William Davis's Blog: Dr. Davis Infinite Health Blog, page 148
January 24, 2015
Protected: Special Extra Resource if you attended the Halifax 50 Shades of Grain presentation!
This content is password protected. To view it please enter your password below:
Password:
The post Protected: Special Extra Resource if you attended the Halifax 50 Shades of Grain presentation! appeared first on Dr. William Davis.
How NOT to have HIGH TRIGLYCERIDES
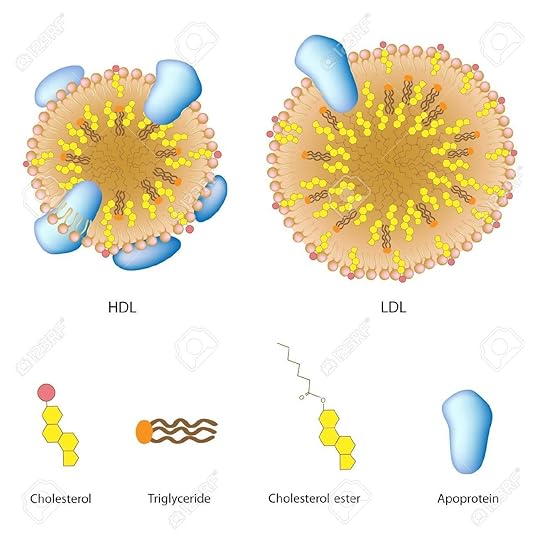 High triglyceride levels are common, as common as muffin tops and man breasts. You will find a triglyceride level among the four values on any standard cholesterol panel. High triglycerides are either ignored by most doctors or reflexively “treated” with drugs, such as fibrates (Lopid, fenofibrate) or prescription fish oil (Lovaza). But buried in this single value is tremendous insight into diet, metabolic efficiencies, and cardiovascular risk, with control using natural, non-medication means very easy to accomplish.
High triglyceride levels are common, as common as muffin tops and man breasts. You will find a triglyceride level among the four values on any standard cholesterol panel. High triglycerides are either ignored by most doctors or reflexively “treated” with drugs, such as fibrates (Lopid, fenofibrate) or prescription fish oil (Lovaza). But buried in this single value is tremendous insight into diet, metabolic efficiencies, and cardiovascular risk, with control using natural, non-medication means very easy to accomplish.
Why are triglycerides important? Triglyceride levels of 60 mg/dl or higher will:
Block insulin, thereby adding to weight gain and higher blood sugars
Cause formation of small LDL particles. Triglycerides occur in the bloodstream mostly as Very Low-Density Lipoproteins, VLDL, that interact with other lipoprotein particles. Abundant triglycerides in VLDL encounter LDL particles and make them triglyceride-rich. This leads to the formation of small LDL particles that causes coronary heart disease and heart attack.
At levels above normal, the pancreatic beta cells that produce insulin are subjected to lipotoxicity, irreversible damage that can lead to inadequate insulin production by the pancreas over time.
At very high levels above 1000 mg/dl, triglycerides cause pancreatitis, pancreatic inflammation that damages the delicate pancreatic tissues.
The higher the triglycerides, the higher the cardiovascular risk. This may work through formation of small LDL particles or by other means. Labs typically quote 150 mg/dl or higher as the cutoff for “normal,” but this is not true: a level of 150 mg/dl is associated with a substantial quantity of the above metabolic distortions. Only at 60 mg/dl or below, for instance, do small LDL particles drop to much lower levels or zero.
What causes triglycerides to rise?
First of all, dietary fats are triglycerides, by definition. Fat on pork, the fat in olive oil, the fat in other foods occur as triglycerides. When we consume fats and oils, there is therefore a modest and nearly immediate rise in blood triglycerides as particles called chylomicrons, large particles formed by the intestinal tract to “package” fats for digestion. Chylomicrons are cleared rapidly and efficiently by the liver over several hours. In most people, fat intake is–counterintuitively–only a minor contributor to blood triglyceride levels, a non-contributor to high fasting triglycerides.
There are two processes that are much larger determinants of both fasting and after-meal (“postprandial” or “non-fasting”) triglyceride levels:
Whenever the liver has fatty acids delivered to it, it manufactures triglycerides (each triglyceride molecule contains 3–tri–fatty acids). Visceral fat–deep abdominal fat in the abdomen–is resistant to insulin and thereby provides a continual flow of fatty acids to the liver, a process that runs 24 hours a day.
Carbohydrates in the diet are converted to triglycerides by the process of liver de novo lipogenesis, the creation of fat from carbohydrates.
These last two processes yield much greater rises in both fasting and postprandial triglycerides than that provided by dietary fat. These two processes explain why, for example, someone has a triglyceride level of 210 mg/dl fasting, 400 mg/dl 6 hours after eating. It also explains why some of the triglycerides manufactured by the liver stay there and accumulate, causing fatty liver.
Understanding these phenomena thereby lead us to practical dietary and natural methods to reduce triglycerides to a level of 60 mg/dl or less:
Eliminate grains and sugars–Contrary to the conventional advice to reduce fat and eat plenty of “healthy whole grains,” the amylopectin A carbohydrate unique to grains provides dietary carbohydrates to fuel liver de novo lipogenesis. High blood sugars that result from grain amylopectin A also lead to insulin resistance. The result: high triglycerides. Eliminate grains and sugars and both processes unwind quickly and dramatically. Most people need to also limit carbohydrate consumption to no more than 15 grams net carbohydrates per meal (net carbs = total carbs – fiber) to prevent liver de novo lipogenesis from proceeding. Do not reduce dietary fat, as this raises triglycerides substantially. (When I was an ultra low-fat vegetarian, my triglycerides rose to 350 mg/dl; they are now 40 mg/dl.)
Reverse insulin resistance–Beyond grain and sugar elimination, vitamin D restoration, getting adequate sleep, and physical activity all help reverse insulin resistance. A very quick way to reverse insulin resistance is through intermittent fasting, fasting for periods of 15-36 hours (while hydrating very well).
Supplement omega-3 fatty acids from fish oil–The EPA and DHA of fish oil activate the enzyme lipoprotein lipase that helps accelerate clearance of both postprandial chylomicrons and VLDL particles. This does not apply to the omega-3 fatty acid, linolenic acid, from chia, flaxseed, or walnuts, nor can it be accomplished by the trivial quantity of EPA and DHA in krill oil; it must come from fish oil. It also requires greater supplemental total daily intakes of 3000-3600 mg EPA + DHA per day (divided into two doses). And not only do you not need the 10-fold more costly prescription fish oil, you can actually purchase fish oil that is superior to prescription fish oil (such as the liquid triglyceride form found in the brands Ascenta NutraSea and Nordic Naturals).
Cultivate healthy bowel flora–“Feeding” bowel microorganisms the fibers they need allow them to convert fiber into butyrate, a fatty acid that yields metabolic effects that include reduction of insulin resistance, reduced blood sugar, reduced LDL values, and reduced triglycerides. This important strategy is discussed further in this Wheat Belly Blog post, as well as a full discussion in Wheat Belly Total Health.
Fibrate drugs and prescription fish oil are not necessary to reduce triglycerides. This is yet another example (among many) where the pharmaceutical industry has managed to persuade physicians that high triglycerides are a reason for prescribing drugs, not a reason to fix the cause. I have prescribed neither agent for high triglycerides in years, despite managing many complex hyperlipidemias that included many people with high triglyceride levels.
The post How NOT to have HIGH TRIGLYCERIDES appeared first on Dr. William Davis.
January 17, 2015
Do you have a WOOD deficiency?
 I can hear the titters now. But, seriously, do you have a deficiency of wood fiber, i.e., cellulose?
I can hear the titters now. But, seriously, do you have a deficiency of wood fiber, i.e., cellulose?
No? Then why were you following the common advice to include breakfast cereals such as All Bran, Fiber One, and Raisin Bran that, yes, are rich in fiber, but mostly rich in the cellulose fiber that is a constituent of wood? Cellulose in small quantities, as occurs in green vegetables and fruit is harmless, perhaps modestly beneficial. But there is no need to “supplement” with large quantities, as occurs with such bran or fiber-rich cereals.
Cellulose fiber undoubtedly bulks up bowel movements, as humans lack the digestive apparatus to break it down. Likewise, very little cellulose is broken down by bowel flora. Cellulose therefore simply passes through, relatively inert, though suspected to yield a damaging abrasive effect on the delicate intestinal lining in its passage when consumed in high quantities.
The discussion surrounding fibers has been confused by the more recently appreciated fact that fiber is not just one thing, but several different varieties. Just as “nutrients” can mean everything from vitamin C in citrus fruit to vitamin K2 in fermented dairy products to carotenoids in yellow/orange fruits and vegetables, so can the term “fiber” refer to a range of different things.
The popular notion of fiber is therefore that of cellulose. The poop-bulking effect of cellulose can fool you into thinking that you have achieved bowel health. In the case of wheat and grains, for instance, wheat germ agglutinin and gliadin peptide fragments are highly toxic to the intestinal wall, block gallbladder and pancreatic function, and induce alterations in bowel flora. Cellulose and phytates bind minerals, such as iron and zinc, and make them unavailable to you. But the cellulose provides the appearance of bulky stools despite the toxic damage incurred, causing you to believe that you’ve had a healthy BM. It is clear that the cellulose fibers of grains do not provide protection from colon cancer, despite the popular notion that they are protective. (The studies that document the health benefits of fibers did not break them down into the various forms, lumping all fibers together.)
We therefore need to get rid of the notion that cellulose fibers are necessary for gastrointestinal health. There is, however, a form of fiber that you will miss when you eliminate grains: arabinoxylan. Minus wheat and grains in your diet, you will lose about 3 grams per day of this beneficial (I hate to admit!) indigestible but prebiotic fiber, i.e., a fiber that is indigestible by you but is metabolized by bowel flora. Because most people obtain only a total of 8-9 grams per day of this hugely beneficial class of fibers, losing the 3 grams per day of arabinoxylan can yield constipation, abdominal discomfort, result in metabolic distortions such as higher blood pressure and blood sugar, and increased potential for colon cancer.
So, if there is a fiber to replace, it is to amp up your intake of prebiotic fibers, AKA “resistant starches.” Even better, increase your intake to a level higher than the average 8-9 grams per day intake to the ideal intake of 20 grams per day. We accomplish this by adding foods such as raw potatoes and green bananas to our daily routine, detailed in this Wheat Belly Blog post.
We therefore need to rid ourselves of the notion that wood fibers–cellulose–are necessary for health, and replace this with the notion that our bowel flora require a specific class of prebiotic fibers to support the health of their host: you. Take care of your bowel flora and they will take care of you. By obtaining a healthy intake of such prebiotic fibers, you not only achieve bowel health and regularity without adding cellulose, but you also enjoy wonderful metabolic benefits, as bowel flora metabolize these fibers to metabolic mediators, such as butyrate, that reduce blood pressure, reduce insulin and blood sugar, raise HDL, reduce triglycerides, reduce LDL values, improve mood and reduce anxiety, and deepen sleep.
The post Do you have a WOOD deficiency? appeared first on Dr. William Davis.
January 16, 2015
How NOT to have an autoimmune condition
 Autoimmune conditions are becoming increasingly common. Estimates vary, but it appears that at least 8-9% of the population in North America and Western Europe have one of these conditions, with The American Autoimmune Related Diseases Association estimating a higher value of 14%. They are conditions that involve an abnormal immune response directed against one or more organs of the body. If the misguided attack is against the thyroid gland, it can result in Hashimoto’s thyroiditis. If it is directed against pancreatic beta cells that produce insulin, it can result in type 1 diabetes or latent autoimmune diabetes of adults (LADA). If it involves tissue encasing joints (synovium), it can result in rheumatoid arthritis. It if involves the liver, it can result in autoimmune hepatitis, and so on.
Autoimmune conditions are becoming increasingly common. Estimates vary, but it appears that at least 8-9% of the population in North America and Western Europe have one of these conditions, with The American Autoimmune Related Diseases Association estimating a higher value of 14%. They are conditions that involve an abnormal immune response directed against one or more organs of the body. If the misguided attack is against the thyroid gland, it can result in Hashimoto’s thyroiditis. If it is directed against pancreatic beta cells that produce insulin, it can result in type 1 diabetes or latent autoimmune diabetes of adults (LADA). If it involves tissue encasing joints (synovium), it can result in rheumatoid arthritis. It if involves the liver, it can result in autoimmune hepatitis, and so on.
While it requires a genetic predisposition towards autoimmunity that we have no control over (e.g., the HLA-B27 gene for ankylosing spondylitis), there are numerous environmental triggers of these diseases that we can do something about. Identifying and correcting these factors stacks the odds in your favor of reducing the autoimmune inflammation, pain, organ dysfunction, even reversing the condition altogether.
Among the most important factors to correct in order to minimize or reverse autoimmunity are:
Wheat and grain elimination–If you are reading this, you likely already know that the gliadin protein of wheat and related proteins in other grains (especially the secalin of rye, the hordein of barley, zein of corn, perhaps the avenin of oats) initiate the intestinal “leakiness” that begins the autoimmune process, an effect that occurs in over 90% of people who consume wheat and grains. The flood of foreign peptides/proteins, bacterial lipopolysaccharide, and grain proteins themselves cause immune responses to be launched against these foreign factors. If, for instance, an autoimmune response is triggered against wheat gliadin, the same antibodies can be aimed at the syapsin protein of the central nervous system/brain, resulting in dementia or cerebellar ataxia (destruction of the cerebellum resulting in incoordination and loss of bladder and bowel control). Wheat and grain elimination is by far the most important item on this list to reverse autoimmunity.
Correct vitamin D deficiency–It is clear that, across a spectrum of autoimmune diseases, vitamin D deficiency serves a permissive, not necessarily causative, role in allowing an autoimmune process to proceed. It is clear, for instance, that autoimmune conditions such as type 1 diabetes in children, rheumatoid arthritis, and Hashimoto’s thyroiditis are more common in those with low vitamin D status, much less common in those with higher vitamin D levels. For this and other reasons, I aim to achieve a blood level of 25-hydroxy vitamin D level of 60-70 ng/ml, a level that usually requires around 4000-8000 units per day of D3 (cholecalciferol) in gelcap or liquid form (never tablet due to poor or erratic absorption). In view of the serious nature of autoimmune diseases, it is well worth tracking occasional blood levels.
Supplement omega-3 fatty acids–While omega-3 fatty acids, EPA and DHA, from fish oil have proven only modestly helpful by themselves, when cast onto the background of wheat/grain elimination and vitamin D, omega-3 fatty acids compound anti-inflammatory benefits, such as those exerted via cyclooxygenase-2. This requires a daily EPA + DHA dose of around 3600 mg per day, divided in two. Don’t confuse EPA and DHA omega-3s with linolenic acid, another form of omega-3 obtained from meats, flaxseed, chia, and walnuts that does not not yield the same benefits. Nor can you use krill oil with its relatively trivial content of omega-3s.
Eliminate dairy–This is true in North America and most of Western Europe, less true in New Zealand and Australia. Autoimmunity can be triggered by the casein beta A1 form of casein widely expressed in dairy products, but not by casein beta A2 and other forms. Because it is so prevalent in North America and Western Europe, the most confident way to avoid this immunogenic form of casein is to avoid dairy altogether. You might be able to consume cheese, given the fermentation process that alters proteins and sugar, but that has not been fully explored.
Cultivate healthy bowel flora–People with autoimmune conditions have massively screwed up bowel flora with reduced species diversity and dominance of unhealthy species. We restore a healthier anti-inflammatory panel of bacterial species by “seeding” the colon with high-potency probiotics, then nourishing them with prebiotic fibers/resistant starches, a collection of strategies summarized in this Wheat Belly Blog post and in greater detail in Wheat Belly Total Health. People sometimes view bowel flora management as optional, just “fluff”–it is anything but. Properly managing bowel flora can be a make-it-or-break-it advantage; don’t neglect it.
There you go: a basic list to get started on if your interest is to begin a process of unraveling the processes of autoimmunity. In some conditions, such as rheumatoid arthritis and polymyalgia rheumatic, full recovery is possible. In other conditions, such as Hashimoto’s thyroiditis and the pancreatic beta cell destruction leading to type 1 diabetes, reversing the autoimmune inflammation does not restore organ function: hypothyroidism results after thyroiditis quiets down and type 1 diabetes and need for insulin persists after pancreatic beta cell damage. But note that the most powerful risk factor for an autoimmune disease is another autoimmune disease–this is why so many people have more than one autoimmune condition. People with Hashimoto’s, for instance, can develop rheumatoid arthritis or psoriasis. So the above menu is still worth following even if you cannot hope for full organ recovery.
More discussions like this, i.e., how to stack the odds in favor of reversing or NOT having numerous health conditions, can be found in Wheat Belly Total Health.
The post How NOT to have an autoimmune condition appeared first on Dr. William Davis.
January 11, 2015
How NOT to have irritable bowel syndrome (IBS)
 Irritable bowel syndrome, or IBS, affects 10-20% of the population. People struggle with unexplained bloating, abdominal discomfort, and inconvenient and embarrassing bowel urgency, having to empty their bowels unexpectedly. Some also struggle with intermittent constipation, as well. It turns something that should be subconscious, predictable, and serene into a nightmare.
Irritable bowel syndrome, or IBS, affects 10-20% of the population. People struggle with unexplained bloating, abdominal discomfort, and inconvenient and embarrassing bowel urgency, having to empty their bowels unexpectedly. Some also struggle with intermittent constipation, as well. It turns something that should be subconscious, predictable, and serene into a nightmare.
The typical medical evaluation involves endoscopy and colonoscopy, since procedures, whether necessary or not, pay gastroenterologists well, performed under the guise of ruling out cancer. When they find nothing or only minor findings, such as mild gastritis or erosions, then the prescriptions begin: acid blocking agents, antidepressants, narcotics for pain, anti spasm agents, etc–none address the cause, none are terribly effective, all have undesirable side effects, many of which people are not told about (e.g., unhealthy changes in bowel flora and increased osteoporosis from acid blockers, weight gain from antidepressants).
We see IBS symptoms disappear daily in the majority of people following the Wheat Belly lifestyle of no wheat or grains, even after years of struggle. It is uncommon to not experience improvement or complete relief. Obtaining relief from IBS symptoms therefore starts with wheat and grain elimination. While modern semidwarf wheat is the worst, other grains overlap in many aspects. For example, wheat germ agglutinin that, by itself, exerts a potent bowel toxic effect, can be found in wheat, rye, barley, and rice. Eliminating all grains thereby eliminates the entire collection of grain bowel toxins.
Whatever you do, please don’t label this going “gluten-free,” as you will recall that gluten is just one bowel toxin among several in wheat and related grains. Other grain toxins include phytates, D-amino acids, wheat germ agglutinin, as well as gliadin-derived peptides and other partially-digested peptide fragments. In other words, wheat and grains represent an entire collection of bowel disruptive toxins. Gluten-free replacement foods made with cornstarch, rice flour, tapioca starch, and potato flour also mess up bowel flora and cause IBS and other bowel symptoms to persist. NOBODY here should be eating such gluten-free junk replacements.
People with IBS as a rule start out with substantially disrupted bowel flora: limited species diversity with predominance of unhealthy species. This needs to be corrected to reverse symptoms. An occasional person has bowel flora that is so irretrievably disrupted that a course of antibiotics is required to start with a clean slate. However, the majority can do well by cultivating healthy bowel flora with a combination of a high-potency probiotic preparation for several weeks to months coupled with a program of prebiotic fibers/resistant starches that nourish bowel flora. (This is discussed here in the Wheat Belly Blog and in detail in Wheat Belly Total Health.) This is a process that typically requires 2-3 months to become established.
It may also help to minimize exposure to ubiquitous environmental chemicals that can modify bowel flora. This is a long and daunting list and includes: bisphenol A from cans and plastics, as well as other plasticizers; chlorine, chloramine, and fluoride in municipal drinking water; antibiotic residues in factory-farmed meats and non-organic dairy; herbicides and pesticides in produce; genetically-modified food with glyphosate and Bt toxin; arsenic from rice.
Some people need to consider dairy elimination, also, to avoid both lactose and the casein protein, especially if the above efforts fail to yield full benefit. Occasionally, there is value is identifying other food intolerances as a source of symptoms either through formal testing or a simple process of trial and error. One potential tripping point for some people: fructose sources, including fruit, at least until bowel flora are restored to a healthy profile.
The basic formula is very simple, but astoundingly effective in the majority of people with this condition. It is certainly better than taking a handful of ineffective drugs with undesirable side-effects, while receiving glazed looks from gastroenterologists mostly interested in knowing when they can get away with yet another unnecessary endoscopy.
More like this discussion, i.e., how to NOT have many common health conditions, can be found in Wheat Belly Total Health.
The post How NOT to have irritable bowel syndrome (IBS) appeared first on Dr. William Davis.
January 8, 2015
How NOT to have diabetes
 If you want type 2 diabetes , follow conventional advice to cut fat and eat more “healthy whole grains.” (This is also true for type 1 diabetes in susceptible individuals with pancreatic beta cell autoimmunity triggered by wheat gliadin or corn zein.)
If you want type 2 diabetes , follow conventional advice to cut fat and eat more “healthy whole grains.” (This is also true for type 1 diabetes in susceptible individuals with pancreatic beta cell autoimmunity triggered by wheat gliadin or corn zein.)
But what if you don’t want to follow the footsteps of the two thirds of Americans and Canadians who are now diabetic or pre-diabetic? What if you don’t want the expense and side-effects of oral drugs and insulin–one of the most powerful weight gain drugs around? What if you don’t want to lose your eyesight, develop cardiovascular disease, experience gastroparesis, develop peripheral neuropathy and peripheral arterial disease that can lead to limb gangrene and amputation? What if you don’t want to add to the growing healthcare bubble being created by misguided dietary advice compounded by the overwhelming profit-motive that drives modern medical care?
Not following this path and being spared the awful future that diabetes creates is really pretty simple. But it cannot be done by following the advice of the American Diabetes Association, nor following the advice of the majority of diabetes educators. There are an increasingly larger number of healthcare practitioners who are enlightened and follow strategies like those listed below. But most doctors sadly remain utterly in the dark, doing more to make the diabetes epidemic worse, not contributing to any solution except to offer drugs and procedures.
Here’s a checklist that, if followed, allow the majority of pre-diabetics and diabetics to become non-pre-diabetic and non-diabetic:
Eat NO grains or sugars–Remember: from a blood sugar standpoint, most grains are worse than sugar in their blood sugar raising potential. The safety of “complex” carbohydrates in grains is complete fiction: their glycemic indexes are higher than sucrose.
Don’t limit fat intake–Yes: eat the fat on your pork or steak, eat bone marrow, have some liver, use more organic butter or ghee, use more coconut oil.
Correct vitamin D deficiency–I aim to achieve a 25-hydroxy vitamin D level of 60-70 ng/ml, a level usually achieved with 4000-8000 units (oil-based gelcap or liquids, not tablets) per day. This helps restore insulin responsiveness/reverse insulin resistance.
Supplement omega-3 fatty acids–from fish oil only, not krill oil, flaxseed, or chia. (Flaxseed and chia are wonderful, but do not provide EPA and DHA.) I believe ideal intake is in the range of 3000-3600 mg EPA + DHA per day, divided in two. EPA + DHA blunt the postprandial (after-meal) surge in digestive byproducts (chylomicrons and VLDL) that oppose insulin.
Correct bowel flora–Start with a high-potency probiotic (e.g., 50 billion CFUs per day with at least a dozen species of Lactobacillus and Bifidobacteria) for several weeks, but it is even more important long-term to properly nourish bowel flora with prebiotic fibers/resistant starches, as discussed here. Properly feeding bowel flora yields fatty acid metabolites that increase your body’s responsiveness to insulin and reduce blood sugar.
Supplement magnesium–e.g., magnesium malate, 1200 mg twice per day (180 mg “elemental” magnesium twice per day), a modest advantage in restoring insulin responsiveness.
Fast intermittently–Brief periods of fasting, e.g., 15-36 hours, allow fatty liver (present to varying degrees in everyone with high blood sugars) to recede, a huge advantage in restoring insulin responsiveness. Be sure to hydrate more than usual during any fasting period.
Sleep adequately–Not a minor factor, as sleep deprivation increases carb cravings and increases snacking, while also blocking insulin. Most people need 7 1/2 hours per night. You might have to make friends with melatonin and tryptophan to manage your circadian rhythm.
Be active–including avoiding prolonged sitting.
Anyone on insulin or oral diabetes drugs, especially glyburide, glipizide, and glimepiride, should talk to their healthcare provider about an immediate reduction in dosage or even eliminating one or more of them, since you do not want any hypoglycemia (low blood sugar). If your doctor refuses to work with you or tells you this is stupid, find a new doctor ASAP. Doctors should be experts in reversing diabetes but you will find that the majority are not, despite knowing how to prescribe the drugs.
There you have it. Should you give it a try, be sure to come back and report your experience. And for more discussions about how to reverse other health conditions with natural means, see Wheat Belly Total Health. This discussion is adapted from Chapter 10: Grainless Metabolic Mastery.
The post How NOT to have diabetes appeared first on Dr. William Davis.
January 4, 2015
Grain-Free Sushi: A guest post from nutritionist Julie Daniluk

Nutritionist, author, and friend, Julie Daniluk from Toronto, provided one of her many wonderful grain-free, low-carb recipes to me, this one for sushi. My mom was Japanese and, boy, could she make some fabulous sushi. As we banish, or at least sharply minimize, rice exposure (due to presence of the wheat germ agglutinin protein, identical to that occurring in wheat, rye, and barley, highly-digestible amylopectin starch, and arsenic), a bit of delicious and nostalgic futomaki would indeed be a treat!
Julie has a moving and powerful personal story of recovery from severe gastrointestinal illness, a journey she accomplished by gaining a deep understanding of food.
If you like this recipe and want to follow Julie’s enlightened conversations further, see her website here with links to her Facebook page, TV show, and quite a few recipes. More about Julie’s book, Slimming Meals that Heal, can also be found on her website.
Grain-Free Sushi from Julie Daniluk
My favorite type of sushi is futomaki—the large, colorful rolls packed with pickled radish, egg, vegetables and rice. Naturally, I felt the need to create a slimming, anti-inflammatory version. Replacing the sweet, refined sushi rice with cauliflower sounds crazy, but it lowers the glycemic index of this dish significantly and you won’t believe how convincing it tastes.
Makes 3 rolls or 24 pieces.
2 cups cauliflower florets broken into small pieces (remove stem)
Sweetener equivalent to 2 teaspoons sugar (e.g., 1/2 teaspoon Wheat-Free Market sweetener)
2 teaspoons apple cider vinegar
1/4 teaspoon pink rock salt or gray sea salt
1 tablespoon pesto
1 tablespoon prepared yellow mustard
80 gram/3 ounce can herring or mackerel, or 1 cup cooked black beans, drained and rinsed
3 large nori sheets
1/2 cup cucumber, sliced vertically into match sticks
1/2 cup carrot, sliced vertically into match sticks
Combine cauliflower, sweetener, vinegar and salt in a food processor or food chopper and pulse until mixture is rice-like in texture. Place into a bowl and set aside.
Place pesto, mustard and fish in a bowl and mash into a paste.
Lay nori sheets on top of a sushi roller. Place a thin layer of “rice” mixture across the nori sheet, leaving 2 inches at bottom clear to allow for rolling. Using a spoon, smooth a layer of fish paste across ”rice”-covered nori sheet. Place cucumber and carrots in a row across center of nori sheet. Roll firmly and seal end of nori with a wet finger.
Cut with a sharp knife into 1-inch coins. Serve immediately.
The post Grain-Free Sushi: A guest post from nutritionist Julie Daniluk appeared first on Dr. William Davis.
January 1, 2015
New cities to air Wheat Belly Total Health!

The Wheat Belly Total Health Public Television Special will be airing on New Years Day, January 1st, 2015 in the cities listed here. But more Public Television stations have been added to the list! If you are new to the Wheat Belly message, this is a terrific way to start out the year empowered by the most powerful nutritional strategies available.
In addition to those listed in a previous Wheat Belly Blog post, these cities will also be airing the Wheat Belly Total Health special on New Years Day:
Los Angeles, California
Ft. Myers/Naples, Florida
West Palm Beach, Florida
Albany Georgia
Augusta, Georgia
Chattanooga, Georgia
Cochran, Georgia
Columbus, Georgia
Jacksonville, Georgia
Savannah, Georgia
Chicago, Illinois
Indianapolis, Indiana
Boston, Massachusetts
Springfield, Massachusetts
Burlington, New Hampshire
Portland/Auburn, New Hampshire
Cleveland/Akron, Ohio
Youngstown, Ohio
Philadelphia, Pennsylvania
Roanoke/Lynchburg, Virginia
If you miss the New Years Day showing, the Wheat Belly special will air just about every day for the next several days in many cities. Please check local Public Television listings for time and date in your area.
The post New cities to air Wheat Belly Total Health! appeared first on Dr. William Davis.
December 31, 2014
Celebrate the New Year With These Recipes!
 Here are a two Wheat Belly recipes that you can enjoy for your New Year holiday!
Here are a two Wheat Belly recipes that you can enjoy for your New Year holiday!
Anyone new to the Wheat Belly discussion: Choose the most benign sweeteners such as pure powdered or liquid stevia; monk fruit; erythritol; Wheat-Free Market sweetener; Swerve; Truvia. We avoid sugar, agave nectar, coconut sugar, or other fructose-containing sweeteners.
Irish Cream
This is an adults-only treat!
If you are a fan of the Irish Cream served as a liqueur or splashed over ice cream or other desserts, this is how you make a healthy version rich with all the flavor but with none of the sugar. I provide the dairy-free version here. Replace the coconut milk with an equivalent quantity of cream or half-and-half for a dairy version. Use the highest quality cocoa powder for the best flavor.
I’ve made this many times and presented it as a gift in a decorative glass bottle, perfect for the holidays. Optionally, top with shaved dark chocolate, ground cinnamon, or serve with a stick of cinnamon or topped with whipped cream. For an alcohol-free version, leave out the rum.
If you use coconut milk, note that refrigeration will make it too thick to drink; allow to sit at room temperature for about an hour to let the oil liquefy.
Makes approximately 2 cups
1 14-ounce can coconut milk
3½ tablespoons unsweetened cocoa powder
Sweetener equivalent to ½ cup sugar
1 tablespoon instant coffee granules
½ teaspoon ground cinnamon
1 1/2 cups unflavored rum
In blender, combine coconut milk, cocoa powder, sweetener, coffee granules, cinnamon, rum and blend until well combined. Serve with optional toppings.
Store in airtight bottle or jar in refrigerator.
Amaretto Macaroons
Here’s a creamy, melt-in-your-mouth treat that has the flavor of the popular liqueur, amaretto. They’re heavenly with coffee. As always, it is wheat/grain-free, very low-carb, and rich in fats.
Makes 16 macaroons
8 ounces whipping cream
2 cups unsweetened shredded coconut
½ cup sliced almonds
Sweetener equivalent to ¼ cup sugar
1 teaspoon almond extract
Whip cream until stiff peaks form. Stir in coconut, almonds, sweetener, almond extract and mix.
Spoon mixture with cookie scoop or spoon onto plate or platter and shape as desired. Cool in refrigerator for at least 30 minutes prior to serving.
The post Celebrate the New Year With These Recipes! appeared first on Dr. William Davis.
December 30, 2014
Make Wheat Belly Total Health part of your New Year’s resolution!

The Wheat Belly Total Health Public Television Special will be airing on New Years Day, January 1st, 2015 in the following cities:
Phoenix, Arizona
Colorado Springs, Colorado
Denver, Colorado
Grand Junction, Colorado
Steamboat Springs, Colorado
Salisbury, Seaford, and Wilmington, Delaware
Boston, Massachusetts
Detroit, Michigan
Lansing, Michigan
Fort Myers and Naples, Florida
West Palm Beach, Florida
Durham, New Hampshire
Keene, New Hampshire
Albuquerque, New Mexico
Garden City, New York
Cincinnati, Ohio
Pittsburgh, Pennsylvania
Burlington, Vermont
Seattle, Washington
Please check local Public Television listings for time and date in your area. If you are new to the Wheat Belly message, this is a terrific way to start out the year empowered by the most powerful nutritional strategies available!
The post Make Wheat Belly Total Health part of your New Year’s resolution! appeared first on Dr. William Davis.
Dr. Davis Infinite Health Blog
Recognize that this i The insights and strategies you can learn about in Dr. Davis' Infinite Health Blog are those that you can put to work to regain magnificent health, slenderness, and youthfulness.
Recognize that this is NOT what your doctor or the healthcare system provides, as they are mostly interested in dispensing pharmaceuticals and procedures to generate revenues. The healthcare INDUSTRY is not concerned with health--you must therefore take the reins yourself.
Dr. Davis focuses on:
--Real, powerful nutritional strategies
--Addresing nutrient deficiencies unique to modern lifestyles
--Deep insights into rebuilding the microbiome disrupted by so many modern factors
Follow Dr. Davis here and on social media and you can witness the extraordinary successes people enjoy on his programs. ...more
- William Davis's profile
- 159 followers



