your body release that stuck emotion. Don’t try to push it away; allow it to be. Tapping will help usher it out of your body if you allow it to come up.
As you tap, you can say, “releasing this _______ (say the emotion)” a few times. Take some deep breaths. Repeat until you feel relief.
Now that you know these truths about anxiety, your new job is only to honor them—and trust that your healing is right around the corner.
The post 3 Truths About Anxiety That Will Help You Feel Better, Fast – appeared first on Reach Out Recovery.
What Happens To My Brain During A Blackout?
From Psychology today:
Blacking out from drinking may be more dangerous than you think.
Alcohol-induced amnesia, more commonly referred to as “blacking out” occurs when an individual indulges in too much alcohol. Blacking out is not uncommon among drinkers, especially college students. Blacking out is dangerous and can be unpredictable as individuals may commit crimes or engage in dangerous activities with no recollection the following day.
According to the director of the National Institute on Alcohol Abuse and Alcoholism (part of the National Institutes of Health), too much alcohol “shuts down the ability of the brain to consolidate memories.” When you’re past your legal limit of blood alcohol concentration (0.08) and up around 0.16, ethanol, the compound in alcohol that causes drunken symptoms, crosses the blood-brain barrier, targeting receptors in the hippocampus (where memories are kept), and memory-making signals are blocked.
The result is a gap in time or a blackout. The good news is that the damage isn’t permanent—although chronic excess drinking does irreversibly damage the brain.
Researchers have identified two types of blackouts:
En bloc, or complete blackout: when a person who had been drinking has an inability to recall entire events during the drinking period of time
Fragmentary-memory loss: when a person who had been drinking can only recall some portion of the events during the drinking period of time
It’s not always about quantity
Early studies on blackouts demonstrated that although alcohol is necessary for initiating a blackout, a large quantity of alcohol alone is not sufficient to cause a blackout. In fact, people sometimes have a blackout even when not drinking at their highest level. Factors such as how alcohol is ingested, gender, and genetic susceptibility all play a role in determining a person’s propensity for blackouts.
Although having a single blackout by itself may not be a sign of alcoholism, repeated blackouts are very often associated with having an alcohol use disorder and being at risk for chronic alcoholism.
Blacking out vs. passing out
There is a huge difference between blacking out and passing out. When a person passes out, they lose consciousness and are in a state similar to being asleep, although they are not likely to respond to stimuli like being spoken to or touched. When a person blacks out, they make decisions, hold conversations, and even continue to drink. They appear to be conscious, but they will not remember what happened. This is extremely risky, as the person may attempt to drive, have sex, or perform other risky behaviors that can lead to permanent harm and even death.
The relationship between blacking out and binge drinking
According to statistics, alcohol is the most commonly used addictive substance in the United States: 17.6 million people, or one in every 12 adults, are diagnosed with an alcohol abuse disorder and millions of more individuals engage in risky behaviors such as binge drinking that can potentially lead to alcohol abuse disorder.
Drinking among college students is no different. Binge drinking culture in colleges and universities creates an increased risk for blackouts and their many negative consequences. The media glorifies college drinking and encourages this behavior through the “party culture” of keg stands, beer bongs, and hazing in sports teams and fraternity and sorority houses. These drinking behaviors among college students have led to thousands of deaths and assaults each year.
According to the National Institute on Alcohol Abuse and Alcoholism, approximately 60% of college students consumed alcohol in the past month and two out of three of them have engaged in binge drinking in this timeframe. Additionally, each year approximately 1,800-college students die from alcohol-related unintentional deaths, 700,000 students are assaulted by another student who has been drinking and 97,000 students experience alcohol-related sexual assault.


The post What Happens To My Brain During A Blackout? appeared first on Reach Out Recovery.