Is Abortion Ever Medically Justifiable?
Today is the 43rd anniversary of the Supreme Court’s landmark decision legalizing abortion. One of the front runners in this year’s Presidential election has taken a stand against abortion, regardless of the reason. Many people believe we must allow abortion in cases of rape, incest or where the life of the mother is at risk. I won’t discuss cases of rape or incest in this post, but I would like to examine the idea that abortion should be reserved for cases where the mother’s life may be at risk. First we need to bring a little clarity to the terms used in this discussion.
As they pertain to abortion, the “life” of the mother is completely different issue from the “health” of the mother. Whether an abortion is necessary to save the life of a pregnant woman is easy to determine. If an abortion is the only (or most reasonable) option known to medical experts to save the life of a pregnant woman with a certain medical condition, it is medically justifiable. The health of a pregnant woman is a completely different issue.
The Supreme Court’s 1973 abortion ruling intended to allow abortion during the first two trimesters, but not during the third—unless the pregnancy posed a threat to the health of the mother. So far, so good. But the Court defined the word “health” so broadly that it can be applied to almost anything. The Court defined “health” to include “physical, emotional, psychological, (or) familial” trauma. These qualifiers allow for an almost unlimited number of possibilities.
If for example, a pregnant woman suffers shame or guilt because of how her family perceives her pregnancy, this would constitute a valid reason for an abortion, because it negatively impacts her metal health. If a mother believes her health may suffer in any way—regardless of which health factor she identifies—she can legally have an abortion at any time during her pregnancy. The point here is that making an exception for the health of the mother is not the same as making an exception to save her life.
There are a number of medical conditions that must be considered when looking at what procedures might be needed to save the life of a pregnant woman. We’ll look at them one at a time, but first a few basic facts about pregnancy:
A full term pregnancy is considered to be 40 weeks in duration. Not surprisingly, full term babies have a very high survival rate. But what about babies delivered before full term?
Due mostly to advances in technology, a baby that is delivered today at 25 weeks gestation has between a 50-80% chance of survival to discharge from the hospital. At 24 weeks the odds are ten percent less. At 23 weeks it has a 10-30% chance of survival. At 22 weeks the chance of survival drops to less than 10%. There are no known cases of a baby surviving birth at 21 week gestation. (source) A baby delivered after 23 weeks (whether by vaginal birth or by c-section) has a decent chance of survival to discharge from the hospital.
Now let’s look at specific medical conditions that could be a threat to a pregnant woman. You might imagine there are dozens of different medical conditions that could potentially threaten the life of a pregnant woman, but in fact—there are only a few. Eclampsia is one of them.
Eclampsia is a condition marked by hypertension, protein in the urine and in serious cases—seizures. In rare cases, eclampsia can be fatal, due to prolonged and uncontrolled seizures. But eclampsia is a late-term condition. Ninety percent of cases occur after the 34th week of gestation. Although the symptoms of eclampsia can be treated with medications, the best treatment is delivering the fetus—either by inducing labor or by c-section.
Preeclampsia is a related condition that has the same symptoms as eclampsia, but without seizures. Preeclampsia can begin around the 20th week, but it is not a threat to the mother’s life. It is only when preeclamspia becomes eclampsia that it threatens the mother’s life, and that happens late enough in pregnancy for the fetus to survive delivery. Since eclampsia is only a threat late in pregnancy and since it can always be treated by delivering the fetus, there is no medical necessity for an abortion to save the mother’s life.
There are a couple of other conditions that pose a threat to the lives of a pregnant woman and fetus during late stage pregnancy. Abruptio placenta is when the placenta detaches from the lining of the uterus and the blood supply to the fetus is compromised. This condition sometimes results in fetal death, but in the majority of cases, a viable baby can be delivered either vaginally or by c-section, if detected early enough. Placenta previa occurs when the placenta blocks the cervical opening. Once diagnosed, most cases are treated with delivery by c-section. Abortion is never necessary to treat either of these conditions.
Some have argued that medical conditions such liver failure, heart failure and kidney failure may require treatment during pregnancy (including the possibility of organ transplant) and such cases may require a pregnancy to be aborted. While it’s true that some mothers who are pregnant may have these conditions, the conditions themselves are not caused by pregnancy and ending the pregnancy won’t provide any therapeutic effect to the mother. Whether the pregnancy is ended or not, the mother will still have the condition, thus there is no medically justifiable reason to terminate a pregnancy for such conditions.
Some have argued that cancer treatments such as chemotherapy and radiation cannot be safely done during pregnancy and since these treatments may save the life of the mother, they are a valid medical reason for abortion. Pregnancy doesn’t interfere with these treatments. All standard treatments that may be necessary for a cancer patient can be done on a pregnant woman just as easily on one who is not pregnant. The effects of such treatments on a fetus cannot be reliably predicted. While it’s true that these treatments may have an adverse effect on the fetus, it’s equally possible that a fetus will suffer no harmful effects. This exhausts the list of medical conditions that pose a threat to a woman’s life in late-term pregnancy.
In any pregnancy where a medical condition threatens the life of the mother, if the pregnancy needs to be terminated, and is past the 23rd week, the baby can simply be delivered either by inducing labor or by c-section, without harming either the baby or the mother. Stated in another way—there is no medically justifiable reason for abortion after about the 23rd week of gestation. This is true regardless of the medical condition in question. Which brings us to conditions that threaten the life of a woman early in pregnancy.
What conditions pose a legitimate threat to the mother’s life in an early-term pregnancy?
There is only one: ectopic pregnancy.
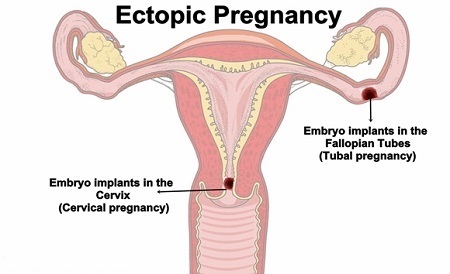 Ectopic pregnancy occurs when the embryo implants outside the uterus—typically in the Fallopian tubes, but rarely in the ovary, abdomen, or cervix. In almost all cases, ectopic pregnancy does not result in a live birth, although there have been documented cases of successful live births:
Ectopic pregnancy occurs when the embryo implants outside the uterus—typically in the Fallopian tubes, but rarely in the ovary, abdomen, or cervix. In almost all cases, ectopic pregnancy does not result in a live birth, although there have been documented cases of successful live births:
In September 1999 an English woman, Jane Ingram gave birth to triplets. Two of the fetuses developed in the uterus, while the third developed outside the uterus. All three survived.
In July 1999, Lori Dalton gave birth by c-section in Ogden Utah, to a healthy baby girl who had developed outside of the uterus.
In 1999, a healthy baby boy was delivered in London after having implanted in his mother’s fallopian tube.
In 2000, a healthy baby girl was delivered in Nottingham (UK) despite the fact that the placenta attached to the lining of her mother’s bowels.
In 2005, a woman in the UK gave birth to a healthy baby girl who spent the entire pregnancy in her mother’s abdomen.
In 2008, a woman in Australia delivered a healthy baby girl from an ovarian pregnancy.
The odds of a fetus surviving ectopic pregnancy are extremely slim, but it does happen. Ectopic pregnancy can, in rare cases, be fatal to the mother. What kind of threat does it pose?
A report on ectopic pregnancy published by the American Academy of Family Physicians (AAFP) reveals that ectopic pregnancy occurs at a rate of about 19.7 cases per 1,000 pregnancies in North America. To date, 14 studies have documented that between 68 and 77 percent of ectopic pregnancies resolve without intervention. Most cases are never treated. The embryo usually miscarries without medical intervention and the pregnancy ends.
Next let’s calculate the risk of death to the mother:
The CDC reports that between 2003–2007, there were 0.5 maternal deaths related to ectopic pregnancy for every 100,000 live births. Death is usually due to hemorrhage after the Fallopian tube ruptures. Although the likelihood of death for a mother with ectopic pregnancy is extremely small, the risk of continuing the pregnancy is real, and the baby’s chance of survival is almost zero.
When the life of the mother is threatened by continued pregnancy, sound ethics tell us that everything possible should be done to save the lives of both the mother and the child. After the 23rd week, the pregnancy can be terminated by inducing labor or performing a c-section. But when pregnancy endangers the life of the mother during the first half of pregnancy, the most ethical course of action is harder to determine. The reason abortion is condemned by so many people is because it kills an innocent human being. What do you do when the existence of one human being, through no fault of their own, threatens the life of another human being? Do you end the life of the child, to save the life of the mother?
The problem can be viewed this way:
A) If the pregnancy is allowed to continue, the mother will die, and if the mother dies, the child will die.
B) If the pregnancy is ended through abortion, the child will die, but the mother will live.
The question is usually put in these terms: If there is no way to save the child, but there is a way to save the mother, it is ethical to save the mother’s life by ending the child’s life? Isn’t it better to save one life, than to lose two?
Those in favor of abortion tend to view the outcomes of such pregnancies as guaranteed: “My doctor said that if I had not had the abortion, I would have died.” Although this reasoning may appear to be sound, in reality, the outcome can never be known with certainty. Although we can say with certainty that if a mother dies, the child will die—we can never say with certainty that if the pregnancy were to continue the mother would die. Unless you are omniscient, it’s impossible to say what would happen to a mother if a procedure had not been done. The best we can do is guess. And if we want to be truthful, we must admit that we can never know with certainty whether a mother will live or die if she does not have an abortion. Therefore, we must modify statement A above. The first part would need to read:
A) If the pregnancy is allowed to continue, the mother might die…
There is a world of difference between “will die” and “might die,” and this is where things get sticky. Like any other medical condition, pregnancy always carries a small risk of death, and an ectopic pregnancy increases that risk slightly. But does that small risk justify an abortion?
By the time an ectopic pregnancy is discovered (typically by 7 to 8 weeks gestation) the embryo has usually died. When an ectopic pregnancy is discovered and the embryo is still alive, one of two procedures is performed. If the mother has a healthy, normal ovary and Fallopian tube on the opposite side of the ectopic pregnancy, the Fallopian tube and embryo are surgically removed. If she does not have healthy organs on the opposite side, an incision is made in the Fallopian tube and the embryo is removed. (Everything possible is done to assure the mother has at least one healthy Fallopian tube and ovary.)
This procedure is always fatal to the embryo. And although it bears some similarity to an elective abortion, it is generally viewed differently—even by religious organizations that oppose abortion. The death of the embryo or fetus is the sole purpose of an elective abortion, but it is the undesired and unavoidable consequence of surgically treating a life-threatening ectopic pregnancy. This seems to be the one situation in which ending a pregnancy is medically justifiable.
Thanks for bearing with me. I hope this article has helped you see this issue a little more clearly.
The post Is Abortion Ever Medically Justifiable? appeared first on Praying Medic.



