Leslie Glass's Blog, page 424
November 15, 2017
Why Your Grumpy Teenager Doesn’t Want to Talk to You
Adolescence
By LISA DAMOUR
Most parents have seen their teenager start the day in a reasonably good mood, but then return from school draped in gloom and chilly silence. As hard as it can be to support our children when they tell us what’s wrong, it’s that much harder to help the obviously upset adolescent who turns down a warm invitation to talk.
These interactions usually unfold in an awkward and predictable sequence. We earnestly ask, “Is everything O.K.?” and our teenager responds with a full stop “No,” an insincere “Yeah,” or freezes us out while fielding a flurry of texts. We then tend to nurse a sense of injury that our teenager has rebuffed our loving support.
But when adolescents hold their cards close to their chests, they often have a good reason. To better ease our own minds and be more useful to our teenagers we can consider some of the ordinary, if often overlooked, explanations for their reticence.
They Worry We’ll Have the Wrong Reaction
Our children often know us better than we know ourselves, having spent their young lives learning our reflexive responses. When a teenager feels lousy about bombing a test but knows that you are likely to tell her that she should have studied more, she won’t be eager to talk.
If you suspect this might be a barrier and can listen without getting defensive, just ask, “Are you worried that I’ll have a bad reaction?” You might start a valuable conversation — even if it’s not the one you were looking for — while paving the way to better talks down the line. And we should probably think twice about the long-term implications of saying “I told you so” to our teenagers (even when we did tell them so).
They Anticipate Negative Repercussions
Parents focused on the narrow question of what went wrong can forget that our adolescents, who have more information than we do, are probably thinking about a bigger picture. Impassive silence can hide a teenager’s whirring deliberations: “Will Dad limit my driving privileges if I tell him that I put a ding in the car?” or “If I explain that Nikki had a pregnancy scare, will Mom be weird about it when I want to hang out with her next weekend?”
We can’t always keep ourselves from feeling judgmental about teenagers. And, to be sure, there are adolescents (and adults) who get stuck in worrisome ruts. But as a psychologist, there are two rules I live by: good kids do dumb things, and I never have the whole story.
Recognizing that teenagers (and, again, adults) screw up from time to time can improve communication. On the days when they do feel like sharing, we can alert adolescents to our compassionate and forgiving stance by saying, “I know you’re bummed about the car. How do you want to make this right?” or “That must have been really scary for Nikki. Is she doing O.K.?”
They Know That Parents Sometimes Blab
Teenagers are often justly concerned that we might repeat what they tell us. Sometimes we only realize in retrospect that news we divulged to others felt top-secret to our teenager. And sometimes they tell us critical information — such as word of a suicidal classmate — that must be passed along.
Whether you owe your teenager an apology for past indiscretions or are trying to get ahead of the issue, I think it’s fair and kind to promise adolescents a very high degree of confidentiality at home. Our teenagers deserve to have a place where they can process, or at least dump, delicate details about themselves or the scores of other kids with whom they must find a way to coexist.
Parents, like therapists, can lay out the limits of what we can keep private. Adolescents are usually sensible; they expect adults to act on news that they or a peer might be in immediate danger. But we can help teenagers speak more freely by making it clear that, barring a crisis, we will keep their secrets and offer moral support as they and their friends weather typical adolescent storms, such as painful breakups. And when our teenagers do share critical information about their peers, we can include them in the process of deciding how to pass along what they’ve told us.
Talking Doesn’t Feel Like the Solution
A wise teenager in my practice once said to me, “You know, I’m 90 percent of the way over what happened at school by the time I get home. Rehashing it all for my mom isn’t going to help me get past it.”
Even when we don’t know the source of our child’s turmoil, we should operate from the assumption that our teenager will soon feel better. Of course there are real grounds for concern when adolescents are miserable day after day and cannot bounce back from their emotional downturns. But most of the time psychological well-being is like physical well-being: Healthy people fall ill, but they recover.
We don’t take our adolescents’ viruses personally and we probably shouldn’t take their grumpy moods personally, either. Happily, the support we offer the flu-stricken also works when teenagers come down with grouchy silence. Without delving into what’s wrong, we can ask if there’s anything we can do to help them feel better. Would they like our quiet company or prefer some time alone? Is there a comfort food we can offer or is there something they want to watch on TV?
There’s more value in providing tender, generic support than we might imagine. It is difficult for teenagers to maintain perspective all the time. The speed of adolescent development sometimes makes teenagers lose their emotional footing and worry that they will never feel right again. We send our teenagers a powerful, reassuring message when we accept and are not alarmed by their inscrutable unease: I can bear your distress, and you can, too.
The post Why Your Grumpy Teenager Doesn’t Want to Talk to You appeared first on Reach Out Recovery.
To Maintain Muscle and Lose Fat as You Age, Add Weights
By GRETCHEN REYNOLDS
Trying to stay trim as you age? Surprisingly, if you’re cutting calories to lose weight, adding weights to your weight loss regimen may be more effective than beginning a walking program, according to a new study that adds to growing evidence that weight training is important for vigorous aging.
Successful weight loss is never easy, as most of us know from experience, and becomes more difficult with age. Instead of losing or maintaining weight as we grow older, most of us gain a pound or two each year during middle age.
At the same time, we also often begin naturally to lose some of our muscle mass, so that our bodies wind up increasingly composed of fat.
This change in body composition matters, because fat tissue is less metabolically active than muscle. As the percentage of our body composed of fat tissue rises, our metabolic rates fall and we burn fewer calories throughout the day, predisposing us to continued weight gain.
We also become less strong, of course, as our muscles shrink.
So most experts agree that the ideal weight-loss program for most people would maximize fat loss while sparing muscle mass.
But this balance is difficult to achieve, since, typically, when we drop a pound while dieting, as much as a third of that loss can come from muscle, with the rest composed of fat.
Some past studies have hinted that exercising while cutting calories might help to lessen this muscle loss. But most of those studies have been small and involved relatively young people or only one gender.
For the new study, which was published this month in Obesity, researchers at Wake Forest University in Winston-Salem, N.C., and other institutions decided to focus on both men and women older than 60. They also set out to enroll African-American as well as the Caucasian participants most earlier studies used.
In the end, they wound up with 249 participants who were overweight or obese and sedentary.
The researchers measured their body compositions and leg-muscle strength and assessed their current diets.
Then they randomly assigned the volunteers to one of three groups. Some began a basic calorie-reduction plan, during which they cut their food intake by an amount expected to help them lose 7 to 10 percent of their body weight over the coming months. For most of them, this meant a reduction of about 300 calories per day.
The members of this group were asked not to exercise.
Another group also cut their calorie intake. But at the same time, they began a supervised aerobic exercise program consisting of walking briskly on a track for 45 minutes four times per week.
The third group likewise reduced calories but also began a weight-training program. Four times a week, they worked with trainers at a gym to complete a full-body resistance training routine using weight machines.
All of the volunteers continued their particular program for 18 months.
By the end of that time, everyone had dropped weight.
But there were notable differences in the amount and type of weight that had been lost in each group.
The men and women in the group that had cut calories but not worked out had lost an average of about 12 pounds each.
Those who had cut calories and walked had dropped far more weight, about 20 pounds each, while those who had dieted and weight trained likewise had lost about 20 pounds per person.
But the weight loss among walkers and weight trainers was qualitatively different, their new body-compositions scans showed. The weight trainers had lost about two pounds of muscle and 18 pounds of fat, while the walkers had dropped about four pounds of muscle and 16 pounds of fat.
The group that had dieted and not exercised had lost about two pounds of muscle.
In effect, the walkers had lost more muscle mass in total and as a percentage of their weight loss than either of the other two groups, including those who had not exercised at all.
That finding surprised the researchers, says Kristen M. Beavers, an assistant professor of health and exercise science at Wake Forest and the study’s lead author.
It would have worried them, too, she says. But subsequent tests of muscular strength showed that, relative to their new, lower body weights, the men and women who had exercised in any way had stronger legs than they had had 18 months before.
Those who had remained sedentary did not have stronger legs.
So although they had dropped some muscle mass, the walkers had gained leg strength. (The researchers did not test upper-body strength.)
But over all, the study’s results imply that walking could have limitations as a weight-loss aid for older dieters, Dr. Beavers says.
“Walking is excellent exercise,” she says. “But it looks as if it might not produce enough of an anabolic signal to really spare muscle mass during weight loss.” In other words, it may not prompt older people’s bodies to hold on to muscle as effectively as weight training seems to do, she says.
Of course, an experiment like this cannot tell us why, at the molecular level, different types of exercise alter the composition of weight loss or whether the results would be the same for younger people or those who were not unfit.
But the results do suggest, Dr. Beavers says, that for healthy weight loss, many of us might consider at least occasionally walking to the gym and, once there, picking up some weights.
The post To Maintain Muscle and Lose Fat as You Age, Add Weights appeared first on Reach Out Recovery.
November 14, 2017
Researchers: Cultural factors take backseat in eating disorder treatment
Cultural and social factors that might affect the development of eating disorders are largely ignored in treatment, even when a patient actively seeks to address them, a new research report suggests.
Researchers from the University of East Anglia in the United Kingdom say gender issues that could be related to eating disorders have been pushed aside amid an emphasis on evidence-based treatment and cognitive-behavioral therapy. Treating professionals might ignore a patient’s request to talk about gender issues because they lack experience in this area or because they see the topic as relatively unimportant.
“The bottom line is that, although eating disorders are now widely recognized as being shaped by biological, psychological and social factors, the social aspect of the equation is poorly served,” said lead researcher Su Holmes, of the university’s School of Art, Media and American Studies. The paper was published in the journal Eating Disorders.
Holmes and a university occupational therapist developed an inpatient treatment intervention in which female patients with anorexia attended 10 weeks of group sessions examining topics such as gender-related constructions of appetite, cultural expectations surrounding female emotion, and the dynamics of healthy-living standards targeting women. The participating women appreciated the intervention’s examination of broad contexts that shape ideas about gender in society, Science Daily reported.
Holmes emphasizes, however, that gender identity issues in the development of eating disorders are not relegated to women only. “The focus on how eating and body distress may be ued to negotiate dominant ideas about gender and sexuality is similarly applicable to male patients, as well as gender minorities, even whilst the cultural constructions at stake may be different,” she said.
The post Researchers: Cultural factors take backseat in eating disorder treatment appeared first on Reach Out Recovery.
How To Talk To Teens About A Parent’s Substance Use
Talking to teens about family substance use is difficult, whether a parent’s or sibling’s. Without the full understanding of what is happening to a loved one, however, we can’t further the process of healthy communication and healthy living. Family dysfunction can only thrive in silence.
By utilizing these guidelines, you can help your teen to understand and cope with the substance use disorder that is harming the family.
Step One: What To Talk About
Open up the subject by giving some basic information to cover the following subjects:
What is addiction
It doesn’t happen overnight. Explain the stages and disease process that occurs with increased use and how substances and alcohol affect brain function. Explaining basic addiction facts and how behavior changes, helps you to educate yourself. Talk with teens about family substance use as if it were cancer or any other progressive disease in an educated, non-judgmental manner. Education is the power to see that addictions are quite common, that you are not alone, and that you can help both the user and the rest of the family.
What are the consequences of addictions
Looking at common consequences helps to frame this information as a part of the addiction picture. This helps teens understand that consequences need to be provided for addictive behaviors, and that consequences are not punishment. Talking about consequences, like traffic accidents, falls, overdoses, arrests, getting fired, losing friends, and financial difficulties help to focus the substance users on their behavior and what must change.
What recovery opportunities are available
By looking at the hope of recovery for family substance use, adolescents can have a sense that much can be done to help the loved one who’s ready for treatment, or already in treatment. Discuss with them 12-step meetings, sponsors, other support groups, or individual or group counseling, intensive outpatient counseling, or inpatient treatment programs for the addict. Let them know that they can be a part of their own recovery through individual counseling, 12-step meetings, support groups, or family therapy that can occur with or without the addict present.
What specific information can be shared about partner’s or child’s addiction
Acknowledge what the kids have seen and experienced with family substance use (such as a parent coming home from work drunk, a sister getting expelled for getting caught smoking pot on her lunch hour). Do not keep these events secret because that maintains family dysfunction and in reality, your teen already has seen the behaviors and may know more than you do (especially about a sibling). However, there are some behaviors that may be inappropriate to talk about – healthy boundaries takes precedence over telling all. If you wonder about this, talk to a therapist about these boundaries.
Step Two: When to talk about family substance use
Talk when you are calm, when there is a quiet time with no distractions. During a fight or the aftermath of a fight is not a good time to rationally discuss the issues facing the family. Don’t lash out with information, for example, while you’re threatening the loved one, or the loved one is screaming back. Times of high drama are not ideal for family meetings. Also, be open any time the teen might want to discuss this, and perhaps set up times for safe talk.
Step Three: How to have the conversation
First of all be calm and listen. While this is a very difficult and painful subject, it needs to be addressed in a quiet and non-judgmental way. The whole family needs to feels safe exploring it. After the subject is raised, then you listen…listen…and listen some more. As always, the focus on inappropriate behaviors caused by substance use disorder that the partner or adolescent is demonstrating, not the person. This also includes a focus on how they family can aid in the recovery of the substance user (if appropriate) as well as recovery for the family itself.
Addictions are difficult but you can be a positive example for your teenager/s regarding empowering, healthy ways to help them cope as well as how to help your entire family to deal with difficult situations. Remember that taking action is a powerful way to help your teen to go beyond the struggles into embracing recovery.
The post How To Talk To Teens About A Parent’s Substance Use appeared first on Reach Out Recovery.
FDA warns on use of kratom to treat opioid addiction amid links to 36 deaths
Kratom is an unapproved substance touted as a treatment for depression, pain, anxiety and even opioid addiction. (iStock)
The FDA issued a public health advisory on Tuesday over the use of kratom, an unapproved botanical substance that originates from Thailand, Malaysia, Indonesia and Papua New Guinea. The warning comes amid an increase in popularity in the U.S., where kratom is touted as a treatment for pain, anxiety, depression and even as an opioid alternative.
“It’s very troubling to the FDA that patients believe they can use kratom to treat opioid withdrawal symptoms,” said FDA commissioner Scott Gottlieb, in part. “There is no reliable evidence to support the use of kratom as a treatment for opioid use disorder. Patients addicted to opioids are using kratom without dependable instructions for use and more importantly, without consultation with a licensed health care provider about the product’s dangers, potential side effects or iterations with other drugs.”
The advisory warned that kratom produced similar effects to narcotics, carrying the risk of abuse, addiction and even death. The FDA noted a 10-fold increase in calls made to U.S. poison control centers regarding kratom from 2010 to 2015, and reports of 36 deaths linked to the substance.
“There have been reports of kratom being laced with other opioids like hydrocodone. The use of kratom is also associated with serious side effects like seizures, liver damage and withdrawal symptoms,” Gottlieb said.
Additionally, the FDA said it has identified kratom products on two import alerts, and is working to prevent shipments of the substance from entering the U.S., as well as detained hundreds of shipments at international mail facilities.
“We’ve learned a tragic lesson from the opioid crisis: that we must pay early attention to the potential for new products to cause addiction and we must take strong, decisive measures to intervene,” Gottlieb said. “From the outset, the FDA must use its authority to protect the public from addictive substances like kratom, both as part of our commitment to stemming the opioid epidemic and preventing another from taking hold.”
The post FDA warns on use of kratom to treat opioid addiction amid links to 36 deaths appeared first on Reach Out Recovery.
FDA warns of the deadly herb kratom, citing 36 deaths

Scott Gottlieb, commissioner of the Food and Drug Administration, testifies during a House Energy and Commerce Committee hearing last month on federal efforts to combat the opioid crisis. On Tuesday, the FDA issued a public health warning saying there was no evidence that the herb kratom was effective in treating opioid addictions. (Drew Angerer/Getty Images)
The Food and Drug Administration Tuesday issued a strong warning to consumers to stay away from the herbal supplement kratom, saying regulators are aware of 36 deaths linked to products containing the substance.
Consumers are increasingly using the supplement, which comes from a plant in Southeast Asia, for pain, anxiety and depression, as well as symptoms of opioid withdrawal. Because it produces symptoms, such as euphoria, similar to opiates, it is also used recreationally. Proponents say it is a safe way to deal with chronic pain and other ailments, and some researchers are exploring its therapeutic potential, including helping people overcome addictions.
But in a statement, FDA commissioner Scott Gottlieb said there is no “reliable evidence” to support the use of kratom as a treatment for opioid-use disorder, and that there are no other FDA-approved uses of kratom.
Rather, he said, evidence shows that the herb has similar effects to narcotics like opioids, “and carries similar risks of abuse, addiction and, in some cases, death.” He said that calls to U.S. poison control centers involving kratom increased 10-fold between 2010 and 2015, and that the herb is associated with side effects including seizures, liver damage and withdrawal symptoms.
Last year, the Drug Enforcement Administration proposed banning the use of kratom. But the agency backtracked after public outcry and pressure from some members of Congress. It asked the FDA to expedite a scientific and medical evaluation and a recommendation for how to handle the compounds in kratom.
The herb is banned in several states, such as Indiana, Tennessee, Alabama, Arkansas and Wisconsin. Gottlieb said the FDA is treating kratom as an unapproved drug and also has taken action against kratom-containing dietary supplements. If the plant is useful in treating various conditions, it should go through the agency’s regular drug-approval process to provide it is safe and effective, he added.
Meanwhile, the FDA is working to prevent shipments of kratom from entering he country, he said.
The post FDA warns of the deadly herb kratom, citing 36 deaths appeared first on Reach Out Recovery.
Codependent Offers Hot Cocoa To Make Amends
I’ve reached the point in recovery where I need to make amends. My husband thought this day would never come. He’s been waiting for over a decade for me to admit I was wrong, but before I address his concerns, I must make amends to one of my closest friends. I was actually in charge of caring for this girl for a number of years. To hold me accountable, I’m sharing this letter with you.
Dear Kay,
This is the hardest letter I’ll ever write. Where do I begin? How can I ask for your forgiveness when I know I don’t deserve it?
I’m Sorry For Calling You fat
I’m sorry I said you were ugly, and I don’t hate your nose, like I said so many times. When faced with a choice of praising you or being critical, I always criticized. If I tell you I love your hair, how it’s dark brown waves naturally wrap into beach-blown curls, will that begin to erase the hundreds of hurtful things I’ve said? Does it help that I think your cheerful smile is reminiscent of a younger Julia Roberts?
I Confess I May Have Lied About The Food I Served You
Ok, that’s still not true. I totally lied to you; I’m so ashamed. I completely dismissed your special dietary needs. That gluten-free blueberry pie wasn’t remotely gluten free. Neither were the gluten-free waffles. I feel awful, but gluten-free foods are so expensive. As I watched you eat those unhealthy foods, which were mildly toxic to you, I saw your health decline, yet I said nothing. In fact, I encouraged you. Not only did I dismiss your wishes, but I discounted your physician’s advice.
Even Worse I Stole Money From You
I knew you were building a savings account for emergencies, and I sabotaged your efforts. More than once, I took money from your grocery fund and treated my husband to Starbucks, or I bought a new toy for my son. Sometimes when I was tired, I borrowed a little here or there to eat out so I wouldn’t have to cook. Most of the time, I meant to pay you back, but that never happened. My irresponsibility often left you short on money for gas and food. Your nest egg is gone; your credit card is maxed; and you have nothing to show for it. I’ve cost you thousands over the years.
I Was Ruthless About Home Improvement Projects
Regarding our home-improvement “projects,” I didn’t give you enough time or money to complete them, yet I demanded perfection. I should’ve known laying tile was a skilled trade. Or that you really can’t cut hardwood flooring with a utility knife. I taunted you to the point of tears, and I was ruthless if you didn’t deliver.
I Forced You To Negotiate With The Evil One
Even though it should have been your husband’s job, I forced you to negotiate with your mother-in-law. But you were the only one selfless enough to keep peace. When I realized your happiness was worth more than appearing happy, it was too late. Above all, I regret talking you out of standing up to her. I don’t know why I stopped you. She was awful.
I Must Make Amends
The words, “I’m sorry,” are hollow and have little value; still, they need to be said. In the rooms of recovery, I’m learning to make living amends, so from now on, I’ll be putting you first. Your feelings and values are my top priority. If you say “No,” I’ll respect you. It will take time, but I will change, one day at a time. From now on, my love for you will match my actions.
Love, Pam
This Is A Letter To Me From Me
For years, I put everyone else first and was hardest on myself. Treating a child or a spouse like would be abusive, but self-abuse is difficult to see. In recovery, I’m learning self-care isn’t selfish, so I’ll be making living amends to me. I have books to read, nails to polish, and naps to take. Most importantly, I’m setting myself free from my self-imposed prison.
Gluten-Free, Easy on the Budget Hot Cocoa
A cup of milk
1 Tablespoon of baking cocoa
1 Tablespoon of sugar
½ teaspoon of vanilla
1 pinch of salt
Pour milk, cocoa, sugar, vanilla, and salt into small sauce pan. Heat on medium, and whisk ingredients together. Whisking eliminates bitter clumps of cocoa and makes the milk frothy. Enjoy with a good book.
The post Codependent Offers Hot Cocoa To Make Amends appeared first on Reach Out Recovery.
Recovery Protects Everyone’s Family Rights
According to my Mother, my brother Ricky needs extra love and care because of his addiction. My family rights are ignored. She always favors what’s right for Ricky. In recovery, I learn I have rights too.
My birthday is on the 4th of July. Last night my Mom told me, “We can’t go to your favorite restaurant, El Taco Loco,” said my Mom, “because they serve beer. Ricky can’t go to restaurants that serve alcohol. Besides,” she added, “Ricky has a meeting on Tuesday nights. We’ll have to celebrate your birthday on Wednesday instead.”
I sound petty, but this isn’t an isolated incident. It’s just the latest in a series of injustices. When we were kids, I had very strict rules. Ricky didn’t. If I disobeyed, I faced harsh consequences. Ricky had “different” punishments because “You just can’t yell at Ricky.” Or “Spanking doesn’t work on Ricky.”
In our teenage years, I fixed dinner, did laundry, washed dishes, and mowed the yard. Ricky had no chores because he wouldn’t do them anyway. I had to pay my way through college. Ricky got bailed out of jail, and my parents paid for his rehab. Twice. Today, Ricky still lives at home with a built-in maid and babysitter, our Mom. Because she does so much for Ricky, she doesn’t have any or energy left to spend time with me and my son.
Ricky Isn’t The Problem
Who do I blame for all of these injustices? For many years, I despised Ricky. I was jealous and angry. When I learned that alcoholism, also known as alcohol use disorder, affects the whole family, I saw more of the picture. My Dad’s drinking also contributed to our problems. For years, my Dad acted out under the influence. My Mom reacted. This became their dysfunctional dance. When Ricky and I came along, we learned their dance moves. These are the generational sins of alcoholism. Unfortunately, identifying the problem doesn’t undo the hurt.
When I came to recovery, I learned that addiction was a disease. I grew less angry at Ricky, but I became furious with Mom. Over time (many, many months), I grew to accept my painful past. I am working on forgiving my Mom. I learned that what happened, happened to me. It doesn’t define me.
I Have Rights Too
One of the best things I’ve learned in recovery is I am equal to Ricky. My Mom has always favored Ricky. Instead of rewarding the successful child, she rushes to the one in need. This speaks of her illness, not of my character. Recovery has given me a new family of trustworthy people who love me unconditionally. This helped heal many of my emotional hurts.
Family Rights Let Everyone Recover
Family healing doesn’t happen overnight. Ricky and I have both been in recovery for a few years, but progress is in recovery is slow. Recovery isn’t a magic 8-ball that delivers the answers to all family conflicts. How do we move forward in a healthy way when we are still working hard to overcome our dysfunctional habits? I’m proposing we adopt The Family Recovery Bill Of Rights. Each person has the right to:
Respect and compassion
Be safe from yelling
Have personal boundaries
Speak and express feelings
Take care of yourself
Ask for what you want
Follow a recovery program
Be trusted when trust is earned
Equal treatment for all
Your own safe space
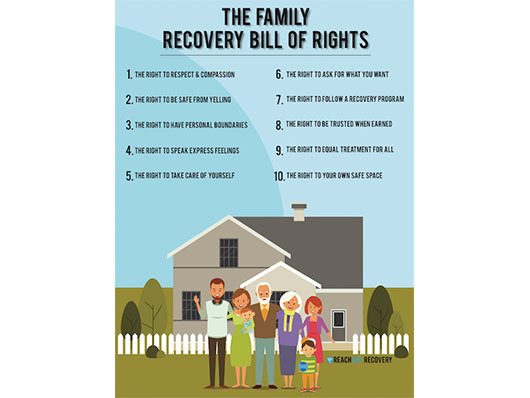
These guidelines protect everyone’s best interest. If, or more likely, when Ricky, my Mom, and I disagree, I take a minute to review my rights. This document reminds me that I don’t have to lose just so Ricky can gain. I can brainstorm for win/win solutions. I can set boundaries to protect myself. I don’t have to blindly trust those who have hurt me. No one can change the past, but I can protect myself now and in the future. It gives me independence in a chemically dependent family.
Save
The post Recovery Protects Everyone’s Family Rights appeared first on Reach Out Recovery.
Sex Addiction And Celebrities
Fox News’ Dr. Manny sits down with two psychologists to discuss what kind of help patients actually get at these expensive facilities and if they work.
As Hollywood’s sexual assault scandal widens with further accusations, reports have emerged that actor Kevin Spacey checked himself into The Meadows treatment facility in Wickenberg, Ariz., the same rehab center where movie mogul Harvey Weinstein is also allegedly seeking treatment.
But at $37,000 a month, what kind of help do patients actually get as these expensive facilities? Dr. Robi Ludwig, a psychotherapist who has treated sex addicts, said many of these rehab centers treat sex addicts similar to how other addiction programs for alcoholism or drug abuse do.
“There’s a supportive treatment environment where you can be amongst other people who are having similar struggles. There’s group therapy, there’s individual therapy, there’s medication management. And it’s just like anything else, it works as good as you work,” Ludwig told Fox News.
In most facilities, inpatient sexual addiction treatment involves a 30- or 60-day stay in a gender-separate facility.
Programs often focus on separating the addict from their addiction or the people, places and things that trigger that addiction.
Psychologist Dr. Kathryn Smerling said identifying triggers can be a big and important step for recovery.
“They should constantly be examining their triggers. For example, if they struggle with internet porn, get a wall that blocks these sites or just cut your WiFi at home completely,” Smerling told Fox News.
The term “sex addiction,” which is also known as Hypersexual disorder, has been hotly debated over. Some experts don’t believe sex addiction exists in the same way as other addictions. In fact, a diagnosis of “sex addiction” has not been added to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
Some specialists describe sex addiction as; a progressive intimacy disorder characterized by compulsive sexual thoughts and acts.
Specific criteria or symptoms for hypersexual disorder were proposed for the DSM-5 in 2010 and included (for a period of at least six months); recurrent and intense sexual fantasies, urges, or behaviors, which were not related to some other mental condition or substance abuse; A pattern of the person using sex as a response to depression, stress or other negative moods or states.
Smerling said there’s never just one cause for addiction.
“It’s usually a multitude of factors- biological, psychological, and social. There can be changes in the brain elicited by compulsion. Psychological risk for any addiction such as sex includes depression, anxiety, and being obsessive compulsive. Anyone who struggles with incredibly low self-esteem and seeks approval or childhood self-esteem that was never dealt with properly,” Smerling told Fox News.
According to The National Council on Sexual Addiction Compulsivity, 6 to 8 percent of Americans are sex addicts, which is about 18 to 24 million people.
“I know that Harvey Weinstein probably had a bunch of people that were covering for him, and same for Kevin spacey, but people who are ‘ordinary’ people who have sex addictions, often lay in bed and masturbate for days, they will go and get risky sex partners and all kinds of things that are not masked by other things,” Smerling added.
The post Sex Addiction And Celebrities appeared first on Reach Out Recovery.
FDA Approves Digital Pill That Tracks When Patients Take It
The system offers doctors an objective way to measure if patients are swallowing their pills on schedule, opening up a new avenue for monitoring medicine compliance that could be applied in other therapeutic areas. (iStock)
U.S. regulators have approved the first digital pill with an embedded sensor to track if patients are taking their medication properly, marking a significant step forward in the convergence of healthcare and technology.
The medicine is a version of Otsuka Pharmaceutical Co Ltd’s established drug Abilify for schizophrenia, bipolar disorder and depression, containing a tracking device developed by Proteus Digital Health.
The system offers doctors an objective way to measure if patients are swallowing their pills on schedule, opening up a new avenue for monitoring medicine compliance that could be applied in other therapeutic areas.
Shares in Otsuka rose 2.5 percent on Tuesday after news of the U.S. Food and Drug Administration (FDA) late on Monday.
The FDA said that being able to track ingestion of medicines prescribed for mental illness may be useful “for some patients”, although the ability of the digital pill to improve patient compliance had not been proved.
“The FDA supports the development and use of new technology in prescription drugs and is committed to working with companies to understand how technology might benefit patients and prescribers,” said Mitchell Mathis of the FDA’s Center for Drug Evaluation and Research.
The system works by sending a message from the pill’s sensor to a wearable patch, which then transmits the information to a mobile application so that patients can track the ingestion of the medication on their smartphone.
About the size of a grain of salt, the sensor has no battery or antenna and is activated when it gets wet from stomach juices. That completes a circuit between coatings of copper and magnesium on either side, generating a tiny electric charge.
In the longer term, such digital pills could also be used to manage patients with other complicated medicine routines, such as those suffering from diabetes or heart conditions.
Poor compliance with drug regimens is a common problem in many disease areas, especially when patients suffer from chronic conditions.
Proteus has been working on the pill tracking system for many years and the sensor used in Abilify MyCite was first cleared for use by the FDA in 2012.
The unlisted Californian company has attracted investments from several large healthcare companies, including Novartis AG, Medtronic Inc and St. Jude Medical Inc, as well as Otsuka.
Abilify MyCite is not approved to treat patients with dementia-related psychosis and contains a boxed warning alerting health care professionals that elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death.
The post FDA Approves Digital Pill That Tracks When Patients Take It appeared first on Reach Out Recovery.



