Stephan Guyenet's Blog, page 2
February 20, 2018
The second NuSI-funded diet trial has arrived
I’ve been eagerly awaiting this study. It was a 12-month randomized controlled trial comparing non-calorie-restricted low-fat and low-carbohydrate diets. Both diets placed a major emphasis on diet quality. I’m not going to review the findings in detail because Examine.com has already beat me to it. But here are some highlights:
Participants achieved large differences in fat and carbohydrate intake for the duration of the 12-month trial, although the difference narrowed somewhat over time (as it does in every diet trial).
The first primary (most important) outcome was about insulin. Genes influencing meal-related insulin secretion were unrelated to a person’s response to the low-fat or low-carbohydrate diets. [Correction 2/21/18: These genes aren’t directly related to insulin; they’re more closely related to fat metabolism and previous preliminary evidence suggested they might impact the response to low-fat/carbohydrate diets]
The second primary outcome was also about insulin. A person’s baseline insulin response to carbohydrate was unrelated to his/her weight loss response to the low-fat or low-carbohydrate diets.
Both diets caused similar weight and fat loss at 12 months (-5.3 kg [-12 lb] for LF vs. -6.0 kg [-13 lb] for LC). These are better 12-month results than most diet trials.
Here are a few reasons why this study is a big deal:
It was funded by the Nutrition Science Initiative, a nonprofit involving Gary Taubes that has been funding additional research to test the carbohydrate-insulin hypothesis of obesity. This is the second of three studies NuSI has funded. The first study showed that a very-low-carbohydrate ketogenic diet doesn’t accelerate fat loss or meaningfully increase metabolic rate relative to a high-carbohydrate, high-sugar diet of equal calories and protein, despite large differences in insulin levels (implying that ketogenic diets promote weight loss by causing people to spontaneously eat fewer calories). So far, these studies are doing a remarkably effective job of further refuting the carbohydrate-insulin hypothesis.
It was large and well-designed. In included 609 people and the research plan was registered in advance, including which outcomes would be the most important (primary). This guarantees that the researchers couldn’t tweak the methods after the fact or use selective outcome reporting to obtain a preferred outcome.
It didn’t involve deliberate calorie restriction in either group. One of the (valid) complaints of the low-carbohydrate community is that in randomized trials, non-calorie-restricted low-carbohydrate diets are often compared with calorie-restricted low-fat diets. Some have speculated that if low-fat dieters were allowed to eat until full rather than controlling portion size, they wouldn’t lose weight, and they might even gain. This is not the case.
It focused on diet quality in both groups. All participants were told to focus on unrefined foods and cook at home whenever possible. This is in contrast to the wimpy low-fat control groups in many randomized trials of low-carbohydrate diets, which I call the “Snackwell diet”.
One typical (somewhat valid) critique about randomized trials like this is that the low-fat diet contained too much fat, or the low-carbohydrate diet contained too much carbohydrate. In this study, both arms were started on very-low-fat (20 g/d) or very-low-carbohydrate (20g/d) diets, and told that they should keep fat/carbohydrate to the lowest level they can sustainably maintain. While it is true that fat and carbohydrate intake rose throughout the 12-month period, this isn’t an indictment of the study: It’s a fact about human nature. This trial showed that even with extensive support, the average person is unable to stick with a very-low-fat or very-low-carbohydrate diet. It is true that they probably would have seen better results on both diets if they had been able to stick with a greater degree of restriction, but the participants demonstrated with their forks that it wasn’t sustainable for them.
Sugar intake declined substantially in both groups, although more in the low-carbohydrate group. I predict that those who are constitutionally unwilling to give up the insulin hypothesis will focus on this as a way to discount the results. Please allow me to inoculate you against this weak argument with the following facts:
Sugar has little impact on insulin levels relative to other types of carbohydrate unless it’s consumed in unusually large amounts.
High sugar intake doesn’t seem to impair weight loss, both in settings where calories are strictly controlled, and in settings where they aren’t.
Sugar probably does contribute to obesity, but the evidence suggests it’s very unlikely to be the primary driver of changes in body fatness. I have no illusions that this study will change the minds of the diehards, but I do expect it to impact everyone else.
Tweet

Share on Tumblr

February 2, 2018
The new Ideal Weight Program
 A slide from the Simple Food Diet course
A slide from the Simple Food Diet courseMy book, The Hungry Brain, covers the science of eating behavior and body fatness and offers some tools for putting that evidence into practice. Yet The Hungry Brain isn’t really a weight loss book because it’s more focused on understanding body fatness than on doing something about it. The practical arm of my work is the Ideal Weight Program, a web-based weight management system that I co-designed with Dan Pardi, a researcher and the CEO of HumanOS. I haven’t talked about it much over the last few years because we’ve been working on a major upgrade. As is often the case, it took longer than anticipated.
That work is now complete and I’m happy to announce a new, much-improved version of the Ideal Weight Program. As before, the program focuses on creating and maintaining awareness of key weight-related behaviors through education, tracking, and feedback. Yet the new version delivers many upgrades:
Free weight insight score. This questionnaire helps you gain insight into the weight-related behaviors that are holding you back from your goals, and which changes may benefit you the most. It’s available to anyone, free of charge. Results are instant and you don’t have to provide your email address to receive them.
The Ideal Weight Program is now course-based. That means it’s divided into courses and lessons with corresponding mini-quizzes. This low-stakes grading system increases engagement and the retention of information.
Aesthetic upgrades. We worked with professional designers to create clear, beautiful content. The program looks much more appealing than the last version.
A greater focus on weight maintenance. I felt that the last version of the Ideal Weight Program didn’t offer enough support for weight maintenance– an important goal for many people. In the new version, we’ve fleshed out our Lean Maintenance Diet, which is a Mediterranean diet modified for weight control. Most of the courses in the current version apply to weight loss and maintenance equally. The Ideal Weight Program is now a good value even if weight maintenance is your only goal.
The Ideal Weight Program dovetails seamlessly with The Hungry Brain, particularly chapter 11.
 A slide from the appetite course
A slide from the appetite courseThe Ideal Weight Program is now part of the HumanOS platform, which is a greatly improved version of the former Dan’s Plan platform. We’ve also switched over to a subscription model in which subscribers pay a monthly fee for access to all courses on the HumanOS platform, including the Ideal Weight Program (people who previously purchased the Ideal Weight Program will maintain lifetime access to the program with no monthly fee).
HumanOS offers many great courses and the number is growing–take a look!
Tweet

Share on Tumblr

January 20, 2018
Reflections on the US News & World Report diet rankings, and my involvement in them
Each year, US News & World Report publishes diet rankings based on the opinions of a panel of experts. This year, I served on the panel. In this post, I’ll discuss my general thoughts on the rankings, as well as the fact that the popular ketogenic diet tied for last place among the 40 diets.
The process
Here’s how it works. US News staff summarizes information on each diet– including the diet’s recommendations and what current evidence says about its effectiveness– and provides it to a panel of expert reviewers. This is the same information that is publicly available on each diet’s US News webpage. It’s not perfect but they appear to put in a good faith effort, and they ask reviewers to recommend corrections if anything seems off. On the basis of this information, as well as the reviewers’ existing knowledge and optional literature searches, reviewers are asked to rate the diets in a number of different ways on a scale of 1-5. These scores are then compiled into four areas that are shared with the public:
How effective is it for short-term weight loss?
How effective is it for long-term weight loss?
How easy is it to follow?
How well does it support general health?
Note that these “diets” also often include lifestyle modification advice, such as physical activity, and these are considered in the scoring. US News also provides an overall score for each diet, which I suspect is an average of the four scores above.
General thoughts
The diet ranking system is necessarily an imperfect process. With 40 diets to review and rank, there isn’t enough time to do comprehensive literature reviews to get the best possible picture of effectiveness for each diet. This less-than-comprehensive approach leaves a certain amount of room for uninformed opinions to substitute for evidence, particularly in areas of evidence that reviewers may not be very familiar with. Still, the information it provides should be more helpful for selecting diets than the current alternatives, like reading Amazon reviews, Googling, or asking your aunt Martha.
The review panel includes people with a diversity of backgrounds, and they don’t agree on everything. This is probably by design. I often agree with the opinions of the rest of the panel, but there are also a number of places where I disagree. I’ll discuss a few of those below. I want to emphasize that the point of the exercise is not for everyone to agree.
For the first time, the Mediterranean diet secured the top spot for best diet overall, tied with the DASH diet. I think this is appropriate. The science of nutrition and chronic disease is complex and uncertain, but in my opinion the Mediterranean diet has more convincing evidence supporting its efficacy for general health than any other diet. It’s also relatively easy to follow, which supports long-term compliance.
However, it’s not really a weight loss diet and there is very little evidence that it causes weight loss as typically applied. Hence, I’m confused about why other reviewers rated it as an effective weight loss diet, especially in the long run. I suspect this has to do with two factors. First, a well-known randomized trial by Shai and colleagues found that a calorie-restricted Mediterranean diet caused weight loss that was similar to a low-carbohydrate diet, and superior to a moderate low-fat diet, over a two-year period (1). Four years after the end of the study (6 years total), people who had been assigned to the Mediterranean diet were maintaining their weight loss better than people who had been assigned the other two diets (2). Second, human nature. When we like something in general, that favorable opinion tends to color our view of more granular aspects of it, even if it isn’t deserved.
I think that if you adopt a standard Mediterranean eating pattern that doesn’t involve calorie restriction, you may lose some weight depending on what diet you’re coming from, but probably not much. I do think the diet shows promise for the long-term maintenance of lost weight, as suggested by the Shai trial.
This issue came up in a few other places as well. For example, the vegetarian diet was ranked fairly well for weight loss. This view seems to be based on observational studies showing that vegetarians tend to be leaner than their meat-eating counterparts. Yet there is little direct evidence that vegetarian diets promote meaningful weight loss, and if you expect to lose a substantial amount of weight just by cutting meat out of your diet, you’re probably going to be disappointed.
The ketogenic diet
The ketogenic diet is a very-low-carbohydrate, high-fat, moderate-protein eating style that forces the body to run almost entirely on fat for fuel. It’s extremely popular right now. Although the popularity of individual diets waxes and wanes, I tend to think that there is usually a nugget of truth underneath the hype.
The ketogenic diet limped in to last place in the rankings, tied with the Dukan diet (a high-protein, low-carb/fat rapid weight loss diet). It was rated by the panel as fairly effective for short-term weight loss, not very effective for long-term weight loss, very unhealthy, and very difficult to follow. Unsurprisingly given its popularity, the snub was not well received by ketogenic diet fans.
I don’t remember exactly how I rated it myself, but here’s the gist of it. I think very-low-carbohydrate diets like the ketogenic diet are some of the more effective diets for short-term weight loss– although no diet is a silver bullet (3, 4, 5, 6). Ketogenic diets also cause weight loss in animal models under tightly controlled conditions (7, 8, 9). I don’t know how effective it is for long-term weight loss and the evidence in humans doesn’t seem very informative to me, but I seriously doubt it’s less effective than diets like Mediterranean and vegetarian that aren’t even weight loss diets (10). In general, my observation is that the more extreme you are on the carbohydrate:fat continuum, the more a diet tends to promote appetite control and weight loss. Very low-carbohdyrate and very low-fat diets both tend to be more effective for weight loss than their more moderate counterparts, and I suspect this also applies in the long run, at least to some extent. This is supported by animal research, which mostly seems to suggest that ketogenic diets can curtail long-term body fat gain (11, 12, 13).
I probably gave it a 2 or a 3 out of 5 in health, assuming that someone is coming from a typical unhealthy diet. The primary reason for this mediocre score is simply that its long-term effects on human health aren’t well known. I can’t really say that ketogenic diets are unhealthy in the long run, but I also can’t say they’re healthy, and that uncertainty makes me feel wary. This concern is compounded by the fact that (to my knowledge) no traditionally-living human population has ever been shown to exist in a state of chronic ketosis, which the diet promotes. Even the arctic Inuit, who traditionally eat a high-fat, low-carbohdyrate diet, were not in chronic ketosis, and the reason is rather troubling for ketogenic dieters: A genetic mutation preventing ketone production spread rapidly throughout the ancestral Inuit population, suggesting that avoiding ketone production conferred a powerful survival advantage (14). Furthermore, few of the people reading this are descended from Inuit and their genomes weren’t shaped by thousands of years of eating the Inuit diet. The vast majority of traditional diets that have been documented contain enough carbohydrate and/or protein to prevent ketosis, although the amount of carbohydrate varies greatly (15). Long-term nutritional ketosis doesn’t appear to be part of the ancestral human metabolic spectrum. Contrary to popular belief, it is probably not Paleo or ancestral. Shouldn’t that worry us a little?
The animal research on the health impacts of the ketogenic diet is a mixed bag. The diet usually prevents weight gain and its effects on lifespan are either neutral or beneficial in mice, which is reassuring (16, 17). However, it tends to cause fat accumulation and inflammation/injury in the liver and other tissues (18, 19, 20, 21, 22). Its effects on insulin sensitivity in animal models are inconsistent between studies. Rodents don’t naturally develop human-like cardiovascular disease, so they can’t help us understand the diet’s long-term impacts on the heart and blood vessels.
That said, we do have multiple randomized trials of very-low-carbohydrate diets, and they have generally found little evidence of harm, and some evidence of benefit, in people who have obesity and/or diabetes in the short-to-medium term (23, 24, 25). About the worst we can say is that they don’t lower “bad” LDL cholesterol as much as other diets. These findings make it seem less likely that the long-term effects are catastrophic. It’s also hard to deny that some people appear to benefit from the diet– particularly people with blood glucose control problems such as diabetes. If the alternative is having poorly controlled blood glucose, using blood glucose-suppressing drugs, and injecting insulin, I can see how a very-low-carbohydrate diet would start to make sense. We still need studies on whether the diet can prevent the complications of diabetes such as heart attacks. For people who are overweight, have blood glucose control issues, and who react well to it, very-low carbohydrate diets seem like a viable option and they don’t appear to cause obvious harm. We still have uncertainty about the long-term effects of such a diet, but given the alternatives I don’t think it’s unreasonable to try it.
Let’s be honest though– most people can’t stick with it. I agree with the other reviewers on this. The more extreme a diet, the harder it is to adhere to, and the ketogenic diet is extreme. “But wait”, you say, “I’ve been on the ketogenic diet for five years and it’s easy!” That may be true, but randomized controlled trials don’t lie. The average person can’t even stick with the diet for six months, as judged by urinary ketone levels (26, 27). The minority of people who find it easy, get good results, and stick with it are the ones who write about it on the Internet.
For the record, I’m not against the ketogenic diet and I doubt it’s a health disaster for people who tolerate it well. I do think people who adopt it should be aware of the uncertainty about its long-term effects. As with any extreme diet, it has strengths and weaknesses and it’s probably best viewed as a medical intervention akin to drugs and surgery, rather than a tool for supporting general health. I think it’s interesting enough that it deserves further research, particularly in the setting of diabetes.
Tweet

Share on Tumblr

January 5, 2018
Interesting new genetic study on insulin secretion and body mass
A new study uses a powerful genetic tool called Mendelian randomization to examine the relationship between meal-related insulin secretion and body mass. The results suggest that gene variants that increase post-meal insulin release may modestly increase body mass. Upon close examination, the findings do not appear to support the hypothesis that insulin is the primary driver of obesity, but they may nevertheless provide a foot in the door for insulin.
Earlier this week, I received a number of messages from people who asked for my opinion of this study. Here it is.
 Most people agree that bagels are fattening, but not everyone agrees on why.
Most people agree that bagels are fattening, but not everyone agrees on why.The study
The study was published in the journal Clinical Chemistry and was conducted primarily by researchers at Harvard medical school, including David Ludwig, MD, PhD, who is a middle author (1).* Ludwig has been a vocal proponent of the carbohydrate-insulin hypothesis of obesity, which posits that the primary cause of obesity is the ability of refined carbohydrate to raise insulin levels, trapping fat inside fat cells and leading to fat gain and excess hunger.
To understand the study, we first need to understand the technique it applies, called Mendelian randomization (MR). The concept behind MR is that nature randomly assigns gene variants within a population, similar to how a researcher would randomly assign people to treatment or placebo groups in a randomized controlled trial. This randomization process ensures that the variable of interest is not systematically associated with confounding factors, allowing us to say something about cause-effect relationships. If we know how specific gene variants impact some trait of interest, in theory we have a pretty clean experiment that tells us about how that trait impacts related outcomes.
Let me give you an example. The scientific community, including myself, believes LDL cholesterol level impacts heart attack risk. LDL cholesterol levels are partially genetic, and we have identified multiple gene variants that impact LDL cholesterol level. Using this information, researchers can see if gene variants that decrease LDL cholesterol are associated with lower cardiovascular risk (and vice versa). If they consistently are, this provides evidence that LDL cholesterol level contributes to cardiovascular disease risk. As it turns out, LDL-decreasing variants are associated with lower cardiovascular risk, supporting the hypothesis (2).
In the current paper, the researchers applied this technique to the relationship between post-meal insulin secretion and body mass index (BMI), a measure of weight for height that correlates with body fatness. Using large sets of human genetic data, they asked whether people who have gene variants that cause greater post-meal insulin secretion also tend to have a higher BMI. As their measure of post-meal insulin, they used insulin measurements taken from volunteers 30 minutes after they had consumed a glucose (sugar) drink.
The study did not have a preregistered research plan, meaning that we cannot be confident that researchers did not tweak the data analysis plan partway through to achieve a desired result, whether intentionally or unintentionally. To be clear, I’m not suggesting that the authors did so, only pointing out that they did not take the opportunity to prove that they didn’t engage in this common practice.
The results
The authors used three different groups of gene variants to estimate the impact of post-meal insulin release on BMI (insulin-30 stringent, GSIS stringent, and insulin-30 relaxed), and they tested them in two large genetic data sets (GIANT and UK Biobank). The key result is below:
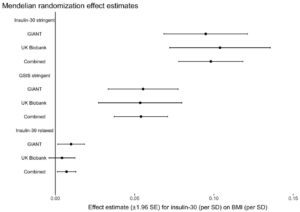
What this graph shows is that depending on the model used, one standard deviation higher post-meal insulin was associated with between about 0.01 and 0.1 standard deviation higher BMI, and this was statistically significant for most models. If I understand this correctly, roughly speaking it suggests that variation in post-meal insulin secretion explains between 1 and 10 percent of variation in BMI. About half of the larger estimate was driven by a single location of genetic variation, QPCTL/GIPR.
They then used the same method to test the reverse hypothesis– that BMI impacts meal-related insulin secretion– and did not find evidence for it, offering an argument that the previous association was not due to reverse causality.
Discussion
This study does provide evidence for a causal role of post-meal insulin release in BMI. However, before we get too carried away, we have to consider a few caveats and place the finding in the context of the rest of the scientific literature. Caveats:
The effect size is much smaller than carbohydrate-insulin proponents generally predict. Depending on the model, post-meal insulin explains between 1 and 10 percent of BMI differences, leaving 90-99 percent unexplained by insulin. This is not consistent with insulin being a major driver of obesity, although it does get insulin’s foot in the door.
The study measured BMI but did not directly measure body composition. We don’t know how much of the weight differences are fat, and how much are lean tissue. I would be less concerned about this if the effect size were large, because large differences in BMI are unlikely to be due to lean mass.
The regulation of glucose, insulin, and body fatness by the brain are closely related to one another (3). Since genes that are involved in one process are often involved in the other as well, it may not be possible to separate the two functions in a genetic analysis like this, meaning that the results could be (unintentionally) misleading. Although the authors tested for this possibility, they acknowledge that due to the inherent limitations of their data set, the test may not be very informative.**
Post-meal insulin secretion is associated with other physiological traits (possibly including leptin resistance***) that may also be influenced by the same gene variants in their models. It’s not clear that insulin itself is the variable impacting BMI, rather than another physiological variable associated with it.
When considered in the context of the rest of the literature, the current study’s finding is somewhat puzzling. For example, another recent MR study suggested that higher fasting insulin does not increase BMI, but higher BMI does increase fasting insulin (4). This result is basically the opposite of what the current study reported, but with fasting insulin swapped in for post-meal insulin. The authors of the current study suggest that the results differ because fasting insulin is simply a marker of insulin resistance, whereas post-meal insulin is a marker of insulin signaling exposure. This explanation doesn’t make much sense, for the following reasons:
Both fasting and post-meal insulin are strong markers of insulin resistance. If a person is insulin resistant, he will generally have higher fasting and post-meal insulin levels. As a matter of fact, the insulin response to a glucose drink is commonly used as part of a formula to estimate insulin resistance (5).
Fasting and post-meal insulin are correlated and respond to diet in concert. The amount of carbohydrate in the diet impacts both fasting and post-meal insulin. When calorie intake is matched, low-carbohydrate diets lead to lower fasting insulin in addition to lower meal-related insulin release (6).
So we are left with the puzzling fact that in the current MR study, insulin seemed to impact BMI, while in the previous study, it didn’t. I don’t know how to reconcile these two findings, and the authors’ explanation doesn’t do it for me.
Another puzzling thing about this study is the finding that BMI does not impact post-meal insulin release. The reason this is puzzling is that previous evidence shows unequivocally that it does! Check out this graph of post-glucose insulin before and after 4.5 months of moderate overfeeding (7). The closed circles are before, and the open circles are after:
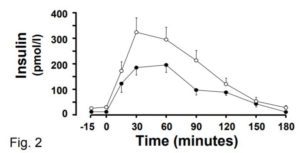
At the 30 minute time point (the one used in the current MR study), insulin secretion has nearly doubled, and this is after a modest weight increase of 2 BMI points. The fact that the current MR study did not observe this robust effect raises questions about how effective their method is at identifying cause-effect relationships in this domain.
Finally, carbohydrate-insulin advocates are using the current paper’s findings to support their larger hypothesis about the causes of obesity. However, there are still very good reasons to believe this larger hypothesis is incorrect, at least in its most prominent incarnation:
Ludwig’s own controlled trial suggests that a low-glycemic diet causes weight loss that is virtually identical to a high-glycemic low-fat diet, despite large differences in insulin secretion (8). This is consistent with the null findings of the longest and best-controlled diet trial of glycemic index I’m aware of, conducted by one of Ludwig’s colleagues at Harvard (9).
A 2016 study continues to be devastating to the idea that inhibiting the release of fat from fat cells increases hunger and body fatness (10). In a randomized trial, researchers gave volunteers with obesity a drug that substantially reduced fat release from fat cells, or placebo, for six months. No differences in calorie intake, macronutrient intake, metabolic rate, body weight, or body composition emerged.
The total rate of release of fat from fat tissue in people with obesity is higher than in lean people, not lower (11). Neither insulin nor anything else is trapping fat inside the fat tissue of people with obesity, making it hard to understand how obesity could be caused by this mechanism.
Rodents release insulin when they eat carbohydrate like humans, and their fat cells respond to insulin in the same way as humans. Yet diets that are predominantly fat tend to be more fattening in rodents than diets that are predominantly refined carbohydrate or sugar (12, 13). In fact, sugar is not very fattening at all in rodents, even at high levels. In every way that is relevant to the carbohydrate-insulin hypothesis, rodents and humans are constructed similarly, so why do rodents not respond to diet in the manner predicted by the hypothesis even under tightly controlled conditions?
Liraglutide is a weight loss drug that mimics the hormone GLP-1. This drug was originally developed as a diabetes treatment because it stimulates insulin release, yet it was extended to obesity therapy because it substantially reduces body weight and fat (14, 15). It also improves metabolic health (16). The increase in insulin is probably not the reason why fat loss occurs, but it certainly doesn’t prevent it.
Based on these results and others, I still feel fairly confident that the carbohydrate-insulin hypothesis as formulated by Ludwig and other public advocates is not correct. But could some version of an insulin hypothesis be correct? Perhaps. The current study offers the most persuasive evidence I’ve seen so far that insulin does impact body fatness, even if only modestly. It is consistent with a model whereby multiple factors, including post-meal insulin release, determine body fatness. If the effect of insulin is small, this may explain why it’s hard to detect in other study designs such as controlled trials of low-glycemic diets. It may also imply that the effect is of little practical relevance.
Due to the caveats I discussed, I’m not ready to endorse this model yet. I’ll need to see the finding replicated independently before placing greater emphasis on it. But this study has put a foot in the door for a model of obesity that includes post-meal insulin secretion, and I’ll endorse it if future research continues to support it persuasively.
* I’m not certain what role Ludwig played in the study, but some of the language and citations in the introduction are characteristic of his writing.
** “The Egger test was not statistically significant for any of the analyses, although this test is not well-powered and may not be valid in the context of substantial heterogeneity and/or violations of the InSIDE assumption.”
*** Higher post-meal insulin release is a marker of insulin resistance, and insulin and leptin resistance tend to be associated (and likely caused by overlapping mechanisms). I would guess that people with higher post-meal insulin release are also more likely to be leptin resistant.
Tweet

Share on Tumblr

October 13, 2017
Obesity prevalence continues to increase in the US
The Centers for Disease Control provides the most accurate estimates of obesity prevalence in the US, based on National Health and Nutrition Examination Survey (NHANES) data. They just released data for the 2015-2016 survey period, and it doesn’t look good.
Since the turn of the 21st century, it has looked like the rate of increase of obesity prevalence is slowing. Many of us were hoping that it would plateau, and perhaps eventually decline. Yet the latest NHANES data show that obesity has been increasing at its maximum historical rate since 2011 in both adults and youths, and is now 39.8 percent in adults, 13.9 percent in children age 2-5, 18.4 percent in children 6-11, and 20.6 percent in adolescents 12-19.
Since the CDC release doesn’t provide a graph showing obesity prevalence over the whole history of NHANES surveys, I’ve created my own:
 Data from NHANES and NHES surveys. Prepared by Stephan Guyenet.
Data from NHANES and NHES surveys. Prepared by Stephan Guyenet.
Since 1961, the prevalence of obesity in US adults has increased by 2.95-fold. According to recent research, the lifetime risk of obesity in the US is greater than 50 percent, meaning that most people will have obesity at some point in life. This is a very serious public health problem and I believe we need to get serious about addressing it. As I explained in the last chapter of my book, our efforts thus far have been halfhearted, largely due to the congenital aversion of US citizens, politicians, and industry executives to further regulation of the food system.
Tweet

Share on Tumblr

October 3, 2017
Where the praties grow: My seven-day potato diet experiment
I recently finished the book Potato: A history of the propitious esculent. In it, John Reader takes his audience on a meandering tour of the potato’s history, ranging from academic explanations of the potato’s role in early industrial labor markets to folksy accounts of his time living in rural Western Ireland. I quite enjoyed it.
One of the things that fascinates me about potatoes is their nutritional near-completeness. Cultures in the Andes subsisted mostly on potatoes for thousands of years, building vast civilizations, and the Aymara and Quechua still eat such a diet today. In 18th and 19th century Ireland, the average person’s diet consisted almost exclusively of potatoes, often with the buttermilk that was left over after butter was sold for income. Despite abject poverty due to crushing oppression by the English, by all accounts the Irish during this time were in excellent health and had the highest fertility rate in all of Europe. On page 157 of the paperback, Reader quotes farmer and Royal Society fellow Arthur Young, who conducted a survey of Irish agriculture in 1776-9:
I have heard [the potato] stigmatized as being unhealthy, and not sufficiently nourishing for the support of hard labour; but this opinion is very amazing in a country, many of whose poor people are as athletic in their form, as robust, and as capable of enduring labour as any upon earth. When I see the people of a country, in spite of political oppression, with well-formed vigorous bodies, and their cottages swarming with children; when I see their men athletic and their women beautiful, I know not how to believe them subsisting on an unwholesome food.
From page 148:
The population of Ireland more than doubled between 1687 and 1791, rising from 2.16 million to 4.75 million. During the fifty years from 1791 to 1841 another 3.4 million were added, taking the population to 8.15 million. Another 1.75 million emigrated to North America, Scotland, England and even Australia during the same period, which brings the total born in Ireland to nearly 10 million — almost a five-fold increase in 154 years (1687 to 1841). ‘Probably in no other western country has so rapid a rate of natural increase been so long sustained,’ writes the historian Kenneth H. Connell.
This book, coupled with a few other influences, inspired me to try a mostly-potato diet for a week. This inspiration happened to coincide with our recent harvest of 1,500 pounds of potatoes from a garden we share with another couple. Here’s a photo of our largest potato, a freshly unearthed Cal White that weighed nearly four pounds:
 We’re proud parents of this baby-sized potato.
We’re proud parents of this baby-sized potato.This potato would have flabbergasted farmers in 18th-century Ireland, where a four-inch diameter potato was considered unusually large (p. 148).
My wife and I chose to eat a slightly more affluent version of the 18th/19th-century Irish diet: baked or microwaved potatoes, homemade whole milk yogurt, and salt to taste. We also supplemented dinner with a portion of vegetables tossed in a little olive oil or vinaigrette. I occasionally had a snack of dried fruit, and one day I had a non-potato lunch with a friend.
This resulted in a diet that was higher in carbohydrate and lower in fat than my typical fare, and also very low in reward value. I knew it would be hard to eat enough calories so I made an effort to stuff as much down as possible.
The first few days were, honestly, rough. Although I wasn’t hungry, I felt mentally foggy and shaky between meals, which eating a bit would correct. My exercise tolerance was terrible and I had to scale back my cycling and strength training routine. My wife felt the same way. Interestingly, this reminds me of a phenomenon people talk about called the “low-carb flu”. I’ve never experienced this, but many people report that in the initial adjustment period to a very-low-carbohydrate diet, they feel foggy, tired, cranky, and have low exercise tolerance. I wasn’t expecting this to happen with potatoes, but perhaps it occurs whenever the body has to adjust to a substantially different macronutrient composition.
As the week went on, I gradually felt better, and by day five I was no longer feeling foggy or shaky between meals and my exercise tolerance had bounced back. In fact, on day five I went for a jog and ran faster, and with less effort, than I can remember running in a long time. My wife also felt better as the week progressed.
After a few days on the diet, non-potato foods began to taste fabulous. I always enjoy fresh vegetables from my garden, but while I was on the potato diet, simple tomato or lettuce salads with vinaigrette dressing were delectable. Despite that, potatoes and yogurt never became unappealing. The diet was certainly monotonous, but not unpleasant.
My weight was stable over the course of the week, and my digestion was brisk. I experienced very little hunger between meals. The experiment would have been more informative if I had continued for longer, but it would have been challenging for social reasons and I didn’t have a compelling reason to do so.
In parting, I’ll leave you with these verses from a traditional Irish folk song, as printed in Potato (page 151):
Says I, ‘My lovely darling I’m tired of single life
And if you’ve no objections I will make you my sweet wife’.
Says she, ‘I’ll ask my parents and tomorrow you shall know
If you’ll meet me in the garden where the praties grow’.
Her parents they consented and we’re blessed with children three
Two girls just like their mother and a boy the image of me.
We’ll train them up in decency the way they ought to go
And I’ll ne’er forget the garden where the praties grow.
Tweet

Share on Tumblr

September 19, 2017
The hungry brain in the 21st century: Challenges and opportunities for health
On October 12, I’ll be speaking at the Evolutionary Nutrition conference and Staffan Lindeberg memorial in Lisbon, Portugal. I was asked to write a one-page abstract of my talk, which I have reproduced below.
The world is undergoing a striking transformation of health and demographics that has been called the “epidemiologic transition”. This term was coined by Abdel R. Omran in 1971, who wrote “During the transition, a long-term shift occurs in mortality and disease patterns whereby pandemics of infection are gradually displaced by degenerative and man-made diseases as the chief form of morbidity and primary cause of death.” It has been forty-six years since Omran wrote these words, yet our ever-expending evidence base continues to support his hypothesis.
Most notably, the Global Burden of Disease project has documented that people in low-income countries continue to die primarily of infectious diseases, accidents, and violence. These are the scourges of our ancestors. In contrast, people in high-income countries have mostly overcome the threat of infectious disease, accidents, and violence, yet we face a new set of scourges: Omran’s “man-made diseases”, more commonly called noncommunicable diseases. These include obesity, diabetes, coronary heart disease, stroke, most heart failure, kidney failure, gout, some cancers, and many more. Although overall mortality is falling as global economic development proceeds, many people in affluent nations live with debilitating noncommunicable diseases that limit their potential for health and well-being. And low-income countries are severely affected by epidemics of noncommunicable disease as they rise to greater affluence.
Studies of traditionally-living cultures suggest that most common noncommunicable diseases, such as obesity and severe coronary heart disease, are evolutionary mismatch disorders, meaning that they result from poor compatibility between our ancient genomes and the modern industrial diet and lifestyle. Yet what is the nature of this mismatch? It is undoubtedly complex, however I will argue that one element of it is as simple as it is influential: Energy excess. Consuming more energy than one expends is well-established to cause obesity, yet evidence also strongly suggests that energy excess is the primary nongenetic cause of type 2 diabetes, and an important contributor to cardiovascular disease, certain cancers, orthopedic problems, and many other common ailments.
To understand why we engage in behaviors that lead us to energy excess, we must first acknowledge that the brain is the source of all behavior, that it evolved in a specific range of contexts, and that the inclinations we have today are a result of that process. Our ancestors evolved in a context in which they had to acquire energy from an environment that does not easily give it up. As a result, they developed learning and motivation systems that attempt to maximize their energy return rate by seeking calorie-dense foods that require the least time and effort to obtain, and avoiding unnecessary physical activity energy expenditure. In affluent countries today, nonconscious brain circuits continue to implement the rules of this obsolete survival game, and they drive most of us to energy excess. They are extremely persuasive due to the key role they played in the reproductive success of our ancestors, explaining why most of us overconsume food despite understanding the serious long-term consequences.
How do we solve the problem of energy excess when it emerges from human nature itself? I propose that instead of fighting the nonconscious brain circuits that drive our food intake, we understand them and provide them with diet and lifestyle cues that align them with our goals of leanness and health. In this way we may avoid exchanging the scourges of our ancestors for the scourges of modernity.
Tweet

Share on Tumblr

July 26, 2017
Why are some people “carboholics”?
In a recent editorial in the New York Times titled “Are You a Carboholic? Why Cutting Carbs Is So Tough”, Gary Taubes describes a phenomenon that is familiar to many of us (1):
The holidays and family vacations are a particular problem. Desserts and sweets, it seems, will appear after every lunch and dinner, and I’m not particularly good at saying no when everyone else is partaking. The more sweets I eat, the more we eat as a family, the longer it takes upon returning home before that expectation of a daily treat fades away.
What I’ve realized is that eating a little of a tasty dessert or a little pasta or bread fails to satisfy me. Rather it ignites a fierce craving for more, to eat it all and then some. I find it easier to avoid sugar, grains and starches entirely, rather than to try to eat them in moderation.
Like Taubes, I have a hard time controlling my intake of certain foods when they’re in front of me, and occasionally, I may continue to think about them for days after I eat them (chocolate-covered ice cream bars, I’m looking at you). Taubes goes on to provide his explanation: these foods elevate insulin levels, and that in turn increases cravings for carbohydrate-rich foods. Par for the course, he provides no evidence for this model other than a few quotes from Drs. Robert Lustig and David Ludwig, which are nothing more than personal speculation. I’m not aware of any research suggesting that high circulating insulin levels promote cravings for carbohydrate, sugar, or dessert foods, and I’m fairly certain those data don’t exist.
What Taubes may not be aware of is that there is no need to propose a speculative new explanation for why we crave desserts, because researchers have already provided an explanation that’s quite compelling. And it doesn’t involve insulin.
It starts with drugs
To understand why we crave food, sex, gambling, winning, catching fish, driving fast cars, playing video games, and everything else we crave in our lives, it’s helpful to start with drugs of abuse. This is because the way in which drugs create cravings is very simple, and we can consider it without burdening ourselves with all of our preconceived notions and feelings about food.
Habit-forming drugs, including drugs of abuse, are habit-forming because they stimulate the dopamine signaling pathway in the brain (2)*. This pathway determines your gut level of motivation for things– what we often call a craving. It evolved to motivate us to get food, water, sex, shelter, social status, and other things that were important for the reproductive success of our distant ancestors. So when a drug increases the level of dopamine in key structures of your brain, you will become more motivated to take the drug– you will crave it. This is called reinforcement.
Some drugs, like amphetamine and injected or smoked (crack) cocaine, are very good at increasing dopamine levels in the brain (3). This means they are also very good at increasing your motivation to take them. If you take the drug repeatedly and your level of motivation/craving crosses a certain threshold, your brain begins to implicitly prioritize drug-seeking behaviors over constructive behaviors like keeping a job and obeying the law. We call that addiction.
When a person with an addiction doesn’t use a drug for a long time, his craving for it will slowly subside. This is why a person who quits smoking will initially feel very strong cravings, but these will diminish to a low level over a period of months to years. Yet when that person exposes himself to the drug again, or cues associated with it– for example, by taking a puff of a cigarette– it often re-awakens those latent brain pathways and triggers a relapse into addictive behavior (4). This can leave a person struggling with strong cravings once again. Note that this abstinence -> cue -> relapse cycle is precisely what Taubes describes in his article, only for sweets instead of cigarettes.
Drug reinforcement and relapse behavior, of course, are not mediated by insulin. The drug goes straight to the brain and spikes dopamine– there is no pit stop in the pancreas. High background levels of circulating insulin are not known to exacerbate addictive behavior. I don’t think anyone believes that cravings and addictions to alcohol, gambling, sex, or video games are due to elevated insulin levels. Is food reinforcement the one exception?
Nope
We actually have a pretty good idea of how food reinforcement works, thanks in large part to the research of Anthony Sclafani, which I describe in more detail in my book. As with drugs, food reinforcement works by spiking dopamine in the brain, a fact that Taubes has come around to (5). The question is, how does food increase dopamine levels in the brain?
Research by Sclafani and others shows that food reinforcement primarily occurs when the upper small intestine detects carbohydrate, fat, and protein, causing a spike in brain dopamine levels (taste receptors in the mouth that detect sugars also contribute, to a lesser extent)** (6, 6b). Researchers can also spike brain dopamine and cause reinforcement by injecting glucose into the liver’s portal vein, but this finding has not been consistently replicated (7, 8). After performing multiple experiments and reviewing the evidence on the role of insulin in reinforcement, Sclafani’s group concluded that “these data do not suggest a primary role for insulin in glucose-based [reinforcement]” (9). Part of the reason why they came to this conclusion is evidence suggesting that “insulin may act in the brain to reduce sweet taste signaling and sugar activation of brain reward systems” (emphasis mine)(10, 11).
Furthermore, if insulin is responsible for spiking dopamine and ultimately food reinforcement, then dietary fat shouldn’t have the same effect because it causes less insulin release. Yet fat is highly reinforcing– a key fact that Taubes neglects to share with readers (12, 13, 14).
Essentially, the brain is wired to be motivated by the food properties that kept our distant ancestors alive and fertile***. When you eat food, the brain analyzes its composition via receptors in your mouth, upper small intestine, and perhaps liver that measure the amount of fat, sugar, starch, protein, and salt it contains. This all happens on a nonconscious level. If the brain “likes” what you just ate, it will release dopamine. The more fat, sugar, starch, protein, and salt your food contains (up to the “bliss point”), the more dopamine your brain releases. The more dopamine your brain releases, the more your cravings increase. This is why we crave cookies and bacon but not lentils and plain celery.
Foods that are skillful combinations of fat, sugar, starch, salt, and delightful flavors likely cause your brain to release high levels of dopamine, sometimes provoking addiction in susceptible people. And when a person excludes a problem food for a long time, then suddenly has it in front of them at the dinner table, those latent craving pathways are reactivated– just as they are for drugs. No insulin required.
I’m not aware of any evidence that insulin is involved in this process, or that chronically high insulin levels accentuate it, and available evidence suggests that insulin is probably not involved. Why propose this unsupported mechanism when we already have an evidence-based mechanism that makes far more sense?
What about fatoholics?
Taubes’s story breaks down further when we consider that many of the most common food cravings aren’t for sweet foods. Rob Markus and colleagues recently published a paper in which they identified the food types that are most commonly associated with addiction-like behavior (15). Here’s what they found:
The majority of respondents experienced these problems for combined high-fat savoury (30%) and high-fat sweet (25%) foods, whereas only a minority experienced such problems for low-fat/savoury (2%) and mainly sugar-containing foods (5%). Overweight correlated only with addictive-like problems for high-fat savoury and high-fat sweet foods (P < 0.0001), while this was not found for foods mainly containing sugar.
Wait, what? The primary foods that trigger addiction-like behaviors are “high-fat savory” foods that aren’t even sweet? And only one person out of twenty reported addiction-like behavior for “mainly sugar-containing” foods? It appears that fatoholics are more common than carboholics.
This lines up with my personal experience, and I suspect, the experience of most readers. I don’t know about you, but to me, hard candy just isn’t that appealing. I have no desire to eat fat-free frozen yogurt. Candy corn and Tootsie Rolls are barely better than starvation. Throw some fat into the mix, as in chocolate, ice cream, or brownies, and now you’re talking! Savory foods like potato chips, bacon, pizza, and ribs are also high on my list. Taubes doesn’t mention that the “desserts and sweets” that provoke his addiction-like behavior are probably also high in fat, tacitly assuming that only the sugar is relevant.
One thing that’s clear from reading Markus’s study is that different people find different foods “addictive”. Most people have a hard time controlling their eating behavior around certain high-fat savory and/or high-fat sweet foods. Yet a small minority have a hard time with low-fat savory foods like pasta or low-fat sweet foods like hard candy.
We’re all built differently, and we each have our own problem foods that drive us to overeat. It’s entirely possible that Taubes is wired to have an unusually strong reinforcement response to foods like bread, pasta, and fatty sweet desserts that are typical on American dinner tables, but not to high-fat savory foods. To him, the common denominator may seem like it’s carbohydrate, which is why the insulin explanation is so irresistible that even a total lack of evidence cannot restrain him from it.
So why are some people carboholics and fatoholics?
The reason is simple. The human brain is hard-wired to be motivated by calorie-dense foods rich in fat, sugar, starch, protein, and salt, because these things kept our distant ancestors alive and fertile in a difficult world. In the modern world, the food industry and home cooks are better at pushing our brain’s reinforcement buttons than ever before in history. Our distant ancestors didn’t have ice cream or pizza, and the brains we inherited from them may not be designed to constructively handle that kind of powerful reinforcement stimulus. We’re so good at pushing our own buttons that some of our modern foods probably provoke very high levels of dopamine release in the brain. Like drugs of abuse, those high levels of dopamine make us crave in ways that don’t always support our health– and sometimes lead to addiction. That’s why we crave dessert.
Due to individual differences in how we’re wired, some of us become “carboholics”, others become “fatoholics”, others become both, and still others become neither. We have much work to do before understanding these individual differences. Yet regardless of whether or not we have addiction-like eating behaviors, nearly all of us eat too much when we encounter foods that are highly reinforcing.
Postscript
I’m not surprised Taubes wrote this article, but I am surprised the New York Times published it. It might seem like fun and games to publish provocative speculation written by people who seem incapable of doing a Google Scholar search, but pieces like this can harm the public understanding of health science, with potentially serious consequences. How hard is it to run a piece like this by a few experts– people who are truly knowledgeable about the subject? Here are names: Anthony Sclafani, Karen Ackroff, Leann Birch, Roy Wise, Paul Kenny, Nora Volkow, Hisham Ziauddeen, Leonard Epstein, Jennifer Temple, Ashley Gearhardt, Stephen Benoit, Dianne Figlewicz, and Kent Berridge. As a reader and a scientist, can I please see some quality control?
* Typically by increasing dopamine levels, but also sometimes by acting on the same downstream pathway dopamine activates. For example, caffeine blocks the adenosine receptor, which increases dopamine’s action on downstream reward pathways.
** We don’t know what mechanism gets the signal from the intestine to the brain yet. Sclafani and Gary Schwartz found that cutting the nerves connecting to the small intestine doesn’t block reinforcement, suggesting that the signal may not be carried directly by nerves to the brain. Instead, it may be a factor released by the intestine into the bloodstream, but that remains to be demonstrated. This is a very important mechanism to understand because it’s so relevant to obesity. I suspect it won’t be too long before we get a toehold on it.
*** Sugar was obviously not the only nutrient that kept our distant ancestors alive, and from an engineering standpoint it would make no sense to design a system that is only motivated by sugar. That’s why our brains are strongly motivated by all concentrated sources of calories– including sugar.
Tweet

Share on Tumblr

July 19, 2017
Evolutionary Nutrition Conference and Staffan Lindeberg Memorial

On October 12 of this year, in Lisbon, Portugal, NutriScience is hosting a nutrition conference at which I’ll be speaking. The purpose of this conference is twofold: to bring together world experts on evolutionary nutrition, and to celebrate the life and work of Staffan Lindeberg, MD, PhD. The conference will be held in English and is for everyone who is interested in nutrition, health, and human evolution. Scroll down for details; register here.
I’ve been thinking about how to benefit the audience and honor Lindeberg. I’ll be touching on some of the themes of my book The Hungry Brain, but I’ll place that information in the broader context of modern global public health, tying it in to my recent work with the Open Philanthropy Project. I think Lindeberg would appreciate this big-picture view of global evolutionary health. Here are some questions my talk will address:
What are the primary challenges facing modern global health? What are the primary health burdens in affluent and low-income settings and how are they likely to change over time?
Do evolutionary mismatches (discrepancies between the environments we are genetically adapted to and the current environment) explain our primary health burdens?
What, exactly, is the nature of the evolutionary mismatches that drive poor health?
I think we can gain significant insight into our current predicament by merging the global health data produced by the World Health Organization and the Global Burden of Disease project with concepts from evolutionary biology, economics, and neuroscience.
If you’ve never been to Lisbon before, it’s a delightful place. The city is lovely and full of culture and good food. The cost of hotels and food are lower than in most large Western European cities. Hope to see you there!
SPEAKERS & MODERATORS
Prof. Loren Cordain (USA.), Prof. Lynda Frassetto (USA), Dr. Ainara Sistiaga (USA/Spain), Dr. Stephan Guyenet (USA), Prof. Frits Muskiet (Netherlands), Dr. Bodo Melnik (Germany), Maelán Fontes (Spain), Óscar Picazo (Spain), Dr. Tommy Jonsson (Sweden), Sérgio Veloso (Portugal), Pedro Carrera Bastos (Portugal), Dr. Csaba Tóth y Dr. Zsófia Clemens (Hungary).
DATE
12/October/2017
SCHEDULE
8h45 AM – 5h00 PM
LOCATION
InterContinental Lisbon Hotel, Rua Castilho 149
PROGRAM
08h45-9h00: Opening remarks (Prof. Lynda Frassetto)
09h00-9h30: Dietary shifts during human evolution (Dr. Ainara Sistiaga)
09h30-10h00: What does a modern Paleolithic diet look like (Prof. Loren Cordain)
10h00-10h15: Round table with Q & A (Moderator: Prof. Lynda Frassetto)
10h15-10h30: Short break
10h30-11h00: Poster session**
11h00-11h25: The Hungry Brain (Dr. Stephan Guyenet)
11h25-11h50: The land-water ecosystem in human brain evolution (Prof. Frits Muskiet)
11h50-12h15: Evolutionary perspective on milk signalling in adults (Dr. Bodo Melnik)
12h15-12h30: Round table with Q & A (Moderator: Pedro Bastos)
12h30-13h30: Lunch break
13h30-13h50: Clinical experience and research with the Paleolithic Ketogenic diet – 2010-2017 (Dr. Csaba Tóth and Dr. Zsófia Clemens)
13h50-14h10: Clinical research with modern Paleolithic diets – The known, unknown and unknowable (Maelán Fontes)
14h10-14h30: Cooking methods as confounders in dietary intervention studies (Óscar Picazo)
14h30-14h50: Beyond diet – lifestyle changes as confounders in nutrition research (Pedro Bastos)
14h50-15h10: Round table with Q & A (Moderator: Dr. Tommy Jonsson)
15h10-15h30: Short break
15h30-16h30: Round table with all the speakers and moderators – establishing future research directions (Moderator: Sérgio Veloso)
16h30-16h45: Closing remarks (Prof. Lynda Frassetto)
*This conference will be held in English.
Tweet

Share on Tumblr

June 20, 2017
The Hungry Brain book update
 The Hungry Brain has been available in the US for four and a half months now, and reactions are rolling in. Here’s a summary of what I’ve learned so far.
The Hungry Brain has been available in the US for four and a half months now, and reactions are rolling in. Here’s a summary of what I’ve learned so far.
Positive feedback
So far, I’ve received uniformly positive feedback from the research and medical communities. One of my primary goals was to accurately and clearly explain a broad swath of neuroscience and obesity research– much of which has never been available to a general audience– and it seems I’ve accomplished that.
After reading The Hungry Brain, my postdoc mentor Mike Schwartz told me it’s the best general-audience explanation of our field he has seen. That’s particularly significant because Schwartz is one of the primary architects of our field. The book also recently received its first review from a scientific journal, which wrote “This is an enthralling book which has lots of cutting-edge research… and is well written” (1). David Katz, director of the Yale University Prevention Research Center, wrote that it “provides an exceptionally complete understanding of why, despite the prevailing desire to be lean, so few of us are” (2). Alan Aragon, nutrition researcher and educator, called it an “awesome book” (3).
I attribute this positive reception from the scientific and medical community to two factors:
I made a good faith effort to understand the evidence from the most informed perspective possible, which is usually the perspective of the researchers themselves. To do that, I read hundreds of papers and interviewed 36 researchers directly. When a researcher’s perspective didn’t make sense to me, I corresponded with him/her and other experts and read papers until I felt the question was resolved (or difficult to resolve given current evidence). I also drew from my preexisting knowledge in the area, gained from 12 years of research experience in neuroscience and obesity.
I had subject-specific experts review the majority of the book before publication and I took their comments seriously.
Feedback from popular media and the general public has been very good as well. The Hungry Brain received a very good review from The New York Times, which called it “essential”, and an outstanding review from Publisher’s Weekly, which called it “a remarkable book” (4, 5). It also received a good review from the rationalist Scott Alexander (Slate Star Codex), who wrote “Not only does it provide the best introduction to nutrition I’ve ever seen, but it incidentally explains other neuroscience topics better than the books directly about them do” (6). The book currently has a 4.5 out of 5 star rating on Amazon.com.
In February, I accomplished one of my long-standing pipe dreams, which was to give a book talk at the Elliott Bay Book Company in Seattle. The talk had good turnout and was well received (thanks to all the locals who came out!).
To date and to my knowledge, none of the major scientific points in The Hungry Brain have been credibly refuted. That said, I don’t present the contents of the book as Immutable Scientific Truth. True scientific beliefs are probabilistic, meaning that there is some probability they will turn out to be wrong. Beliefs can be wrong either through limitations of the evidence or limitations of the person interpreting it, and I understand that neither the evidence nor I are infallible. I made an effort to convey uncertainty in the book when I thought it was appropriate.
Despite a very positive response overall, knowledgeable people have pointed out a few mistakes in the book. The most significant of these is on page 44 of the hardcover, where I use the term negative reinforcement rather than the correct term punishment (first pointed out by Sylvia Karasu– thank you). It’s an embarrassing mistake, but not one that undermines my point. If you find any mistakes, please pass them along– I may have the opportunity to correct them someday!
Negative feedback
No book will satisfy everyone, and that is true of The Hungry Brain. Negative feedback gives me an opportunity to learn about my audience and about the book market. The primary theme of the negative feedback I’ve seen is that some people wanted more of a practical focus and were frustrated that I didn’t present a simple, novel approach to weight control (some of the weight control strategies in the book are things I haven’t seen in other general-audience books, but most of them can be found elsewhere). You can see feedback like this on the book’s Amazon page.
I totally understand why people want me to distill weight control into one core idea and use that idea to deliver confident, simple, effective advice that they haven’t seen elsewhere. In all areas of our lives, we want the most benefit for the least effort– that’s human nature. Yet eating behavior and weight control can’t be shoehorned into one simple concept– that’s reality. Another part of the problem lies in the fact that The Hungry Brain isn’t a diet book. It does provide strategies for managing eating behavior and weight, and I believe those strategies are effective, but the primary focus of the book is on understanding why we overeat.
Furthermore, I think some readers are looking for a silver bullet that not only doesn’t exist in The Hungry Brain, but doesn’t exist anywhere. If there is a silver bullet for easy weight loss, no one has figured it out yet (the closest thing we have right now is bariatric surgery). The truth is that most people with obesity would rather be lean, and many of them go to great lengths to try to slim down, usually without substantial, lasting success. If there were a simple and easy solution, the US would not have an adult obesity rate of 38 percent. Yet due to the aforementioned human nature, we’re constantly on the lookout for that silver bullet. This is why people get swindled by an endless treadmill of ineffective quick fixes. There is a perverse incentive to tell people what they want to hear even if you can’t back it up.
I know I could have sold many more copies if The Hungry Brain had been about a new miracle cure for obesity, or about the one cause of obesity “they” don’t want you to know about (or both). I could easily have found a publisher happy to print all sorts of garbage with my PhD stamped on it, and popular media would have amplified my controversial claims. But I don’t have the stomach for that, and I also don’t have much incentive because writing isn’t my primary source of income.
The future of The Hungry Brain
I wrote The Hungry Brain for a very broad audience. My goal was to write a book that is accessible enough for a sophisticated general audience, but rigorous and informative enough to interest the research and medical communities–even those who are already knowledgeable about eating behavior and obesity. I realize that’s a lofty goal, but I think it’s possible, which is why I spent many long hours agonizing over how to present the concepts in a way that’s as easily digested as possible (using both text and professional medical illustrations). I’ve often been amazed at how much I can learn from a good book, even on a topic I know well.
My hope for the future is that the book will remain relevant and continue to appeal to a broad audience for many years. I hope it will continue to shift the global conversation on obesity in a more evidence-based direction, and help individuals understand themselves and find compassion for themselves. I would also love to see the book used in a classroom setting to teach topics related to neuroscience, eating behavior, and obesity.
Tweet

Share on Tumblr

Stephan Guyenet's Blog
- Stephan Guyenet's profile
- 40 followers



