Mark Sisson's Blog, page 180
June 8, 2017
ACEs and Primal Health
 It’s fair to say that I gravitate towards tangible, actionable subject matter when it comes to improving my own and others’ health. Things like nutrition, fitness, sleep, hormonal responses, and supplement science may seem like a lot to chew on for the layperson, but these are my personal passions as well as my long-time profession.
It’s fair to say that I gravitate towards tangible, actionable subject matter when it comes to improving my own and others’ health. Things like nutrition, fitness, sleep, hormonal responses, and supplement science may seem like a lot to chew on for the layperson, but these are my personal passions as well as my long-time profession.
And while these are certainly the big, actionable players in the game of health, I fully acknowledge there may be more lurking behind the scenes than we realize. A body that refuses to heal no matter how Primal you eat. Stubborn health conditions that simply refuse to fully go away, despite all the changes you make in your life. A propensity for disease that defies everything you’ve learned about ancestral nutrition and wellness. An intriguing new angle in the health sphere suggests the hurdle for some people may be embedded deeper than outer changes can access.
What Are ACEs (Adverse Childhood Experiences)?
Oddly enough, it all began with a weight loss program. Working out of Kaiser Permanente in Oakland, CA, Dr. Vincent Felitti was on a mission to get to the bottom of obesity. The problem was, the patients in his program kept dropping out, and he had no idea why. After a series of rather awkward and unintended questions, an interview with one obese woman provided the answer: Adverse Childhood Experiences (ACEs).
It turned out that the woman had been sexually abused as a kid, and her weight gain was a way of disappearing; of minimizing her risk of further sexual assault. Felitti dug deeper, and discovered that of the hundreds in his weight loss program, at least half of his patients had suffered from some form of ACE. What those people had experienced in their childhoods was somehow systematically preventing them from losing weight. If they did manage to lose weight, they regained all of it in short order.
The findings couldn’t be ignored, and Felitti soon teamed up with Dr. Robert Anda from the CDC to delve deeper. Beginning in 1995 and running until 1997, the resulting ACE study was one of the largest of its kind, encompassing a whopping 17,000+ participants. What Felitti and Anda found not only verified the earlier links between obesity and ACEs, but amplified them exponentially. Adverse Childhood Experiences were a pivotal factor for many of the most common major diseases and health conditions of our time.
The findings were simple yet far-reaching. Through the use of an uncomplicated questionnaire and scoring system, each participant was assigned an ACE score. Each traumatic experience during their childhood would give them a point, with more adverse experiences equating to a higher score. These experiences included sexual, verbal and physical abuse, five forms of family dysfunction (alcoholism, violence, incarceration, divorce, or abandonment), and 2 forms of neglect. Someone who had been verbally abused and had an alcoholic mother, for example, would get an ACE of 2. Those fortunate souls without any adverse experiences sailed through the survey with 0.
How ACEs Affect Our Health
Our heroes at Kaiser Permanente found that, perhaps unsurprisingly, the higher the ACE score, the greater the propensity for certain diseases. But it was the extent to which those ACEs affected the health of participants that had me doing a double take. Compared with people who achieved an ACE score of 0, those who ticked 4 ACE boxes were found to be at a 240% greater risk of hepatitis, and a 390% higher risk of developing chronic obstructive pulmonary disease. As the score went up, Felitti and Anda noted that people were more prone to violence, more broken marriages, more broken bones, more drug prescriptions, more depression, and more auto-immune disease. Thanks a lot, childhood.
As Felitti and a host of other researchers dug deeper in the following years, the picture became even more ominous. In short order, a higher ACE score was linked to greater risk of ischemic heart disease, chronic and frequent headaches, lung cancer and other forms of cancer, and liver disease. Whichever disease or health condition researchers homed in on, inevitably a link was found to Adverse Childhood Experiences. More “minor” but broadly influential conditions like sleep disturbance corresponded with ACEs as well with those people who had an ACE score of 5 or more being up to 2.4 times more likely to have trouble falling or staying asleep. As the ACE count went down, the sleep quality slowly improved.
Taking a step back, it became apparent that ACEs were impacting all areas of health. People with an ACE score of 5 or more had a nearly threefold increase in rates of psychotropic drug subscriptions, while a 2009 study conducted by Felitti and company found that risk of autoimmune disease in general went up significantly with increasing adverse experiences during the childhood or teen years. Breaking it down, they demonstrated that an ACE score at or above 2 meant a 70% increased risk of idiopathic myocarditis (a cardiovascular disease), 80% greater risk for myasthenia gravis (a chronic autoimmune neuromuscular disease), and 100% increased risk for rheumatic diseases. I don’t like those odds.
The ACE Pyramid
As Felitti and his team began to piece together the links between current-day health and past adverse experiences, a certain trend started to emerge. That trend is as follows:
Adverse childhood experiences
Disrupted neurodevelopment
Social, emotion and cognitive impairment
Adoption of health-risk behaviors
Disease, disability and social problems
Early death
It looks like a decidedly morbid take on something that happened many years ago during childhood, but if the numbers are anything to go by it’s a very accurate synopsis. This progression, known as the ACE Pyramid, was observed and documented in thousands upon thousands of people.
Demographically speaking, in the original study of 17,000 participants, nearly 75% were white. Almost 40% had a college or graduate degree. Another 36% had some college.
In a 2009 commentary posted in the Journal of Academic Pediatrics, the Godfather (aka Felitti) himself noted that the pathway from ACE to early death isn’t always linear. ACEs can work their destructive ways via two feedbacks: first, disease and early death is the consequence of various trauma-coping mechanisms like smoking, overeating and drug use. In this scenario, the maladaptive behavior brought on by the trauma of childhood could lead to excessive eating and poor diet, for example, which then leads to type 2 diabetes, the culmination of which is coronary artery disease.
Second, chronic stress generated by the trauma (and the brain’s inability to let go of the incident) directly leads to impairment of immunity and chronically elevated inflammation, which in turn paves the way for disease. Even worse, both of these mechanisms can work in tandem, further sealing the fate of the person in their grip.
The Neurobiological Role of Trauma
Where things get interesting indeed is with regards to neurobiology. The trauma of Adverse Childhood Experiences can literally rewire and re-form the brain, changing the way a person develops neurologically for the rest of his/her life without intervention. As this study noted, “the risk of every outcome in the affective, somatic, substance abuse, memory, sexual, and aggression-related domains [of the brain] increased in a graded fashion as the ACE score increased.” The result of a single ACE, then, could be permanent impairment of multiple brain structures and functions.
Put simply, the stress of a traumatic childhood event, such as being beaten or constantly belittled, releases hormones that physically damage a child’s developing brain. These children live their lives in a constant state of fight or flight, as the brain begins to perceive everyday places and situations as potentially dangerous. Thus, an adaptation to danger becomes a maladaptation in its permanency.
With the world either promising danger around every corner or heaping guilt on the developing child, they begin to find solace in diversions. Food, alcohol, drugs, sex, high-risk sports—anything to get their minds off the trauma that is set on rerun in the back of their minds.
But while this is easy to compute in theory, it’s much harder to diagnose in practice. A neurobiological response to an ACE may remain dormant for years, perhaps not even emerging until much later on in a person’s adult life. A triggering event or phase hits, and latent dysfunction goes haywire, developing into mental illness or morbid obesity, or ruining their marriage (take your pick). So, was it really a midlife crisis gone horribly wrong, or an ACE finally rearing its ugly head?
Add to this the fact that trauma, like many factors, interacts with genetic susceptibility, and we’ve got a very confusing picture indeed. Two people in the same household can go through the exact same experiences but be affected in very different ways, depending on an innate dimension of resilience.
It’s generally assumed that neurobiological markers for PTSD are acquired following a traumatic event. What researchers are finding, however, is that certain PTSD symptoms in a patient may in fact represent pre-existing “upstream” pathological functions that remain dormant until released by trauma. Meaning some of us were hard-wired for obesity, but just needed a supremely unpleasant event to unlock that unhealthy potential.
The Far-Reaching Significance of ACEs
Rather than trying too hard to convince you why these findings are so important, I’ll refer you to Nadine Burke Harris and her excellent TED Talk. She paints a vivid picture from a practitioner’s perspective, explaining that ACEs essentially provide the missing link to solving head-scratching health cases in many patients.
But if we’re looking for cold, hard facts, it’s hard to ignore the economic viability of integrating ACEs into healthcare. According to a CDC study published in 2012, a single year of trauma during childhood can add up to $124 billion in costs over the lifetime of those children. Of those costs, healthcare and productivity loses account for the lion’s share. If recognizing and treating ACEs could cut those costs by even a quarter, we’re talking astronomical savings down the line.
But what’s the entry point for action here?
In this case, I’d say it starts with knowledge as power—recognition, self-reflection, and support as needed. Just because someone is consciously healthy now, doesn’t mean they’re living their best life. It doesn’t mean they’re immune to the effects of any latent traumatic childhood events they’ve been unwittingly carrying around. These factors might be responsible for any number of unexplainable things that have and continue to happen in a person’s life, including stubborn health anomalies.
For this reason, the true importance of ACEs lies with you. Recognizing any ACE influence from your own history can provide Burke’s missing link for your own self-diagnosis, enabling you to direct your healing inwards, finally accessing the potential undercurrent of chronic stress and correcting coping behaviors that have been set on repeat. Maybe a strong innate resilience protected you from lasting effects. Maybe that isn’t the case. Unpacking the question may just open up the possibility for a better life, and improved long-term health.
Healing with ACEs
It might seem a bit cliche, but recognizing that you might be harboring a traumatic event or experience from your childhood can be an incredibly productive, even “freeing” step. There’s plenty of people within the Primal community who have had to work ridiculously hard to get their health back on track—harder than the average person should have to work, it seems. They might occasionally wonder why eating this way or living that way promotes healing in others but doesn’t have any effect on them, or why they always seem to gain weight with but the slightest of dietary tweaks. Or why the penchant for self-sabotage is so powerful….
With this in mind, maybe you’d be interested in taking the quiz. It’ll force you to cast your mind back and analyze your childhood from an objective viewpoint, highlighting experiences that you might formerly have brushed over. Take it seriously—this might just change your life.
The amygdala part of your brain can be relaxed, the hippocampus can restore proper memory function, and the nervous system can rewire itself back to a semblance of normalcy. Ever-present stress can be banished, and widespread inflammation can dissipate.
There’s also a link between gut dysbiosis and stress, and even a single traumatic event can shift your microbiome. We’re familiar with this by now, and recognize that a healthy gut microbiome and a healthy intestinal lining is critical to both physical and mental health. Use this knowledge—it’s a powerful weapon against PTSD and other accumulated symptoms from buried ACEs.
But this is just the start. Your pathway will need to be one of calm consideration and deep inflection. Here’s a quick set of suggestions for moving through it.
Write it down. Writing about traumatic or emotional events in one’s life has been directly correlated to improvements in both physical and psychological health. Studies generally indicate that 20 minutes a day is a good amount for this kind of traumatic digging. Examine the event(s) from every angle. It’s up to you what you do with the writing afterwards, but burning it is always cleansing (provided you don’t burn the house down in the process).
Practice mindfulness meditation. We keep coming back to meditation as a form of mental rewiring, and it’s not without reason. The research is there to back it up time and again.
Find a skilled therapist. Sharing your experience with an impartial third party can help you to find resolution, along with acceptance of a past you can’t change. There’s no reason this should be work you make yourself do alone. Community heals. The right therapist might be part of the breakthrough you’ve been looking for.
Look to embodied therapies. Top experts in the field of trauma consider this the new standard for healing because effective embodiment therapies uniquely access parts of the brain most severely distorted by trauma. This could include (particularly trauma-sensitive) yoga (which in one study offered more sustainable resolution to trauma than talk therapy did).
Final Thoughts…
Developments in ACEs represent one of the rare forays of “mainstream” medical thinking into something resembling a more holistic, less reactive style of healthcare. Clearly, it’s only one small offshoot, and as the CDC has cut virtually all funding to this area of research it’s got many roadblocks ahead of it, but it shows some serious promise.
More importantly, it forces us to examine our history in a different light. We are the culmination of a lifetime of experiences, and not all of those experiences are positive. A Primal approach to health should be open-minded and even fearless. In treading where we’re wary to go, we may discover the circumstances that got us stuck in the first place. Loosening old burdens means a freer life and more expansive health.
Thanks for reading, everyone. I’d love to hear your thoughts on this one. Take care.
The post ACEs and Primal Health appeared first on Mark's Daily Apple.



21-Day Check-in (and Plug for Instagram)
 I’ll be serving up a traditional post soon, but I thought I’d check in and see how everybody is doing. I know we have a LOT of folks participating in the 21-Day Challenge led by my excellent staff. It’s been exciting to watch from the sidelines this week—to see them share their best tips and connect with our audiences.
I’ll be serving up a traditional post soon, but I thought I’d check in and see how everybody is doing. I know we have a LOT of folks participating in the 21-Day Challenge led by my excellent staff. It’s been exciting to watch from the sidelines this week—to see them share their best tips and connect with our audiences.
If you aren’t joining the crew on Vimify (or if you are!), you can check out their Instagram Story videos and photos from the Mark’s Daily Apple, Primal Blueprint, and PRIMAL KITCHEN® Instagram accounts. (Just click on the circle logos when you pull up the app to see the latest additions.) The staff and videos are all different, so you’ll get the most by following all three channels. Definitely worth popping in and seeing what they’re up to!
Have a great day, everybody, and Grok on!
The post 21-Day Check-in (and Plug for Instagram) appeared first on Mark's Daily Apple.



June 7, 2017
The Definitive Guide to Keto
 I use my Los Angeles surroundings as a barometer for changes in the mainstream approach to health, and it holds up quite well. Silicon Valley can claim to be the cradle of technology, but L.A. is definitely the cradle of diet and fitness trends; and the latest is most definitely keto. At the local cafe where every species of Malibu fitness enthusiast gathers to gossip and fuel up, I’m seeing fewer gels and energy bars, and way more butter coffees and discarded packets of the new powdered ketone supplement products.
I use my Los Angeles surroundings as a barometer for changes in the mainstream approach to health, and it holds up quite well. Silicon Valley can claim to be the cradle of technology, but L.A. is definitely the cradle of diet and fitness trends; and the latest is most definitely keto. At the local cafe where every species of Malibu fitness enthusiast gathers to gossip and fuel up, I’m seeing fewer gels and energy bars, and way more butter coffees and discarded packets of the new powdered ketone supplement products.
Sure enough, keto is entering into mainstream health consciousness everywhere. Google searches for “ketogenic diet” are at an all-time high. The stream of keto-related email queries and comments I receive has seen a major uptick. And early this year, a major publisher approached me with a keto book proposal, which I accepted. I dove headlong into a total 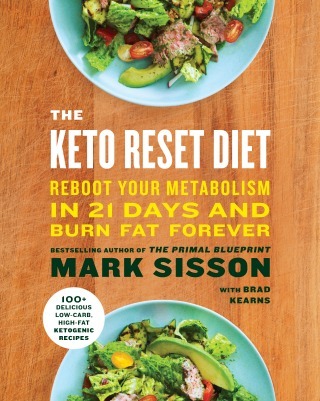 immersion/participatory journalism experience where I walked my talk, and pricked my finger for blood tests enough times to get a little scar tissue going, for the past several months. The book is called The Keto Reset Diet and it’s coming out October 3rd. This is a comprehensive presentation to educate you on the science and benefits of ketone burning and to give you step-by-step guidance to go keto the right away, avoiding the common setbacks that happen when many adopt an ill-advised approach to something as delicate and rigorous as nutritional ketosis. You can pre-order a copy from major retailers right now. We are also filming a comprehensive online multimedia educational course to give you a guided immersion experience that will be available in 2018.
immersion/participatory journalism experience where I walked my talk, and pricked my finger for blood tests enough times to get a little scar tissue going, for the past several months. The book is called The Keto Reset Diet and it’s coming out October 3rd. This is a comprehensive presentation to educate you on the science and benefits of ketone burning and to give you step-by-step guidance to go keto the right away, avoiding the common setbacks that happen when many adopt an ill-advised approach to something as delicate and rigorous as nutritional ketosis. You can pre-order a copy from major retailers right now. We are also filming a comprehensive online multimedia educational course to give you a guided immersion experience that will be available in 2018.
Meanwhile, it’s definitely time to do a Definitive Guide….
To understand ketogenic diets, you must understand the conditions that promote ketosis. And to do that, you must understand how our bodies beta-oxidize fatty acids for energy.
Fatty acids are broken down into acetyl-CoA.
Acetyl-CoA combines with oxaloacetate.
The acetyl-CoA/oxaloacetate duo starts the Krebs cycle.
The Krebs cycle produces ATP, the body’s energy currency.
Congratulations. You’ve just turned fat into energy.
Where does ketosis come in?
If the supply of acetyl-CoA exceeds the supply of oxaloacetate, the liver converts any excess acetyl-CoA into ketone bodies. These ketone bodies are an “alternative” energy source for the brain and body.
Both carbohydrates and protein provide oxaloacetate to the liver, so both carbohydrates and protein can prevent ketone production or knock you out of ketosis. Carbohydrates also elevate insulin, which blocks the release of body fat and reduces the amount of fatty acids making their way to the liver for conversion into ketones. A ketogenic diet, then, is one that limits carbohydrate and, to a lesser extent, protein.
Ketosis occurs in certain instances without any dietary change at all:
Extreme physical exertion that depletes liver glycogen (total around 100 grams) and depletes around half of stored muscle glycogen (total around 400-500 grams)
Fasting for significant time period (at least 24 hours for most people)
Starvation or significant restriction in total calories for a signification time period
In all of these conditions, there’s a common ketogenic thread: liberation of body fat in excess of that which we can beta-oxidize. Any fat that isn’t beta-oxidized for energy will convert to ketones.
In one sense, ketosis is a stop-gap solution for situations where you’re burning huge amounts of body fat, like during a famine. Why would I want to mimic abject starvation if there’s all this food around?
Grocery stores are an evolutionary aberration. The constant drip of glucose into our blood is a modern luxury. For most of human history, if we wanted carbs, we had to climb a tree and extricate a bee’s nest, spend hours digging tubers, or wait around for the wild fruit to ripen. We are adapted to periods of low food availability, and, especially, low glucose availability.
Plus, humans are remarkably good at slipping into ketosis. Whereas for most other animals ketosis is difficult to achieve, a human will be mildly ketotic just waking up from a full night’s sleep. Heck, breastfed babies spend much of their time in ketosis despite drinking nutritionally balanced breastmilk. We’re clearly meant to produce and utilize ketones from time to time, and it’s safe to assume that mimicking this ancestral milieu provides adaptive benefits.
Let’s go over some of the major ones.
Adaptive Benefits of Ketosis
Treatment for Major Disease States
The ketogenic diet first emerged as a tool for clinicians to treat their patients with epilepsy. It was—and remains—the only thing with the consistent ability to prevent seizures. Whether it’s Thai kids with intractable epilepsy, Scandinavian kids with therapy-resistant epilepsy, or adults with refractory epilepsy, ketogenic diets just work.
Ketosis improves epilepsy via several mechanisms.
It increases conversion of glutamate into glutamine into GABA, reducing neuronal excitability.
It increases antioxidant status in the neuronal mitochondria, improving their function.
It reduces free radical formation in neurons, a likely cause of seizures.
These effects on neuronal function and health, along with the ability of aging or degenerating brains to accept and utilize ketone bodies, also have implications for other brain conditions, like Parkinson’s, Alzheimer’s, bipolar disorder, and many psychiatric disorders.
Ketogenic diets aren’t just beneficial for brain disorders, though.
A Spanish ketogenic diet (keto with wine, basically) cured people of the metabolic syndrome and improved health markers of non-alcoholic fatty liver disease. Over 92% of subjects improved their liver health; 21% resolved it entirely.
In cancer patients, a keto diet preserves lean mass and causes fat loss. Many researchers are exploring the use of ketogenic diets in preventing and treating cancer, although results are very preliminary.
Cognitive Function
Since ketosis can help with major brain disorders, many have wondered whether it can improve cognitive function in otherwise healthy people. Unfortunately, researchers haven’t studied the nootropic effects of ketogenic diets in healthy people—yet. They have looked at people with “milder” cognitive deficits, though, finding some promising effects.
In mild cognitive decline, a ketogenic diet improves memory.
In type 1 diabetics who experience reduced cognitive function when their blood sugar is low, increasing ketone production via medium chain triglycerides (found in coconut oil) restores it.
In adults with bad memory, adding ketones improves cognition. The higher the serum ketones, the better the scores.
In older adults, a very low-carb diet improves memory. Again, higher ketones predicts bigger improvements.
Anecdotes abound of people with intact cognitive function going on ketogenic diets and experiencing huge benefits to their mental performance. I’ve been experimenting with more protracted ketosis for some time now, and I can add my hat to the pile. What could be going on?
It may clear up brain fog, that enemy of clear thinking, by clearing ammonia from the brain and upregulating conversion of glutamate into GABA.
It definitely increases brain energy production by increasing mitochondrial biogenesis in the brain. More mitochondria, more energy production.
It tends to produce a sense of euphoria. If you can parlay that into productivity instead of getting caught up in the sensation, your mental output will increase. A cup of strong coffee helps here.
Physical Performance
Being keto-adapted has several advantages for anyone interested in physical performance.
It increases energy efficiency. At any given intensity, a keto-adapted athlete burns more fat and less glycogen than a sugar-burning athlete. Long-term elite keto athletes can burn up to 2.3 times more fat at peak oxidation and 59% more fat overall than non-keto athletes, and they do it at higher intensities. They remain in the predominantly fat-burning zone at 70% of VO2max, whereas non-keto athletes switch over from predominantly fat burning to a spike in sugar-burning at 54.9% VO2max.
It spares glycogen. Glycogen is high-octane fuel for intense efforts. We store it in the muscles and liver, but only about 2400 calories-worth—enough for a couple hours of intense activity at most. Once it’s gone, we have to carb up to replenish it. Keto-adaptation allows us to do more work using fat and ketones for fuel, thereby saving glycogen for when we really need it. Since even the leanest among us carry tens of thousands of calories of body fat, our energy stores become virtually limitless on a ketogenic diet.
It builds mitochondria. Mitochondria are the power plants of our cells, transforming incoming nutrients into ATP. The more mitochondria we have, the more energy we can utilize and extract from the food we eat—and the more performance we can wring out of our bodies. Ketosis places new demands on our mitochondria, who adapt to the new energy environment by increasing in number.
Fat Loss
Although keto is not a classical weight loss diet, it can certainly help a person lose body fat. After all, to generate ketones without eating ketogenic precursors, you have to liberate stored body fat.
But that’s not the main mechanism for ketogenic fat loss. Ketosis isn’t “magic”—it doesn’t melt body fat away. Instead, it works for many of the same reasons a standard low-carb Primal way of eating works: by reducing insulin, increasing mobilization of stored body fat, and decreasing appetite.
Ketosis suppressing appetite may be the most important feature. The overriding drive to eat more food is the biggest impediment to weight loss, and it’s the reason why most diets fail. When people attempt to eat less food despite wanting more, they butt up against their own physiology. Few win that battle.
Ketogenic dieting avoids this issue altogether, suppressing the increase in hunger hormones that normally occurs after weight loss.
Ketogenic diets are especially effective for massive weight loss. If you have a ton of weight to lose, aiming for ketosis could help you lose body fat. Again, not because of any inherent fat-burning quality of the ketones, but because in order to make ketones you must liberate stored body fat.
Many diets work in the short-term and fail in the long run. Weight loss isn’t worth anything if you can’t keep it off. Ketogenic diets appear to be good for long-term maintenance of weight loss, at least compared to low-fat diets.
How to Do It Right
I’ll have more details in The Keto Reset Diet book, but there are right ways and wrong ways to do keto. What’s wrong or right is contextual, of course. It depends on several factors.
If you’re part of a small group that uses keto to keep seizures at bay, or treat serious neurological diseases, you’ll want to diligently maintain high blood ketone levels. That means sticking to very-low-carb (5-10% of calories) and low/moderate protein (10-15% of calories). But even then, modified ketogenic diets with slightly higher carbs and relaxed protein intakes are also effective against epilepsy.
If you’re doing keto for general health or weight loss, you can handle more protein and still remain in ketosis. Protein will help stave off the muscle loss, and, because calories are reduced, you can handle a bit more protein without interfering with ketosis. An older ketogenic diet study in obese subjects shows that 50% protein diets are highly ketogenic as long as calories are kept low. And in another study, subjects eating a weight-maintaining ketogenic diet ate up to 129 grams of protein without leaving ketosis (129 grams is fairly high).
If you’re trying to lose weight, artificially boosting ketones won’t accelerate the process. Higher ketones do not enhance fat loss, but they may indicate it’s taking place.
How to Make Keto Work
Ketogenic dieting is a big jump for some people. You’re literally switching over to a new metabolic substrate. That can take some getting used to. Make sure you are well-prepared with a Primal-aligned eating pattern in place for ideally several months before you ponder a journey into nutritional ketosis.
Make a minimum commitment to six weeks of nutritional ketosis. The first three weeks will be the most difficult as you transition to new fuel sources, but then you can expect breakthroughs. Some serious athletes may experience a temporary performance dip in the early weeks, but then will come back strong after 4 weeks and beyond. Once you get to the six-week mark, the metabolic machinery is in place, and it’s hard to reverse the adaptation. Extra mitochondria don’t just disappear.
Get plenty of electrolytes. You’ll want lots of sodium, magnesium, and potassium. Try 4.5 grams sodium (about 2 teaspoons of fine salt or a little under 3 teaspoons of kosher salt), 300-400 mg magnesium, and 1-2 grams of potassium each day on top of your normal food. Going keto really flushes out water weight, and tons of electrolytes leave with it.
Eat fat, but don’t be crazy about it. Just because a ketogenic diet is a high-fat diet doesn’t mean you should eat ungodly amounts of fat. Being ketogenic is more about not eating carbohydrates than it is eating as much fat as you possibly can.
Eating extra fat in the first 4-7 days can accelerate keto-adaptation by increasing AMPK signaling. Dial it down after.
Lift heavy things. A common criticism of ketogenic diets is that they cause loss of lean mass. This isn’t totally unfounded. If your ketogenic diet reduces appetite so much that you undereat, you might lose muscle. If you’re on a super-low-protein ketogenic diet, you might lose muscle. Lifting weights prevents these issues by sending an anabolic signal to your muscles and allowing the consumption of more protein without hampering ketosis.
Do lots of low level aerobic activity. Walk, hike, jog, cycle, row. Keep things in the aerobic HR zone (under 180 minus age in heart beats per minute), and you’ll increase your utilization of body fat, which will speed up ketone production and adaptation.
Eat vegetables. The vast majority of vegetables are keto-friendly. Not only do they provide important micronutrients and phytonutrients, they provide negligible amounts of carbohydrates.
Eat berries. Raspberries, blackberries, strawberries, and blueberries are all quite low in glycemic load and extremely high in phytonutrients. While eating a flat of strawberries isn’t very ketogenic, a large bowlful won’t knock you out.
Eat fiber. Many people on ketogenic diets tend to ignore or malign fiber. That’s a mistake. First, fiber doesn’t digest into glucose. It doesn’t “count.” Second, fiber feeds your gut biome, providing fermentable substrate for your gut bacteria to turn into beneficial short chain fatty acids and to provide support to your immune system.
How to Know if You’re Ketogenic
You can test your blood, urine, or breath ketones. There are drawbacks to each, and unless you have a medical condition necessitating a specific level of ketones, obsessive testing may be unnecessary/unwise/expensive. Forget the inexpensive urine strips, as they measure only what you excrete, not what you are making and burning.
Once you’re keto-adapted and naturally good at burning fat, the ketone measuring devices might not put up impressive numbers. That’s because, after weeks in ketosis, you have built enough metabolic machinery in your muscles that they run extremely well on free fatty acids and don’t require much additional fuel from glucose or ketones. You’re still making ketones, since your brain can’t run on fatty acids and needs them to offset the glucose that isn’t coming, but your muscles no longer require them. Many people who have been in long term ketosis can get by quite nicely on 20-30 net grams of carbs a day and might only show .4 or .7 millimolar ketones on a blood test, but they have plenty of energy from burning free fatty acids and maintain muscle mass on relatively fewer calories than when they were dependent on carbs. Few people understand this, but it’s a major benefit of keto-adaptation. You might even say that ketogenic diets are ultimately about becoming free fatty acid-adapted.
Instead of objective numbers, I prefer to go by symptoms and signs. Since you’re trying to divine what works best for you, relying on the subjective signs and symptoms you experience is perfectly legitimate. These include:
Reduced urge to snack: Being ketone-adapted means you’re less reliant on outside calories.
Steady energy: When I’m feeling full of relaxed energy, calm but not sleepy, I know I’m in ketosis.
You may have heard talk about the dreaded ketone breath, caused by the presence of the metabolite acetone (the breakdown product of the ketone bodies acetoacetate and beta-hydroxybutyrate). A sweet and fruity odor to your exhalations is a reliable indicator that you are in a state of ketosis, but it’s also a likely indicator that you are not yet super efficient at burning ketones. Don’t worry, that will come in short order.
So, are carbs out forever? What if you want to incorporate carbs for high intensity performance while maintaining the benefits of ketosis?
First of all, it may not make much of a difference if you’re just strength training. A series of recent studies looked at the effects of introducing carbs into a ketogenic diet in resistance trained adults, finding little to no benefit.
Carbs likely will help certain populations, namely CrossFitters, sprinters, and anyone else engaged in intense glycolytic work. But even then, being keto-adapted reduces the amount of glycogen you’ll use for a given intensity —so err on the side of fewer carbs and eat only as many as you actually earn.
There are two basic ways to construct a ketogenic diet that includes carbs: with one big weekly carb load (the classic CKD) or multiple smaller carb loads adjacent to training sessions (often called the targeted ketogenic diet, or TKD).
On a CKD, you spend the majority of the week and your workouts in ketosis and devote a day or a pair of days to eat lots of carbs. You might be ketogenic Monday through Friday, exercising all the while and capping the work week off with a really intense glycogen-depleting training session, then go high-carb, low-fat Saturday through Sunday to refill your depleted and newly-insulin sensitive muscle glycogen stores.
On a TKD, you spend the majority of your time in ketosis but selectively eat carbohydrate before, during, and/or after your workouts. Most people seem to benefit most from pre- and peri-workout carbs. These aren’t large carb loads — 15-30 grams of relatively fast-absorbing, simple carbs. If you don’t want to opt for dextrose or other powders, a baked potato works well.
Whatever option you choose, you’ll need to deplete glycogen if you want to include carbs in a ketogenic diet. As long as you have a glycogen debt, any carbs you eat will go toward restoring those glycogen stores and won’t interfere with ketone production.
Final Thoughts…
Also: Ketosis doesn’t have to be for life.
Going ketogenic can be refreshing. You’re not hungry like before. You’re euphoric. You have steady, even energy levels. Your brain works better. You’re leaner. You start thinking: Why not do this all the time?
A recent study of long-term (5 years) ketogenic dieting in patients with glucose transporter 1 deficiency syndrome found no apparent downsides. Bone mineral density, which can be a problem for growing kids on long term ketogenic dies for epilepsy, was unaffected.
Yet, I’ll admit to being a bit leery of long-term, protracted ketosis in people who aren’t treating a medical condition. It just doesn’t seem necessary. After all, while humans are unique in our ability to slip into ketosis and there are clear evolutionary precedents for being in ketosis, Grok wasn’t starving all the time. He wasn’t living through famine after famine.
Not everyone needs to be on a ketogenic diet. Even fewer need to be on a ketogenic diet for life. But I do think that everyone should try it for a few or (even better) six weeks, build and install some new mitochondria, remain long enough to get really good at burning free fatty acids in your muscles, and then return to a ketogenic state on a regular basis to keep your capacities topped up.
That’s it for me today. Have you recently tried keto, or are you hoping to? Maybe you’ve done it for a while. I’d love to hear your tips and questions. Thanks for stopping by, and have a great week, everyone.
The post The Definitive Guide to Keto appeared first on Mark's Daily Apple.



June 6, 2017
3 Ways to Regulate Insulin That Have Nothing to Do with Food
 Today’s guest post is served by a good friend of Mark’s Daily Apple, Dr. Sarah Ballantyne, PhD, or as you might know her—The Paleo Mom.
Today’s guest post is served by a good friend of Mark’s Daily Apple, Dr. Sarah Ballantyne, PhD, or as you might know her—The Paleo Mom.
Regulating blood sugar levels is a key feature of any health-promoting diet [15, 20] . High blood sugar levels after eating are a major stimulator of reactive oxygen species (ROS), which are chemically reactive molecules that have important roles in cell signaling (the complex communication between and within cells) and in homeostasis (maintenance of a stable environment inside and outside the cell). But ROS are also potent signals for inflammation and stimulate the production of proinflammatory cytokines (chemical messengers), and also injure cells and tissue. As a result, chronic high blood sugar levels can cause serious damage throughout the body, including to blood vessels and vital organs. This is why diabetes (chronical hyperglycemia) is associated with higher risk of stroke, cardiovascular disease, vision problems, kidney disease, and nerve damage.
When we consume carbohydrates, blood sugar increases. In response to the rise in blood sugar, the pancreas releases the hormone insulin, which facilitates the transport of glucose into the cells of the body and signals to the liver to convert glucose into glycogen and triglycerides for storage.
Using a wide array of enzymes, liver cells (called hepatocytes) first convert excess glucose into glycogen (which is stored in the liver and in muscle tissue) for short-term storage. When needed, the glycogen is rapidly converted back into glucose and released into the blood to maintain normal blood sugar levels and provide energy for the body’s cells between meals. There is also a maximum glycogen storage capacity in the muscle tissue and liver, so whatever glucose is consumed beyond that amount is converted into triglycerides (molecules composed of three fatty acids and a glycerol) for longer-term storage in adipocytes (fat-storage cells). This process is also stimulated by insulin. Triglycerides are released by the liver into the blood to circulate to adipose tissues (fat deposits), where they are taken up by adipocytes. So when we eat a high-carbohydrate meal, blood glucose and blood triglycerides are increased.
Chronically elevated blood sugar levels stimulate adaptations within cells, rendering them less sensitive to insulin. These adaptations may include decreasing the number of receptors to insulin embedded within the cell membranes and suppressing the signaling within the cell that occurs after insulin binds to its receptor. This causes the pancreas to secrete more insulin to lower the elevated blood-glucose levels. This is called insulin resistance or loss of insulin sensitivity, when more insulin than normal is required to deal with blood glucose. When blood-sugar levels can no longer be maintained in a normal range (due to the pancreas being unable to keep up with insulin demand and/or substantial loss or inhibition of insulin receptors in cells), you get type 2 diabetes.
While the Paleo diet and several other popular dietary templates focus on food choices that help to regulate blood sugar levels—generally, by moderating intake of carbohydrates while choosing low-glycemic-load options—blood glucose responses are impacted by more than just the quality and quantity of carbohydrates that we consume. In fact, there’s emerging evidence that lifestyle factors may be equally, or perhaps even more, important that dietary choices when it comes to insulin sensitivity.
1. Exercise
Physical activity provides a wide range of benefits, from improving bone density to cardiovascular health to metabolic health. Exercise helps improve insulin sensitivity through a direct action on the glucose transport molecules (GLUT-4 receptors) in the individual cells of our muscles [1]. It also affects the full range of hormones related to accessing stored energy and regulating how that energy is used. This “boost” in metabolism is one reason why exercising can make us feel more energetic throughout the day. This is also a major reason exercise is linked with a reduce risk of diabetes and cardiovascular disease.
On the flip side, sedentary behavior itself can actually induce insulin resistance. A series of studies performed in healthy adults, in overweight and obese adults, and in athletes have shown that even a relatively short period of inactivity (for example, 3-days bed rest due to injury, illness or volunteering for a clinical trial) induces insulin resistance [1, 7, 9, 17].
And, it’s a pretty major effect: one study in healthy adults showed a 67% increase in insulin secretion following a glucose challenge test (meaning two thirds more insulin was needed to regulate blood glucose levels) following 5-days of bed rest [9]. And, this inactivity-induced insulin resistance is paired with dyslipidemia, increased blood pressure, and impaired microvascular function—no wonder being inactive so dramatically increases risk of diabetes, obesity, and cardiovascular disease.
So, while exercise itself improves insulin sensitivity, we still need to avoid prolonged periods of inactivity, like sitting at a desk job. Fortunately, even short activity breaks regularly spaced throughout sedentary periods can dramatically improve glucose metabolism. One study in overweight and obese adults showed that a 2-minute movement break every 20 minutes of sitting time lowered post-meal glucose and insulin levels substantially [7].
What does this mean? It’s important to both include regular exercise into our routines but also to avoid prolonged periods of inactivity in order to regulate insulin sensitivity.
2. Stress
Psychological stress causes the release of both catecholamines (via activation of the sympathetic nervous system) and glucocorticoids (via activation of the hypothalamic-pituitary-adrenal [HPA] axis). The combined actions of catecholamines and glucocoritcoids like cortisol (as wells as corticotropin-releasing hormone which is also secreted upon activation of the HPA axis) prioritize the most essential functions for survival (perception, decision making, energy for our muscles so we can run away or fight for our life, and preparation for wound healing) while inhibiting non-essential functions (like some aspects of the immune system especially in the skin, digestion, kidney function, reproductive functions, growth, collagen formation, amino acid uptake by muscle, protein synthesis and bone formation). This is beneficial in the case of acute stress (from a survival standpoint) but is also the reason why chronic stress is so detrimental to immune and metabolic health.
Chronic stress causes insulin resistance, mediated directly via the actions of cortisol and indirectly via increased inflammation that is also a feature of chronic stress [14, 18, 19]. In fact, many researchers have proposed that chronic stress may be a dominant contributor to the pathogenesis of metabolic syndrome, that nasty combination of obesity, insulin resistance and/or type 2 diabetes, dyslipidemia and hypertension.
Epidemiological studies linking chronic stress with insulin resistance are now supported by mechanistic studies showing that chronically elevated cortisol is diabetogenic (meaning it can cause diabetes). Cortisol suppresses insulin secretion from pancreatic beta cells, impairs insulin-mediated glucose uptake in cells throughout the body (by inhibiting GLUT-4 translocation into the cell membrane), and by disruption of insulin signaling in muscle tissue [5, 10]. In addition, a growing list of inflammatory cytokines, such as TNF-? which is induced by chronic stress, are known to cause insulin resistance [8, 16].
Recent evidence shows that even acute stress causes hyperglycemia and insulin resistance [11]. Liver insulin signaling is impaired following acute stress independent of cortisol. Plus, cortisol acutely suppresses insulin secretion by the pancreas as well as increasing glucose output by the liver.
What does this mean? Both acute and chronic stress can directly cause insulin resistance independent of diet, making mitigating stress and improving resilience to stress a primary target for blood sugar regulation.
3. Sleep
Only about 35% of Americans get the recommended 8 hours or more of sleep each night. The health detriments of inadequate sleep are pervasive, affecting every system in the human body and increasing risk of nearly every chronic disease, including type 2 diabetes and insulin resistance. In fact, sleeping less than 6 hours per night (like an estimated 40% of Americans) increases risk of type 2 diabetes by 50%. And, if we pool diabetes and impaired glucose tolerance together, that risk soars to a whopping 2.4 times [12]!
In fact, a variety of studies evaluating the effects of partial sleep (sleeping 4 to 5 hours per night, rather than the recommended 8) demonstrate that inadequate sleep causes insulin resistance in healthy people [2, 3, 5, 12].
And while most studies show insulin sensitivity decreasing by 15-30% after four or five nights of partial sleep, one study showed that even a single night of partial sleep causes insulin resistance in healthy people (a 25% decrease in insulin sensitivity!)[6].
Sleep restriction also increases the measurable free fatty acids in the blood, a contributor to insulin resistance that plays a central role in the development of metabolic diseases. Getting 4.5 hours of sleep per night compared to spending 8.5 hours in bed increased serum free fatty acids in healthy men by 15 to 30 percent [13]!
What might be even more fascinating is that there’s emerging evidence that the impact of sleep on insulin sensitivity and glucose metabolism is even greater than diet. Research presented at last fall’s Obesity Society Annual Meeting showed that a single night of lost sleep was worse than six months of a high-fat Western diet in terms of insulin sensitivity and glucose metabolism [21].
Even a modest sleep debt, getting a mere 30 minutes less per night than you need on weeknights, can have a big impact on insulin sensitivity. One fascinating study looked at the impact of sleep on patients newly diagnosed with type 2 diabetes [2]. The study participants kept sleep logs, and the researchers calculated how much less sleep they got than the recommended 8 hours a night cumulative over the workweek (not including sleeping in to “catch up on sleep” on the weekends).They were randomized into one of three groups: usual care, physical activity intervention, or diet and physical activity intervention. When the participants were recruited, those that typically didn’t get enough sleep were 72% more likely to be obese. The researchers then followed the participants over a year to see what would change. Note that addressing sleep was not part of any of the study interventions. The amount of sleep debt that individuals had didn’t typically change during the study.
Sleep debt dramatically impacted risk of obesity and insulin resistance, and the correlation between the two increased throughout the study. At 12 months, for every 30 minutes of weekday sleep debt, the risk of obesity was 17% higher and the risk of insulin resistance 39% higher.
What does this mean? Getting adequate sleep every single night is absolutely critical for insulin sensitivity and blood sugar regulation! And given that inadequate sleep is considered a cause of chronic stress, this emphasizes the need to carve out sufficient time for sleep even more!
If you struggle to get enough sleep or the quality of your sleep needs improving, you will absolutely love the comprehensive and epic online sleep program I’ve created, Go To Bed! This program gives you all of the scientifically validated tips and tricks for improving your sleep and provides you with a 14-day challenge so you can get the best sleep of your life! Mark’s Daily Apple readers can save 10% off the entire Go To Bed online program by using coupon code DailyAppleSleep.
Take Home Message
Dialing in lifestyle habits are absolutely critical for maintaining (and regaining!) insulin sensitivity and regulating our blood sugar responses. So, for those who struggle with blood sugar regulation, rather than adopting more and more extreme dietary interventions (e.g. consuming fewer and fewer carbohydrates, which can cause dietary insufficiency of many important vitamins, minerals, antioxidant phytochemicals and fiber), have a critical look at your stress levels, your activity levels (both in terms of engaging in regular exercise and in terms of avoiding prolonged periods of inactivity), and your sleep habits. Chances are good that expending some effort into improving these will pay great dividends in terms of insulin sensitivity and overall health!
 Sarah Ballantyne, Ph.D. (a.k.a. The Paleo Mom) is the blogger behind the award-winning blog www.ThePaleoMom.com, cohost of the top-rated and syndicated The Paleo View podcast, and New York Times Bestselling author of The Paleo Approach, The Paleo Approach Cookbook, and The Healing Kitchen. Sarah earned her doctorate degree in medical biophysics at the age of 26. She spent the next four years doing research on innate immunity and inflammation before becoming a stay-at-home mom. After her second daughter was born, she began to experiment with the Paleo lifestyle. It had an amazing effect on her health, including contributing to her 120-pound weight loss! Over time, she healed herself of a long laundry list of physical complaints including: Hashimoto’s thyroiditis, fibromyalgia, Irritable Bowel Syndrome, acid reflux, migraines, anxiety, asthma, allergies, eczema, psoriasis and an autoimmune skin condition called lichen planus. Sarah successfully transitioned her originally skeptic husband and two spirited young daughters to a paleo diet and lifestyle. Her passion for providing straightforward explanations of the science behind the paleo diet and its modifications, plus her love of food and cooking and her dedication to her family form the foundations of her blog, her podcast and her books. You can also find Dr. Sarah on Facebook, Twitter, Instagram and Pinterest.
Sarah Ballantyne, Ph.D. (a.k.a. The Paleo Mom) is the blogger behind the award-winning blog www.ThePaleoMom.com, cohost of the top-rated and syndicated The Paleo View podcast, and New York Times Bestselling author of The Paleo Approach, The Paleo Approach Cookbook, and The Healing Kitchen. Sarah earned her doctorate degree in medical biophysics at the age of 26. She spent the next four years doing research on innate immunity and inflammation before becoming a stay-at-home mom. After her second daughter was born, she began to experiment with the Paleo lifestyle. It had an amazing effect on her health, including contributing to her 120-pound weight loss! Over time, she healed herself of a long laundry list of physical complaints including: Hashimoto’s thyroiditis, fibromyalgia, Irritable Bowel Syndrome, acid reflux, migraines, anxiety, asthma, allergies, eczema, psoriasis and an autoimmune skin condition called lichen planus. Sarah successfully transitioned her originally skeptic husband and two spirited young daughters to a paleo diet and lifestyle. Her passion for providing straightforward explanations of the science behind the paleo diet and its modifications, plus her love of food and cooking and her dedication to her family form the foundations of her blog, her podcast and her books. You can also find Dr. Sarah on Facebook, Twitter, Instagram and Pinterest.
Thanks to Dr. Sarah Ballantyne for today’s excellent post. Insights, questions? Share your thoughts in the comment section, and thanks for stopping by today. Enjoy the week, everybody!
Citations
1. Arciero PJ, et al, Effects of short-term inactivity on glucose tolerance, energy expenditure, and blood flow in trained subjects. J Appl Physiol. 1998;84:1365–1373.
2. Teresa Arora, et al, The impact of sleep debt on excess adiposity and insulin sensitivity in patients with early type 2 diabetes mellitus. J Clin Sleep Med. 2016 May 15; 12(5): 673–680.
3. Bosy-Westphal, A., et al., Influence of partial sleep deprivation on energy balance and insulin sensitivity in healthy women, Obes Facts. 2008;1(5):266-73
4. Broussard JL, et al, Impaired insulin signaling in human adipocytes after experimental sleep restriction: a randomized, crossover study. Ann Intern Med. 2012 Oct 16;157(8):549-57.
5. Coderre L, et al, In vivo effects of dexamethasone and sucrose on glucose transport (GLUT-4) protein tissue distribution. Am J Physiol. 1996 Oct;271(4 Pt 1):E643-8.
6. Donga, E., et al., A single night of partial sleep deprivation induces insulin resistance in multiple metabolic pathways in healthy subjects, J Clin Endocrinol Metab. 2010 Jun;95(6):2963-8.
7. Dunstan DW, et al. Breaking up prolonged sitting reduces postprandial glucose and insulin responses. Diabetes Care. 2012 May; 35(5): 976–983.
8. Glovatchcka, V, et al, Chronic stress-induced changes in pro-inflammatory cytokines and spinal glia markers in the rat: a time course study. Neuroimmunomodulation. 2012; 19(6): 367–376.
9. Hamburg, NM, et al, Physical inactivity rapidly induces insulin resistance and microvascular dysfunction in healthy volunteers. Arterioscler Thromb Vasc Biol. 2007 Dec; 27(12): 2650–2656.
10. Lambillotte C, et al, 1997 Direct glucocorticoid inhibition of insulin secretion. An in vitro study of dexamethasone effects in mouse islets. J Clin Invest 99:414–423
11. Li L, et al, Acute psychological stress results in the rapid development of insulin resistance. J Endocrinol. 2013 Apr 15;217(2):175-84. doi: 10.1530/JOE-12-0559. Print 2013 May.
12. Lucassen EA, et al., Interacting epidemics? Sleep curtailment, insulin resistance, and obesity, Ann N Y Acad Sci. 2012 Aug;1264(1):110-34
13. Rao MN, et al, Subchronic sleep restriction causes tissue-specific insulin resistance. J Clin Endocrinol Metab. 2015 Apr;100(4):1664-71.
14. Rosmond R 2003 Stress induced disturbances of the HPA axis: a pathway to Type 2 diabetes? Med Sci Monit 9:RA35–RA39
15. Samuel VT and Shulman GI. Mechanisms for insulin resistance: common threads and missing links. Cell. 2012 Mar 2;148(5):852-71.
16. Solomon SS, et al. TNF-alpha inhibits insulin action in liver and adipose tissue: A model of metabolic syndrome. Hormone and Metabolic Research. 2010;42:115–121.
17. Stuart CA, et al, Bed-rest-induced insulin resistance occurs primarily in muscle. Metabolism. 1988;37:802–806.
18. Tamashiro KL, et al, Chronic stress, metabolism and metabolic syndrome. Stress. 2011;14:468–474
19. van Raalte DH, et al, 2009 Novel insights into glucocorticoid-mediated diabetogenic effects: towards expansion of therapeutic options? Eur J Clin Invest 39:81–93.
20. Wilcox G. Insulin and Insulin Resistance. Clin Biochem Rev. 2005 May; 26(2): 19–39.
21. Obesity Society. “Insulin sensitivity: One night of poor sleep could equal six months on a high-fat diet, study in dogs suggests.” ScienceDaily. ScienceDaily, 4 November 2015. .

The post 3 Ways to Regulate Insulin That Have Nothing to Do with Food appeared first on Mark's Daily Apple.



June 5, 2017
Dear Mark: Too Much Serotonin and Broccoli Sprouts
 For today’s edition of Dear Mark, I’m answering two questions from readers. The first is more of a comment, but it brought up a few questions for me to address. Is “more serotonin” always a good thing? Is there such a thing as too much serotonin? And second, what’s the deal with broccoli sprouts? Are they good for us? Has the grungy hippy hawking sprouts next to your meat guy at the farmers market been right all along?
For today’s edition of Dear Mark, I’m answering two questions from readers. The first is more of a comment, but it brought up a few questions for me to address. Is “more serotonin” always a good thing? Is there such a thing as too much serotonin? And second, what’s the deal with broccoli sprouts? Are they good for us? Has the grungy hippy hawking sprouts next to your meat guy at the farmers market been right all along?
Let’s go:
All good tips everyone should follow and a good reminder, thanks Mark BUT … it’s not always about trying to load up on serotonin nor is it necessarily safe to do so in excess, it’s also about your ability to USE what serotonin is there, it needs to be transported to the appropriate receptors. I’ve discovered this the hard way over the years. I’m in my 60’s and only take one pharmaceutical, an SSRI, and I no longer beat myself up about needing a reuptake inhibitor to literally help stay sane (I would not wish the panic attacks I get otherwise on my worst enemy).
I agree. More serotonin isn’t necessarily “better” and can even be counterproductive. For instance, one important function of serotonin is to increase “social awareness.” Adequate serotonin allows us to gauge the room. It increases empathy, helping us place ourselves in another’s shoes—a necessary skill for reading a situation. It helps us decide whether caution is warranted.
Yet, too much serotonin can backfire. A recent study found that brains of subjects with social anxiety disorder made more serotonin and transported it more efficiently than control brains. More specifically, the anxious patients’ amygdalae—the section of the brain associated with the fear and anxiety response—were awash in serotonin.
That’s one reason why I didn’t discuss taking 5-HTP supplements to increase serotonin in the brain: It works too well. Your brain has a theoretically limitless capacity to convert 5-HTP to serotonin. More 5-HTP crossing the blood-brain barrier (which it does), more serotonin production in the brain. If there’s 5-HTP available, you’ll make serotonin.
Sounds good at first glance, yet 5-HTP supplementation consistently fails to beat placebo in randomized controlled trials of depression. Sometimes it even worsens depression and other conditions by depleting dopamine and norepinephrine. All those neurotransmitters play important roles, too. To isolate and obsess over a single one misses the boat. Besides, we have a reliable way to increase serotonin production on demand—and it doesn’t really help the conditions “high serotonin” is supposed to address.
That’s why it’s important to disabuse the whole notion that there are good and bad neurotransmitters (or hormones, or cholesterol, or…). We’re finally starting to understand that our bodies aren’t producing things like LDL to clog our arteries or insulin to make us fat. Everything our body makes has a purpose. We must also understand that it goes the other way, too: endogenous production of neurotransmitters, hormones, and other compounds has an upper limit. More isn’t always better or safe.
Luckily, it’s unlikely that you’ll overdo serotonin following the guidelines I laid out in the post, because those guidelines promote natural production and regulation of serotonin.
Thanks for the comment.
Hi Mark,
What are your thoughts on sprouts? Not sprouted grains, nuts, beans, etc, but instead stuff like broccoli sprouts? Healthy, neutral, bad?
Thanks. I love broccoli sprouts and don’t want to give them up.
I’m a big fan of sprouts. Well, I’ll rephrase: they interest me greatly. They aren’t a regular part of my diet, but in the last few months I’ve been stumbling across information that makes me think they should be.
Luckily for you, broccoli sprouts show the most promise, particularly against oxidative stress. They are the single best source of the powerful phytonutrient sulforaphane or its precursor which converts to sulforaphane, having about 10x more than the next richest source, broccoli. What can sulforaphane-rich broccoli sprouts do for people?
They can reduce oxidative stress markers and improve liver function in people with liver abnormalities.
They increase the body’s detoxification of airborne pollutants.
They reduce the nasal allergic response to diesel exhaust particulates.
They reduce oxidized LDL and improve other heart health markers in type 2 diabetics.
They reduce inflammation in smokers exposed to infuenza virus, possibly by decreasing the amount of virus residing in the nose.
They reduce symptoms in autistic teens and adults, improving social interaction and verbal communication in about half the the people tested. That’s really, really cool.
More generally, the sulforaphane in broccoli sprouts activate detoxification and antioxidant pathways in the body. In other words, sulforaphane is a hormetic stressor—a plant toxin that elicits a protective, beneficial response in the organism.
It’s not a panacea, of course. In asthmatics, broccoli sprouts failed to reduce oxidative stress or improve lung function despite drastically boosting sulforaphane levels. And as a hormetic stressor, there’s probably an upper limit to the amount of sulforaphane we eat and frequency with which we eat it.
But broccoli sprouts are clearly helpful and powerful, and people have caught on and are figuring out ridiculous ways to eat them, like eating bread made out of broccoli sprouts. I’m sure that’s great and all, but why not have a salad or a smoothie? This preserves the sulforaphane, whereas heating degrades it.
If you want to get started with broccoli sprouts, you have a few options:
The aforementioned grungy hippy at the farmer’s market. Nice way to start and see if you even like broccoli sprouts, but $3-5 a pop will add up if you start consuming Rhonda Patrick-esque levels of sprouts.
Sprout your own. It’s apparently a simple process. Buy some seeds, get some jars, find a warm windowsill, and you’re good.
Get some broccoli sprout extract or powder. Many of the studies use supplements, so they should work.
I think I’ll give these a shot myself.
That’s it for today, folks. Thanks for reading!
I’d love to hear about your experiences with serotonin and/or broccoli sprouts?
Take care, all.
The post Dear Mark: Too Much Serotonin and Broccoli Sprouts appeared first on Mark's Daily Apple.



Don’t Forget—The Staff 21-Day Challenge Starts TODAY
 Before I delve into Dear Mark questions today, I want to put out the reminder that the June 21-Day Staff Challenge begins TODAY! The community board on Vimify is already hopping this morning as folks share their goals in the Challenge and what they’re doing today toward those intentions.
Before I delve into Dear Mark questions today, I want to put out the reminder that the June 21-Day Staff Challenge begins TODAY! The community board on Vimify is already hopping this morning as folks share their goals in the Challenge and what they’re doing today toward those intentions.
As I mentioned in last week’s Summer Reset post, this Challenge is all about getting a foothold on the summer you want. It’s about living the good life at its finest and healthiest.
And there’s no need to go it alone! Join several members of the Mark’s Daily Apple, Primal Blueprint, and Primal Kitchen staff as they kick off our first ever staff-led 21-Day Primal Blueprint Challenge reset.
Follow along on the Vimify app (accessible from your desktop computer or iOS-compatible device – iPhone or iPad) for Challenge prompts and progress, and see more of the staff’s tips, recipes, and stories on the PRIMAL KITCHEN®, Primal Blueprint and Mark’s Daily Apple Instagram pages.
It’s not to late to sign up! Get set for next week with these preparation ideas. And for more guidance and tools, check out the 21-Day Transformation Challenge Packages—for the ultimate in reset support.
And congratulations to Sara Rainey, the winner of last week’s Summer Reset giveaway (and 21-Day Challenge participant)!
Have a great Challenge (and great week), everybody!
The post Don’t Forget—The Staff 21-Day Challenge Starts TODAY appeared first on Mark's Daily Apple.



June 4, 2017
Weekend Link Love – Edition 455
 RESEARCH OF THE WEEK
RESEARCH OF THE WEEKCoffee boosts your workout, even if you drink the stuff all the time.
Farming selected for genetic variants that increase conversion of plant fats into long-chained fats.
New mummy data reveals that ancient Egyptian genetics were more closely related to Middle Eastern and European populations than Central African ones.
Sherpas possess genetic adaptations that increase energy generation in low-oxygen environments.
Giving violent and aggressive boys a multi-micronutrient supplement makes them less violent and aggressive.
In adults with IBS and depression or anxiety, a probiotic may reduce symptoms.
Your brain is protecting you from sick people before “you” are “aware” they’re even sick.
NEW PRIMAL BLUEPRINT PODCASTS
Episode 171: Genevieve Howland: Host Elle Russ chats with Genevieve Howland about natural pregnancy, childbirth, and parenting.
Each week, select Mark’s Daily Apple blog posts are prepared as Primal Blueprint Podcasts. Need to catch up on reading, but don’t have the time? Prefer to listen to articles while on the go? Check out the new blog post podcasts below, and subscribe to the Primal Blueprint Podcast here so you never miss an episode.
Interesting Blog Posts
Food: more than just nutrients.
To attract women, men should eat lots of garlic and enough carrots to turn their skin yellow.
The fascinating history of the banana babies.
MEDIA, SCHMEDIA
India is getting wealthier and more diabetic.
Overworked doctors can’t keep up with the literature, so it’s up to you.
EVERYTHING ELSE
Fred Kummerow, one of the first researchers to question the sanity of filling our diets with artificial trans-fats (and a major butter lover/vegetable oil hater), just passed away at the ripe old age of 102.
OJ consumption is down, and it’s hurting Brazilian orange farmers.
Millennials aren’t eating at chain restaurants, and it’s hurting Applebee’s.
Meet Iron Grandpa.
Cows have been eating Skittles.
Seafood, now with microplastics.
A new milk-sharing app helps British mothers exchange breastmilk.
I hear Google’s interview process culminates in a 20-rep set of front squats at bodyweight.
THINGS I’M UP TO AND INTERESTED IN
Concept I’m pondering: The stress-reducing effects of fractals.
I’m somehow not surprised: CRISPR likely causes hundreds of unintended mutations.
Article I’m loving: How Adrian Ballinger Summited Everest Without Oxygen.
Japanese news I enjoyed: They need more ninjas.
I’ve always said this: Wasp nests don’t belong in vaginas.
RECIPE CORNER
Cherries, jicama, and mac nuts in a salad? Yep.
Sour cherry elk meatballs. No elk? Go with beef or lamb.
TIME CAPSULE
One year ago (June 4– June 10)
14 Ways to Help You Look Primal – How to improve vision.
Why the Kind of Body Fat You Carry Matters – What does your body fat distribution say about your health?
COMMENT OF THE WEEK
“They’re the only place I can find chicken hearts.”
– Not exactly sure why, but this comment from bill really hit home.

The post Weekend Link Love – Edition 455 appeared first on Mark's Daily Apple.



June 3, 2017
Primal Keto Ice Cream
 This is the keto ice cream you’ve been waiting for. It’s creamy, rich and luscious, and made with just 5 ingredients. Primal keto ice cream is pure, unadulterated, guilt-free bliss. There’s no dairy, no added sugar or artificial sweeteners, and no additives.
This is the keto ice cream you’ve been waiting for. It’s creamy, rich and luscious, and made with just 5 ingredients. Primal keto ice cream is pure, unadulterated, guilt-free bliss. There’s no dairy, no added sugar or artificial sweeteners, and no additives.
It’s almost impossible to make rich and creamy dairy-free ice cream without dumping sugar or additives into it. Here’s the secret: High-fat coconut milk and macadamia butter, pure vanilla extract, and PRIMAL KITCHEN® Collagen Fuel. This combination is all you need to make delicious dairy-free, high-fat, low-carb, low sugar, keto ice cream.
High-fat, low-carb foods are critical to the ketogenic diet, and this ice cream delivers on both fronts. Plus, you get collagen protein from the PRIMAL KITCHEN® Collagen Fuel. Even so, a daily bowl of Primal keto ice cream probably isn’t the best idea. It’s still dessert, after all. But when you need a treat, this ice cream is where it’s at. Primal keto ice cream is just sweet enough to gratify a sweet tooth, and the rich, full-fat flavor is truly satisfying, even in small servings.
The two recipes below make both vanilla and chocolate Primal keto ice cream. They’re delicious separately, or swirled together.
Time in the Kitchen: 10 minutes, plus time to churn in the ice cream maker
Servings: 4 to 6

Vanilla Coconut Collagen Fuel Keto Ice Cream
Ingredients
1 13.5 ounce can full-fat coconut milk (400 ml)
1 scoop PRIMAL KITCHEN® Vanilla Coconut Collagen Fuel (16.5 g)
¼ cup macadamia nut butter* (60 ml)
2 teaspoons pure vanilla extract (without propylene glycol) (10 ml)
pinch of salt

Chocolate Coconut Collagen Fuel Keto Ice Cream
Ingredients
1 13.5 ounce can full-fat coconut milk (400 ml)
1 scoop PRIMAL KITCHEN® Chocolate Coconut Collagen Fuel (16.5 g)
¼ cup macadamia butter* (60 ml)
2 teaspoons pure vanilla extract (without propylene glycol) (10 ml)
3 tablespoons unsweetened cocoa powder (45 ml)
pinch of salt

Instructions
Recipe Note:
Like all low sugar, additive-free, dairy-free ice creams, this one has the creamiest and fluffiest texture straight out of the ice cream maker. Once it’s frozen, the ice cream will harden. Before eating, let it sit out for 10-20 minutes to soften. The ice cream will return to a creamy texture, but won’t be as airy and fluffy. Running it briefly through a food processor, however, will restore the original consistency.
.
*To make macadamia butter, blend 1 cup raw, unsalted macadamia nuts in the food processor for 3 to 5 minutes until very smooth.
To make the ice cream, whisk coconut milk, PRIMAL KITCHEN® Collagen Fuel, macadamia butter, vanilla, and salt together until smooth. If making chocolate ice cream, whisk in cocoa powder.
Follow ice cream maker instructions for churning. Pour the mixture into the bowl of your ice cream maker and churn until desired consistency is reached.

The post Primal Keto Ice Cream appeared first on Mark's Daily Apple.



June 2, 2017
We’ve Experienced the Best Results When We Follow the Primal Blueprint Recommendations
It’s Friday, everyone! And that means another Primal Blueprint Real Life Story from a Mark’s Daily Apple reader. If you have your own success story and would like to share it with me and the Mark’s Daily Apple community please contact me here. I’ll continue to publish these each Friday as long as they keep coming in. Thank you for reading!
It is now nearly four years ago that our initial story was shared on MDA. Over that time, we have experimented a lot with our diet and lifestyle to see what type of diet-exercise regimen best suits our bodies. To make a long story short, we have experienced the best results when we follow the Primal Blueprint recommendations. The path that MDA set us on many years ago has been hugely beneficial to us and our family and we are very grateful for that.
In the past years, our family has grown and we are now the proud parents of four children. This obviously puts a lot of pressure on our time, but one of the biggest benefits we feel we get from eating clean and staying active is that we can manage the emotional and physical rollercoasters of having children whilst working full-time well.
Around the time when our story was published I started getting into CrossFit, which felt like a very natural progression for me coming from a Primal Blueprint prescribed way of working out. As part of being immersed in the CrossFit world, however, there is a different set of diet recommendations that one is subjected to. It seems that a more relaxed diet approach, e.g. regular oatmeal breakfasts and more grain-based meals are ok. I did shift my approach to eating towards that and although I experienced strength gains along the way, I ended up not being happy about how my body reacted to the change in diet.
 I have now for the past year been working my way back to following the Primal Blueprint style of eating and have hugely benefitted from it. I am still getting stronger and faster all the time, but my body has shifted to a more fat-burning machine again, which is a big visual change compared to a year ago.
I have now for the past year been working my way back to following the Primal Blueprint style of eating and have hugely benefitted from it. I am still getting stronger and faster all the time, but my body has shifted to a more fat-burning machine again, which is a big visual change compared to a year ago.
My wife has obviously pushed her body a lot in terms of having had four children in the span of six years. The challenges for her were down to not wanting certain foods during her pregnancies, like eggs or meat at times. Also, there are different needs for a mum who is breastfeeding her babies, for example, intermittent fasting was not an option her. However, I am most amazed by how fast her body has always recovered, including her losing her baby weight in-between pregnancies. This has been due to her developing a passion to source and create primal meals for her family as well as developing a regular and fun exercise regimen.
Having gone primal has been amazing for our family and we love providing healthy meals for our children, who love their vegetables for lunch every day. My wife and I are both certified CrossFit adult and kids’ trainers and we love taking our children along this journey of healthy eating and staying active. Through being primal, we have managed to achieve a lot in the past years, including me completing the SealFit Kokoro camp a year ago and my wife and I are now enrolled on the Primal Health Coach course. Thanks to Marc and this amazing community of primal/paleo folks.
Tobias & Harriet Emonts-Holley
The post We’ve Experienced the Best Results When We Follow the Primal Blueprint Recommendations appeared first on Mark's Daily Apple.



Join Me with Tony Horton TODAY on Facebook Live
 Mark your calendars, folks, because this is an event I hope you can join me for! Together with my longtime friend and health and fitness powerhouse, Tony Horton, I’ll be hosting a Facebook Live TODAY at 11:00 a.m. PDT, on the Mark’s Daily Apple Facebook page.
Mark your calendars, folks, because this is an event I hope you can join me for! Together with my longtime friend and health and fitness powerhouse, Tony Horton, I’ll be hosting a Facebook Live TODAY at 11:00 a.m. PDT, on the Mark’s Daily Apple Facebook page.Join us as we discuss our beginnings as struggling personal trainers nearly 30 years ago and how life has evolved since. After that, I’ll dive into the newest addition to my cookbook series, The Primal Kitchen Cookbook, chock full of amazing contributors including Mr. P90X himself! And make sure to stay tuned through the end as we’ll be picking THREE winners to receive an exclusive pre-launch copy signed on air by myself and Tony!

The post Join Me with Tony Horton TODAY on Facebook Live appeared first on Mark's Daily Apple.



Mark Sisson's Blog
- Mark Sisson's profile
- 199 followers