Nelson Vergel's Blog, page 3
May 9, 2013
Variable Accuracy of Testosterone Concentrations in Compounded Testosterone Products
Accuracy of Testosterone Concentrations in Compounded Testosterone Products
Ethan Grober; Andrea Bozovic; Fanipour Majid; Vathany Kulasingam; Eleftherios Diamandis
Abstract: 1510
http://www.aua2013.org/program/plenary.cfm
Introduction and Objectives
Many patients with testosterone deficiency inquire about the use of compounded testosterone products as an option for testosterone replacement. The safety and accuracy of the active ingredients within these products is not well established. The current study evaluated the accuracy of the testosterone concentrations within testosterone gels and creams manufactured by compounding pharmacies.
Methods
Ten compounding pharmacies within Toronto with experience in compounding testosterone products were included in this study. All pharmacies were blinded as to the nature of the study. A standardized prescription for 50mg of compounded testosterone gel/cream applied once daily was presented to each pharmacy. Two independently compounded samples (batch 1 and 2) were analyzed from each of the 10 pharmacies 1 month apart. For quality control, several samples from each batch were tested. Testosterone concentrations in a 5g sachet of Androgel 1% (Abbott) and 5g tube of Testim 1% (Auxilium) were evaluated as controls. Samples were analyzed independently and in a blinded fashion by the Department of Laboratory Medicine at the University of Toronto. Measurement of testosterone concentration was performed using a modified liquid chromatography tandem mass spectrometry validated for serum testosterone. Results are reported as % testosterone recoved compared to the prescribed testosterone concentration.
Results
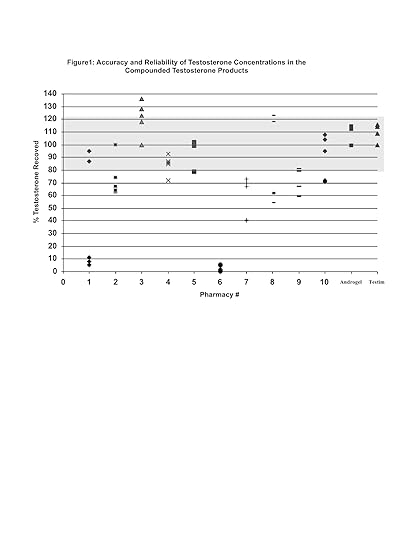
Compounded formulations included 7 gels and 3 creams with a volume/daily dose ranging from 0.2ml -1.25ml. Product cost ranged from $26 to $75 for a 7-day supply. There was significant variability both within and between pharmacies with respect to the measured concentration of testosterone in the compounded products (Figure 1). In contrast, the concentration of testosterone within Androgel and Testim was consistent and accurate. Collectively, only 50% (batch 1) and 30% (batch 2) of the compounding pharmacies provided a product with a testosterone concentration within /-20% of the prescribed dose. Two pharmacies compounded products with >20% of the prescribed dose. One pharmacy compounded a product with essentially no testosterone.
Conclusions
Testosterone concentrations in compounded testosterone products can be variable and potentially compromise the efficacy and safety of treatment.

Published on May 09, 2013 21:32
April 29, 2013
Testosterone Injections Helped Obese Men Lose Weight
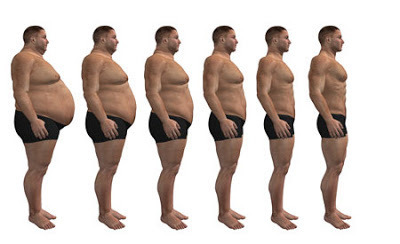
Introduction: Abdominal adipose tissue suppresses testosterone production by various mechanisms affecting the hypothalamic–pituitary–gonadal axis. Hypogonadism leads to further accumulation of fat mass thus creating a vicious circle. This study analysed the effects of restoring testosterone in obese hypogonadal men.
Methods: Cumulative, prospective, registry study of 181 men (mean age: 59.11±6.06 years) with testosterone levels below 12.1 nmol/l and a BMI of ≥30 kg/m2. All men received parenteral testosterone undecanoate 1000 mg/12 weeks following an initial 6-week interval. 89 men were treated 5 years, 114 4 years, 133 3 years, 159 2 years, 181 1 year. The changing numbers do not reflect drop-out rates but are a result of the design as new patients are added once they have received at least 1 year of treatment.
Results: At the end of the observation period, mean weight (kg) decreased from 114.71±11.59 (minimum 87.0, maximum 139.00) to 93.24±8.49 (min 80.0; max 115.0). This decrease was statistically significant vs baseline .
Waist circumference (cm) as a measure of abdominal fat decreased from 111.2±7.54 (min 89.00; max 129.00) to 100.47±7.11 (min 84.00; max 117.00), BMI from 36.72±3.72 (min 30.10; max 46.51) to 30.22±2.6 (min 25.66; max 36.71).
Fasting glucose decreased from 5.84±0.84 to 5.41±0.12 mmol/l, total cholesterol from 7.63±0.95 to 4.9±0.28, LDL from 4.47±1.03 to 2.94±0.93, triglycerides from 3.31±0.56 to 2.17±0.13 mmol/l. Systolic blood pressure decreased from 159.17±15.9 to 139.08±10.99 mmHg, diastolic blood pressure from 96.5±11.01 to 80.39±7.51 mmHg (P
Conclusion: Normalising testosterone produced loss of weight/waist circumference and improved metabolic profile. These improvements were progressive over 5 years.
http://www.endocrine-abstracts.org/ea/0032/ea0032p740.htm

Published on April 29, 2013 18:01
April 26, 2013
Clomid (clomiphene) Increases Testosterone and Sperm Count in Men- But No Mention About Sex Drive
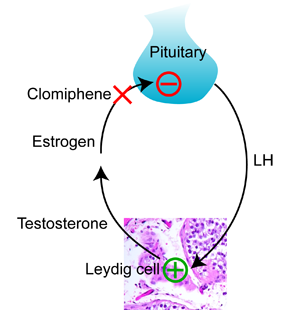
Oral Enclomiphene Citrate Stimulates the Endogenous Production of Testosterone and Sperm Counts in Men with Low Testosterone: Comparison with Testosterone Gel. The Journal of Sexual Medicine. http://onlinelibrary.wiley.com/doi/10.1111/jsm.12116/abstract
Introduction - Clomiphene citrate is employed off-label in men who have low testosterone and for the restoration of sperm counts in men who have used exogenous testosterone. Clomiphene is a mixture of two diastereoisomers: zuclomiphene and enclomiphene. We evaluated enclomiphene citrate in men with secondary hypogonadism.
Aim - Our aim was to compare oral enclomiphene citrate as an alternative to topical testosterone.
Main Outcome Measures - Blood levels of total testosterone (TT), estradiol, follicle-stimulating hormone (FSH), luteinizing hormone (LH), sex hormone binding globulin, thyroid stimulation hormone, prolactin, and insulin-like growth factor 1 IGF-1 were measured at certain times after treatment with each agent. Sperm parameters were determined at the same visits. Free testosterone (FT) was calculated.
Methods - This was a proof-of-principle, randomized, open-label, fixed dose, active-control, two-center phase IIB study in 12 men with secondary hypogonadism treated previously with topical testosterone.
Results - After discontinuation of topical testosterone, morning TT values averaged 165 ± 66 pg/dL. After 3 months, there was a significant rise in men receiving enclomiphene citrate and gel that was sustained for 3 months. At 6 months, TT levels were 545 ± 268 and 525 ± 256 pg/dL for groups receiving the gel and enclomiphene citrate, respectively. Only men in the enclomiphene citrate group demonstrated increased LH and FSH. TT decreased one month posttreatment to pretreatment values. Enclomiphene citrate elevated sperm counts in seven out of seven men at 3 months and six out of six men at 6 months with sperm concentrations in the 75–334 × 106/mL range. The gel was ineffective in raising sperm counts above 20 × 106/mL for all five men at 3 months and raised counts in only two or five men at 6 months. At follow-up, only enclomiphene citrate treatment was associated with elevated sperm counts.
Conclusions - Enclomiphene citrate increased testosterone and sperm counts. Concomitant changes in LH and FSH suggest normalization of endogenous testosterone production and restoration of sperm counts through the hypothalamic–pituitary–testicular axis.

Published on April 26, 2013 08:27
April 10, 2013
Another Company is Caught Adding an Analog of Viagra to Its "Natural" Testosterone Booster Supplement
Consumer Concepts, Inc. notified the public of a consumer/user level recall of all ROCK-It MAN Male Enhancement Capsules sold between October, 2012 and April, 2013. Analytical tests conducted by the FDA concluded that the product contained hydroxythiohomosildenafil.
Hydroxythiohomosildenafil is an analogue of sildenafil (Viagra) and is expected to possess a similar pharmacological and adverse event profile. Sildenafil is the active pharmaceutical ingredient in a FDA approved drug that is used to treat erectile dysfunction, making these products unapproved new drugs.
http://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm347125.htm?source=govdelivery

Published on April 10, 2013 13:00
April 9, 2013
Effect of Age, Body Weight and Smoking on Testosterone in Men
This study showed that
1- Men with higher Body Mass Index (a measure of weight that takes into account height, calculate yours here: http://1.usa.gov/XBIO5K ) had lower testosterone as they aged compared to thinner men. In fact, "a change in BMI from nonobese to obese may be equivalent to a 15 yr fall in T" Note: BMI is a very rough measure that does not take into account muscle or fat mass. A muscular man with little body fat may have high BMI (in my case, my BMI is 30). A better study would measure fat mass, but that tends to be cumbersome and expensive.
2- Smoking did not affect testosterone, but it made the pituitary gland send a higher LH signal to testicles, which could be caused by progressive testicular dysfunction.
3- Not surprisingly, sex hormone binding globulin increased with age. SHBG binds to testosterone and renders it ineffective. Higher insulin levels and lower IGF-1 levels caused by aging may account for this increase in SHBG.
4- Aging causes primary testicular dysfunction with maintained total T and progressively blunted free T associated with higher LH. This interpretation is supported by the age-related attrition of the testicular Leydig cell population and other factors involved with testicular function.
Reference: http://jcem.endojournals.org/content/93/7/2737.long

Published on April 09, 2013 14:18
April 8, 2013
Media Sensationalism: Meat and Carnitine are Bad for your Heart

This study was recently published, pushing the hypothesis that L-Carnitine in meats could be a connection between meats and cardiovascular disease risk, via TMAO (Trimethylamine oxide). It has received a lot of media coverage today. But there is a lot of speculation in this study.
For more click here
Carnitine and Heart Disease- Positive Results
8.1. Blood Pressure
ALCAR in conjunction with ALA can potentially reduce hypertension in via their combined anti-oxidant and pro-energetic effects[165] as well as insulin resistance and glucose tolerance in those with compromised cardiac health[166] with minimal to no side-effects at the dosage of 2g a day. At this dose of 2g daily, it has been implicating in reducing blood pressure in persons with poor glucose tolerance by almost 10 points systolic, with some decrease in diastolic as well.[49]
A dose of 4.5g GPLC has been shown to increase nitric oxide levels after 28 days of supplementation in some persons,[1] and does so at a dose of 3g as well.[33]
May benefit blood pressure in unhealthy persons (metabolic syndrome, high blood pressure). Has the mechanisms to improve blood pressure independent of a disease state via nitric oxide, but it is unclear how it affects blood pressure in those with normal blood pressure.
8.2. Disorders of Blood Flow
Carnitine, in the form of Propionyl-L-Carnitine (PLC, or GPLC if bound to Glycine), has been shown to improve symptoms of intermittent claudication. PLC supplementation at a dose of 1-3g a day seems to reliably increase maximum walking time in persons suffering from intermittent claudication[14][167][15] and improve quality of life.[13] The benefit does not appear to be dose dependent, and seems to benefit persons with more severe symptoms to a greater degree than persons with lesser symptoms.
PLC aids peripheral arterial diseases in general as it increases peripheral microcirculation.[168][169] In persons with peripheral arterial diseases, PLC supplementation can increase strength and exercise performance[170] although exercise itself can also be seen as therapeutic.[171]
Quite promising for periphery artery disease and intermittent claudication
8.3. Aging
During aging, defects in oxidative phosphorylation occur exclusively in Interfibrillar mitochondria, located between myofibrils.[172][173] Due to substrate poorly oxidized when introduced into complexes I, III, and IV and not alleviated by uncoupling it appears the aging 'defect' associated with cardiac mitochondria is located in the Electron Transport Chain.[113]Enzymatic activity of complexes III (through cytochrome C binding) and IV also appear to be decreased during cardiac aging.[172][174][175]
It appears these damages may be secondary to cardiac Ischemia.[113] Ischemia causes damage to the Electron Transport Chain after 10-20 minutes via reducing activity of complex I[176] and reducing phosphorylation at complex V and adenine dinucleotide translocase.[177][178] Complex III[176] and IV[179] are hindered at longer periods of Ischemia. It appears that the general process of Ischemia hits elderly persons harder than youth[180] despite some level of damage at both ages.[181]
Acetyl-L-Carnitine is proposed to target these defects its various mitochondrial benefits, discussed elsewhere. One such benefit is seen when aged rats were given a bolus of Acetyl-L-Carnitine 3 hours before cardiac Ischemia, and suffered less damage.[182] The same benefits were not seen with adult hearts subject to Ischemia, and the damage induced to aged hearts defaulted to similar levels as adult hearts.[182][113]
Another possible mechanism is increasing levels of CPT1 in the myocardium, without affecting overall carnitine levels.[183] A decline of this rate-limiting step is seen during aging, thus upregulating it may attenuate changes seen with aging. It has been noted in human hearts that less fatty acid oxidation occurs with aging, causing a shift towards cardiac glucose metabolism[184]which are thought to be due to less CPT1 activity.[185][186]

Published on April 08, 2013 17:56
April 3, 2013
Blood Analysis Reference Table
From the book:ANABOLIC
STEROIDS-A QUESTION OF MUSCLE-
PROBLEMS & SOLUTIONS (By Michael Scally)
Test
Reference Range
Alanine
aminotransferase (ALT, SGPT)
Levels are
extremely increased in cases of liver cell necrosis of any cause, right heart
failure, acute anoxia, extensive trauma, or left heart failure. A slightly
high level may indicate cirrhosis, obstructive jaundice, liver tumors,
extensive myocardial infarction, myositis, muscular dystrophy, fatty liver,
chronic alcohol abuse, or severe pancreatitis. Levels will by low in cases of
pyridoxal phosphate deficiency
Female
7-30 U/liter
Male
10-55 U/liter
Albumin
There is no
naturally occurring hyperalbuminemia. Any condition that results in the
decrease of plasma water will increase the concentration of all plasma
proteins, including albumin. Low concentrations of blood albumin may be due
to acute and chronic inflammation, decreased synthesis by the liver,
increased loss via body surfaces, increased catabolism, or increased blood
volume. *albumin is the principal oncotically active component of plasma. As
the major plasma protein, albumin acts as a nitrogen pool. Its role in
transporting bilirubin, bile acids, metal ions, and drugs will be markedly
affected by variations in concentrations.
3.1-4.3 g/dl
Alkaline
phosphatase (adult)
Origins of the
major phosphatases are liver, bone, intestine, endometrium, and lung.
Ingestion of a meal increases the intestinal isoenzyme of alp in serum,
especially in individuals who are blood type o or b and who are
Lewis-positive secretors. Increased levels of alp may indicate increased bone
metabolism (during healing of fracture, primary and secondary
hyperparathyroidism, osteomalacia, or juvenile rickets). May also indicate bone
disease, renal disease, or liver disease. Low levels may indicate
hypothyroidism, scurvy, gross anemia, vitamin b12 deficiency or nutritional
deficiency of zinc or magnesium.
Female
30-100 U/liter
Male
45-115 U/liter
Androstenedione
(adult)
Androstenedione
is a major precursor in the biosynthesis of androgens and estrogens. It
is produced in adrenals and gonads and serves as prohormone for testosterone
and estrone. The test is useful in conjunction with other tests in the
evaluation and management of androgen disorders
50-250 ng/dl
Aspartate
aminotransferase (AST, SGOT)
Increased
levels may indicate liver cell necrosis or injury of any cause, including
cholestatic and obstructive jaundice, chronic hepatitis, or drug-induced
injury to liver. May also be associated with hepatic metastases and hepatoma,
necrosis or trauma to heart or skeletal muscle, inflammatory disease of heart
or skeletal muscle, heart failure, Forbes's disease, heat stroke,
hypothyroidism, intestinal obstruction, lactate acidosis, or toxic shock
syndrome. Also distinguishes neonatal hepatitis from biliary atresia.
Female
9-25 U/liter
Male
10-40 U/liter
Bilirubin,
direct
High serum
blood levels are associated with intrahepatic and extrahepatic biliary tree
obstruction, hepatocellular damage, cholestasis, Dubin-Johnson syndrome, or
rotor's syndrome.
0.0-0.4 mg/dl
Bilirubin,
total
High serum
levels may indicate hepatocellular damage (inflammatory, toxic, neoplastic),
intrahepatic and extrahepatic biliary tree obstruction, hemolytic diseases,
fructose intolerance, hypothyroidism or neonatal physiological jaundice
0.0-1.0 mg/dl
Calcium
High blood
calcium levels may indicate primary and tertiary hyperparathyroidism,
malignant disease with bone involvement (in particular metastatic carcinoma
of the breast, lung, kidney, multiple myeloma, lymphomas, and leukemia),
vitamin d intoxication, milk-alkali syndrome, Paget's disease with
immobilization, thyrotoxicosis, acromegaly, diuretic phase of acute tubular necrosis
or dehydration. Low levels of calcium may indicate hypoparathyroidism;
vitamin d deficiency, chronic renal failure, magnesium deficiency, prolonged
anticonvulsant therapy, acute pancreatitis, anterior pituitary hypofunction,
hypoalbuminemia, or inadequate nutrition.
8.5-10.5 mg/dl
Carbon dioxide
content, total
High levels
may indicate respiratory acidosis caused by poor gas exchange or depression
of respiratory center; generalized respiratory disease; metabolic acidosis
(after severe vomiting in pyloric stenosis, hypokalemic states, or excessive
alkali intake). Low levels may indicate compensated respiratory alkalosis,
metabolic acidosis in diabetes mellitus, renal glomerular or tubular failure,
renal tubular acidosis and intestinal loss of alkali with coexisting increase
in c1 and normal anion gap
24-30
mmol/liter
Chloride
High chloride
levels may be attributed to dehydration, renal tubular acidosis, acute renal
failure, diabetes insipidus, metabolic acidosis associated with prolonged
diarrhea with loss of nahco3, respiratory alkalosis, and some cases of
primary hyperparathyroidism. Low serum chloride levels may be due to
excessive sweating, prolonged vomiting from any cause or gastric suction,
persistent gastric secretion, salt-losing nephritis, aldosteronism, potassium
depletion associated with alkalosis, respiratory acidosis
100-108
mmol/liter
Cholesterol
High total
cholesterol levels may indicate familial or polygenic hyperlipoproteinemia
types IIa and IIb, hyperlipidemia, hyperlipoproteinemias secondary to
hepatocellular disease, intra- and extrahepatic cholestasis, chronic renal
failure, malignant neoplasms of pancreas and prostate, hypothyroidism, gout,
ischemic heart disease, pregnancy, diabetes, alcoholism, analbuminemia,
dysglobulinemia, anorexia nervosa, idiopathic hypercalcemia, acute
intermittent porphyria, or isolated hgh deficiency. Low levels may be
associated with lipoprotein deficiency, hepatocellular necrosis, malignant
neoplasm of liver, hyperthyroidism, malabsorption, malnutrition,
megaloblastic anemias, chronic obstructive lung disease, mental retardation,
rheumatoid arthritis, or intestinal lymphangiectasia. *secondary disorders
that elevate cholesterol levels should be ruled out prior to initiating
therapy with cholesterol-lowering drugs. *factors that have variable effects
on cholesterol levels in different people include posture before and at time
of blood sampling, a recent meal, emotional stress, and menstrual cycle.
Desirable
< 200 mg / dl
Borderline
high
200-239 mg/dl
High
> 239 mg/dl
Creatinine
High serum or
plasma levels may indicate renal function impairment, both acute and chronic;
active acromegaly and gigantism, hyperthyroidism, and meat meals
0.6-1.5 mg/dl
Dehydroepiandrosterone
(DHEA) sulfate (adult)
Decreased
levels may be associated with increased age in men & women,
hyperlipidemia, psychosis, or psoriasis. Weakly androgenic
Male
10-619 µg/dl
Female
Premenopausal
12-535 µg/dl
Postmenopausal
30-260 µg/dl
Estradiol
Estradiol is
the most active of endogenous estrogens. The test is of value, together with
gonadotropins, in evaluating menstrual and fertility problems in adult
females. Measurement is also useful in the evaluation of gynecomastia or
feminization states due to estrogen or producing tumors.
Female
Menstruating
Follicular
phase
50-145 pg/ml
Midcycle
peak
112-443 pg/ml
Luteal
phase
50-241 pg/ml
Postmenopausal
< 59 pg / ml
Male
< 50 pg / ml
Follicle-stimulating
hormone (FSH)
In
hypogonadism, FSH and LH levels lower than normal for the patient's age
indicate hypothalamic or pituitary problems; higher levels indicate a primary
gonadal defect
Female
Menstruating
Follicular
phase
3.0-20.0
U/liter
Ovulatory
phase
9.0-26.0
U/liter
Luteal
phase
1.0-12.0
U/liter
Postmenopausal
18.0-153.0
U/liter
Male
1.0-12.0
U/liter
Globulin
High levels
may be associated with chronic hepatitis, plasma cell dyscrasias/ lymphoproliferative
disorders, cirrhosis, chronic liver diseases, chronic infections or certain
autoimmune disorders. Low levels may indicate immune deficiency or
suppression or lymphoproliferative disorder. Decreases in all fractions may
be seen in bulk loss of proteins into the gut.
2.6-4.1 g/dl
Glucose,
fasting
Serum glucose
levels may be high due to diabetes mellitus, strenuous exercise, increased
epinephrine, pancreatic disease or an endocrine disorder. A high serum level
may also be related to acute myocardial infarction or severe angina, chronic
liver disease, or chronic renal disease.
70-110 mg/dl
(gamma)-Glutamyltransferase
(GGT)
Very high levels can be associated with
obstructive liver disease and posthepatic obstruction. Moderately high levels
may indicate liver disease (inflammation, cirrhosis, space-occupying
lesions), infectious mononucleosis, renal transplant, hyperthyroidism,
myotonic dystrophy, diabetes mellitus, pancreatitis, or alcohol-induced liver
disease. Low GGT levels will indicate hypothyroidism. *useful marker for
pancreatic cancer, prostatic cancer, and hepatoma because levels reflect
remission and recurrence.
Male
1-94 U/liter
Female
1-70 U/liter
Growth hormone
(resting)
Secretion of
GH is episodic and pulsatile; highest values occur during periods of deepest
sleep. Ability to secrete GH in response to a conventional challenge declines
with age. Random levels of GH provide little diagnostic information; GH
secretion is best assessed during tests that stimulate or suppress release.
Patients with GH-producing pituitary disorders often release GH in response
to TRH or GnRH; and patients with suspected GH deficiencies have subnormal
responses to stimulation tests (i.e. GH stimulation test after arginine,
insulin, l-dopa, glucagon, propanolol and insulin tolerance test.)
2-5 ng/ml
Hemoglobin A1C
Glycated
hemoglobin concentration appears to reflect the mean blood glucose
concentration over the previous 4-8 wks. This test, while not useful
for the diagnosis of diabetes mellitus, has been shown to be useful in
monitoring its long-term control. Glycated hemoglobins are increased as
a reflection of hyperglycemia during the lifespan of erythrocytes
3.8-6.4%
High-density
lipoprotein cholesterol, as major risk factor
Epidemiological
studies demonstrate the inverse association between HDL-c levels and the
incidence and prevalence of coronary heart disease (CHD). It is suggested
that for every 5 mg/dl decrease in HDL-c below the mean, the risk of CHD
increases 25%. Another approach in assessing CHD risk is to calculate the
ratio of HDL-c to either LDL-c or total cholesterol. The following primary
disease states can lead to secondary decrease in HDL-c: uncontrolled
diabetes, premature coronary heart disease, hepatocellular disorders,
cholestasis, nephrotic syndrome, and chronic renal failure.
above 40 mg/dl men
above 50 mg/dl women
Insulin
Decreased
serum levels indicate inadequately treated type I diabetes mellitus.
High serum levels may indicate insulin overdose, insulin resistance
syndromes, or endogenous hyperinsulinemia
2-20 U/ml
Lactate
dehydrogenase (LDH)
Extremely high
levels may indicate megaloblastic and pernicious anemia, extensive
carcinomatosis, viral hepatitis, shock, hypoxia or extreme hyperthermia. Very
high levels are associated with cirrhosis, obstructive jaundice, renal
diseases, neoplastic diseases, skeletomuscular diseases, or congestive heart
failure. Mildly high levels are associated with any cellular injury that
results in loss of cytoplasm, myocardial or pulmonary infarction, leukemias,
hemolytic anemias, hepatitis (nonviral), sickle cell disease, lymphoma, renal
infarction, or acute pancreatitis.
110-210
U/liter
Lipoprotein(a)
0-30 mg/dl
Low-density
lipoprotein cholesterol
LDL
encompasses all of the lipoproteins with density greater than 1.006 kg/l and
less than or equal to 1.063 kg/l. High levels may indicate primary
hyperlipoproteinemia types IIa and IIb; tendon and tuberous xanthomas,
corneal arcus, and premature coronary heart disease. The following diseases
can lead to secondary elevation of LDL-c: hyperlipoproteinemia secondary to
hypothyroidism, nephrotic syndrome, hepatic obstruction, hepatic disease,
pregnancy, anorexia nervosa, diabetes, chronic renal failure, and Cushing's
syndrome.
Desirable
mg/ dl
Borderline
high risk
130-159 mg/dl
High risk
greater than
or equal to 160 mg/dl
Iron
High serum
levels may indicate pernicious, aplastic, and hemolytic anemias;
hemochromatosis, acute leukemia, lead poisoning, acute hepatitis, vitamin b6
deficiency, excessive iron supplementation/therapy, repeated transfusions, or
nephritis. Low serum iron levels may indicate iron-deficiency anemia,
remission of acute and chronic infection, carcinoma, nephrosis,
hypothyroidism, or postoperative state. *symptoms of iron poisoning include
abdominal pain, vomiting, bloody diarrhea, cyanosis, lethargy, and
convulsions. Levels may vary widely for an individual within the same day or
from day to day.
45-180 ug/dL
(MALES FEMALES).
Luteinizing
hormone (LH)
Test used to
determine the preovulatory LH surge; also provides an integrated picture of
LH secretion throughout the day. Shows pituitary or hypothalamic impairment
or overproduction
Female
Menstruating
Follicular
phase
2.0-15.0
Ovulatory
phase
22-105
Luteal
phase
0.6-19
Postmenopausal
16-64
Male
2.0-12.0
Magnesium
Mg plays a
vital role in glucose metabolism by facilitating the formation of muscle and
liver glycogen from blood-borne glucose. Also participates as a
cofactor in the breakdown of glucose, fatty acids, and amino acids during
energy metabolism. High serum levels may indicate dehydration, renal
insufficiency, uncontrolled diabetes mellitus, adrenocortical insufficiency,
Addison's disease, hypothyroidism or lupus erythematosus.
Phytate, fatty acids, and an excess of phosphate impair mg absorption.
Symptoms of deficiency usually do not occur until serum levels are above 1 meq / liter
1.4-2.0
meq/liter
Phosphorus,
inorganic (adult)
Serum
phosphorus concentrations have a circadian rhythm (highest level in late
morning, lowest in evening) and are subject to rapid change secondary to
environmental factors such as diet (carbohydrate), phosphate-binding
antacids, and fluctuations in growth hormone, insulin, and renal function.
High levels may indicate osteolytic metastatic bone tumors, myelogenous
leukemia, milk-alkali syndrome, vitamin d intoxication, healing fractures,
renal failure, hypoparathyroidism, pseudohypoparathyroidism,
diabetes mellitus with ketosis, acromegaly, portal cirrhosis, pulmonary
embolism, lactic acidosis or respiratory acidosis.
2.6-4.5 mg/dl
Potassium
High potassium
levels are associated with reduced renal excretion of potassium or
redistribution of potassium in the body (i.e. Massive hemolysis, severe
tissue damage, severe acute starvation-anorexia nervosa, hyperkinetic
activity, malignant hyperpyrexia following anesthesia, hyperkalemic periodic
paralysis, and dehydration).
3.4-4.8
mmol/liter
Progesterone
The diagnostic
value of this test lies in its detection of ovulation and in the evaluation
of the function of the corpus luteum. Serial sampling during the
menstrual cycle is required. During menopause, levels drop to 0
Female
Follicular
phase
< 1 ng / ml
Midluteal
phase
3-20 ng/ml
Male
< 1 ng / ml
Prolactin
May help
assess Prolactin reserve and abnormal Prolactin secretion by the pituitary.
May indicate pituitary tumors.
Female
Premenopausal
0-20 ng/ml
Postmenopausal
0-15 ng/ml
Male
0-15 ng/ml
Prostate-specific
antigen (PSA)
PSA is
prostate-tissue specific, not prostate-cancer specific. Used for early
detection of the recurrence of prostatic cancer. The test is of great value
as a marker in the follow-up of patients at high risk for disease
progression. PSA values increase with age.
Female
0
Male
less than 40 years of age
0.0-2.0 ng/ml
greater
than or equal to 40 yr old
0.0-4.0 ng/ml
Prostate-specific
antigen (PSA), free, in males 45-75 yr old, with PSA values between 4 and 20
ng/ml
above 25%
associated with benign prostatic hyperplasia
Protein, total
High blood
levels may be associated with anabolic steroid use, androgens,
corticosteroids, coritcotropin, epinephrine, insulin, progesterone, or
thyroid preparations. Severe protein deficiency, chronic liver disease,
malabsorption syndrome, and malnutrition may also lead to abnormal levels.
Serum total protein decreases in the third trimester of pregnancy.
6.0-8.0 g/dl
Sodium
High serum
levels are associated with water loss in excess of salt through skin, lungs,
GI tract, and kidneys. Also may indicate increased renal sodium conservation
in hyperaldosteronism, Cushing's syndrome or disease, inadequate water intake
because of inadequate thirst mechanism, dehydration, or excessive saline
therapy. Low sodium levels may indicate low sodium intake, sodium losses due
to vomiting, diarrhea, excessive sweating with adequate water intake and
inadequate salt replacement, diuretics abuse, or salt-losing nephropathy
135-145
mmol/liter
Somatomedin C
(Insulin-like growth factor I)
Blood
concentrations of IGF-1 are constant during the day and after eating. In acromegaly,
the test may serve as an indicator of the severity of the disease; serial
determinations may be used to monitor efficacy of treatment. In dwarfism
IGF-1 may be used to determine the response to GH therapy. Concentrations of
IGF-1 rise during the first year of life, reaching the highest values in
preadolescent or early adolescent years. Normal values tend to decline
progressively until age 50
16-24
yr
182-780 ng/ml
25-39
yr
114-492 ng/ml
40-54
yr
90-360 ng/ml
> 54
yr
71-290 ng/ml
Testosterone,
total (morning sample)
This test is a
measure of total circulating testosterone, both protein bound and free. In
adult men, serum levels peak in the early morning, decreasing 25% to the
evening minimum. Levels increase after exercise and decrease after
immobilization and after glucose load. Progressive decreases begin after age
50
Female
6-86 ng/dl
Male
270-1070 ng/dl
Testosterone,
unbound (morning sample)
Free
(nonprotein-bound) testosterone is independent of changes in concentrations
of the principal testosterone transport protein, sex hormone-binding
globulin.
Female
20-40
yr
0.6-3.1 pg/ml
41-60
yr
0.4-2.5 pg/ml
61-80
yr
0.2-2.0 pg/ml
Male
20-40
yr
15.0-40.0
pg/ml
41-60
yr
13.0-35.0
pg/ml
61-80
yr
12.0-28.0
pg/ml
Thyroid-stimulating
hormone (TSH)
First-line
test for hyper- and hypothyroidism. Test is considered by some to be the
preferred screening test for evaluation of thyrometabolic states. Moderately
high TSH is often found in euthyroid patients during treatment of
hyperthyroidism.
0.5-5.0 U/ml
Thyroxine,
total (T4)
Used in
conjunction with other tests to measure thryoid function. T4
testing is frequently used when TSH levels are abnormally high or low. In
hypothyroidism, total serum t4 falls before t3. High
serum levels may represent hyperthyroidism.
4.5-10.9 g/dl
Transferrin
Transferrin is
the major plasma transport protein for iron. High serum levels may
indicate iron deficiency (high levels often precede the appearance of anemia
by days to months). Serum ferritin levels fall with iron deficiency and
with generalized malnutrition but remain normal in the presence of
inflammation and iron deficiency
191-365 mg/dl
Triglycerides
(fasting)
Increased
triglyceride levels indicate hyperlipoproteinemia types I, IIb, III, IV, and
V due to familial or sporadic endogenous hypertriglyceridemia. The following
primary disease states or conditions can lead to secondary elevation of
triglycerides: obesity, impaired glucose tolerance, viral hepatitis,
alcoholism, alcoholic cirrhosis, biliary cirrhosis, acute and chronic
pancreatitis, extrahepatic biliary obstruction, nephrotic syndrome, chronic
renal failure, essential hypertension, acute myocardial infarction, chronic
ischemic heart disease, cerebral thrombosis, hypothyroidism, diabetes
mellitus, gout, pregnancy, glycogen storage diseases types I, II, III, and
IV, down syndrome, respiratory distress syndrome, Werner's syndrome, anorexia
nervosa, or idiopathic hypercalcemia. Low levels of triglycerides may
indicate chronic obstructive lung disease, brain infarction, hyperthyroidism,
hyperparathyroidism, lactosuria, malnutrition, malabsorption syndrome,
intestinal lymphangiectasia or end-stage parenchymal liver disease.
40-150 mg/dl
Triiodothyronine,
total (T3)
Used in
conjunction with other tests to measure thyroid function. High serum
levels may indicate hyperthyroidism while low levels may indicate
hypothyroidism. At least 80% of circulating T3 is derived
from monodeiodination of T4 in peripheral tissues. T3
is 4 to 5 times more potent in biological systems than T4
60-181 ng/dl
Urea nitrogen
(BUN) (adult)
High serum
blood levels may indicate impaired kidney function associated with an
increase with age or protein content of diet.
8-25 mg/dl
Uric acid
High serum
levels may indicate gout, renal failure, leukemia, lymphoma, psoriasis,
polycythemia, multiple myeloma, kidney disease, and or chronic lead
nephropathy. Associated with hyperlipidemia, obesity, hypertension,
arteriosclerosis, diabetes mellitus, hypoparathyroidism, acromegaly, and
liver disease.
Male
3.6-8.5 mg/dl
Female
2.3-6.6 mg/dl
Differential
blood count
Reference
Range
Neutrophils
45-75%
Bands
0-5%
Lymphocytes
16-46%
Monocytes
4-11%
Eosinophils
0-8%
Basophils
0-3%
Erythrocyte
count
Red Blood Cell
count; filled with hemoglobin and specialized for carrying O2 and
CO2 (adult)
Male
4.50-5.30 X 106/mm3
Female
4.10-5.10 X 106/mm3
Ferritin
Surplus iron
is stored as Ferritin, primarily in the liver
Male
30-300 ng/ml
Female
10-200 ng/ml
Folate (folic
acid)
Water soluble
vitamin involved with amino acid metabolism & transfer of single-carbon
units in nucleic acid
Normal
3.1-17.5 ng/ml
Borderline
deficient
2.2-3.0 ng/ml
Deficient
< 2 ng / ml
Excessive
above 17.5 ng/ml
Hematocrit
(adult)
% of Red Blood
Cells present in total blood
Male
37.0-49.0
Female
36.0-46.0
Hemoglobin
(adult)
Oxygen-carrying
compound of blood. Numerical value of hemoglobin present in Red Blood
Cells
Male
13.0-18.0 g/dl
Female
12.0-16.0 g/dl
Iron
Constituent of
hemoglobin (transport of oxygen in blood) and enzymes involved in energy
metabolism
30-160 g/dl
Leukocyte
count (WBC)
White Blood
Cell (WBC); Central to the immune system that defends against infection
4.5-11.0X103/mm3
Mean
corpuscular hemoglobin (MCH)
Value is
calculated from hemoglobin and erythrocyte count. MCH= Erc÷Hb
25.0-35.0
pg/cell
Mean corpuscular
hemoglobin concentration (MCHC)
Mean cell
hemoglobin concentration is calculated from Hb and hematocrit (Hct)
MCHC=
Hct÷Hb
31.0-37.0 g/dl
Mean
corpuscular volume (MCV) (adult)
Mean cell
volume may not be reliable when a large number of abnormal erythroctes or a
dimorphic population of erythrocytes is present. It may also be calculated
from the hematocrit and erythrocyte count
MCV= Erc÷Hct
Male
78-100 m3
Female
78-102 m3
Platelet count
Helps mediate
the blood clotting that prevents loss of blood after injury
150-350X103/mm3
Platelet, mean
volume
6.4-11.0 m3

STEROIDS-A QUESTION OF MUSCLE-
PROBLEMS & SOLUTIONS (By Michael Scally)
Test
Reference Range
Alanine
aminotransferase (ALT, SGPT)
Levels are
extremely increased in cases of liver cell necrosis of any cause, right heart
failure, acute anoxia, extensive trauma, or left heart failure. A slightly
high level may indicate cirrhosis, obstructive jaundice, liver tumors,
extensive myocardial infarction, myositis, muscular dystrophy, fatty liver,
chronic alcohol abuse, or severe pancreatitis. Levels will by low in cases of
pyridoxal phosphate deficiency
Female
7-30 U/liter
Male
10-55 U/liter
Albumin
There is no
naturally occurring hyperalbuminemia. Any condition that results in the
decrease of plasma water will increase the concentration of all plasma
proteins, including albumin. Low concentrations of blood albumin may be due
to acute and chronic inflammation, decreased synthesis by the liver,
increased loss via body surfaces, increased catabolism, or increased blood
volume. *albumin is the principal oncotically active component of plasma. As
the major plasma protein, albumin acts as a nitrogen pool. Its role in
transporting bilirubin, bile acids, metal ions, and drugs will be markedly
affected by variations in concentrations.
3.1-4.3 g/dl
Alkaline
phosphatase (adult)
Origins of the
major phosphatases are liver, bone, intestine, endometrium, and lung.
Ingestion of a meal increases the intestinal isoenzyme of alp in serum,
especially in individuals who are blood type o or b and who are
Lewis-positive secretors. Increased levels of alp may indicate increased bone
metabolism (during healing of fracture, primary and secondary
hyperparathyroidism, osteomalacia, or juvenile rickets). May also indicate bone
disease, renal disease, or liver disease. Low levels may indicate
hypothyroidism, scurvy, gross anemia, vitamin b12 deficiency or nutritional
deficiency of zinc or magnesium.
Female
30-100 U/liter
Male
45-115 U/liter
Androstenedione
(adult)
Androstenedione
is a major precursor in the biosynthesis of androgens and estrogens. It
is produced in adrenals and gonads and serves as prohormone for testosterone
and estrone. The test is useful in conjunction with other tests in the
evaluation and management of androgen disorders
50-250 ng/dl
Aspartate
aminotransferase (AST, SGOT)
Increased
levels may indicate liver cell necrosis or injury of any cause, including
cholestatic and obstructive jaundice, chronic hepatitis, or drug-induced
injury to liver. May also be associated with hepatic metastases and hepatoma,
necrosis or trauma to heart or skeletal muscle, inflammatory disease of heart
or skeletal muscle, heart failure, Forbes's disease, heat stroke,
hypothyroidism, intestinal obstruction, lactate acidosis, or toxic shock
syndrome. Also distinguishes neonatal hepatitis from biliary atresia.
Female
9-25 U/liter
Male
10-40 U/liter
Bilirubin,
direct
High serum
blood levels are associated with intrahepatic and extrahepatic biliary tree
obstruction, hepatocellular damage, cholestasis, Dubin-Johnson syndrome, or
rotor's syndrome.
0.0-0.4 mg/dl
Bilirubin,
total
High serum
levels may indicate hepatocellular damage (inflammatory, toxic, neoplastic),
intrahepatic and extrahepatic biliary tree obstruction, hemolytic diseases,
fructose intolerance, hypothyroidism or neonatal physiological jaundice
0.0-1.0 mg/dl
Calcium
High blood
calcium levels may indicate primary and tertiary hyperparathyroidism,
malignant disease with bone involvement (in particular metastatic carcinoma
of the breast, lung, kidney, multiple myeloma, lymphomas, and leukemia),
vitamin d intoxication, milk-alkali syndrome, Paget's disease with
immobilization, thyrotoxicosis, acromegaly, diuretic phase of acute tubular necrosis
or dehydration. Low levels of calcium may indicate hypoparathyroidism;
vitamin d deficiency, chronic renal failure, magnesium deficiency, prolonged
anticonvulsant therapy, acute pancreatitis, anterior pituitary hypofunction,
hypoalbuminemia, or inadequate nutrition.
8.5-10.5 mg/dl
Carbon dioxide
content, total
High levels
may indicate respiratory acidosis caused by poor gas exchange or depression
of respiratory center; generalized respiratory disease; metabolic acidosis
(after severe vomiting in pyloric stenosis, hypokalemic states, or excessive
alkali intake). Low levels may indicate compensated respiratory alkalosis,
metabolic acidosis in diabetes mellitus, renal glomerular or tubular failure,
renal tubular acidosis and intestinal loss of alkali with coexisting increase
in c1 and normal anion gap
24-30
mmol/liter
Chloride
High chloride
levels may be attributed to dehydration, renal tubular acidosis, acute renal
failure, diabetes insipidus, metabolic acidosis associated with prolonged
diarrhea with loss of nahco3, respiratory alkalosis, and some cases of
primary hyperparathyroidism. Low serum chloride levels may be due to
excessive sweating, prolonged vomiting from any cause or gastric suction,
persistent gastric secretion, salt-losing nephritis, aldosteronism, potassium
depletion associated with alkalosis, respiratory acidosis
100-108
mmol/liter
Cholesterol
High total
cholesterol levels may indicate familial or polygenic hyperlipoproteinemia
types IIa and IIb, hyperlipidemia, hyperlipoproteinemias secondary to
hepatocellular disease, intra- and extrahepatic cholestasis, chronic renal
failure, malignant neoplasms of pancreas and prostate, hypothyroidism, gout,
ischemic heart disease, pregnancy, diabetes, alcoholism, analbuminemia,
dysglobulinemia, anorexia nervosa, idiopathic hypercalcemia, acute
intermittent porphyria, or isolated hgh deficiency. Low levels may be
associated with lipoprotein deficiency, hepatocellular necrosis, malignant
neoplasm of liver, hyperthyroidism, malabsorption, malnutrition,
megaloblastic anemias, chronic obstructive lung disease, mental retardation,
rheumatoid arthritis, or intestinal lymphangiectasia. *secondary disorders
that elevate cholesterol levels should be ruled out prior to initiating
therapy with cholesterol-lowering drugs. *factors that have variable effects
on cholesterol levels in different people include posture before and at time
of blood sampling, a recent meal, emotional stress, and menstrual cycle.
Desirable
< 200 mg / dl
Borderline
high
200-239 mg/dl
High
> 239 mg/dl
Creatinine
High serum or
plasma levels may indicate renal function impairment, both acute and chronic;
active acromegaly and gigantism, hyperthyroidism, and meat meals
0.6-1.5 mg/dl
Dehydroepiandrosterone
(DHEA) sulfate (adult)
Decreased
levels may be associated with increased age in men & women,
hyperlipidemia, psychosis, or psoriasis. Weakly androgenic
Male
10-619 µg/dl
Female
Premenopausal
12-535 µg/dl
Postmenopausal
30-260 µg/dl
Estradiol
Estradiol is
the most active of endogenous estrogens. The test is of value, together with
gonadotropins, in evaluating menstrual and fertility problems in adult
females. Measurement is also useful in the evaluation of gynecomastia or
feminization states due to estrogen or producing tumors.
Female
Menstruating
Follicular
phase
50-145 pg/ml
Midcycle
peak
112-443 pg/ml
Luteal
phase
50-241 pg/ml
Postmenopausal
< 59 pg / ml
Male
< 50 pg / ml
Follicle-stimulating
hormone (FSH)
In
hypogonadism, FSH and LH levels lower than normal for the patient's age
indicate hypothalamic or pituitary problems; higher levels indicate a primary
gonadal defect
Female
Menstruating
Follicular
phase
3.0-20.0
U/liter
Ovulatory
phase
9.0-26.0
U/liter
Luteal
phase
1.0-12.0
U/liter
Postmenopausal
18.0-153.0
U/liter
Male
1.0-12.0
U/liter
Globulin
High levels
may be associated with chronic hepatitis, plasma cell dyscrasias/ lymphoproliferative
disorders, cirrhosis, chronic liver diseases, chronic infections or certain
autoimmune disorders. Low levels may indicate immune deficiency or
suppression or lymphoproliferative disorder. Decreases in all fractions may
be seen in bulk loss of proteins into the gut.
2.6-4.1 g/dl
Glucose,
fasting
Serum glucose
levels may be high due to diabetes mellitus, strenuous exercise, increased
epinephrine, pancreatic disease or an endocrine disorder. A high serum level
may also be related to acute myocardial infarction or severe angina, chronic
liver disease, or chronic renal disease.
70-110 mg/dl
(gamma)-Glutamyltransferase
(GGT)
Very high levels can be associated with
obstructive liver disease and posthepatic obstruction. Moderately high levels
may indicate liver disease (inflammation, cirrhosis, space-occupying
lesions), infectious mononucleosis, renal transplant, hyperthyroidism,
myotonic dystrophy, diabetes mellitus, pancreatitis, or alcohol-induced liver
disease. Low GGT levels will indicate hypothyroidism. *useful marker for
pancreatic cancer, prostatic cancer, and hepatoma because levels reflect
remission and recurrence.
Male
1-94 U/liter
Female
1-70 U/liter
Growth hormone
(resting)
Secretion of
GH is episodic and pulsatile; highest values occur during periods of deepest
sleep. Ability to secrete GH in response to a conventional challenge declines
with age. Random levels of GH provide little diagnostic information; GH
secretion is best assessed during tests that stimulate or suppress release.
Patients with GH-producing pituitary disorders often release GH in response
to TRH or GnRH; and patients with suspected GH deficiencies have subnormal
responses to stimulation tests (i.e. GH stimulation test after arginine,
insulin, l-dopa, glucagon, propanolol and insulin tolerance test.)
2-5 ng/ml
Hemoglobin A1C
Glycated
hemoglobin concentration appears to reflect the mean blood glucose
concentration over the previous 4-8 wks. This test, while not useful
for the diagnosis of diabetes mellitus, has been shown to be useful in
monitoring its long-term control. Glycated hemoglobins are increased as
a reflection of hyperglycemia during the lifespan of erythrocytes
3.8-6.4%
High-density
lipoprotein cholesterol, as major risk factor
Epidemiological
studies demonstrate the inverse association between HDL-c levels and the
incidence and prevalence of coronary heart disease (CHD). It is suggested
that for every 5 mg/dl decrease in HDL-c below the mean, the risk of CHD
increases 25%. Another approach in assessing CHD risk is to calculate the
ratio of HDL-c to either LDL-c or total cholesterol. The following primary
disease states can lead to secondary decrease in HDL-c: uncontrolled
diabetes, premature coronary heart disease, hepatocellular disorders,
cholestasis, nephrotic syndrome, and chronic renal failure.
above 40 mg/dl men
above 50 mg/dl women
Insulin
Decreased
serum levels indicate inadequately treated type I diabetes mellitus.
High serum levels may indicate insulin overdose, insulin resistance
syndromes, or endogenous hyperinsulinemia
2-20 U/ml
Lactate
dehydrogenase (LDH)
Extremely high
levels may indicate megaloblastic and pernicious anemia, extensive
carcinomatosis, viral hepatitis, shock, hypoxia or extreme hyperthermia. Very
high levels are associated with cirrhosis, obstructive jaundice, renal
diseases, neoplastic diseases, skeletomuscular diseases, or congestive heart
failure. Mildly high levels are associated with any cellular injury that
results in loss of cytoplasm, myocardial or pulmonary infarction, leukemias,
hemolytic anemias, hepatitis (nonviral), sickle cell disease, lymphoma, renal
infarction, or acute pancreatitis.
110-210
U/liter
Lipoprotein(a)
0-30 mg/dl
Low-density
lipoprotein cholesterol
LDL
encompasses all of the lipoproteins with density greater than 1.006 kg/l and
less than or equal to 1.063 kg/l. High levels may indicate primary
hyperlipoproteinemia types IIa and IIb; tendon and tuberous xanthomas,
corneal arcus, and premature coronary heart disease. The following diseases
can lead to secondary elevation of LDL-c: hyperlipoproteinemia secondary to
hypothyroidism, nephrotic syndrome, hepatic obstruction, hepatic disease,
pregnancy, anorexia nervosa, diabetes, chronic renal failure, and Cushing's
syndrome.
Desirable
mg/ dl
Borderline
high risk
130-159 mg/dl
High risk
greater than
or equal to 160 mg/dl
Iron
High serum
levels may indicate pernicious, aplastic, and hemolytic anemias;
hemochromatosis, acute leukemia, lead poisoning, acute hepatitis, vitamin b6
deficiency, excessive iron supplementation/therapy, repeated transfusions, or
nephritis. Low serum iron levels may indicate iron-deficiency anemia,
remission of acute and chronic infection, carcinoma, nephrosis,
hypothyroidism, or postoperative state. *symptoms of iron poisoning include
abdominal pain, vomiting, bloody diarrhea, cyanosis, lethargy, and
convulsions. Levels may vary widely for an individual within the same day or
from day to day.
45-180 ug/dL
(MALES FEMALES).
Luteinizing
hormone (LH)
Test used to
determine the preovulatory LH surge; also provides an integrated picture of
LH secretion throughout the day. Shows pituitary or hypothalamic impairment
or overproduction
Female
Menstruating
Follicular
phase
2.0-15.0
Ovulatory
phase
22-105
Luteal
phase
0.6-19
Postmenopausal
16-64
Male
2.0-12.0
Magnesium
Mg plays a
vital role in glucose metabolism by facilitating the formation of muscle and
liver glycogen from blood-borne glucose. Also participates as a
cofactor in the breakdown of glucose, fatty acids, and amino acids during
energy metabolism. High serum levels may indicate dehydration, renal
insufficiency, uncontrolled diabetes mellitus, adrenocortical insufficiency,
Addison's disease, hypothyroidism or lupus erythematosus.
Phytate, fatty acids, and an excess of phosphate impair mg absorption.
Symptoms of deficiency usually do not occur until serum levels are above 1 meq / liter
1.4-2.0
meq/liter
Phosphorus,
inorganic (adult)
Serum
phosphorus concentrations have a circadian rhythm (highest level in late
morning, lowest in evening) and are subject to rapid change secondary to
environmental factors such as diet (carbohydrate), phosphate-binding
antacids, and fluctuations in growth hormone, insulin, and renal function.
High levels may indicate osteolytic metastatic bone tumors, myelogenous
leukemia, milk-alkali syndrome, vitamin d intoxication, healing fractures,
renal failure, hypoparathyroidism, pseudohypoparathyroidism,
diabetes mellitus with ketosis, acromegaly, portal cirrhosis, pulmonary
embolism, lactic acidosis or respiratory acidosis.
2.6-4.5 mg/dl
Potassium
High potassium
levels are associated with reduced renal excretion of potassium or
redistribution of potassium in the body (i.e. Massive hemolysis, severe
tissue damage, severe acute starvation-anorexia nervosa, hyperkinetic
activity, malignant hyperpyrexia following anesthesia, hyperkalemic periodic
paralysis, and dehydration).
3.4-4.8
mmol/liter
Progesterone
The diagnostic
value of this test lies in its detection of ovulation and in the evaluation
of the function of the corpus luteum. Serial sampling during the
menstrual cycle is required. During menopause, levels drop to 0
Female
Follicular
phase
< 1 ng / ml
Midluteal
phase
3-20 ng/ml
Male
< 1 ng / ml
Prolactin
May help
assess Prolactin reserve and abnormal Prolactin secretion by the pituitary.
May indicate pituitary tumors.
Female
Premenopausal
0-20 ng/ml
Postmenopausal
0-15 ng/ml
Male
0-15 ng/ml
Prostate-specific
antigen (PSA)
PSA is
prostate-tissue specific, not prostate-cancer specific. Used for early
detection of the recurrence of prostatic cancer. The test is of great value
as a marker in the follow-up of patients at high risk for disease
progression. PSA values increase with age.
Female
0
Male
less than 40 years of age
0.0-2.0 ng/ml
greater
than or equal to 40 yr old
0.0-4.0 ng/ml
Prostate-specific
antigen (PSA), free, in males 45-75 yr old, with PSA values between 4 and 20
ng/ml
above 25%
associated with benign prostatic hyperplasia
Protein, total
High blood
levels may be associated with anabolic steroid use, androgens,
corticosteroids, coritcotropin, epinephrine, insulin, progesterone, or
thyroid preparations. Severe protein deficiency, chronic liver disease,
malabsorption syndrome, and malnutrition may also lead to abnormal levels.
Serum total protein decreases in the third trimester of pregnancy.
6.0-8.0 g/dl
Sodium
High serum
levels are associated with water loss in excess of salt through skin, lungs,
GI tract, and kidneys. Also may indicate increased renal sodium conservation
in hyperaldosteronism, Cushing's syndrome or disease, inadequate water intake
because of inadequate thirst mechanism, dehydration, or excessive saline
therapy. Low sodium levels may indicate low sodium intake, sodium losses due
to vomiting, diarrhea, excessive sweating with adequate water intake and
inadequate salt replacement, diuretics abuse, or salt-losing nephropathy
135-145
mmol/liter
Somatomedin C
(Insulin-like growth factor I)
Blood
concentrations of IGF-1 are constant during the day and after eating. In acromegaly,
the test may serve as an indicator of the severity of the disease; serial
determinations may be used to monitor efficacy of treatment. In dwarfism
IGF-1 may be used to determine the response to GH therapy. Concentrations of
IGF-1 rise during the first year of life, reaching the highest values in
preadolescent or early adolescent years. Normal values tend to decline
progressively until age 50
16-24
yr
182-780 ng/ml
25-39
yr
114-492 ng/ml
40-54
yr
90-360 ng/ml
> 54
yr
71-290 ng/ml
Testosterone,
total (morning sample)
This test is a
measure of total circulating testosterone, both protein bound and free. In
adult men, serum levels peak in the early morning, decreasing 25% to the
evening minimum. Levels increase after exercise and decrease after
immobilization and after glucose load. Progressive decreases begin after age
50
Female
6-86 ng/dl
Male
270-1070 ng/dl
Testosterone,
unbound (morning sample)
Free
(nonprotein-bound) testosterone is independent of changes in concentrations
of the principal testosterone transport protein, sex hormone-binding
globulin.
Female
20-40
yr
0.6-3.1 pg/ml
41-60
yr
0.4-2.5 pg/ml
61-80
yr
0.2-2.0 pg/ml
Male
20-40
yr
15.0-40.0
pg/ml
41-60
yr
13.0-35.0
pg/ml
61-80
yr
12.0-28.0
pg/ml
Thyroid-stimulating
hormone (TSH)
First-line
test for hyper- and hypothyroidism. Test is considered by some to be the
preferred screening test for evaluation of thyrometabolic states. Moderately
high TSH is often found in euthyroid patients during treatment of
hyperthyroidism.
0.5-5.0 U/ml
Thyroxine,
total (T4)
Used in
conjunction with other tests to measure thryoid function. T4
testing is frequently used when TSH levels are abnormally high or low. In
hypothyroidism, total serum t4 falls before t3. High
serum levels may represent hyperthyroidism.
4.5-10.9 g/dl
Transferrin
Transferrin is
the major plasma transport protein for iron. High serum levels may
indicate iron deficiency (high levels often precede the appearance of anemia
by days to months). Serum ferritin levels fall with iron deficiency and
with generalized malnutrition but remain normal in the presence of
inflammation and iron deficiency
191-365 mg/dl
Triglycerides
(fasting)
Increased
triglyceride levels indicate hyperlipoproteinemia types I, IIb, III, IV, and
V due to familial or sporadic endogenous hypertriglyceridemia. The following
primary disease states or conditions can lead to secondary elevation of
triglycerides: obesity, impaired glucose tolerance, viral hepatitis,
alcoholism, alcoholic cirrhosis, biliary cirrhosis, acute and chronic
pancreatitis, extrahepatic biliary obstruction, nephrotic syndrome, chronic
renal failure, essential hypertension, acute myocardial infarction, chronic
ischemic heart disease, cerebral thrombosis, hypothyroidism, diabetes
mellitus, gout, pregnancy, glycogen storage diseases types I, II, III, and
IV, down syndrome, respiratory distress syndrome, Werner's syndrome, anorexia
nervosa, or idiopathic hypercalcemia. Low levels of triglycerides may
indicate chronic obstructive lung disease, brain infarction, hyperthyroidism,
hyperparathyroidism, lactosuria, malnutrition, malabsorption syndrome,
intestinal lymphangiectasia or end-stage parenchymal liver disease.
40-150 mg/dl
Triiodothyronine,
total (T3)
Used in
conjunction with other tests to measure thyroid function. High serum
levels may indicate hyperthyroidism while low levels may indicate
hypothyroidism. At least 80% of circulating T3 is derived
from monodeiodination of T4 in peripheral tissues. T3
is 4 to 5 times more potent in biological systems than T4
60-181 ng/dl
Urea nitrogen
(BUN) (adult)
High serum
blood levels may indicate impaired kidney function associated with an
increase with age or protein content of diet.
8-25 mg/dl
Uric acid
High serum
levels may indicate gout, renal failure, leukemia, lymphoma, psoriasis,
polycythemia, multiple myeloma, kidney disease, and or chronic lead
nephropathy. Associated with hyperlipidemia, obesity, hypertension,
arteriosclerosis, diabetes mellitus, hypoparathyroidism, acromegaly, and
liver disease.
Male
3.6-8.5 mg/dl
Female
2.3-6.6 mg/dl
Differential
blood count
Reference
Range
Neutrophils
45-75%
Bands
0-5%
Lymphocytes
16-46%
Monocytes
4-11%
Eosinophils
0-8%
Basophils
0-3%
Erythrocyte
count
Red Blood Cell
count; filled with hemoglobin and specialized for carrying O2 and
CO2 (adult)
Male
4.50-5.30 X 106/mm3
Female
4.10-5.10 X 106/mm3
Ferritin
Surplus iron
is stored as Ferritin, primarily in the liver
Male
30-300 ng/ml
Female
10-200 ng/ml
Folate (folic
acid)
Water soluble
vitamin involved with amino acid metabolism & transfer of single-carbon
units in nucleic acid
Normal
3.1-17.5 ng/ml
Borderline
deficient
2.2-3.0 ng/ml
Deficient
< 2 ng / ml
Excessive
above 17.5 ng/ml
Hematocrit
(adult)
% of Red Blood
Cells present in total blood
Male
37.0-49.0
Female
36.0-46.0
Hemoglobin
(adult)
Oxygen-carrying
compound of blood. Numerical value of hemoglobin present in Red Blood
Cells
Male
13.0-18.0 g/dl
Female
12.0-16.0 g/dl
Iron
Constituent of
hemoglobin (transport of oxygen in blood) and enzymes involved in energy
metabolism
30-160 g/dl
Leukocyte
count (WBC)
White Blood
Cell (WBC); Central to the immune system that defends against infection
4.5-11.0X103/mm3
Mean
corpuscular hemoglobin (MCH)
Value is
calculated from hemoglobin and erythrocyte count. MCH= Erc÷Hb
25.0-35.0
pg/cell
Mean corpuscular
hemoglobin concentration (MCHC)
Mean cell
hemoglobin concentration is calculated from Hb and hematocrit (Hct)
MCHC=
Hct÷Hb
31.0-37.0 g/dl
Mean
corpuscular volume (MCV) (adult)
Mean cell
volume may not be reliable when a large number of abnormal erythroctes or a
dimorphic population of erythrocytes is present. It may also be calculated
from the hematocrit and erythrocyte count
MCV= Erc÷Hct
Male
78-100 m3
Female
78-102 m3
Platelet count
Helps mediate
the blood clotting that prevents loss of blood after injury
150-350X103/mm3
Platelet, mean
volume
6.4-11.0 m3

Published on April 03, 2013 15:11
March 31, 2013
Effective Hair Loss Treatment with Eyelash Growth Drug
Bimatoprost is known as the brand name Latisse. It was used for glaucoma for years and it was found that one of its side effects was eyelash growth. So it was approved for that purpose with the name Latisse. Emerging data show that this drug may also work to reverse hair loss in men and women.
Posted: 30 Mar 2013 07:24 AM PDT
Khidhir KG, Woodward DF, Farjo NP, et al. The prostamide-related glaucoma therapy, bimatoprost, offers a novel approach for treating scalp alopecias. Faseb J 2013;27(2):557-67. http://www.fasebj.org/content/27/2/557.long
Balding causes widespread psychological distress but is poorly controlled. The commonest treatment, minoxidil, was originally an antihypertensive drug that promoted unwanted hair. We hypothesized that another serendipitous discovery, increased eyelash growth side-effects of prostamide F(2alpha)-related eyedrops for glaucoma, may be relevant for scalp alopecias. Eyelash hairs and follicles are highly specialized and remain unaffected by androgens that inhibit scalp follicles and stimulate many others. Therefore, we investigated whether non-eyelash follicles could respond to bimatoprost, a prostamide F(2alpha) analog recently licensed for eyelash hypotrichosis. Bimatoprost, at pharmacologically selective concentrations, increased hair synthesis in scalp follicle organ culture and advanced mouse pelage hair regrowth in vivo compared to vehicle alone. A prostamide receptor antagonist blocked isolated follicle growth, confirming a direct, receptor-mediated mechanism within follicles; RT-PCR analysis identified 3 relevant receptor genes in scalp follicles in vivo. Receptors were located in the key follicle regulator, the dermal papilla, by analyzing individual follicular structures and immunohistochemistry. Thus, bimatoprost stimulates human scalp follicles in culture and rodent pelage follicles in vivo, mirroring eyelash behavior, and scalp follicles contain bimatoprost-sensitive prostamide receptors in vivo. This highlights a new follicular signaling system and confirms that bimatoprost offers a novel, low-risk therapeutic approach for scalp alopecias.
Possible Mechanism For The Stimulation Of Hair Growth By Bimatoprost
Bimatoprost stimulates eyelash growth in vivo, human scalp hair growth in organ culture, and mouse pelage hair growth in vivo. In our hypothesis, these effects are due to bimatoprost binding to appropriate receptors on the plasma membrane of cells in the regulatory dermal papilla in the hair bulb (middle panel). This probably stimulates intracellular signaling pathways, which trigger alterations in the gene expression of paracrine signals and their extracellular release. Some of these factors would leave the dermal papilla, crossing the basement membrane, isolating it from the rest of the follicle, to stimulate the coordinated activity of the keratinocytes and melanocytes to produce increased hair growth and pigmentation. Red dots indicate FP and/or prostamide F2α receptors, blue arrows indicate direction of movement of paracrine factors.
For more information on a compounded version of the drug: Click Here

Posted: 30 Mar 2013 07:24 AM PDT
Khidhir KG, Woodward DF, Farjo NP, et al. The prostamide-related glaucoma therapy, bimatoprost, offers a novel approach for treating scalp alopecias. Faseb J 2013;27(2):557-67. http://www.fasebj.org/content/27/2/557.long
Balding causes widespread psychological distress but is poorly controlled. The commonest treatment, minoxidil, was originally an antihypertensive drug that promoted unwanted hair. We hypothesized that another serendipitous discovery, increased eyelash growth side-effects of prostamide F(2alpha)-related eyedrops for glaucoma, may be relevant for scalp alopecias. Eyelash hairs and follicles are highly specialized and remain unaffected by androgens that inhibit scalp follicles and stimulate many others. Therefore, we investigated whether non-eyelash follicles could respond to bimatoprost, a prostamide F(2alpha) analog recently licensed for eyelash hypotrichosis. Bimatoprost, at pharmacologically selective concentrations, increased hair synthesis in scalp follicle organ culture and advanced mouse pelage hair regrowth in vivo compared to vehicle alone. A prostamide receptor antagonist blocked isolated follicle growth, confirming a direct, receptor-mediated mechanism within follicles; RT-PCR analysis identified 3 relevant receptor genes in scalp follicles in vivo. Receptors were located in the key follicle regulator, the dermal papilla, by analyzing individual follicular structures and immunohistochemistry. Thus, bimatoprost stimulates human scalp follicles in culture and rodent pelage follicles in vivo, mirroring eyelash behavior, and scalp follicles contain bimatoprost-sensitive prostamide receptors in vivo. This highlights a new follicular signaling system and confirms that bimatoprost offers a novel, low-risk therapeutic approach for scalp alopecias.
Possible Mechanism For The Stimulation Of Hair Growth By Bimatoprost
Bimatoprost stimulates eyelash growth in vivo, human scalp hair growth in organ culture, and mouse pelage hair growth in vivo. In our hypothesis, these effects are due to bimatoprost binding to appropriate receptors on the plasma membrane of cells in the regulatory dermal papilla in the hair bulb (middle panel). This probably stimulates intracellular signaling pathways, which trigger alterations in the gene expression of paracrine signals and their extracellular release. Some of these factors would leave the dermal papilla, crossing the basement membrane, isolating it from the rest of the follicle, to stimulate the coordinated activity of the keratinocytes and melanocytes to produce increased hair growth and pigmentation. Red dots indicate FP and/or prostamide F2α receptors, blue arrows indicate direction of movement of paracrine factors.
For more information on a compounded version of the drug: Click Here

Published on March 31, 2013 20:53
March 18, 2013
Testosterone+ HCG Preserves Healthy Sperm in Men on TRT
[image error]
Tung-Chin Hsieh,
Alexander W. Pastuszak, Kathleen
Hwang and Larry I. Lipshultz*,†
From the Division of Urology, University
of California-San Diego (TCH), San Diego, California, Scott Department of Urology, Baylor College of
Medicine (AWP, LIL), Houston, Texas, and Department of Urology (KH), Brown University School of Medicine, Providence, Rhode Island
Purpose: Testosterone replacement therapy results
in decreased serum gonadotropins (hormones produced by the pituitary gland- LH and FSH- that jump start testicular function) and intratesticular testosterone (inside the testicles), and impairs spermatogenesis (sperm production), leading to azoospermia (no viable sperm) in
40%
of patients. However,
intratesticular testosterone can be maintained during testosterone replacement therapy with co-administration of low dose human chorionic gonadotropin, which may support continued
spermatogenesis in
patients on testosterone replacement therapy.
Materials and Methods: We retrospectively reviewed
the records of hypogonadal men treated with testosterone replacement therapy
and concomitant low dose human chorionic gonadotropin (HCG). Testosterone replacement consisted of daily
topical gel or weekly intramuscular injection with intramuscular human chorionic gonadotropin (500 IU) every
other day.
Serum and free testosterone, estradiol, semen parameters and
pregnancy rates were evaluated before
and during therapy.
Results: A total of 26 men
with a mean age of 35.9 years were included in the study. Mean followup was 6.2 months. Of the men
19 were
treated with injectable
testosterone and 7 were treated with transdermal gel. Mean serum hormone levels before
vs during treatment were testosterone
207.2 vs 1,055.5
ng/dl
(p<0.0001),
free testosterone 8.1 vs 20.4 pg/ml (p = 0.02) and
estradiol 2.2 vs 3.7 pg/ml (p = 0.11). Pretreatment semen parameters were volume 2.9 ml, density 35.2 million per ml, motility 49.0% and forward progression 2.3. No differences in
semen
parameters were observed during greater
than 1 year of followup. No impact on semen parameters was observed as a function of
testosterone formulation. No
patient became azoospermic during
concomitant testosterone replacement and human chorionic gonadotropin therapy. Nine of 26 men
contributed to
pregnancy with the partner during followup.
Conclusions: Low dose human chorionic gonadotropin appears to maintain semen parameters in hypogonadal men on testosterone replacement therapy. Concurrent testosterone replacement and human
chorionic gonadotropin use may preserve fertility in
hypogonadal males who desire fertility
preservation while on testosterone replacement therapy.
***********************
Here is another study that showed that HCG at 500 IU every other day increased intratesticular testosterone in the absence of testosterone injections or gels (lower doses failed to achieve that):
http://www.ncbi.nlm.nih.gov/m/pubmed/15713727/
More information on HCG+TRT

Published on March 18, 2013 07:53
March 16, 2013
Most Men on Androgel and Testim Stop Using Them
Medication Adherence and Treatment
Patterns for Hypogonadal
Patients Treated with Topical
Testosterone Therapy: A Retrospective Medical Claims Analysis
Michael Jay Schoenfeld, MA, Emily Shortridge, PhD, Zhanglin Cui, PhD, and David Muram, MD
Eli Lilly and Company,
Indianapolis, IN, USA DOI:
10.1111/jsm.12114
[image error]A B S T R A C T
Introduction . There is limited information on adherence to topical
testosterone replacement therapy (TRT) among hypogonadal
men.
Aim . To determine adherence rates among
men treated with topical
testosterone gels and to examine factors
that may influence adherence, including age, presence of a specific diagnosis, and index dose.
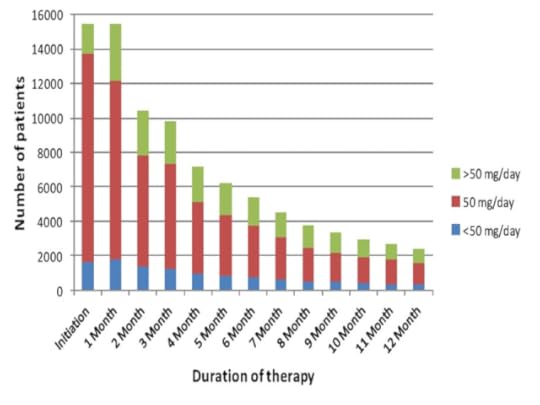
Methods . Included were 15,435 hypogonadal men, from the Thomson Reuters MarketScan® Database, who had an initial
topical testosterone prescription
in 2009 and who were followed
for 12 months.
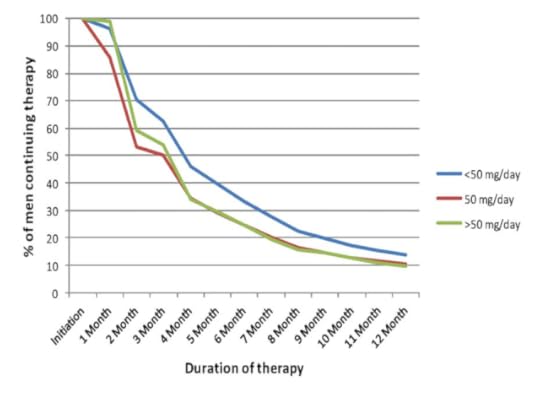
Mai n Outcome Measures. Adherence to testosterone was measured by medication possession ratio (MPR), with high adherence
defined as >0.8. Persistence was defined as the
duration of therapy from the index date to the earliest
of the following events: end date of the last prescription, date of the first gap of >30 days between
prescriptions, or end of the study period (12 months).
Results .
Adherence to topical
TRT was low. By 6 months, only
34.7% of patients
had continued on medication; at 12 months, only 15.4%. Adherence rates were numerically similar among men who received
AndroGel® or Testim® topical gels and did not differ among men of different age groups. Approximately 80% of patients initiated at the recommended dose of 50 mg/day. Over time, an increased proportion of
men used a higher dose. This change was
the result of dose escalation, rather than
of greater adherence
among men initiating
therapy
at a high dose.
Dose escalation was seen as early
as 1 month into therapy.
Approximately
50%
of men who discontinued treatment resumed therapy; most men used the same medication
and dose.
Conclusions . Discontinuation
rates are high among
hypogonadal men treated
with testosterone gels, irrespective of their age, diagnosis, and index dose. Further study, evaluating other measurable factors associated with low adherence among patients
receiving topical TRT, may lead to interventions designed to improve adherence
with therapy.
COMMENTS:
About 50% of patients who were followed over time resumed
TRT. It
is possible that some patients experienced alleviation of symptoms and were not sure they needed to remain on therapy. Once therapy
was discontinued and symptoms recurred in some patients, the benefits of
replacement therapy may have become clearer; thus,
prompting
these men
to restart
therapy at the same effective
dose.
An important
limitation of the study is that claims
data do not include important patient level data, such as symptoms, reasons
for discontinuation (e.g., application
method), side effects (e.g., skin reaction), testosterone levels, responses to therapy, and so forth.
While perception of efficacy has significant effect
on patient adherence, this study was
unable to assess
severity of symptoms or of symptomatic relief, once patients initiated therapy.
The study was unable to identify characteristics that were associated with the time patients would be on therapy
before treatment was interrupted or
who would resume
therapy after a brief
interruption. Most patients
who
resumed
therapy
did
so
by using
the same
topical TRT agent and the same dose they used prior to the interruption. It is possible
that these patients
perceived efficacy,
were proficient in the application method, and possibly had a prescription that
they
were able to use or refill
without the need
for an office visit.
Only a small percentage of patients
using topical
therapy resumed therapy
by using a different method
or a change
in the dosing regimen.
Lesson:
Patients on testosterone should have their blood levels and symptoms evaluated after a few weeks on therapy. Depending on these follow up results, dose adjustment or change of delivery method should be explored as well as other issues that may potentially affect efficacy and adherence (life style, other medications, body mass index, etc). Expectations should also be clearly described at the start of therapy (for more on what to expect, read this ) so that patients have realistic views. Stamina and sexual function are multifactorial and testosterone blood levels are only part of the puzzle.

Published on March 16, 2013 05:59



