Leslie Glass's Blog, page 301
January 31, 2019
3 Truths About Anxiety That Will Help You Feel Better, Fast
From Yoga Journal:
There are many words we might use to describe how anxiety makes us feel: uncomfortable, scared, unsettled, conflicted, anxious, antsy, nervous, attacked, unsafe, and out of control. But there is one thing that almost everyone can agree on: It feels bad. In fact, anxiety is often described to me as a deep-seated feeling that something bad is happening or is about to happen.
But anxiety may not be what you think. Which can make it really hard to heal.
Despite popular belief, anxiety is not “just fear” that can be worked through with enough therapy. And while anxiety can be linked to certain medical and psychiatric conditions, many people who struggle with anxiety have seen doctor after doctor with no relief.
Is it time to look at anxiety in a new way?
The feeling of something bad happening, even if there is no medical condition, is actually quite accurate because something bad is happening inside of you. Your body is feeling unresolved emotional energy, or baggage, that’s stuck in your system.
Anxiety comes from your body being in freak-out mode, not because of what’s happening outside of you but because of what’s stuck inside of you. While external circumstances outside of your control certainly may trigger you, that is not the actual origin of anxiety.
The feeling of anxiety arises because your body is trying so hard to keep old emotional baggage contained, and it’s just too much for anyone to hold. Anxiety manifests when stored emotional energy is trying to bubble up and out. Anxiety can be caused by any emotional baggage that you have not dealt with. I’ve seen as many people with anxiety due to suppressed anger and frustration as due to fear.
To heal anxiety, you first need to understand it. Here’s 3 truths that will help you do just that.
1. Anxiety Shows Up In Sneaky Ways
Many people have anxiety and yet have absolutely none of the typical symptoms you might imagine. Knowing how anxiety is showing up in your life can help you be more aware of how it’s affecting you.
Anxiety can manifest in ways you may not even be aware of, including:
• Negative, compulsive, or obsessive thoughts
• Needing to be in control of life and others
• Inability to relax
• Difficulty making decisions
• Being too hard on yourself
• Resistance to accepting help from others
• Feeling shaky or unstable
• Feeling sad, angry, or pretty much any other difficult emotion
• Being moody
• Inability to concentrate
• Digestive upset
• Heartburn
• Fatigue
2. Anyone Can Be Affected by Anxiety
Many believe that only weak or highly emotional people get anxiety. People who experience anxiety often feel bad about themselves, feeling delicate and unable to handle life in the way that others can. Sometimes these perceptions do actually become beliefs that perpetuate anxiety. Imagine subconsciously telling yourself all day, “I can’t handle life” or “I’m so delicate.” Nothing could be further from the truth.
Many people who experience anxiety have a constitutional makeup or personality traits that actually tend toward anxiety, such as being highly empathic, overachieving, self-sacrificing, self-critical, or always being the “strong” one or a Type-A perfectionist who prides themselves on keeping everything under control.
Anxiety sufferers are often in leadership and caretaking roles and are able to “do or conquer anything.” These are awesome personality traits. However, these people may also take on the world at the expense of themselves.
3. One Reason You Can’t “Just Get Over It”
Many anxiety sufferers are told that it’s all in their head and they should just get over it, take deep breaths, or don’t stress so much. It’s not hard to end up feeling like anxiety is your fault—that if only you had more willpower or discipline you could fix this. But, of course, it’s not nearly that easy. One of the reasons it’s impossible to take that approach is because your body is stuck in freak-out mode.
When your body is stuck in fight, flight, or freeze—or what I call freak-out mode—it’s very difficult to heal. This freak-out mode is linked to the triple warmer meridian (an energy pathway in your body’s energy system), which governs the fight, flight, or freeze response in the body. It affects the nervous system, immune system, and so much more. This freak-out response essentially creates a feeling of danger in your whole system. Anxiety is not just in your head; it’s in your entire body. In order to fully heal, you need to train your body to be relaxed and calm. In other words, you need to get your body out of freak-out mode and into healing mode.
Emotions that you felt in the past can get lodged in the body and contribute to this freak-out mode. When they become stuck, you are essentially feeling each of those emotions (which can number in the hundreds or thousands) at a low level all the time. So it’s no surprise now why you’re feeling so uncomfortable, right? In addition, the sheer force of having to “hold” all of these unexpressed emotions can create a sense of anxiety.
How to Heal Anxiety
There are many ways to deal with stuck emotions that contribute to anxiety. Thymus tapping is one of them.
The thymus gland is the master gland of the body’s immune system and is located in the upper part of the chest, behind the breastbone. It sits right over the heart. The thymus is vital to the healthy functioning of the immune system and is connected to the entire energy system and is so powerful that it can work as a stress modulator when stimulated.
A lot of people are naturally drawn to the thymus area when they are feeling anxious and don’t even realize that their body is trying to help them tend to this special gland.
How to Use Thymus Tapping: First, try to tune into the anxiety and ask yourself: “If there was an emotion under this anxiety, what would it be?” Remember, anxiety happens from suppressing emotions. That’s why identifying the true emotion your body is very helpful. Next, tap the thymus gland using your fingertips to help your body release that stuck emotion. Don’t try to push it away; allow it to be. Tapping will help usher it out of your body if you allow it to come up.
As you tap, you can say, “releasing this _______ (say the emotion)” a few times. Take some deep breaths. Repeat until you feel relief.
Now that you know these truths about anxiety, your new job is only to honor them—and trust that your healing is right around the corner.
The post 3 Truths About Anxiety That Will Help You Feel Better, Fast appeared first on Reach Out Recovery.
January 30, 2019
Exercise May Improve Thinking Skills In People As Young As 20
From Science Daily:
Regular aerobic exercise such as walking, cycling or climbing stairs may improve thinking skills not only in older people but in young people as well, according to a study published in the January 30, 2019, online issue of Neurology®, the medical journal of the American Academy of Neurology. The study also found that the positive effect of exercise on thinking skills may increase as people age.
The specific set of thinking skills that improved with exercise is called executive function. Executive function is a person’s ability to regulate their own behavior, pay attention, organize and achieve goals.
“As people age, there can be a decline in thinking skills, however our study shows that getting regular exercise may help slow or even prevent such decline,” said study author Yaakov Stern, PhD, of Columbia University in New York, and a member of the American Academy of Neurology. “We found that all participants who exercised not only showed improvements in executive function but also increased the thickness in an area of the outer layer of their brain.”
The study involved 132 people between the ages of 20 and 67 who did not smoke or have dementia but who also did not exercise at the start of the study and were determined to have below average fitness levels. Participants were randomly assigned to six months of either aerobic exercise or stretching and toning four times a week. The two groups were equally balanced for age, sex, education as well as memory and thinking skills at the start of the study.
All participants either exercised or stretched and toned at a fitness center and checked in weekly with coaches monitoring their progress. They all wore heart rate monitors as well. Participants’ thinking and memory skills were evaluated at the start of the study as well as at three months and at the end of the six-month study.
Participants in the exercise group chose from aerobic activities including walking on a treadmill, cycling on a stationary bike or using an elliptical machine. They ramped up their activity during the first month, then during the remainder of the six-month study they trained at 75 percent of their maximum heart rate. People in the stretching and toning group did exercises to promote flexibility and core strength.
Researchers measured participants’ aerobic capacity using a cycling machine called an ergometer that estimates exercise intensity. Participants also had MRI brain scans at the start and end of the study.
Researchers found that aerobic exercise increased thinking skills. From the beginning of the study to the end, those who did aerobic exercise improved their overall scores on executive function tests by 0.50 points, which was a statistically significant difference from those who did stretching and toning, who improved by 0.25 points. At age 40, the improvement in thinking skills was 0.228 standard deviation units higher in those who exercised compared to those who did stretching and toning and at age 60, it was 0.596 standard deviation units higher.
“Since a difference of 0.5 standard deviations is equivalent to 20 years of age-related difference in performance on these tests, the people who exercised were testing as if they were about 10 years younger at age 40 and about 20 years younger at age 60,” Stern said.
He added, “Since thinking skills at the start of the study were poorer for participants who were older, our findings suggest that aerobic exercise is more likely to improve age-related declines in thinking skills rather than improve performance in those without a decline.”
Researchers also found an increase in the thickness of the outer layer of the brain in the left frontal area in all those who exercised, suggesting that aerobic exercise contributes to brain fitness at all ages.
“Our research confirms that exercise can be beneficial to adults of any age,” said Stern.
Overall, researchers did not find a link between exercise and improved memory skills. However, those with the genetic marker for dementia, the APOE ?4 allele, showed less improvement in thinking skills.
A limitation of the study is the small number of participants. Larger studies over longer periods of time may allow researchers to see other effects in thinking and memory skills.
The post Exercise May Improve Thinking Skills In People As Young As 20 appeared first on Reach Out Recovery.
Data Show No Evidence That Teens’ Social Media Use Predicts Depression Over Time
From Science Daily:
Longitudinal data from adolescents and young adults show no evidence that social media use predicts later depressive symptoms, according to research published in Clinical Psychological Science, a journal of the Association for Psychological Science. However, the findings do show that relatively higher depressive symptoms predicted later social media use among adolescent girls.
This research stands in contrast with recent claims that adolescents’ use of social media may lead to depression, claims based primarily on studies that examined associations between average social media use and average well-being measured at a single point in time.
“You have to follow the same people over time in order to draw the conclusion that social media use predicts greater depressive symptoms,” says lead author Taylor Heffer of Brock University. “By using two large longitudinal samples, we were able to empirically test that assumption.”
Beginning in 2017, Heffer and coauthors surveyed 6th, 7th, and 8th graders in Ontario, Canada once a year for two years. The researchers also conducted annual surveys of undergraduate participants, beginning in their first year of university over a span of 6 years.
To measure depressive symptoms, the researchers used the Center for Epidemiological Studies Depression Scale for the young adults and an age-appropriate version of the same scale for the adolescents. All participants answered two questions about their average daily hours spent on social media — one measuring weekday use and the other measuring weekend use. The participants also answered questions about other screen time, such as watching TV, and non-screen activities including doing homework and exercising.
Heffer and colleagues analyzed the data separately for each age group and gender.
The results showed that social media use did not predict later depressive symptoms among adolescents or college undergraduates. Rather, greater depressive symptoms predicted more social media use over time, but only among adolescent girls.
“This finding contrasts with the idea that people who use a lot of social media become more depressed over time. Instead, adolescent girls who are feeling down may turn to social media to try and make themselves feel better,” says Heffer.
Overall, the research suggests that the fear surrounding social media use and its impact on mental health may be premature.
“When parents read media headlines such as ‘Facebook Depression,’ there is an inherent assumption that social media use leads to depression. Policymakers also have recently been debating ways to tackle the effects of social media use on mental health,” says Heffer.
Evaluating whether fears about the impacts of social media have merit requires prospective longitudinal studies that allow researchers to examine whether it is social media use that predicts depressive symptoms (rather than the other way around), while controlling for other potential influences. As Heffer and colleagues note, individual differences in personality, motivation, and current well-being are likely to play a critical role in the relationship between media use and future well-being.
“There may be different groups of people who use social media for different reasons,” Heffer explains. “For example, there may be a group of people who use social media to make social comparisons or turn to it when they are feeling down, while another group of people may use it for more positive reasons, such as keeping in contact with friends.”
Examining the role that these differences play will help clarify the ways in which social media interacts with mental health, with implications for parents, policymakers, and healthcare professionals alike.
The post Data Show No Evidence That Teens’ Social Media Use Predicts Depression Over Time appeared first on Reach Out Recovery.
January 29, 2019
Adult Children Of Alcoholics: Meeting Basic Needs
In 1978, Tony A. wrote The Laundry List: 14 Traits of an Adult Child of an Alcoholic. Since then, other equally powerful lists have been written, including: The Other Laundry List, The Flip Side of The Laundry List, and The Flip Side of The Other Laundry List. (You can read all of the lists here.) This information is invaluable BUT overwhelming. Today, we’re focusing on list items that relate specifically to caring for our most basic needs.
Breaking Down The Laundry List
We can get better, and taking small slow steps are the key. Item numbers 6 and 7 from Tony A.’s original list explain how our ability to care for ourselves is affected:
“We have an overdeveloped sense of responsibility and it is easier for us to be concerned with others rather than ourselves; this enables us not to look too closely at our own faults, etc.”
“We get guilt feelings when we stand up for ourselves instead of giving in to others.”
What Is An Overdeveloped Sense Of Responsibility?
Being an adult child of an alcoholic means when we were kids, we had responsibilities beyond our years. I, for example, knew how to kill and clean a chicken before I entered high school. As a teenager, I spent my summers caring for other people’s children. I had two after school jobs by the time I was 16.
Because this is all we know, we tend to marry people who are OK with our super sense of self-reliance and selflessness. Probably because we called it ambition. As parents, we’re extremely over-protective because we’ve already had years of experience in high-stress parenting.
When I first found recovery, I was so enmeshed with my husband and son that I felt deep shame for spending 20 minutes alone in my bedroom to do my 12-step homework! Making myself slow-down to put on body lotion was a major accomplishment, and it took MONTHS for me to buy MY favorite foods at the grocery store. Little did I know, taking these small steps to care for myself was essential to my recovery.
It’s More Than Self-Care; It’s Self-Parenting
Per the ACA’s Flip Side Of The Other Laundry List, when:
We accept and comfort the isolated and hurt inner child we have abandoned and disavowed, we thereby end the need to act out our fears of enmeshment and abandonment with other people.
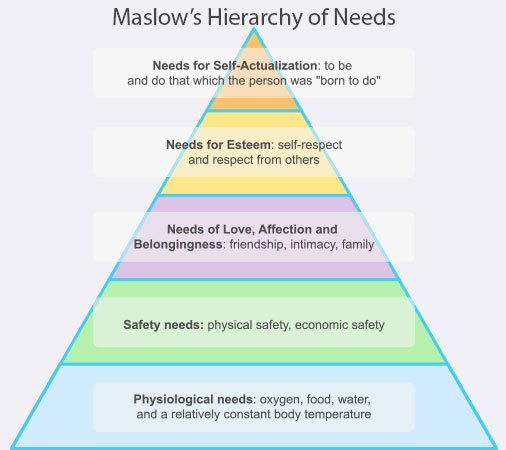
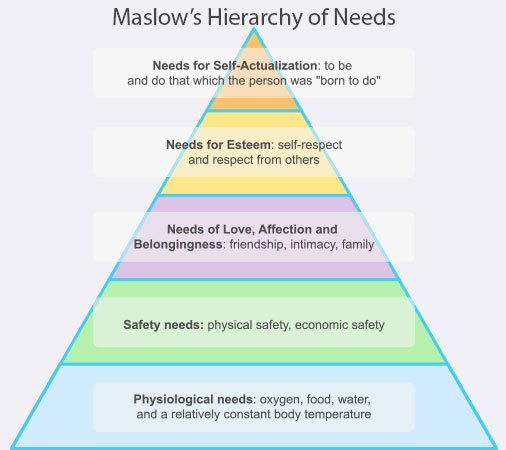
To heal, we have to go back, find, and meet the needs of that inner child who got lost along the way. American psychologist Abraham Maslow explained that our most basic need is for physical survival, and this will be the first thing that motivates our behavior. Once our basic physiological needs are fulfilled, we’ll naturally be motivated to fill the next level of needs.
Meeting My Basic Needs
When I first began recovery, I couldn’t meet my basic physical needs. I had no money for groceries because I was paying the minimum amount due on every outstanding debt. Never getting ahead, my debt grew. I stood in more than one food pantry line before I was willing to try something different. Finally, I took Dave Ramsey’s Financial Peace University.
Dave’s teachings coincide with Maslow’s Hierarchy of Needs. I learned to get out of debt, I had to protect my four walls, which included basic necessities, like:
Food
Shelter (including utilities)
Basic clothing and
Transportation
Thanks to recovery, now instead of feeling guilty for buying the healthy foods I like at the grocery store, I buy groceries first before paying any bills. I select the best in fruits, veggies, and meats. I savor the time spent making healthy meals for myself. Instead of being thought of as selfish as I feared, my family is sharing my delicious meals with me. It’s a slow, sweet healing.
Feeling Safe Somewhere
Once my condition stabilized, I was then strong enough to tackle my safety needs. I made a safe space in my home. My husband and son are both energetic, enthusiastic, loud people. Watching sports with them triggers me, as I’m afraid of angry people. To me, loud means angry. This trait is item #3 on Tony A.’s list:
“We are frightened by angry people and any personal criticism.”
About 18 months ago, I set up my bedroom as a “storm shelter”. It’s equipped with a bathroom, shower, reading materials, candles, and my pets food and water bowls. If I need to, I can hunker down in my room and ride out any emotionally angry storm, whether real or imagined by me. Hanging outside my room is a sign with this Melody Beattie quote,
“If you want to act crazy, that’s your business, but you can’t do it in front of me. Either you leave, or I will walk away.”
At first, I went there often, sometimes in an angry huff. Sometimes the door would be locked all night. Gradually, I felt safer and more free. Now I often sit in bed reading with the door open. I almost never hide, and usually, my family stops by to visit.
What’s The Next Self-Care Step?
Maslow’s Hierarchy of Needs is an excellent unbiased tool from a renowned psychologist. Every person deserves to have these basic needs met. Yet, we are fantastic resisters. Here are a few questions to hold ourselves accountable:
When is the last time you’ve been to the Doctor? Or Dentist? Or Eye Doctor?
Think of your most favorite health foods. Are you using them to fuel your body? Do you make the time to prepare and eat when you are hungry?
Are you getting enough sleep or do you work in the wee hours of the night promising you’ll catch up on the lost sleep tomorrow?
Do you still attend stressful family meals or dinners with angry friends because you don’t want to rock the boat?
Are you actively participating in one-way relationships?
Are you willing to find a sponsor or counselor to help you work through these issues?
More important than which item we tackle first is when we get started. An old Chinese problem says,
‘The best time to plant a tree is twenty years ago. The second best time is today.”
The post Adult Children Of Alcoholics: Meeting Basic Needs appeared first on Reach Out Recovery.
Signs of Depression Can Be So Subtle Even Doctors Miss Them
From Dr. Keith Roach @ Men’s Health: When I broke up with my first serious girlfriend (well, she did the breaking up), I was naïve, egocentric, and convinced I could think my way out of anything. I was also 17 years old, which may explain a large part of that. I was intensely sad, but the sadness didn’t go away. I had just moved from California to Chicago, right at the beginning of my senior year in high school, and felt I had a perfect explanation why I felt down all the time. I thought of it as a sign that my relationship was so deep and powerful that I looked at my feelings with a sense almost of pride.
Weeks went by and I continued not to take pleasure in anything. Things that should have made me happy didn’t. I didn’t look forward to anything. I had a hard time falling asleep at night, and I woke up with a physical pressure sensation on my chest and my beloved’s name on my lips. Dying of consumption seemed a romantic notion (I read a LOT of nineteenth century literature). But it wasn’t until I had unbidden thoughts of who should get all my stuff when I died that I realized that something was really wrong. It was briefly clear to me that the depth of feeling I had—despair is not too strong a term—was affecting me far more deeply than I thought it could. In a strange way, this gave me a sense of relief. It’s not that I felt better, merely that I could identify where my mental and physical symptoms were coming from.
I didn’t talk to my parents, to my sister, or to any of my friends about it. It wasn’t that I was ashamed, it just didn’t occur to me to do so. It certainly didn’t cross my mind to see a doctor: I was seventeen years old and in perfect health. The idea I might not be in perfect mental health didn’t even cross my mind.
Six months went by, and as my first winter in Chicago started to turn to Spring, I slowly began to feel myself again. I enjoyed time with friends. I started to do better in school and to take interest in academics again, rather than going through the motions.
It wasn’t until years later, in medical school, that I finally realized that I had been through a pretty textbook case of major depressive disorder. It was a bit of a shock reading about it. The diagnosis of depression is clinical, meaning that it comes from an experienced clinician doing a careful interview and exam, and not from blood testing or imaging studies. Experience is essential because interpreting the answers to the questions requires judgment: it isn’t always a simple yes or no answer, despite the fact that the official diagnostic criteria (from the psychiatric reference book called the DSM-5) sound like yes or no questions:
Depressed mood most of the day
Loss of interest or pleasure in most or all activities
Too much or too little sleep
Weight loss or weight gain; or increase or decrease in appetite
Moving and speaking more slowly (or much faster) than normal
Fatigue or low energy
Decreased ability to concentrate, think, or make decisions
Thoughts of worthlessness or inappropriate guilt
Recurrent thoughts of death, or thinking about or attempting suicide
Five or more of these criteria for almost every day for two or more weeks meet the diagnosis of major depressive disorder (but that has to include one of the first two listed). There are some conditions that exclude the diagnosis: symptoms cannot be due to another medical condition (uncommon); may not be due to drug use or withdrawal (not as uncommon); and if these occur with episodes of mania or hypomania (times of extreme energy, often associated with poor judgment), the diagnosis is not unipolar depression but bipolar disorder. The symptoms have to be severe enough to cause significant distress or psychosocial impairment.
Psychiatrists are the experts in making the diagnosis, but primary care doctors like me are the ones who most frequently do make the diagnosis—although they may not catch it every time. It’s now recommended for physicians to screen patients for major depression, but there will still be people like me who have symptoms but don’t bring themselves to medical attention. It’s much easier to treat if you do check in with a doctor. What else to do:
Get One Of The Leading Treatments
There are two major treatment options for major depression: medications and psychotherapy. Some people have strong feelings about these treatments. Each is effective on its own; a combination of the two is even more effective. There are many different types of drug treatments, and a clinician will choose one based on their best guess of effectiveness and side-effects in an individual. There is increasing evidence that testing for genetic variants can help precisely guide the best medication for an individual; however, this is not yet recommended in general, and I have used it only when a patient has not had success in finding an effective treatment.
Psychotherapy often makes people think of many sessions undergoing analysis on a couch: this type, called psychodynamic therapy, is not the way therapy is typically done for depression. Interpersonal therapy addresses a person’s relationships, and is intended to change behaviors with family and friends and lasts for 3-4 months, typically, as opposed to psychodynamic therapy, which addresses unresolved childhood issues and unconscious feelings, and typically lasts for years. Cognitive behavioral therapy is another short-term treatment which helps people learn how to understand their feelings and beliefs, and gives exercises to improve awareness of these and make changes to improve them. Both of these therapies have been shown to be effective in depression.
Lose The Idea That It’s Something To Be Hidden
Even in 2019, there remains a stigma to mental illness, and many people (especially men) feel that depression is a sign of weakness, and they are loath to admit it, to themselves or to people who might help them. This is a barrier I have had to fight many times. I tell people that they can’t control whether they get high blood pressure, but that it can be treated, and treatment reduces the risk of harms. Depression is similar. Untreated, it leads to a higher likelihood of bad outcomes that aren’t just about continuing to feel depressed; they include effects on other people (family, friends, work); a higher likelihood of drug and alcohol abuse; and the biggest danger of all, suicide. Depression can be a fatal illness.
Beware Being Number One
Men are at higher risk for suicide. Although men and women are about equal in thinking about suicide and in suicide attempts, men are much more likely to be successful. We’re number one, but this is not an area where men want to be leading the way. Treatment of depression in somebody contemplating, or worse, planning, suicide is a little different. Also, a person’s age determines not only their risk for suicide (older men are at the highest risk of all), but also how treatment affects suicidal risk. A medicine like Prozac (fluoxetine), for example, increases suicide risk in adolescents and young adults (at least in the short term), but decreases risk in older men.
Know It Will Get Better—But You May Not See That
One barrier to treatment of depression is the depression itself. Some people have an overwhelming fatigue that prevents them from going to see someone about it. If you are suffering, this means you need to make the effort. Get some help from family or friends in making the appointment. If you are the family or friend who’s seeing signs of depression in someone, you can help by helping to get them to an appointment. Assist them in finding a therapist in their network, offer to drive them to an appointment, help with child care if appropriate, or find some other way to reduce the barriers to getting there. One common finding in depression is an inability to see that things can ever get better. This sense of hopelessness is a cruel facet of the issue that prevents proper treatment. However, treatment is effective at restoring hope.
Stay Vigilant To The Signs
Once a person has had an episode of depression, future bouts are much more likely than in a person who hasn’t: one study found that 13 percent of people had a recurrence within 5 years, 23% within 10 years, and 42% within 20 years. Fortunately, most people have a much easier time recognizing symptoms the second time around and are faster to seek care. Nobody who has had severe depression and who has gotten better wants to feel that way again.
It’s been well over 30 years since I have had depression. I know I am at risk in the future, and in times of stress, I have been vigilant about paying attention to my own feelings. Everyone has ups and downs, but feeling down most days for more than 2 weeks would be a red flag. I also recommend being forthright with the people that matter most: if they recognize that I am not myself they can feel safe in letting me know so that I could get treatment sooner. I don’t want to feel that way, and my family, coworkers, and friends don’t want that for me either.
The post Signs of Depression Can Be So Subtle Even Doctors Miss Them appeared first on Reach Out Recovery.
11 Male Celebrities Open Up About Anxiety
From Jordyn Taylor @ Men’s Health: Do you ever have worry or fear that goes way beyond what a situation calls for? Do you find yourself plagued by jitters, stomachaches, and racing thoughts you can’t seem to control? If so, you might be dealing with anxiety.
Anxiety disorders are the most common mental illness in the U.S., according to the Anxiety and Depression Association of America. In fact, 40 million adults over 18 years old experience some form of anxiety every year.
Lots of guys have anxiety—including some of your favorite celebrities. What’s more, they’re using their platforms to bring awareness to mental health issues and encourage other men to get help. Here are 11 celebrities with anxiety.
Clark Gregg
Clark Gregg, who plays Agent Phil Coulson in the Marvel Cinematic Universe, opened up about his anxiety and panic attacks in an op-ed for Men’s Health in 2018. He said cognitive behavioral therapy—aka CBT—has been a “game-changer.”
“I find it calming to know that wherever I am, I don’t have to wonder if I have a pill nearby; I just know I can do these exercises, and it’s going to become manageable,” he said.
Ryan Reynolds
“I have anxiety. I’ve always had anxiety,” the Deadpool actor told the New York Times in 2018.
“I have three older brothers,” he said. “Our father was tough. He wasn’t easy on anyone. And he wasn’t easy on himself. I think the anxiety might have started there, trying to find ways to control others by trying to control myself. At the time, I never recognized that. I was just a twitchy kid.”
Carson Daly
In 2018, NBC’s Carson Daly revealed he has generalized anxiety disorder.
“I was a worrywart kid. I was always worrying,” he said on the Today show. “My father died when I was 5. I had an ulcer when I was in high school. I’ve been nervous my whole life.”
Michael Phelps
“Throughout my career, I struggled with depression and anxiety at various times, and I found it so difficult to get the help I needed,” the Olympic swimmer said in a 2018 statement on his partnership with the therapy app Talkspace.
At a Talkspace event in October of 2018, Phelps gave Men’s Health some helpful tips for managing mental health issues.
Zayn Malik
Shortly after cancelling a concert due to “extreme anxiety,” pop star Zayn Malik explained in an essay for Time why he decided to go public with his mental health issues.
He wrote:
“One of my team members offered to write a statement saying that I’d been taken ill, but I didn’t want to do that. I was done with putting out statements that masked what was really going on. I wanted to tell the truth. Anxiety is nothing to be ashamed of; it affects millions of people every day. I know I have fans out there who have been through this kind of thing, too, and I wanted to be honest for their sake, if nothing else.
“When I was in One Direction, my anxiety issues were huge but, within the safety net of the band, they were at least manageable. As a solo performer, I felt much more exposed, and the psychological stress of performing had just gotten to be too much for me to handle—at that moment, at least. Rather than hiding away, sugar-coating it, I knew I had to put it all out there.”
Royce White
Pro basketball player Royce White has been open about having generalized anxiety disorder and a fear of flying. “”It’s a day-by-day struggle for me,” he told CNN in 2012.
White has also advocated for the NBA to update its mental health policy.
Charlamagne Tha God
In October of 2018, the radio host released a memoir called Shook One: Anxiety Playing Tricks on Me. Earlier in the year, Charlamagne Tha God talked about his struggles with anxiety and panic attacks in an op-ed for Men’s Health.
“I have had anxiety literally my whole life,” he said. “When you’re young and running the streets, you think all of that paranoia and anxiousness comes with the territory. As you get older, when you’re damn near 40, and life is good and you still have those feelings…that’s when you know something is wrong.”
Mardy Fish
In 2012, Mardy Fish pulled out of the US Open before facing off against Roger Federer. He cited “health reasons,” which turned out to be the symptoms of severe anxiety disorder, according to USA Today.
“It’s OK not to be OK,” he told the outlet in 2017. “To show weakness, we’re told in sports, is to deserve shame. But showing weakness, addressing your mental health, is strength.”
Rick Ankiel
In 2000, former professional baseball player Rick Ankiel suddenly lost his ability to pitch—and severe anxiety turned out to be the culprit, according to USA Today.
“For anyone who hasn’t had it happen to them, they don’t understand how deep and how dark it is,” he told the publication in 2017. “It consumes you. It’s not just on the field. It never goes away. … It’s this ongoing battle with your own brain. You know what you want to do—in your heart. But your body and brain won’t let you do it.”
In 2017, Ankiel published a best-selling book called The Phenomenon: Pressure, the Yips, and the Pitch That Changed my Life.
Darryel McDaniels
In a 2018 op-ed for Men’s Health, Run DMC’s Darryel “D.M.C.” McDaniels said he didn’t know he had a problem until he finally got help for his mental health issues, which included substance abuse.
“I had anxiety that I didn’t know was anxiety. I had panic attacks that I didn’t know were panic attacks. Any time I felt something I considered abnormal, I just reached for the bottle,” he said.
Harry Styles
In One Direction’s official autobiography, Who We Are, singer Harry Styles revealed that he deals with anxiety.
“I suffered some pretty serious confidence issues when I first appeared on stage,” he wrote. “I’m naturally a fairly confident person in most situations, but not all. At that point any natural confidence I had was being taken over by nerves because back then I had no idea how to channel and control my anxiety.
“One Direction have always been a band that gigs heavily, so over time I’ve been able to learn about nerves, to understand why and when they might hit and, best of all, how to control them.”
The post 11 Male Celebrities Open Up About Anxiety appeared first on Reach Out Recovery.
13 Signs Of Exhaustion & 5 Ways To Recover
From Alice Boyles, Ph.D. @ Psychology Today: Here are some signs you’re exhausted. Perhaps you’ve been overworking and scraping the bottom of the barrel of your energy for too long, or perhaps you’re slightly depressed. Another scenario is that you’re chronically anxious or in physical pain, and that’s wearing you down. If you’re experiencing more than a few of these symptoms of exhaustion, then you need to change your coping strategies.
Note: If the exact example doesn’t fit your situation, but you relate to the general principle it illustrates, you can still check that item.
1. Doing slightly unpleasant tasks that will take under five minutes still feels overwhelming and triggers procrastination (e.g., taking out the trash or emptying your vacuum cleaner).
2. If you pump yourself up briefly (e.g., through listening to an upbeat song), it works momentarily, but leaves you feeling totally wiped out afterwards.
3. You only eat food you can microwave or eat straight out of the package.
4. You have several hours per day when all you’ve got the energy for is watching videos or clicking around the internet. Even reading a book would feel like too much effort.
5. There’s something you should be doing to manage a medical condition, like taking a medication or using an ointment, but you don’t have the energy or willpower to do it consistently.
6. You keep doing tasks in inefficient ways, because organizing yourself is beyond you. For instance, you keep buying food for one or two meals rather than doing a big grocery shop for the full week. (This is a self-sabotaging pattern I cover in-depth in my book, The Healthy Mind Toolkit).
7. You consume short bites of content (e.g., YouTube videos), because at the end of your workday, you don’t have the concentration left for anything longer.
8. You put off small tasks that, if not attended to promptly, could turn into expensive (or otherwise onerous) problems. For example, the oil light comes on in your car, and you just ignore it for a few days.
9. You let your children have hours of screen time, because you’re too tired to have a battle over it or to do activities with them (e.g., read to them).
10. You wake up still feeling tired.
11. If you have a partner, you ignore their relationship-related complaints, because you haven’t got the mental space to deal with their emotional needs.
12. You spend time each day doing something that feels like it’s just wasting your life. For instance, you go on social media everyday. You find it unfulfilling, but you do it anyway. You don’t have the energy to break the habit and plan an alternative activity.
13. You don’t have the energy to plan or set goals, such as you’d like to plan a vacation, but you can’t muster the energy to organize it. Or, you know you need to return an item by a certain date. You think about it daily, but then let the date go by, because you just can’t be bothered.
Suggestions to Address Exhaustion
Have a few early nights to give yourself a reset.
Invest in yourself for a couple of weeks. Instead of pushing yourself for other people (e.g., your job, friends, or family), save some of that energy to refill your tank.
Check any potential physical causes of how you’re feeling, such as low iron or low B12. This is mainly relevant if you know you haven’t been eating well, or you’re a vegetarian, but there can be other causes of feeling tired all the time, like sleep apnea or under-active thyroid. Ask your family doctor to check for physical causes of low energy.
Try something different from how you’ve been coping recently. For instance, if you read a lot of self-help, but have never seen a therapist, try it. You can also try strategies you’ve used at other times in your life, but not recently. For instance, when you were younger, you used to go to yoga for stress, but you haven’t been in years. Or you used to take baths or run to unwind, but now rarely do.
Learn strategies that will help you break the cycle of being a hamster on a wheel. Create more energy for planning and organization, which will gradually lower your stress over the long term.
Give yourself more support. If you’ve reached the level of exhaustion indicated by these examples, it’s time to stop trying to go it alone. The support you need and can access could be medical, child care, therapy, other practical support, or anything that would feel supportive to you.
The post 13 Signs Of Exhaustion & 5 Ways To Recover appeared first on Reach Out Recovery.
January 28, 2019
Doctor Recommends Marijuana For 4-Year-Old Boy
From Soumya Karlamangla @ LA Times: A Hollywood physician could lose his medical license after recommending that a father give his 4-year-old son marijuana cookies to control temper tantrums, according to California’s medical board.
Dr. William Eidelman, a natural medicine physician, improperly diagnosed the boy with attention deficit hyperactivity disorder and bipolar disorder before recommending marijuana as the treatment, the medical board said in a decision announced last month.
The board ordered the doctor’s license revoked as of Jan. 4. However, his lawyers say a judge stayed the order so his license is active and he continues to practice.
The penalties against Eidelman stem from his treatment of a young boy who was misbehaving in school and brought to the doctor’s office by his father in September 2012, according to the medical board report.
Much of Eidelman’s practice centers on writing letters for patients to obtain medical marijuana, which he said he began doing in 1997, shortly after the state first legalized the drug for medical use.
After a 30-minute visit with the boy and his father, the doctor wrote in his chart that the child had a “probable combination of ADD/ADHD and bipolar disorder” and should “try cannabis in small amounts in cookies,” according to the medical board’s decision.
The boy appeared nervous and agitated but not “abnormal,” according to an interview with the doctor that was included in medical board documents.
The doctor had previously recommended cannabis for the father’s ADHD and bipolar disorder, according to the board report.
The board found Eidelman “grossly negligent” for determining the boy’s diagnosis without consulting a psychiatrist, collecting information from the boy’s teachers, or asking his father about the child’s moods and sleep patterns.
“Tantrums alone … do not support either diagnosis,” the board’s decision said. “‘Being agitated’ and ‘having trouble sitting still’ hint at ADHD, but could simply hint at a preschooler not happy to have driven many miles to a doctor’s appointment.”
The board did not find fault with Eidelman for recommending marijuana to a child. The decision states that there is not enough scientific evidence to disprove that cannabis could have benefits for children.
“It has not been established, by clear and convincing evidence, that the recommendation of medical marijuana to [the boy], with his father’s consent, violated the standard of care,” the decision reads.
However, the board still views the recommendation for cannabis as improper, because the boy did not actually have the conditions that Eidelman diagnosed him with and for which he prescribed the cannabis.
The decision also took into account that Eidelman had been previously punished for prescribing marijuana to several undercover investigators in 2000 and 2001.
Though the medical board says Eidelman’s license has been inactive for the last three weeks, the doctor’s attorney, Tracy Green, said the doctor can legally practice medicine.
She said that she appealed the board’s decision before the revocation took effect, and that a San Francisco County Superior Court judge ordered that the revocation be halted, pending a hearing in March.
Eidelman, 69, said in an interview last week: “The judge ruled that the revocation is stayed, so yes, I’m still practicing.”
The online register of actions in the case in Superior Court does not include the judge’s stay. The judge’s clerks could not be reached for comment.
The medical board website lists Eidelman’s license as revoked.
“The Medical Board of California has not received a court order indicating that the revocation was stayed,” said medical board spokesman Carlos Villatoro in an email. “Accordingly, Eidelman’s license is currently revoked.”
Practicing medicine without a license can be punished with up to a year of jail under California law.
According to the medical board case documents, the 4-year-old’s father had tried more traditional medicines, such as Ritalin, for his own ADHD as a child and found them not only unhelpful but harmful. He said he felt like a “guinea pig.”
So the father began giving his preschool-aged son cannabis cookies in the morning, which calmed him, the dad reported. But the bad behavior returned in the afternoon, so the father asked a school nurse to give the cookies to the boy at lunch.
The nurse turned the father over to child protective services and law enforcement, leading to an eventual medical board investigation against Eidelman, according to the board report.
“Although he did not outright suggest a diagnosis … he all but made one up out of whole cloth,” the decision reads. “Labeling a child with a significant mental condition can be harmful … if those labels are incorrect, pernicious results may follow.”
Eidelman estimated that he has written more than 10,000 letters recommending cannabis to patients over the last 20 years.
He said he has long recognized that conventional medicine was a “train on the wrong track.” On his website, he offers several unique treatments, including one in which cigarette smokers affix to their ears a device that emits electric currents and thereby reduces their cravings for nicotine.
“From the beginning of my career, I’ve been looking for things that really worked and weren’t toxic,” Eidelman said in an interview. “And cannabis really works.”
Revoking a California medical license is very rare. Of the 149,283 doctors licensed in the state, 43 lost their licenses in the most recent fiscal year, only seven of which were for gross negligence — the misconduct of which Eidelman was found guilty — according to board’s latest annual report.
The post Doctor Recommends Marijuana For 4-Year-Old Boy appeared first on Reach Out Recovery.
Adult Children Of Alcoholics: Creating A Safe Space
Being an Adult Child of an Alcoholic (ACA) comes with an overwhelming laundry list of traits. Many of us are terrified, afraid, and frightened. It’s easier for us to be concerned with others rather than ourselves, and we lose our identity. Here’s how creating a safe space helps us heal.
An Example Of Lost Identity
Being an adult child of an alcoholic means when we were kids, we had responsibilities beyond our years or capabilities. I, for example, knew how to kill and clean a chicken before I entered high school. Because this is all we know, we tend to marry people who are OK with our selflessness. As parents, we’re extremely over-protective because we’ve already had years of experience in high-stress parenting.
When I first found recovery, I was so enmeshed with my husband and son that I felt deep shame for spending 20 minutes alone in my bedroom to do my 12-step homework! Making myself slow-down to put on body lotion was a major accomplishment, and it took MONTHS for me to buy MY favorite foods at the grocery store. Little did I know, taking these small steps to care for myself was essential to my recovery.
It’s More Than Self-Care; It’s Self-Parenting
Per the ACA’s Flip Side Of The Other Laundry List, when:
We accept and comfort the isolated and hurt inner child we have abandoned and disavowed, we thereby end the need to act out our fears of enmeshment and abandonment with other people.
To heal, we have to go back, find, and meet the needs of that inner child who got lost along the way. American psychologist Abraham Maslow explained that our most basic need is for physical survival, and this will be the first thing that motivates our behavior. Once our basic physiological needs are fulfilled, we’ll naturally be motivated to fill the next level of needs.
Meeting My Basic Needs
When I first began recovery, I couldn’t meet my basic physical needs. I had no money for groceries because I was paying the minimum amount due on every outstanding debt. Never getting ahead, my debt grew. I stood in more than one food pantry line before I was willing to try something different. Finally, I took Dave Ramsey’s Financial Peace University.
Dave’s teachings coincide with Maslow’s Hierarchy of Needs. I learned to get out of debt, I had to protect my four walls, which included basic necessities, like:
Food
Shelter (including utilities)
Basic clothing and
Transportation
Feeling Safe Somewhere
Once my condition stabilized, I was then strong enough to tackle my safety needs. I made a safe space in my home. My husband and son are both energetic, enthusiastic, loud people. Watching sports with them triggers me, as I’m afraid of angry people. To me, loud means angry.
About 18 months ago, I set up my bedroom as a “storm shelter”. It’s equipped with a bathroom, shower, reading materials, candles, and my pets food and water bowls. If I need to, I can hunker down in my room and ride out any emotional storm, whether real or imagined by me. Hanging outside my room is a sign with this Melody Beattie quote,
“If you want to act crazy, that’s your business, but you can’t do it in front of me. Either you leave, or I will walk away.”
At first, I went there often, sometimes in an angry huff. Sometimes the door would be locked all night. Gradually, I felt safer and more free. Now I often sit in bed reading with the door open. I almost never hide, and usually, my family stops by to visit.
Instead of feeling guilty for buying the healthy foods I like at the grocery store, I buy groceries first before paying any bills. I select the best in fruits, veggies, and meats. I savor the time spent making healthy meals for myself. Instead of being thought of as selfish as I feared, my family is sharing my delicious meals with me. It’s a slow, sweet healing.
The post Adult Children Of Alcoholics: Creating A Safe Space appeared first on Reach Out Recovery.
Has The Opioid Epidemic Obsession Overshadowed Meth?
From Psychology today:
We’ve been focused on opioids for years, but meth is quickly coming back.
When I was immersed deeply in the world of drugs in the early 2000s, heroin was rarely spoken of in the media. But according to local and national media, cocaine and methamphetamine (“meth”) were huge problems. Everywhere, you’d hear stories of police busting huge meth (also known as speed or crystal meth) operations and the terrible problem the drug was creating in our country. Because meth labs were seemingly blowing up everywhere, the fear that meth was taking over was perpetuated.
Though fewer and fewer people were making the stuff locally, more and more gangs from Central America (primarily Mexico) were stepping in to cover the gaps. But, as police and the DEA continued closing in, it seemed that meth gradually disappeared from our consciousness, if not necessarily from the streets. The next thing you knew, the opioid epidemic seemed to be the only thing anyone could talk about.
But has it overshadowed the growing meth problem in the United States? Lately, we’ve been hearing a lot of media coverage surrounding the opioid crisis. According to a new report on preventable deaths from the National Safety Council, Americans have a 1 in 96 chance of dying from an opioid overdose. To put it in perspective, the probability of dying in a motor vehicle crash is 1 in 103.
But have we been too hyper-focused on this single drug?
The history of methamphetamines in the United States
There has been a long standing history of use of amphetamines in the U.S. since the 1930s and 40s. And methamphetamines (particularly the illicit drug methamphetamines hydrochloride) was popular in the 1990s and 2000s but began to decline in the mid-2000’s when stricter laws were passed and enforced. One of the key ingredients in meth is ‘pseudoephedrine’ which could be acquired from a common cold medicine—Sudafed—but the new law required pharmacies to retain records of all pseudoephedrine purchases. States such as Mississippi and Oregon required a prescription for purchase. I knew groups of meth “cooks” and dealers who would send out dozens of people (they literally called them smurfs) to go to hundreds of pharmacies around the state and obtain the large quantities of Sudafed that was needed. It took a lot of work and dedication (and a lot of meth to keep them going!). But the hard work got to everyone, and fewer and fewer labs could operate, so meth lab explosions became a thing of the past, and everyone seemingly forgot about meth.
Nowadays there may be fewer household meth labs, but there is actually more meth being smuggled in from Mexico. Sourcing the ingredients within the United States made it nearly impossible to produce on our home turf so Mexican cartels took this opportunity to produce purer, cheaper meth. And they became very good at it, creating Mexican superlabs that produced hundreds of pounds a day. The best meth I ever bought came from these “Breaking Bad” style labs…
If you don’t use meth or know anyone that does, you may be thinking “it’s not my problem.” But, if you’re a taxpayer (or a normal human being with emotions) it most certainly is your problem. According to a recent study in the Journal of the American Medical Association, the cost of amphetamine-related hospitalizations had increased from $436 million in 2003 to close to $2.2 billion by 2015. That’s a nearly 5-fold increased! Now, wouldn’t that money be better spent on mental health for anyone who needed it so people wouldn’t have to self-medicate?
The post Has The Opioid Epidemic Obsession Overshadowed Meth? appeared first on Reach Out Recovery.





