Stephan Guyenet's Blog, page 3
May 24, 2017
Two things I’ve changed my mind about, part II: Phytic acid
Phytic acid is a substance found primarily in whole grains, beans, and nuts that reduces the absorption of specific minerals from food. I previously wrote that minimizing phytic acid may be an important part of a healthy diet, but new evidence—and a reexamination of old evidence—has convinced me that it probably isn’t as important as I initially thought. At least in the context of a diverse, omnivorous diet.
Phytic acid is a small molecule found in seeds like grains, beans, and nuts that binds (chelates) certain essential minerals—particularly calcium, iron, magnesium, and zinc—and reduces their absorption from food. What this means is that the nutritional value of these foods isn’t as high as you might expect if you looked them up in a nutritional database. Many traditionally-living cultures with grain-heavy diets used techniques such as soaking, grinding, and fermentation that reduce phytic acid levels and increase mineral availability (1). Let me explain why I think phytic acid is less of a nutritional concern than I used to.
The human gut adapts somewhat to phytic acid-rich food
The small intestine of certain animals produces phytase, an enzyme that breaks down phytic acid and releases the minerals it binds. Humans are among these animals. However, until recently it was thought that the production of phytase by the human small intestine is too low to have much effect (2). A 2015 study suggests that in fact, our intestine can ramp up phytase production in response to a diet rich in phytic acid, and this eventually helps us absorb more minerals from seeds like whole grains (3). [update 5/30: commenter Carl pointed out that the mechanism isn’t necessarily an increase in phytase production. Iron absorption increased over time, but the study didn’t directly demonstrate that phytase was responsible.]
That doesn’t mean phytic acid has no effect on mineral absorption in the long term—it still does (4). But our intestines are able to adapt over time and mitigate this effect, meaning that phytic acid eventually becomes less important.
Most people have bigger problems than phytic acid
The more I learn about health, the more I tend to focus my attention on a few simple factors that I think account for most of the health benefits of diet and lifestyle. Don’t smoke cigarettes or use alcohol excessively. Get regular physical activity. Eat whole foods. Get restorative sleep. Manage stress. And don’t eat too many calories. These guidelines may not be very exciting, but they deliver a lot more value than the details that often distract us.
The US diet, and the diets of most other affluent nations, are a nutritional disaster in some ways. Although we’ve largely solved the problems of frank nutrient deficiency and starvation, we grow fat and undermine our health by eating calorie-dense processed and refined foods. The number one source of calories in the diet of Americans of all ages is “grain-based desserts” like cake, cookies, donuts, and pastries (5). Pizza, soda, and alcohol are also in the top six. The diets of most other affluent nations aren’t much better– nearly all of them are high in refined starch, sugar, added fats, and convenience foods.
Considering this context, avoiding phytic acid is simply not high on my priority list anymore. Replacing refined and processed foods with unrefined foods is more important, and if that means a higher intake of phytic acid, then so be it.
A diverse omnivorous diet is robust to modest changes in mineral availability
Diets that are overly reliant on whole grains can get people into nutritional trouble—and that is at least in part due to phytic acid. Populations with a high intake of unfermented whole grains sometimes suffer from nutritional problems including deficiency of calcium and zinc leading to rickets, osteomalacia, and stunting (6, 7). And this doesn’t just happen to poor rural farmers—it also happens to affluent people following the macrobiotic diet, which is an extreme type of vegan diet based largely on brown rice, vegetables, and soy (8).
But there’s a simple solution to this nutritional problem: eat a diverse diet. Meat, eggs, vegetables, potatoes, and particularly dairy contain easily absorbed minerals that complement the shortcomings of whole grains.
We often think of food in terms of the essential nutrients it provides, and we tend to intuitively assume that more is better. But despite a large volume of research, there is hardly any evidence that exceeding an adequate intake of essential vitamins and minerals is beneficial. If it were, multivitamin pills would be the bee’s knees—but the evidence overall suggests that they add little or no value to the average affluent diet* (9). Given these findings, I’m even more skeptical that they add value to a whole-food-based diet for most people.
The point is that unless your diet is based primarily on unfermented whole grains, if you eat a nutrient-dense diet you can probably get away with a lower absorption rate of certain minerals without any ill effects. And few people in affluent nations eat a diet that’s based primarily on unfermented whole grains.
Phytic acid remains a nutritional concern among people whose diets are based primarily on unfermented whole grains and who eat little or no animal foods. This includes people from parts of India or Pakistan who rely heavily on unleavened whole wheat chappatis, as well as people following a vegan diet, particularly a macrobiotic vegan diet. This follows a general nutritional principle: the more restricted your diet, the more carefully you have to compose it to achieve adequate nutrition.
Conclusion
Phytic acid is a substantial nutritional concern in people with a high intake of whole grains and a low intake of animal foods, but it’s probably much less important in the context of a diverse, omnivorous diet. In countries like the US, most of us have more pressing things to worry about than how much phytic acid we’re eating, and in my opinion, focusing on whole foods is a higher priority. I now often eat regular rolled oats for breakfast, but I tend to eat it with plain yogurt to make up for its high content of phytic acid. I don’t worry about the phytic acid in beans and nuts.
*There are a few exceptions. Folic acid supplementation decreases the risk of neural tube defects in infants. But these are fairly rare to begin with (less than 1 in 1,000 live births in the US; 10). Vitamin D supplementation can prevent rickets and perhaps reduce the risk of respiratory tract infections (11).
Tweet

Share on Tumblr

May 17, 2017
Two things I’ve changed my mind about, part I: Butter
I like to believe I can update my beliefs when presented with new evidence or a better interpretation of the same body of evidence, rather than clinging to my old beliefs. In the next two posts, I’ll discuss two examples where that has happened. Years ago, I argued that butter may make positive contributions to health. My thinking has gradually evolved since then, and I now think less refined forms of dairy are preferable to butter. Here’s why.
The whole food heuristic
Heuristics are simple rules that get us most of the way to the truth. One of the most valuable heuristics in nutrition is also one of the simplest: eat minimally refined foods. This single-handedly eliminates nearly all of the calorie-dense, nutrient-poor ingredients and foods that contribute to obesity and noncommunicable disease. The whole food heuristic is not only supported by a large and growing body of evidence, it’s also consistent with evolutionary considerations and common sense.
Food refining is a continuum. For example, when considering sugar, whole fresh fruit is a minimally refined source, while white sugar is a maximally refined source. Fruit leather and fruit juice are somewhere in between. Where is butter on that continuum? It’s not as refined as liquid seed oils, which are typically solvent extracted, degummed, bleached, and deodorized. It doesn’t require industrial technology to produce. But it’s certainly much more refined than milk, the whole food it’s derived from. To illustrate this, consider that typical milk only contains 3-4 percent fat by weight when it comes out of a cow. Making butter is a process of concentrating a small fraction of milk by 30-fold. And as a result, a wide variety of nutrients are separated out and calorie density increases greatly.
Dairy fat may still have nutritional value, but why not eat it in a less refined form that is more nutritious and less calorie-dense?
Blood lipids
Circulating lipoproteins influence cardiovascular disease risk, and LDL is a particularly important one. Things that increase the number of LDL particles, and/or their total cholesterol cargo (called LDL cholesterol) tend to increase cardiovascular disease risk. The evidence supporting this is now extremely strong (1, 2).
As it turns out, butter increases LDL cholesterol and particle number more than most other fats (3, 4, 5, 6). While butter also increases “good” HDL cholesterol, recent drug trials have questioned the causal relevance of increasing HDL cholesterol, meaning that it may not actually protect you from an increase in LDL cholesterol (7).
Recent evidence suggests that the effect of dairy fat on LDL cholesterol depends heavily on the context in which the fat is delivered. Less refined forms of dairy such as yogurt, cheese, and cream have little effect on LDL cholesterol, even when they deliver the same amount of dairy fat as butter (8, 9, 10, 11)! Some research suggests that this is due to a protective substance in less refined dairy foods called the milk fat globule membrane, which is lost during the butter-making process (12).
Calorie intake
Face it: the main reason we eat butter is that it tastes amazing. And this is no surprise. Butter is one of the most calorie-dense foods in the world, and the human brain likes calories (for an explanation of why, see my book The Hungry Brain). Most of us eat too many calories, and butter isn’t helping.
Fat isn’t automatically fattening, but research suggests that it can be fattening when it meets two criteria: high calorie density and high palatability. Butter gets near-maximal scores on both. Why not get the same nutrients and more from yogurt, which is less calorie-dense, less extreme in palatability, more sating per calorie, and therefore more likely to favor a healthy calorie intake?
Conclusion
The whole food heuristic is probably the simplest and most effective diet rule we have, and it suggests that whole sources of dairy should be healthier than butter. Research in the areas of cardiovascular disease and appetite control are increasingly supporting this prediction.
That said, butter isn’t toxic, and if you want to use a little to saute onions or mix into steamed vegetables, I doubt it will have much negative impact on an otherwise healthy diet. But extra-virgin olive oil is probably better for cardiovascular health, and if you choose to eat dairy, it may be preferable to focus on less refined forms of it, particularly yogurt.
Tweet

Share on Tumblr

April 1, 2017
Announcing the Bland Food Cookbook
Old April Fools post!
My book The Hungry Brain explains why we overeat and offers strategies to combat it, but it doesn’t go into great detail on how to apply this knowledge. One of the most potent drivers of overeating is food reward, or the seductiveness of food that drives us to eat things like cookies, chocolate, fancy coffee drinks, bacon, and chips. Eating a lower-reward diet helps reduce calorie intake and body fatness, but how do we put that into practice? By popular demand, the answer is here: The Bland Food Cookbook.
If you’ve been following my writing over the years, including my recent book, you know that the diets of our distant ancestors were much blander than the modern affluent diet, and that this is probably one of the reasons why they tended to be leaner than we are today.
How can we reclaim the leanness of our ancestors? We know what we should be doing, but sometimes we don’t know how. Enter The Bland Food Cookbook, available today.
To research The Bland Food Cookbook, I scoured dozens of 19th and 20th century cookbooks from the British Isles, selecting only the very blandest recipes. Offering 53 recipes in stunning black-and-white print, The Bland Food Cookbook includes such classics as “potato”– a dish perfected in 19th century Ireland:

The Bland Food Cookbook also brings back some of the most popular recipes from The Eocene Diet, such as the perennial favorite “termites on a stick”.

Described by The New York Times as “delightfully boring” and Publisher’s Weekly as “palate-numbing”, The Bland Food Cookbook is certain to keep your unruly tastebuds in check. Buy your copy today!
April fools!!
Tweet

Share on Tumblr

March 20, 2017
Meta-analysis: Impact of carbohydrate vs. fat calories on energy expenditure and body fatness
Sometimes, a meta-analysis (quantitative study of studies) is just what the doctor ordered to inoculate us against the shortcomings of our own cognition. When a topic has been studied extensively and it has produced many studies of varying quality, this lends itself to incorrect conclusions because we can find studies to support almost any belief. This is problematic because we naturally tend to gravitate toward evidence that reinforces pre-existing beliefs, and away from evidence that challenges beliefs. Called confirmation bias, this phenomenon afflicts all of us and has to be actively managed if we want to arrive at reliable knowledge. Systematically examining a body of evidence and integrating it mathematically is a useful tool for combating this bias. A new meta-analysis examines the effect of carbohydrate vs. fat calories on energy expenditure and body fatness, giving us the most objective view of this question to date.
The study
Recently, Drs. Kevin Hall and Juen Guo published what I believe is the first meta-analysis of controlled feeding studies that compared diets of equal calorie content but differing in carbohydrate and fat content (1). They only considered studies in which all food was provided by researchers and protein intake was held constant between diets. Their outcomes were energy expenditure and body fatness.
The results
They identified 28 studies that met their criteria for energy expenditure. Combining the data of these 28 studies, they found that calorie-matched diets predominating in fat vs. carbohydrate have almost identical effects, but higher-carbohydrate diets do lead to a slightly higher energy expenditure. This difference was statistically significant but of little medical or practical relevance, since it only amounted to 26 Calories per day. This slightly higher energy expenditure is consistent with the fact that the metabolism of carbohydrate is slightly less efficient than the metabolism of fat, meaning that a bit more energy is wasted*.
Examining the data, the paper’s result is not hard to believe because only 8 of the 28 studies reported that lower-carbohydrate diets led to a higher energy expenditure than higher-carbohydrate diets, and among those 8, the results were only statistically significant in four. In contrast, 20 studies reported higher energy expenditure with higher-carbohydrate diets, and that was statistically significant in 14. One can choose individual studies that support either belief, but the overall evidence suggests that the relative carbohydrate and fat content of the diet has little impact on energy expenditure.
Onward to body fatness. Hall and Guo identified 20 controlled feeding studies that reported changes in body fatness on equal-calorie diets differing in fat and carbohydrate content. Echoing the energy expenditure finding, they found that diets predominating in carbohydrate or fat have similar effects on body fatness. Yet higher-carbohydrate diets do lead to a slightly greater loss of body fat per calorie, amounting to a 16 gram per day difference. This is actually a larger difference than one would predict from the difference in energy expenditure, which would only be 2.8 g/day.
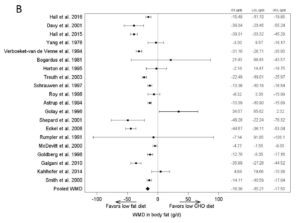
Discussion
Given this new meta-analysis, I think it’s now fairly safe to say that in a general sense, equal calories from fat and carbohydrate have similar effects on energy expenditure and body fatness, with a possible small “metabolic advantage” for higher-carbohydrate diets. This doesn’t imply very much about the real-world effectiveness of low-fat and low-carbohydrate diets because it doesn’t factor in free-living calorie intake, but it is relevant to certain popular theories about how those diets work. The upshot is that you shouldn’t expect altering the carbohydrate-to-fat ratio of your diet to work magic on your metabolic rate, but rather you should choose a diet that controls your calorie intake effectively and sustainably.
It is no longer tenable to suggest that carbohydrate per se reduces energy expenditure and causes the accumulation of body fat independent of calorie intake. This idea was never very well rooted in evidence, but now that we have a meta-analysis it is clear that it resulted from confirmation bias.
This meta-analysis leaves many questions unanswered. Is the same effect observed during weight gain, weight maintenance, weight loss, and weight loss maintenance, or could the ratio of carbohydrate to fat matter in these scenarios**? Is the effect observed equally at moderate macronutrient ratios and at the extremes? We have individual studies that address these questions, but no meta-analysis yet.
Hall and Guo’s paper is not just a meta-analysis. It’s a review of obesity energetics, body weight regulation, and their relationship to diet composition. It is hands-down the single most informative paper I’ve encountered for explaining the relationship of energy intake and expenditure to body fatness, and the big-picture view of how the body’s energy control systems work. It comes from a research group that is at the leading edge of these questions. It took me years of study to formulate the high-level perspective that you can now get from an hour of reading (1). It also dovetails nicely with chapters 1, 6, and 7 of The Hungry Brain.
* I’m not certain that this explains the higher energy expenditure; I’m just suggesting that it’s an obvious possibility.
** A study by Dr. David Ludwig’s group suggests the possibility that the outcome could be different in the context of weight loss maintenance (2). I doubt there are enough studies on this to support a proper meta-analysis.
Tweet

Share on Tumblr

February 23, 2017
The impact of weight loss on the drive to eat
Weight loss engages a “starvation response” that acts to regain the lost weight, and this is a key reason why weight loss is difficult and often temporary. This starvation response includes an increase in the drive to eat and a decrease in calorie expenditure. Using a clever study design, Kevin Hall and colleagues recently quantified the contribution of eating drive to this starvation response. The results suggest that increased eating drive is the primary way in which the starvation response opposes weight loss.
Countless controlled trials have shown that weight loss is difficult, regardless of the approach. Not only is it unlikely that a person with obesity will lose all of his excess fat, but in most cases even moderate losses are regained over time. A key reason for this is that weight loss decreases the circulating concentration of the hormone leptin, activating a negative feedback process that I call the “starvation response”, which I explain in greater detail in my book. This response attempts to bring more calories into the body, and curtail the flow of calories out of the body, thereby refilling fat stores. The starvation response includes an increase in the drive to eat (hunger, food seductiveness) and a decrease in calorie expenditure (slowed metabolic rate and physical activity calorie expenditure).
The “calories out” side of this equation has been fairly well characterized, yet we don’t know nearly as much about the “calories in” side due to the challenges inherent in measuring it. A new paper from Kevin Hall’s research group asks the important question, how strongly does the increased drive to eat counter weight loss? To do this, they used a clever study design in which weight loss was covertly induced.
The study
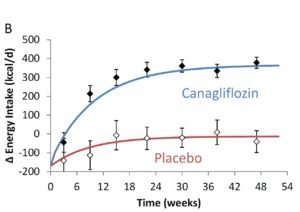
Hall’s team used data from a one year randomized, placebo-controlled trial of a drug called canagliflozin in 242 people with type 2 diabetes and obesity. Canagliflozin causes substantial loss of glucose via the urine and is used to improve blood glucose control in diabetes. This loss of glucose is roughly 90g per day, amounting to about 360 Calories.
Importantly, since this was a double-blind trial, neither the investigators nor the subjects had direct knowledge of who was receiving the drug. The study involved a long-term, covert perturbation of energy balance that “largely bypasses the volition of the subjects”, which makes it an unusually pure test of the brain’s response to changes in body weight.
Using previously validated mathematical models, and measured body weight changes, Hall’s team estimated the calorie intake of the canagliflozin and placebo groups over the course of the one-year trial. They then used the resulting output to estimate how calorie intake, calorie expenditure, and the drive to eat change with typical weight loss, using two years of data from a commercial weight loss program (Weight Watchers).
The results
The canagliflozin group gradually lost weight over the course of the trial, eventually plateauing about 8 pounds (3.5 kg) lighter than at the beginning. In contrast, the placebo group lost about two pounds (just under 1 kg).
Hall’s model estimates that as the canagliflozin group lost weight and the starvation response kicked in, their calorie intake gradually increased by about 350 Calories per day, eventually halting their weight loss. The model estimates that for each 2.2 pounds (1 kg) of body weight lost, the brain ramps up the drive to eat by about 100 Calories per day in an attempt to regain the weight!
With this information in hand, the researchers were able to gain insight into what happens during typical weight loss due to diet and lifestyle change. Data from a two-year commercial weight loss trial showed that participants experienced their maximum weight loss at 6 months, then gradually regained over the following year and a half.
Plugging these numbers into Hall’s model, they estimate that the initial calorie deficit was about 700 Calories per day, but that this rapidly rebounded, and had almost returned to baseline by 9 months. This might suggest that the participants just stopped trying, but in fact this is unlikely to be the case, because they were still weight reduced at that point and therefore their brains were still experiencing a heightened drive to eat (see the line below labeled “homeostatic drive to eat”).
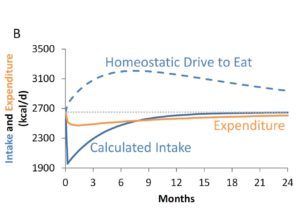
The researchers were actually able to quantify the effort the participants were putting into their diets by calculating the difference between actual calorie intake and the estimated drive to eat. The results suggest that even though people were already almost back to their baseline calorie intake by 9 months, and already beginning to regain weight, they were nevertheless expending considerable effort to stop themselves from eating substantially more than their baseline intake (to the tune of about 600 Calories per day).
Gradually, as their body weights rebounded over the last year and a half of the trial, their effort level declined toward baseline.
Discussion
This study has a notable strength, which is that energy balance and body weight were perturbed without the participants’ knowledge. We can be confident that the effects the researchers observed had nothing to do with the participants’ conscious feelings or behaviors around dieting and weight loss. They were the result of nonconscious biological processes.
The study also had at least two notable weaknesses. The first is that the participants in the first trial had type 2 diabetes, which means that we can’t know how well the results would apply to people without diabetes. I’m not aware of any reason why they wouldn’t apply, and the results are consistent with what we know about weight regulation in people without diabetes, but we still have to be cautious. The second weakness is that the trial perturbed calorie balance via a specific mechanism– the excretion of blood glucose in the urine. It’s theoretically possible that the results would have been different if the drug had caused the participants to excrete fat. I don’t think this is very likely, but this question might be tractable by studying randomized trials of Olestra, the fat substitute that gets excreted in feces. Or perhaps by studying liposuction patients.
There are several interesting implications of this study. The first is that the data support our current understanding of how body weight is regulated. Even when energy balance was perturbed without the participants’ knowledge, a powerful starvation response occurred that favored the regain of lost weight. The data support the concept that a sort of body weight “set point” is defended against changes, particularly changes in the downward direction.
A second implication is that between the two arms of the starvation response– the increased drive to eat and the decreased calorie expenditure– the former is by far the most influential. In other words, the primary way in which the brain opposes weight loss is by increasing the biological drive to eat. The data also give us a quantitative estimate of this drive: for each 2.2 lbs (1 kg) of weight lost, the drive to eat increases by about 100 Calories per day*. This is even stronger than I would have predicted.
A third implication– which I think is the most novel of the study– relates to the dynamics of the heightened drive to eat that people experience when they diet, and how this undermines weight loss efforts. After a person loses weight, the biological drive to eat can be so high that they have to exert considerable effort just to prevent themselves from overeating substantially. Even though it seems like they’re no longer adhering to their reduced calorie regimen, they may still be trying hard to eat fewer calories– and succeeding, relative to the amount their brain “wants” them to eat.
The amount of effort that people put into a diet does slowly decline over time however, and as this effort recedes, the biological drive to eat takes over and weight comes back. It’s hard to fight the starvation response forever.
This study strengthens my conviction that the brain’s starvation response has to be managed for long-term weight loss success– and particularly its impact on the drive to eat. Rather than pretending like the starvation response doesn’t exist, as most weight loss approaches do, a better method may be to try to dampen appetite and/or passive calorie intake sufficiently to counterbalance the heightened drive to eat. In other words, find ways to keep the brain happy at a lower calorie intake rather than using willpower to continually struggle against the biological drive to eat.
* I don’t think these results can tell us whether or not the relationship is linear, e.g. if 1 kg of weight loss causes an increase in the drive to eat by 100 Calories, would a 5 kg loss cause an increase of 500 Calories, 10 kg, 1000 Calories, etc.? It’s possible that there is a plateau at some point where the response reaches its maximum strength. Another way of saying this is that this simple rule of thumb may not necessarily apply over the entire range of weight changes. We would need more research to explore this possibility.
Tweet

Share on Tumblr

February 14, 2017
Book Review: Syndrome X, The Silent Killer
Gerald Reaven is the researcher who first identified the state of insulin resistance and played a central role in defining its consequences. Understanding insulin resistance is worthwhile, and if we want to do so, his work is one of the most informative places to look. I recently read his general-audience book Syndrome X: The Silent Killer, and I’ll share my thoughts on it in this review.
While doing research for my review of The Case Against Sugar, I saw that Gerald Reaven had written a general-audience book on insulin resistance, its consequences, and how to manage it. The book is titled Syndrome X: The Silent Killer, and it has two co-authors named Terry Kristen Strom and Barry Fox. It was published in 2000 and is a bit outdated in some ways, but since Reaven has played such a key role in our modern understanding of insulin resistance, much of the information it contains is still relevant. It isn’t very technical but it does cover a lot of scientific ground, and the book includes a nice bibliography at the end chronologically summarizing Reaven’s work on this topic as of 1999.
My review will be organized differently than the book, but in the way that I find the most logical. First, I’ll discuss Reaven’s definition of insulin resistance and a related condition he calls “syndrome X”, then what causes it, then its consequences, and finally how to manage it.
What is syndrome X?
Syndrome X is Reaven’s term for a common cluster of metabolic abnormalities that is now more commonly called the metabolic syndrome. This includes some combination of elevated circulating insulin, high blood pressure, high blood triglycerides, low HDL cholesterol, slow clearance of glucose and fat from the blood following a meal, small, dense LDL particles, increased blood clotting, and a decreased ability to dissolve blood clots. Today, abdominal obesity is also considered a defining characteristic. The book says that syndrome X affects 25-30 percent of people, although the number is likely higher today.
The common cause of these metabolic problems, the authors argue, is an impaired response of tissues to the hormone insulin. Insulin is a very important hormone for metabolic regulation. It plays many roles, but most of them revolve around regulating levels of glucose and fat in the blood, and coordinating the metabolic shift between using carbohydrate vs. fat as fuel in response to what’s coming in via the diet.
When tissues don’t respond to insulin effectively, the pancreas secretes more of it in an attempt to compensate. Yet different tissues become insulin resistant to different degrees, so in the end some tissues get too little insulin while others get too much. This, they argue, likely accounts for the various manifestations of syndrome X.
The causes of syndrome X
The book’s position on the causes of insulin resistance and syndrome X is inconsistent, at least superficially. The authors repeatedly state that excess body fatness, physical inactivity, cigarette smoking, and genetics contribute to insulin resistance, and that weight loss and exercise can substantially decrease insulin resistance. Yet in chapter 6, one of the “fallacies” they list is that obesity causes insulin resistance.
How do we reconcile this apparent contradiction? I think the point the authors were trying to make with their “fallacy” comment is that obesity is not the sole driver of insulin resistance, and that genetics may in fact be more important. Elsewhere in the book, they explore the evidence on the contributions of genetics, body fatness, and lifestyle to insulin resistance, and conclude that genetics accounts for about half of it, body fatness about 25 percent, and physical fitness about 25 percent. This is consistent with the current majority view in the scientific community, which I share, that insulin resistance is primarily driven by body fatness, physical inactivity, and genetics.
Reaven has harsh words for public low-carbohydrate diet advocates such as Robert Atkins, who he feels have misrepresented his research. I don’t know what Atkins wrote about Reaven’s work, but it was definitely misrepresented in Gary Taubes’s book The Case Against Sugar. Reaven’s work validates some of the views that are prevalent in the low-carbohydrate diet community and undermines others. It’s notable that nowhere in the book do they argue that eating carbohydrate or sugar contributes to insulin resistance, and they also state that calorie intake and expenditure, not macronutrients, determine body fatness.
The consequences of syndrome X
Much of Reaven’s research, and his book, focused on the cardiovascular consequences of syndrome X. From the list of metabolic characteristics I shared above, it’s not hard to understand how syndrome X might damage the cardiovascular system. High blood pressure, high blood glucose and lipids, low HDL, high triglycerides, small, dense LDL particles, and a tendency to form blood clots are all risk factors for cardiovascular disease. Consistent with this, his research has shown that insulin resistance is a strong predictor of cardiovascular risk (1).
He also discusses how syndrome X often gives way to type 2 diabetes as the pancreas fails to keep up with the increasing insulin demands of insulin-resistant tissues. Reaven’s subsequent work provided a compelling basis for believing that insulin resistance is a major driver of chronic disease, including coronary heart disease, diabetes, and perhaps even cancer (2).
In popular discussions of cardiovascular disease risk, I often see two opposing camps. One camp thinks cardiovascular disease is all about LDL cholesterol, and insulin resistance is unimportant. The other camp thinks insulin resistance is everything, and LDL cholesterol is unimportant. In Syndrome X, the authors take a position that I think remains the most evidence-based today: LDL and insulin resistance are both important drivers of cardiovascular disease risk. They argue that the absence of elevated LDL cholesterol is not sufficient assurance of low cardiovascular risk, and that LDL cholesterol and insulin resistance are largely independent of one another and must be managed separately.
Managing syndrome X
The authors state that people with syndrome X respond poorly to high-carbohydrate, low-fat diets because these diets accentuate the excessive insulin release that underlies some of the metabolic features of the syndrome. While a person who is insulin sensitive may thrive on such a diet, someone who is insulin resistant may not. This is important because in the late 1990s when the book was written (and to some extent today), this was precisely the type of diet that was prescribed for people with obesity, cardiovascular disease, and prediabetes.
As an alternative, the authors offer the “Syndrome X Diet”. In a nutshell, this is a diet in which carbohydrate is partially replaced by unsaturated fat. The book contains extensive meal plans illustrating how to apply the diet. Looking through the meal plans, much of the fat comes from low-trans-fat margarine. My view is that it would be preferable to get unsaturated fat from whole food sources like nuts, avocados, and poultry.
This portion of the book contains a few statements that had me scratching my head. For example, poultry fat is classified as “saturated”, although it is generally about one quarter saturated or less. Because of this, they recommend low-fat cuts such as skinless breast. It seems to me that if the goal is to eat more unsaturated fat and less carbohydrate, full-fat poultry should be helpful.
It’s important to point out that the Syndrome X Diet is not really a low-carbohydrate diet, although my impression from the book is that Reaven isn’t against low-carbohydrate diets as a therapeutic tool. Here is the recommended macronutrient breakdown of the Syndrome X Diet, by calories:
45 percent carbohydrate
40 percent fat
15 percent protein
It’s worth noting that these numbers are pretty close to what the average American was eating in the year the book was published, as reported by the USDA (these add up to 101% due to rounding error; 3):
48 percent carbohydrate
41 percent fat
12 percent protein
So I think the goal of the Syndrome X Diet is not so much to eat a low-carbohydrate diet, but to avoid a low-fat diet.
In addition to diet, the authors recommend weight loss and physical activity to improve insulin sensitivity. As they note, these two approaches have been repeatedly shown to reduce insulin resistance.
The verdict
Syndrome X is a classic book written by a giant in the field of physiology, and I think it has stood the test of time relatively well. Although some of Reaven’s views were controversial at the time he first articulated them, at this point many of them have been incorporated into mainstream thinking.
Syndrome X probably won’t satisfy researchers who want a more technical view of Reaven’s work, but it does review this research in a way that’s approachable for a general audience, and offers evidence-based strategies for managing insulin resistance.
Tweet

Share on Tumblr

January 26, 2017
Bad sugar or bad journalism? An expert review of “The Case Against Sugar”.
 Photo by Lauri Andler
Photo by Lauri AndlerI’ve been asked by a number of people to review Gary Taubes’s new book, The Case Against Sugar. I reluctantly agreed that it would probably be a good idea for me to do so. In this post, I’ll provide something that is not available anywhere else (to my knowledge): a review of the book from the perspective of a former researcher who is an expert in some of the topics it discusses.
The Case Against Sugar is a journey through sugar history and science that argues the point that sugar is the principal cause of obesity, diabetes, coronary heart disease, and many other common noncommunicable diseases. This differs from the prevailing view in the research and public health communities that obesity and noncommunicable disease are multi-factorial, with refined sugar playing a role among other things like excess calorie intake, physical inactivity, cigarette smoking, alcohol and illegal drug use, and various other diet and lifestyle factors. I side with the latter view. In case anyone is wondering, I’ve never had any contact with the sugar industry and I have no other relevant conflicts of interest.
I’ll break the review into two parts, the first covering the historical aspects of the book, and the second covering its scientific aspects.
The History
Taubes excels at constructing detailed historical narratives to make his points. In The Case Against Sugar, he presents a colorful and informative history of sugar and the sugar industry. He also provides a history of the use of sugar in tobacco processing and how it may have contributed to the rise of cigarette smoking, which I wasn’t aware of.
His discussion of the history of research on sugar, dietary fat, obesity, and noncommunicable disease is less compelling due to its one-sided nature. For example, The Case Against Sugar portrays an epic struggle decades ago between researchers who believed that saturated fat was the primary cause of coronary heart disease, and those who believed that sugar was. These views are embodied by the American researcher Ancel Keys and the British researcher John Yudkin, respectively.
Taubes makes hay of the fact that Keys was supported in part by the sugar industry, painting Yudkin as a righteous underdog standing up to a corrupt and aggressive Keys. Yet he never gives serious consideration to the strength of the evidence supporting each man’s beliefs, instead using a historical narrative to imply that Keys was a stooge of the sugar industry who unfairly won the argument due to his sharp elbows (whether or not this is true, it’s also true that Yudkin’s evidence was not as compelling as Keys’s). This tactic of using historical narratives as a substitute for evidence is one that recurs throughout the book.
In his haste to undermine Keys, Taubes neglects to mention that Yudkin had his own conflicts of interest: he was funded by the egg, edible oil, and dairy industries, all of which had an interest in pinning the blame for obesity and chronic disease on sugar (1). It’s interesting to note that if we substitute the egg, meat, and dairy industries for the sugar industry, Taubes’s arguments about the corrupting influence of industry on science sound very similar to those that are made by certain people in the vegan community about animal foods.
The truth is that both sides have somewhat of a point, but both are also exaggerated and incomplete. Each industry jockeys to promote its own interests, and those that are sufficiently well heeled often do so by supporting research. This includes the sugar industry, as well as the egg, edible oil, meat, and dairy industries. If Taubes wants to decry research funded by the sugar industry, he should apply the same principle to research funded by other industries, including Yudkin’s. Yet Yudkin gets a pass, while Taubes probes every nook and cranny of history to uncover the dastardly Keys’s conflicts of interest.
A related point is that in 2017, research institutions and reputable scientific journals have policies in place for disclosing and limiting conflicts of interest. These policies aren’t perfect, but they’re much better than what we had two decades ago. In contrast, the book industry has no policies for managing the conflicts of interest of its authors, and it also has virtually no accountability for what it publishes. Taubes points his finger at others while never disclosing his own conflict of interest, which is that his fame and fortune rely on perpetuating his controversial ideas to an audience that has little basis for evaluating them.
In chapter 8, The Case Against Sugar discusses the process that led the Food and Drug Administration to designate sugar as “generally recognized as safe” (GRAS). GRAS is a designation that is given to substances that have been consumed for a long time and are not overtly toxic, like vinegar. Taubes implies that sugar was unjustly given GRAS status by the FDA due to food industry influence, but this reveals a lack of understanding of the GRAS designation (he repeated this claim in a recent article; 2). The purpose of the FDA is not to be a nanny that prevents us from eating food that has long-term health consequences, and consequently GRAS status doesn’t imply that a substance supports leanness or health when consumed regularly. You can eat your way to obesity and heart disease on an all-GRAS diet: Everything in pizza, white bread, French fries, soda, ice cream, potato chips, and bacon is GRAS. By all logic, sugar should be GRAS, but that doesn’t make it healthy.
Also, revoking GRAS status means that a substance cannot be sold as food. Is Taubes suggesting that the FDA should have made the sale of sugar illegal, yet continue to allow us to buy cigarettes, whiskey, and cheese crust pizza? That seems a bit extreme.
The Science
Scientifically, The Case Against Sugar suffers from a condition Steven Pinker has called the “Igon Value Problem”. This term describes the tendency of certain science journalists to arrive at obtuse conclusions due to a superficial understanding of their subject matter (3). There are many examples of this in The Case Against Sugar, but the underlying theme is that Taubes misunderstands (or chooses not to apply) the scientific method itself.
Evidence of this can be found on the first page:
The purpose of this book is to present the case against sugar– both sucrose and high-fructose corn syrup– as the principal cause of the chronic diseases that are most likely to kill us, or at least accelerate our demise, in the twenty-first century… If this were a criminal case, The Case Against Sugar would be the argument for the prosecution.
Trials proceed by very different principles than science does. The prosecutor is not expected to present a balanced case– he is expected to be biased against the defendant. What ensures balance in the legal process is the inclusion of a defendant who is equally biased in favor of himself. Yet in The Case Against Sugar, the defendant is nowhere to be found. What results is an argument that is carefully crafted to support the prosecution, while facts that support the defense are omitted, minimized, or misrepresented.
This is the opposite of the scientific method, which emphasizes objective analysis of facts and seeking evidence that might falsify your beliefs. This might be forgiven in a popular book, but in this case Taubes attempts to take the scientific high ground, portraying his views as rational and evidence-based and those prevailing in the scientific community as biased, irrational, and corrupt.
The Igon Value Problem doesn’t take long to rear its ugly head. In the introduction, Taubes deploys an argument that he believes is sufficient to negate most of the scientific literature on obesity and chronic disease… drumroll please… Occam’s Razor:
If this were a criminal investigation, the detectives assigned to the case would start from the assumption that there was one prime suspect, one likely perpetrator, because the crimes (all the aforementioned diseases [including obesity, diabetes, cardiovascular disease, Alzheimer’s, and several others- SG]) are so closely related. They would only embrace the possibility that there were multiple perpetrators when the single suspect was proved insufficient to explain all the evidence. Scientists know this essential concept as Occam’s Razor.
What if I were to tell you that the structure of DNA is actually a single straight strand rather than a double helix? Would you believe me just because my hypothesis is simpler than the conventional one? Of course not, and for good reason: evidence suggests the more complex hypothesis is correct. The truth is that Occam’s Razor is a weak argument that only applies when two hypotheses are equally well supported (or equally unsupported). As soon as one hypothesis has a stronger evidence basis than another, Occam’s Razor becomes irrelevant. Yet for Taubes, this flimsy argument is sufficient to throw most of the relevant scientific literature out the window, besides, of course, a few tidbits that support the prosecution.
Besides its misapplication of Occam’s Razor, the passage above manifests the Igon Value Problem in a second way: the diseases in question are actually not all correlated with one another, or even with sugar intake. Statistics demonstrating this are readily available. For example, sugar intake is higher today in the US than it was in the 1970s, and while obesity has increased three-fold, coronary heart disease mortality has declined by over 60 percent (4, 5, 6). Taubes neglects to inform the reader that sugar intake has been declining since 1999 in the US, a period over which obesity and diabetes rates have increased substantially (7, 8, 9).
Taubes argues that sugar is the only factor that reliably shows up when a culture develops Western noncommunicable diseases, supporting the point with examples of cultures that adopted sugar-rich diets and became ill. Yet he makes no effort to look for a counterexample that could refute his argument: a traditionally-living culture that has a high intake of sugar and does not suffer from Western noncommunicable diseases. If such a culture can be found, this piece of evidence is sufficient to reject Taubes’s argument that sugar reliably associates with the onset of these diseases in a population. Let’s do Taubes’s research for him. A well-studied Tanzanian hunter-gatherer tribe called the Hadza gets 15 percent of its average year-round calorie intake from honey, plus fruit sugar on top of it. This approximates US sugar intake, yet the Hadza do not exhibit obesity, cardiovascular disease, or any of the other disorders Taubes attributes to sugar (10, 11). In fact, many hunter-gatherer groups relied heavily on honey historically, including the Mbuti of the Congo whose diet was up to 80 percent honey during the rainy season (10). Yet they do not exhibit obesity or insulin resistance (12).
The Igon Value Problem frequently appears in Taubes’s portrayal of opposing viewpoints from the scientific community. For example, Taubes repeatedly asserts that researchers, physicians, and nutritionists simply assume that obesity causes diabetes. In fact, there is abundant and compelling evidence supporting this “assumption”, and such evidence is only a few keystrokes away on Google Scholar (13, 14, 15, 16). Yet it receives no mention in the book. Instead, the reader is gravely informed that today’s scientists, physicians, and nutritionists simply inherited the idea from the previous generation of scientists, who themselves essentially plucked it out of thin air. This is followed by Taubes’s alternative viewpoint, which seems downright reasonable by comparison despite the weak evidence offered to support it.
Here’s a third example. Taubes upbraids the research community for its belief that body fatness is determined by calorie intake, rather than the impact of foods on insulin. He supports the latter proposition with semi-anecdotal observations from Africa suggesting that a group of people eating a high-sugar diet supplying “as little as sixteen hundred calories per day” were sometimes obese and diabetic.
A person who actually wants to get to the bottom of this question should conduct their investigation in a very different manner. The first order of business is to look up the relevant metabolic ward studies, which are the most tightly controlled diet studies available. These studies consistently show that calorie content is the only known food property that has a meaningful impact on body fatness. This is true across a wide range of carbohydrate-to-fat ratios and sugar intakes, and a correspondingly wide range of insulin levels (17).
What makes Taubes’s oversight so extraordinary is that he was involved in funding one of these metabolic ward studies, which compared two diets that differed more than tenfold in sugar content. The results showed that a 25 percent sugar, high-carbohydrate diet caused slightly more body fat loss than a 2 percent sugar, very-low-carbohydrate (ketogenic) diet of equal calories (18). Despite these clear and consistent findings, Taubes continues to insist that calorie intake is not an important determinant of body fatness, and he offers the reader questionable evidence in support of this while omitting high-quality evidence to the contrary. All while exuding righteous indignation about the scientific community’s misguided beliefs.
A fourth and final example of the Igon Value Problem. Taubes states that obesity researchers have been barking up the wrong tree since World War II because they are so focused on calories that they have no interest in the influence of hormones on body fatness. This is another instance in which a cursory Google Scholar search could have prevented a colossal mistake: the search term “leptin obesity” alone returns 385,000 results, all since 1994. In fact, researchers are extremely interested in hormonal influences on body fatness, which is why the topic has been studied extensively and so many relevant hormones have been identified (for example, leptin, ghrelin, glucagon, GLP-1, epinephrine, and amylin).
Taubes’s revisionist history of obesity research allows him to argue that the reason why insulin’s central role in obesity hasn’t been uncovered is that no one is looking. The truth is that researchers have examined insulin up, down, and sideways, and found that it is unlikely to contribute to common obesity. Yet this evidence isn’t discussed in The Case Against Sugar, nor in Taubes’s previous book Good Calories, Bad Calories— it is simply assumed not to exist.
In the final chapters of The Case Against Sugar, Taubes argues that insulin resistance is the primary cause of common noncommunicable diseases like coronary heart disease, diabetes, Alzheimer’s disease, and gout, and that sugar is the primary cause of insulin resistance (he goes out of his way to emphasize that dietary fat, calorie intake, and physical activity are irrelevant). The former proposition can be reasonably argued, while the latter is a case of Taubes cramming a square peg into a round hole. Taubes leans heavily on the animal literature, correctly stating that high intakes of refined sugar sometimes cause insulin resistance in rodent models. But he omits two inconvenient facts: First, sugar is not very fattening in rodents, particularly relative to added fats like lard; and second, added fats also tend to cause more severe insulin resistance than sugar (19, 20, 21, 22, 23, 24).
The combination of added fat and sugar is even more harmful than fat alone, and the most fattening and insulin-resistance-inducing diet of all is to give rodents free access to a variety of highly palatable human foods (25, 26). Sugar alone cannot remotely explain the effects of palatable human food on body fatness and health in rodents– or in humans– although it does contribute.
The mechanism Taubes proposes for how sugar causes insulin resistance is that the fructose component, making up 50 percent of table sugar, overloads the liver, rendering it less sensitive to the insulin signal, and this eventually causes whole-body insulin resistance. Taubes is correct about the impact of fructose on the liver, although again he leaves out critical information: realistic doses of fructose primarily overload the liver if a person is overconsuming calories and liver energy stores are already full (25). This is probably why hunter-gatherer groups such as the Hadza can eat as much sugar as Americans and not develop health problems (26, 27). These facts do not fit Taubes’s narrative that calories are irrelevant, and they are not shared with the reader.
Here are two other inconvenient facts that Taubes omits from his finely crafted narrative: Both sedentary behavior and overeating calories cause pronounced insulin resistance, and conversely, physical activity and eating fewer calories powerfully combat insulin resistance (28, 29, 30, 31). Physical activity almost instantaneously increases the insulin sensitivity of muscle tissue, which is a major determinant of whole-body insulin sensitivity. Again, abundant evidence of this is only a few keystrokes away on Google Scholar, yet Taubes dismisses the idea out of hand.
During the course of his argument, Taubes uses sleight of hand to portray the views of researchers as more favorable to his ideas than they really are. For example, in chapter 9 he argues that obesity and physical inactivity are not the real causes of insulin resistance, rather sugar causes both insulin resistance and obesity. To support his theory, he invokes the work of Stanford endocrinologist Gerald Reaven, claiming that he “was bringing back the notion that carbohydrates were bad”. This seemed mighty fishy to me, so I looked up what Reaven actually thinks. Here’s a quote from a review paper he wrote (emphasis mine) (32):
Since being overweight/obese and sedentary decreases insulin sensitivity, it is not surprising that the prevalence of the manifestations of the [insulin resistance syndrome] is increasing at a rapid rate. From a dietary standpoint, there are two approaches to attenuating the manifestations of the [insulin resistance syndrome]: (a) weight loss to enhance insulin sensitivity in those overweight/obese individuals who are insulin resistant/hyperinsulinemic; and (b) changes in macronutrient content of diets to avoid the adverse effects of the compensatory hyperinsulinemia [i.e., replacing carbohydrate with unsaturated fat- SG].
Taubes neglects to inform the reader that Reaven thinks obesity and physical inactivity cause insulin resistance, and that these factors explain the rising prevalence of metabolic disease– precisely what Taubes is arguing against in that passage. Furthermore, Reaven explains in no uncertain terms that he does not think insulin resistance causes weight gain.
Rather than straightforwardly reporting what Reaven’s studies revealed and what the man believes, Taubes takes Reaven’s argument that people with existing insulin resistance may benefit from carbohydrate restriction and warps it to make it appear as if Reaven supports Taubes’s beliefs about the origins of insulin resistance. In doing so, Taubes flips Reaven’s position by 180 degrees. If you want the real scoop on Reaven’s important work, go straight to Reaven’s book Syndrome X.
I’ll end this section on a positive note. In The Case Against Sugar, Taubes finally acknowledges the importance of food reward in eating behavior and obesity. As a reminder, food reward is the seductiveness of certain foods (like ice cream and chips) that motivates us to eat them, and as common sense suggests, it’s an important influence on what and how much we eat. Previously on his blog, Taubes argued at length that food reward has nothing to do with obesity, and (remarkably) that the brain itself is unimportant (33). In The Case Against Sugar, he argues that the seductiveness of sugar is precisely why we eat it, ultimately leading to obesity. He even briefly discusses dopamine, the chemical mediator of reward, acknowledging both the importance of food reward and the brain generally in food intake and obesity. This is progress.
Conclusion
Science is imperfect, and scientists are as well. Pioneers such as John Ioannidis, Brian Nosek, Vinayak Prasad, Adam Cifu, Chris Chambers, and David Allison are making a good faith effort to identify flaws in the scientific process and address them. Journalists have an important role to play here as well, by helping to identify problems and raising awareness about how to fix them. Taubes also views science as flawed, but primarily where it disagrees with his personal beliefs. Rather than contribute to the solution, Taubes adds to the problem by promoting an unscientific thought process that systematically excludes opposing evidence.
To answer the question posed in the title, refined sugar is bad, although not the singular cause of all humankind’s ills. A core principle of journalism is the accurate, objective, and complete transmission of pertinent facts to the reader. The Case Against Sugar is a journey through sugar history and science that is heavily distorted through the lens of Taubes’s personal beliefs. By this metric, it is not journalism, but advocacy. To a general audience that has little basis for evaluating its claims, the book will be misleading. Yet for readers who are willing to take The Case Against Sugar with a case full of salt, it does contain some interesting history.
Tweet

Share on Tumblr

January 25, 2017
Book Update
 Hello, folks. My book, The Hungry Brain: Outsmarting the Instincts that Make Us Overeat is due to be released on February 7, and I’m very excited about it. It’s substantially different from any other book on overeating and weight management, and I believe it will inject much-needed information into the public discourse on obesity. Given that the brain governs all behavior including eating, it’s remarkable that no other general-audience book has looked broadly at its role in overeating and body weight (to my knowledge). The Hungry Brain is based on thirty-six expert interviews, hundreds of scientific papers, and my own scientific expertise. My goal is to give you the best that neuroscience, obesity research, and my noggin have to offer.
Hello, folks. My book, The Hungry Brain: Outsmarting the Instincts that Make Us Overeat is due to be released on February 7, and I’m very excited about it. It’s substantially different from any other book on overeating and weight management, and I believe it will inject much-needed information into the public discourse on obesity. Given that the brain governs all behavior including eating, it’s remarkable that no other general-audience book has looked broadly at its role in overeating and body weight (to my knowledge). The Hungry Brain is based on thirty-six expert interviews, hundreds of scientific papers, and my own scientific expertise. My goal is to give you the best that neuroscience, obesity research, and my noggin have to offer.
The Hungry Brain has received outstanding reviews from The New York Times, Publisher’s Weekly, and many knowledgeable individuals. You can read excerpts on my book page.
I’ll be doing a book reading and signing at The Elliott Bay Book Company in Seattle on February 8 at 7:00 pm. Come hear me read a bit from the book, expand on one of the topics in it, and take questions.
Behind the scenes, my publicist and I are cooking up a few strategies to help get the word out. In the coming weeks, I’ll be appearing in a number of interviews. I may do a Reddit AMA. If you think my work is valuable, please spread the word!
Tweet

Share on Tumblr

Did the US Dietary Guidelines Cause the Obesity Epidemic?
A popular argument holds that the US Dietary Guidelines caused our obesity epidemic by advising Americans to reduce fat intake. Does the evidence support this idea, or is it simply a fantasy?
Introduction
Low-fat diets have fallen out of style and are now a favorite punching bag in some corners of the popular media, the Internet, and the scientific literature. And there are reasons for this. As typically implemented, low-fat diets have largely failed to live up to their promise of reducing the risk of obesity, cardiovascular disease, and diabetes. Randomized controlled trials over the last two decades have increasingly supported the position that higher-protein, lower-carbohydrate, and sometimes higher-fat diets promote greater weight loss than low-fat diets over the short- to medium- term.
The truth is that this is a significant medical reversal. Researchers and public health authorities accepted a hypothesis– and dispensed advice based on it– to later learn that the hypothesis was not as well supported as they had thought. This is fair to point out.
Yet this idea often gets pushed a step further: by shifting our diets away from fat and toward carbohydrate beginning in 1980, the US Dietary Guidelines actually contributed to the obesity epidemic. This idea has been promoted in several popular books, and most recently, in an editorial published in the Journal of the American Medical Association (1). Here is the relevant quote:
As a result of [US dietary guidelines], dietary fat decreased to near the recommended limit of 30% total energy. But contrary to prediction, total calorie intake increased substantially, the prevalence of obesity tripled, the incidence of type 2 diabetes increased many-fold, and the decades-long decrease in cardiovascular disease plateaued and may reverse, despite greater use of preventive drugs and surgical procedures. However, other changes in diet (such as meals away from home) and lifestyle (such as physical activity level) may have influenced these trends.
Recent research suggests that the focus on dietary fat reduction has directly contributed to this growing burden of chronic disease.
As usual, when someone makes a factual statement, they are stating a hypothesis. Whether or not the hypothesis is correct depends on whether its key predictions are supported by compelling evidence. So let’s go through some key predictions of this hypothesis and see if the evidence supports them.
Prediction 1: There should be a correlation between the publication of the Dietary Guidelines and the obesity epidemic
The US government has been publishing dietary information for at least 120 years, and the 1980 version wasn’t the first to recommend limiting the intake of fatty foods (2). Still, it could be argued that the 1980 version was more strongly worded and more influential of public eating habits.
Americans have been growing fatter for over a century (3), but the trend has accelerated over the past 3-4 decades, and we call this acceleration the “obesity epidemic”. This epidemic was first clearly detected by the 1988-1994 NHANES survey. The previous survey was conducted between 1976 and 1980, so we can say that it began sometime between 1980 and 1988 (4).
Roughly speaking, it is true that there’s an association between the publication of the 1980 Guidelines and the obesity epidemic. Yet by itself, this is very weak evidence, due to the large number of other things that also changed over that time period. For the hypothesis to be credible, it will need more support.
Prediction 2: Americans should have reduced our fat intake in response to the Guidelines
If the Dietary Guidelines caused us to gain weight by putting us on a low-fat diet, there should be evidence that we actually began eating less fat in response to the Guidelines. If not, the hypothesis cannot be correct.
Two independent lines of evidence suggest that our absolute fat intake did not decline after the publication of the Guidelines (5, 6). Proponents of the hypothesis invariably cite the fact that the percentage of fat in the US diet declined, which is true (although the change was rather small). The reason the percentage changed is not because our fat intake decreased, but because our carbohydrate intake increased, along with our total calorie intake. Does this count as a low-fat diet?
As an analogy, imagine a man named Jim who has obesity. Jim wants to lose weight, so he decides to eat a low-carbohydrate diet. Rather than reducing his intake of carbohydrate, Jim adds fat to all his meals so that the percentage of carbohydrate in his diet decreases. Jim’s calorie intake increases from 3,000 to 4,000 Calories per day, and his absolute carbohydrate intake remains the same. Yet the percentage of carbohydrate in his diet decreases from 45% to 34%. Is Jim on a low-carbohydrate diet, and should we expect him to lose weight?
Of course not. Jim isn’t eating a low-carbohydrate diet, and neither have Americans been eating a low-fat diet.
3. Low-fat diets should cause weight gain
For this hypothesis to be correct, low-fat diets have to cause weight gain. While low-fat diets as typically implemented may not be a very effective weight management tool, decades of research shows that they cause weight loss, not weight gain. This is true even when we only consider studies that didn’t involve deliberate calorie restriction (7, 8).
The fact that low-fat diets cause less weight loss than low-carbohydrate diets over the short- to medium-term doesn’t mean low-fat diets cause weight gain. Both diets are more slimming than eating as much as you want of everything.
4. People who followed the Guidelines should have gained more weight than people who didn’t
If the Guidelines caused the obesity epidemic, then the people who actually followed the advice should have gained more weight than the people who didn’t. Yet the evidence shows precisely the opposite (9). Here’s the money quote:
Poor compliance with the Guidelines, rather than the guidelines themselves, is likely responsible for the weight gain observed in the American population. Adoption of an eating pattern consistent with the Dietary Guidelines should facilitate population weight control if sustained long term.
5. Other countries with dissimilar dietary guidelines should not have a similar obesity problem
I’m not going to do an in-depth analysis of how national dietary guidelines relate to changes in weight, but I’ll simply point out that nearly all affluent nations have been gaining weight rapidly in recent years, regardless of dietary advice or lack thereof (10). The US is only unique in the sense that we’re on the leading edge of economic, dietary, lifestyle, weight, and health changes that are affecting the entire affluent world.
The verdict
Although the low-fat diet doesn’t appear to be a silver bullet for our national weight problem, the hypothesis that US Dietary Guidelines caused the obesity epidemic by reducing our national fat intake has more holes in it than Swiss cheese on baguette.
Tweet

Share on Tumblr

Stephan Guyenet's Blog
- Stephan Guyenet's profile
- 40 followers



