Michael Greger's Blog, page 5
July 3, 2025
Does Black Cumin Seed (Nigella Sativa) Help with Weight Loss?
For three cents a day, black cumin may improve our cholesterol and triglyceride levels, blood pressure, and blood sugar control, as well as accelerate the loss of body fat.
Black cumin, also known as Nigella sativa or simply “black seed,” is not related to cumin; it’s a member of the buttercup family rather than the carrot family. Black cumin, with its peppery flavor, is a spice commonly used in Indian and Middle Eastern cuisines, but it’s also been prized for its purported medicinal benefits. Described as “a miracle herb,” with mentions going back to the Old Testament, it was found cached in King Tut’s tomb, and it’s been reported that the “Islamic prophet Muhammad once stated that the black seed can heal every disease except death.” Only in the last 50 years or so has it been put to the test, though, culminating in more than a thousand papers published in the medical literature.
Typical doses used in studies are one or two grams a day, which is only about a quarter teaspoon. This enables researchers to perform randomized, double-blind, placebo-controlled trials by putting the whole-food spice powder into capsules rather than studying a component or extract.
A systematic review and meta-analysis of randomized, placebo-controlled trials found that daily black cumin consumption significantly improves cholesterol and triglycerides. Researchers also found that it not only improves blood pressure, but it also improves blood sugar control. Some of the results are quite extraordinary. For example, one study found that postmenopausal women randomized to a gram a day (less than a quarter teaspoon) of black cumin powder reduced their LDL cholesterol by 27 percent within two months, significantly better than placebo. Those are the kinds of results we’d expect from a statin drug, yet it was achieved with just a sprinkle’s worth of a simple spice. Black cumin may also help with menopausal symptoms.
Now, it doesn’t appear to cure anything—a month after stopping the spice, cholesterol levels began to creep back up, for instance, as you can see below and at 2:00 in my video Benefits of Black Cumin Seed (Nigella Sativa) for Weight Loss—but it does appear to be a cheap, safe, effective, and delicious (if you like spice) treatment for some of our deadliest risk factors. And its side effects include loss of appetite and weight loss!

The latest systematic review and meta-analysis of randomized controlled weight-loss trials found that about a quarter teaspoon of black cumin powder a day does appear to cause weight loss within a span of a few months. If it really can benefit so many facets of health, why don’t we hear more about it? Why wasn’t I taught about it in medical school? Maybe because there’s little profit motive. Black cumin is just a common, natural spice. The daily dose used in most of these studies would cost about three cents a day. Stockholders won’t be thrilled to sell something that can’t be patented and costs only three pennies a day. Black cumin has become a staple in my family’s daily diet. I keep a pepper mill filled with it right on the kitchen table and grind it onto foods just as I would black pepper—easy and delicious.
July 1, 2025
Should We Drink Kombucha
What are the risks versus benefits of drinking kombucha?
Is Kombucha Tea Good for You? is one of my first videos. It was featured in a blog entry entitled “NutritionFacts.org: the first month,” where I marveled the video had reached nearly 100,000 people. You can see it below and at 0:20 in my video Kombucha’s Side Effects: Is It Bad for You?. I’m honored to say that we now reach more than 100,000 people a day.

In that first kombucha video, I profiled a report published in the Journal of Intensive Care Medicine of “a case of kombucha tea toxicity” in which a young man ended up in an acidotic coma. The authors concluded, “While Kombucha tea is considered a healthy elixir, the limited evidence currently available raises considerable concern that it may pose serious health risks. Consumption of this tea should be discouraged, as it may be associated with life-threatening lactic acidosis.” And this was just one of several case reports of “serious, and sometimes fatal, hepatic [liver] dysfunction and lactic acidosis within close proximity of ingestion.”
For example, there were two cases in Iowa of severe metabolic acidosis, including one death. There was also a triggering of a life-threatening autoimmune muscle disease that required emergency surgery and was “probably related to the consumption of a fermented Kombucha beverage.” Another patient presented with shortness of breath, shaking, and a movement disorder “after consumption of tea and no other medications,” and a middle-aged woman complained of xerostomia, dizziness, nausea, vomiting, headache, and neck pain,” and her symptoms recurred on reingestion of the tea. There was another case of severe metabolic lactic acidosis, as well as a case of hepatotoxicity (liver toxicity) that resolved after stopping kombucha.
Why these sporadic cases? Maybe some unusual toxins developed in a particular batch. I mean, it is a fermented product, so it’s possible there was just some contamination by a bad bug, like the time people smeared kombucha on their skin because they were told it had “magical healing power.” What it had instead was anthrax. So, even though such reports were rare, I concluded ten years ago that we should probably stick to foods that haven’t put people in a coma. But what about its risks versus benefits? Maybe kombucha is worth it. After all, it’s “reputed to cure cancer,” “eliminate wrinkles,” “and even restore gray hair to its original color”—as “marketed by alternative and naturopathic healers throughout the United States.”
“Currently, kombucha is alternately praised as ‘the ultimate health drink’ or damned as ‘unsafe medicinal tea.’” It’s been “claimed to be a universal wonderful drug…a potion which improves awareness and concentration, slimming, also purifying, regenerating and life extending.” Which is it? Is it “potion or poison?
Back in the 1920s, 1930s, and 1940s, there were several medical studies conducted by recognized physicians confirming all sorts of beneficial effects, as you can see below and at 2:55 in my video.
I couldn’t wait to read them. Dufrense and Farnworth were cited, and when I went to that paper, I saw the same claim, citing Allen 1998. When I went to that source, I saw the citation is for a random kombucha website, as shown below, and at 3:10 in my video. And guess what? That website’s been defunct since 2001, and “much of the Kombucha information” posted came from comments on some mailing list.

Finally, in 2003, a systematic review of the clinical evidence that had been published was conducted. “The main result of this systematic review, it seems, is the total lack of efficacy data…No clinical studies were found relating to the efficacy of this remedy.” We just have these cautionary tales, these case reports. So, based on these data, it was concluded that the largely undetermined benefits do not outweigh the documented risks of kombucha. It can therefore not be recommended for therapeutic use.” That was back in 2003, though. How about a 2019 systematic review of the empirical evidence of human health benefit?
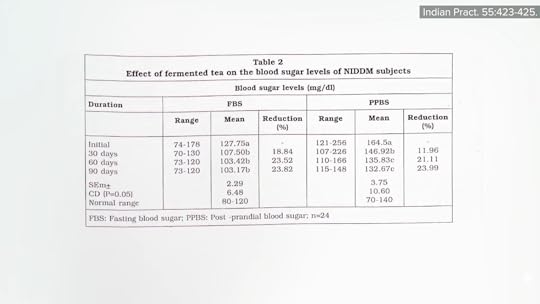
“The nonhuman subjects literature claims numerous health benefits of kombucha,” with “nonhuman” meaning mice and rats. We need human clinical trials, yet there is still not a single controlled human study. (I did find one uncontrolled study purporting to show a significant reduction in fasting and after-meal blood sugars among individuals with type 2 diabetes, though, as seen below and at 4:19 in my video.)
“Nonetheless,” despite no controlled trials, “significant commercial shelf space is now dedicated to kombucha products, and there is widespread belief that the products promote health.” So, we are left with this extreme disparity between science and belief: “There is no convincingly positive clinical evidence at all; the [health] claims for it are as far-reaching as they are implausible; the potential for harm seems considerable. In such extreme cases, healthcare professionals should discourage consumers from using (and paying for) remedies that only seem to benefit those who sell them.”
Doctor’s Note:
Friday Favorites: What Are the Best Beverages? Watch the video to find out.
June 26, 2025
Treating Hashimoto’s Disease (Hypothyroidism) Naturally with Diet
What were the results of a randomized, double-blind, placebo-controlled trial of a daily half teaspoon of powdered black cumin in Hashimoto’s patients?
“Autoimmune thyroiditis, also known as Hashimoto’s thyroiditis, is an organ-specific autoimmune disorder,” where our body attacks our own thyroid gland, often leading to hypothyroidism due to destruction and scarring of the gland itself. We know there’s a genetic component, since identical twins are more likely to share the disease than fraternal twins. “However, even with identical twins, the concordance rate was only about 50%, emphasizing that important factors such as the environment play a role in disease pathogenesis.” Indeed, even if your identical twin, who has basically your exact same DNA, has the disease, there’s only like a flip of a coin’s chance you’ll get it. Genes load the gun, but the environment may pull the trigger.
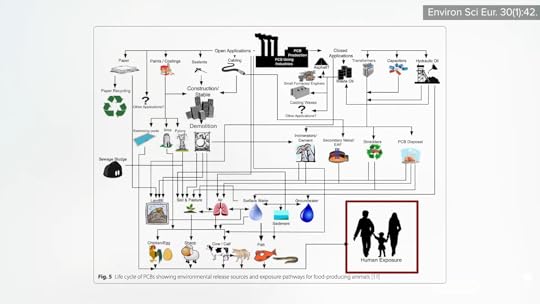
More than 90 synthetic chemicals were noted to show disruption of hormonal balance or thyroid dysfunction.” However, only a few such ‘pollutants show evidence that they contribute to autoimmune thyroid disease.” These include polyaromatic hydrocarbons. Smokers get a lot of them from cigarettes, but in nonsmokers, exposure comes almost entirely from food, as you can see below and at 1:18 in my video Diet for Hypothyroidism: A Natural Treatment for Hashimoto’s Disease.

Polycyclic aromatic hydrocarbons are primarily formed when muscle meats, such as beef, pork, fish, or chicken, are cooked using high-temperature methods, such as grilling. PBBs, polybrominated biphenols, are a type of flame-retardant chemical no longer manufactured in the United States, but are still found in the aquatic food chain. PCBs, polychlorinated biphenols, are used in a number of industrial processes and end up in people’s bodies, again, largely through the consumption of fish, but also eggs and other meats, as seen here and at 1:41 in my video.
So, one might suspect those eating plant-based diets would have lower rates of hypothyroidism, and, indeed, despite their lower iodine intake, vegan diets tended to be protective. But they’ve never been put to the test in an interventional trial. A modification of the Paleolithic diet has been tried in Hashimoto’s patients, but it didn’t appear to improve thyroid function. What did, though, is Nigella Sativa. That name should sound familiar to anyone who’s read my book How Not to Diet or watched my live Evidence-Based Weight Loss presentation. Nigella Sativa is the scientific name for black cumin, which is just a simple spice that’s also used for a variety of medicinal purposes.
In one study, Hashimoto’s patients received a half teaspoon of powdered black cumin every day for eight weeks in a randomized, double-blind, placebo-controlled trial. Not only was there a significant reduction in body weight, which is why I profiled it in my book, but the black cumin also significantly reduced the thyroid-stimulating hormone, a sign that thyroid function was improving. It even lowered the level of autoimmune anti-thyroid antibodies, as well as increased blood levels of thyroid hormone T3 in these Hashimoto’s patients. In addition, there was a significant drop in Interleukin 23, a proinflammatory cell signal thought to help promote the autoimmune inflammation of the thyroid, which “further confirms the anti-inflammatory nature of the plant.” And what were the side effects? There was a 17 percent drop in “bad” LDL cholesterol, as shown below and at 3:19 in my video.
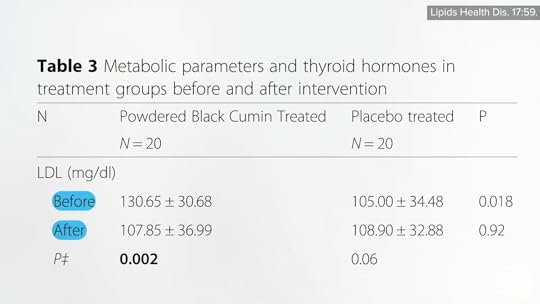
Given the fact that patients with Hashimoto’s may be at particularly high risk of developing heart disease, this is exactly the kind of side effects we’d want. “Considering these health-promoting effects of N. Sativa [black cumin], it can be considered as a therapeutic approach in the management of Hashimoto-related metabolic abnormalities.”
A similar trial failed to find a benefit, though. Same dose, same time frame, but no significant changes in thyroid function. In contrast with the previous study, though, the study participants were not all Hashimoto’s patients, but rather hypothyroid for any reason, and that may have diluted the results. And it’s possible that telling patients to take the black cumin doses with their thyroid hormone replacement therapy may have interfered with its absorption, which is an issue similar to other foods and drugs, and why patients are normally told to take it on an empty stomach. Since there are no downsides—it’s just a simple spice—I figure, why not give it a try? The worst that can happen is you’ll have tastier food.
Doctor’s Note:
I get a lot of questions about thyroid function, and I am glad to have been able to do this series. If you missed any of the other videos, see the related posts below.
For more on black cumin, see my book How Not to Diet and my presentation Evidence-Based Weight Loss.
June 24, 2025
Eating with Hypothyroidism and Hyperthyroidism
Is the apparent protection of plant-based diets for thyroid health due to the exclusion of animal foods, the benefits of plant foods, or both?
Several autoimmune diseases affect the thyroid gland, and Graves’ disease and Hashimoto’s thyroiditis are the most common. Graves’ disease results in hyperthyroidism, an overactive thyroid gland. Though slaughter plants are supposed to remove animals’ thyroid glands as they “shall not be used for human food,” should some neck meat slip in, you can suffer a similar syndrome called Hamburger thyrotoxicosis. That isn’t from your body making too much thyroid hormone, though. Rather, it’s from your body eating too much thyroid hormone. Graves’ disease is much more common, and meat-free diets may be able to help with both diseases, as plant-based diets may be associated with a low prevalence of autoimmune disease in general, as observed, for example, in rural sub-Saharan Africa. Maybe it’s because plants are packed with “high amounts of antioxidants, possible protective factors against autoimmune disease,” or because they’re packed with anti-inflammatory compounds. After all, “consuming whole, plant-based foods is synonymous with an anti-inflammatory diet.” But you don’t know until you put it to the test.
It turns out that the “exclusion of all animal foods was associated with half the prevalence of hyperthyroidism compared with omnivorous diets. Lacto-ovo [dairy-and-egg] and pesco [fish] vegetarian diets were associated with intermediate protection.” But, for those eating strictly plant-based, there is a 52 percent lower odds of hyperthyroidism.
As I discuss in my video The Best Diet for Hypothyroidism and Hyperthyroidism, this apparent protection “may be due to the exclusion of animal foods, the [beneficial] effects of plant foods, or both. Animal foods like meat, eggs, and dairy products may contain high oestrogen concentrations, which have been linked to autoimmunity in cell and animal studies.” Or it could be because the decrease in animal protein by excluding animal foods may downregulate IGF-1, which is not just a cancer-promoting growth hormone, but may play a role in autoimmune diseases. The protection could also come from the goodness in plants that may “protect cells against autoimmune processes,” like the polyphenol phytochemicals, such as flavonoids found in plant foods. Maybe it’s because environmental toxins build up in the food chain. For example, fish contaminated with industrial pollutants, like PCBs, are associated with an increased frequency of thyroid disorders.
But what about the other autoimmune thyroid disease, Hashimoto’s thyroiditis, which, assuming you’re getting enough iodine, is the primary cause of hypothyroidism, an underactive thyroid gland? Graves’ disease wasn’t the only autoimmune disorder that was rare or virtually unknown among those living in rural sub-Saharan Africa, eating near-vegan diets. They also appeared to have less Hashimoto’s.
There is evidence that those with Hashimoto’s have compromised antioxidant status, but we don’t know if it’s cause or effect. But if you look at the dietary factors associated with blood levels of autoimmune anti-thyroid antibodies, animal fats seem to be associated with higher levels, whereas vegetables and other plant foods are associated with lower levels. So, again, anti-inflammatory diets may be useful. It’s no surprise, as Hashimoto’s is an inflammatory disease—that’s what thyroiditis means: inflammation of the thyroid gland.
Another possibility is the reduction in intake of methionine, an amino acid concentrated in animal protein, thought to be one reason why “regular consumption of whole-food vegan diets is likely to have a favourable influence on longevity through decreasing the risk of cancer, coronary [heart] disease, and diabetes.” Methionine restriction improves thyroid function in mice, but it has yet to be put to the test for Hashimoto’s in humans.
If you compare the poop of patients with Hashimoto’s to controls, the condition appears to be related to a clear reduction in the concentration of Prevotella species. Prevotella are good fiber-eating bugs known to enhance anti-inflammatory activities. Decreased Prevotella levels are also something you see in other autoimmune conditions, such as multiple sclerosis and type 1 diabetes. How do you get more Prevotella? Eat more plants. If a vegetarian goes on a diet of meat, eggs, and dairy, within as few as four days, their levels can drop. So, one would expect those eating plant-based diets to have less Hashimoto’s, but in a previous video, I expressed concern about insufficient iodine intake, which could also lead to hypothyroidism. So, which is it? Let’s find out.
“In conclusion, a vegan diet tended to be associated with lower, not higher, risk of hypothyroid disease.” Why “tended”? The associated protection against hypothyroidism incidence and prevalence studies did not reach statistical significance. It wasn’t just because they were slimmer either. The lower risk existed even after controlling for body weight. So, researchers think it might be because animal products may induce inflammation. The question I have is: If someone who already has Hashimoto’s, what happens if they change their diet? That’s exactly what I’ll explore next.
This is the third in a four-video series on thyroid function. The first two were Are Vegans at Risk for Iodine Deficiency? and Friday Favorites: The Healthiest Natural Source of Iodine.
Stay tuned for the final video: Diet for Hypothyroidism: A Natural Treatment for Hashimoto’s Disease.
June 19, 2025
A Healthy, Natural Source of Iodine?
How much nori, dulse, or arame approximates the recommended daily allowance for iodine?
Dairy milk supplies between a quarter and a half of the daily iodine requirement in the United States, though milk itself has “little native iodine.” The iodine content in cow’s milk is mainly determined by factors like “the application of iodine-containing teat disinfectants,” and the “iodine residues in milk originate mainly from the contamination of the teat surface…” Indeed, the teats of dairy cows are typically sprayed or dipped with betadine-type disinfectants, and the iodine just kind of leaches into their milk, as you can see at 0:35 in my video Friday Favorites: The Healthiest Natural Source of Iodine.

Too bad most of the plant-based milks on the market aren’t enriched with iodine, too. Fortified soy milk is probably the healthiest of the plant milks, but even if it were enriched with iodine, what about the effects soy may have on thyroid function? When I searched the medical literature on soy and thyroid, this study popped up: “A Cost-Effective, Easily Available Tofu Model for Training Residents in Ultrasound-Guided Fine Needle Thyroid Nodule Targeting Punctures”—an economical way to train residents to do thyroid biopsies by sticking the ultrasound probe right on top a block of tofu and get to business, as you can see below and at 1:10 in my video. It turns out that our thyroid gland looks a lot like tofu on ultrasound.

Anyway, “the idea that soya may influence thyroid function originated over eight decades ago when marked thyroid enlargement was seen in rats fed raw soybeans.” (People living in Asian countries have consumed soy foods for centuries, though, “with no perceptible thyrotoxic effects,” which certainly suggests their safety.) The bottom line is that there does not seem to be a problem for people who have normal thyroid function. However, soy foods may inhibit the oral absorption of Synthroid and other thyroid hormone replacement drugs, but so do all foods. That’s why we tell patients to take it on an empty stomach. But you also have to be getting enough iodine, so it may be particularly “important for soy food consumers to make sure their intake of iodine is adequate.”
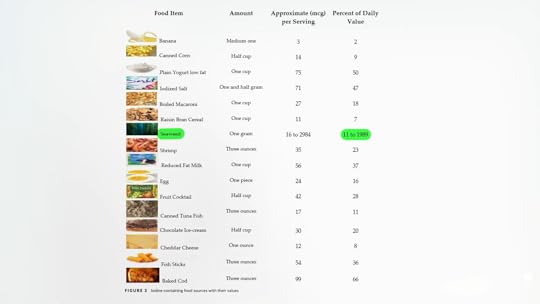
What’s the best way to get iodine? For those who use table salt, make sure it’s iodized. “Currently, only 53% of salt sold for use in homes contains iodine, and salt used in processed foods typically is not iodized.” Ideally, we shouldn’t add any salt at all, of course, since it is “a public health hazard.” A paper was titled: “Salt, the Neglected Silent Killer.” Think it’s a little over the top? Dietary salt is the number one dietary risk factor for death on planet Earth, wiping out more than three million people a year, twice as bad as not eating your vegetables, as you can see here and at 2:38 in my video.

In that case, what’s the best source of iodine then? Sea vegetables, as you can see below and at 2:50. We can get a little iodine here and there from a whole variety of foods, but the most concentrated source by far is seaweed. We can get up to nearly 2,000 percent of our daily allowance in just a single gram, about the weight of a paperclip.
“Given that iodine is extensively stored in the thyroid, it can safely be consumed intermittently,” meaning we don’t have to get it every day, “which makes seaweed use in a range of foods attractive and occasional seaweed intake enough to ensure iodine sufficiency.” However, some seaweed has overly high iodine content, like kelp, and should be used with caution. Too much iodine can cause hyperthyroidism, a hyperactive thyroid gland. A woman presented with a racing heartbeat, insomnia, anxiety, and weight loss, thanks to taking just two tablets containing kelp a day.
In my last video, I noted how the average urinary iodine level of vegans was less than the ideal levels, but there was one kelp-eating vegan with a urinary concentration over 9,000 mcg/liter. Adequate intake is when you’re peeing out 100 to 199 mcg/liter, and excessive iodine intake is when you break 300 mcg/liter. Clearly, 9,437 mcg/liter is way too much.
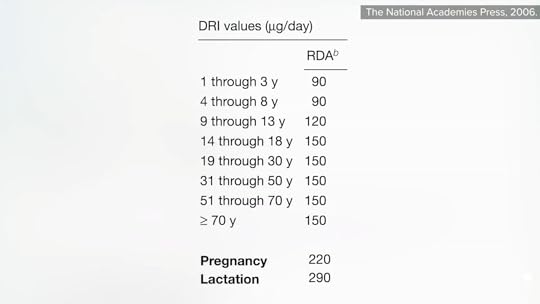
As you can see below and at 3:57 in my video, the recommended average daily intake is 150 mcg per day for non-pregnant, non-breastfeeding adults, and we may want to stay below 600 mcg a day on a day-to-day basis, but a tablespoon of kelp may contain about 2,000 mcg. So, I’d stay away from kelp because it has too much iodine, and I’d also stay away from hijiki because it contains too much arsenic.
This can give you an approximate daily allowance of iodine from some common seaweed preparations: two nori sheets, which you can just nibble on them as snacks like I do; one teaspoon of dulse flakes, which you can just sprinkle on anything; one teaspoon of dried arame, which is great to add to soups; or one tablespoon of seaweed salad.
If iodine is concentrated in marine foods, “this raises the question of how early hominins living in continental areas could have met their iodine requirements.” What do bonobos do? They’re perhaps our closest relatives. During swamp visits, they all forage for aquatic herbs.
Doctor’s Note:
This is the second in a four-video series on thyroid function. If you missed the previous one, check out Are Vegans at Risk for Iodine Deficiency?.
Coming up are The Best Diet for Hypothyroidism and Hyperthyroidism and Diet for Hypothyroidism: A Natural Treatment for Hashimoto’s Disease.
What else can seaweed do? See the related posts below.
June 17, 2025
Vegans and Iodine Deficiency Risk
Most plant-based milks are not fortified with iodine.
“Adequate dietary iodine is required for normal thyroid function.” In fact, the two thyroid hormones are named after how many iodine atoms they contain: T3 and T4. “Given that iodine is extensively stored in the thyroid gland itself, it can safely be consumed intermittently,” so we don’t need to consume it every day. However, our overall diet does need a good source of it. Unfortunately, the common sources aren’t particularly health-promoting: iodized salt and dairy foods. (Iodine-based cleansers like betadine are used on cows “to sanitize the udders, resulting in leaching of iodine in the milk.”) Iodine may also be added to cattle feed, and some commercially produced breads contain food additives with iodine.
If you put people on a paleo-type diet and cut out their dairy and table salt, they can develop an iodine deficiency, even though they double their intake of seafood, which can also be a source of iodine. What about those switching to diets centered around whole plant foods? They also cut down on ice cream and Wonder Bread, and if they aren’t eating anything from the sea, like seaweed or other sea vegetables, they can run into the same problem.
A three-year-old’s parents reported striving to feed her only the healthiest foods, and her diet included only plant-based, unsalted, and unseasoned foods. She got no unprocessed foods, but she also got no vitamin supplementation, which could be deadly. Without vitamin B12, those on strictly plant-based diets can develop irreversible nerve damage, but in this case, a goiter arose first, due to inadequate iodine intake.
In another case of “veganism as a cause of iodine-deficient hypothyroidism,” a toddler became ill after weaning. Before weaning, he was fine because his mother kept taking her prenatal vitamins, which fortunately contained iodine.
Most vegetarians and vegans are apparently unaware of the importance of iodine intake during pregnancy, “for the neurodevelopment of the unborn child, similar to their omnivorous counterparts.” The American Thyroid Association and the American Academy of Pediatrics have recommended that women, even just planning on getting pregnant, should take a daily supplement containing 150 micrograms (mcg) of iodine, yet only 60 percent of prenatal vitamins marketed in the United States contain this essential mineral. So, despite the recommendations, about 40 percent of prenatal vitamins don’t contain it. “Therefore, it is extremely important that women, especially when pregnant, breastfeeding, or planning a pregnancy, read the labels of their multivitamin supplements to ensure that they are receiving an adequate amount of iodine.”
Women of reproductive age have an average iodine level of 110 mcg/liter, which is fine for nonpregnant individuals, but we’d really like women to get at least 150 mcg/liter during pregnancy. (It’s basically a 24-hour urine test, in which iodine sufficiency is defined as 100 mcg/liter of urine in nonpregnant adults; the average vegan failed to reach this in the largest study done to date, one out of Boston.)
The recommended average daily intake is 150 mcg per day for most people, which we can get in about a cup and a half of cow’s milk. Regrettably, plant-based milks aren’t typically fortified with iodine and average only about 3 mcg per cup. Although many plant-based milks are fortified with calcium, researchers found in the largest systematic study to date that only 3 out of 47 were fortified with iodine. Those that were fortified had as much as cow’s milk, but those that weren’t fell short, as you can see at 3:30 in my video Are Vegans at Risk for Iodine Deficiency?.
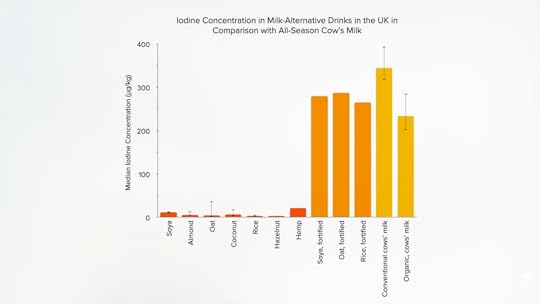
Plant-based milk companies brag about enriching their milks with calcium and often vitamins B12, D, and A, but only rarely are attempts made to match iodine content. The only reason cow’s milk has so much is that producers enrich the animals’ feed or it comes dripping off their udders. So, why don’t plant-milk companies add iodine, too? I was told by a food scientist at Silk that my carrageenan video played a role in the company switching to another thickener. Hopefully, Silk will see this video, too, and consider adding iodine, or maybe another company will snatch the opportunity for a market advantage.
The researchers conclude that individuals who consume plant-based milks not fortified with iodine may be at risk for iodine deficiency, unless they consume alternative dietary iodine sources, the healthiest of which are sea vegetables, which we’ll cover next.
Doctor’s Note:
This is the first in a four-video series on thyroid function. The next three are:
Friday Favorites: The Healthiest Natural Source of Iodine The Best Diet for Hypothyroidism and Hyperthyroidism Diet for Hypothyroidism: A Natural Treatment for Hashimoto’s DiseaseFor more on iodine, see the related posts below.
June 12, 2025
What About Elderberry, Echinacea, and Cranberries for Colds and the Flu?
How effective are flu shots, elderberries, echinacea, and cranberries?
The U.S. Centers for Disease Control and Prevention (CDC) recommends that everyone over the age of six months get a routine flu shot every year, unless you have some sort of contraindication, such as an allergy to any of the vaccine’s components. CDC recommends getting vaccinated by the end of October, but it may even be beneficial when received in December or later. How effective are flu vaccines? It depends on the year, but, as you can see below and at 0:33 in my video Friday Favorites: Elderberry Benefits and Side Effects: Does It Help with Colds and the Flu?, the flu vaccine typically reduces the risk of getting the flu by about 40 to 50 percent.

So, in healthy adults, we can say with moderate certainty that we can decrease our risk of influenza from about 2 percent each year down to just under 1 percent. Older adults may get a similar relative risk reduction, but the baseline risk is higher and the consequences greater, so the absolute benefits are greater, too. In kids, flu vaccines shine; there’s a high certainty of evidence of a substantial drop in risk. But even in this kind of best-case scenario, there’s still a risk with vaccination, so what else can we do?
In the United States alone, each year, Americans experience millions of cases of influenza and hundreds of millions of colds. What about elderberry supplements? In a test tube, elderberry extracts can inhibit pathogens, including the flu virus. In a petri dish, it can rev up the production of flu-fighting molecules from human immune system cells, like tumor necrosis factor, as much as nearly 45-fold. Elderberry juice can help mice fight off the flu. But what about actual people?
The first clinical trial was published back in the 1990s: a double-blind, randomized, placebo-controlled trial to treat flu-like symptoms. Researchers found that the odds for improvement before the fifth day in those in the treated group were more than 20 times the odds of the participants in the control group (p < 0.001). Two subsequent double-blind, randomized, placebo-controlled trials showed similar accelerated healing in the elderberry groups, as you can see here and at 1:54 in my video.
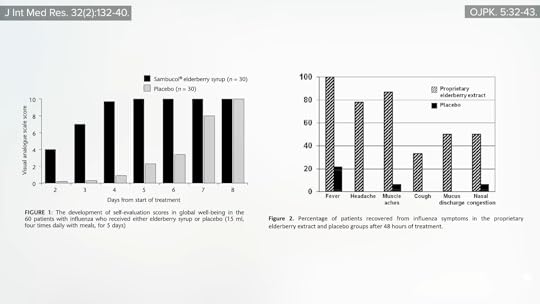
I was excited to see this study—“Elderberry Supplementation Reduces Cold Duration and Symptoms in Air-Travelers”—given a 200-city book tour I was embarking on. It was a randomized, double-blind, placebo-controlled clinical trial of 312 economy class passengers. While taking elderberry didn’t seem to prevent people from coming down with cold symptoms, the duration and severity of symptoms in those who did get a cold seemed to have been lessened, and they suffered an average of about five days instead of seven.
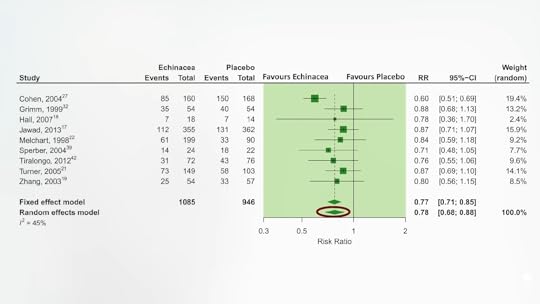
A similar study using the herb echinacea found a lessening of symptom scores, but it was of only borderline statistical significance. Nevertheless, even though most of the individual trials didn’t find statistically significant improvements, when all such studies were compiled, it seems there may be about a 20 percent decrease incidence of colds, as seen below and at 2:50 in my video.
Note, though, that there is a concern about publication bias and selective reporting. A number of findings and some entire studies seem to be MIA, suggesting that negative studies may have been quietly shelved. So, we aren’t really sure about echinacea, but all the elderberry studies seem to have positive results, suggesting elderberry supplementation “provides an effective treatment option when advanced or more invasive care [more serious treatment] is not warranted.” This conclusion came from someone with apparent conflicts of interest, though. In fact, each of the four elderberry studies was funded by the elderberry product companies themselves.
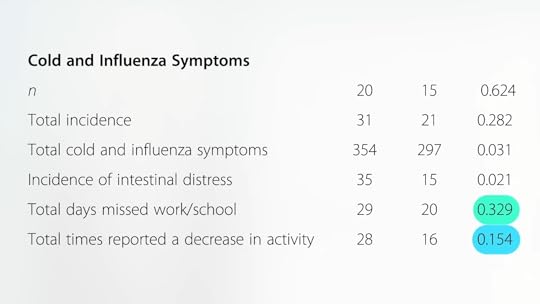
Any other berries that might be helpful? A randomized, placebo-controlled, interventional study—funded, predictably, by Ocean Spray—found that the gamma-delta-T-cells of those drinking a low-calorie cranberry juice beverage for ten weeks appeared to be proliferating at nearly fivefold the rate. These immune cells “serve as a first line of defense.” Though the study participants didn’t get fewer colds, they did seem to suffer less, but not enough to prevent days missed from work or an impairment of their activities, as shown here and at 3:56 in my video.
At least cranberries have never been reported to cause pancreatitis. A man taking an elderberry extract not only suffered an attack of acute pancreatitis, a sudden painful inflammation of the pancreas, but it went away when he stopped it, then reappeared again years later when he tried taking it again, which suggests cause-and-effect. Why take elderberry extracts when you can just eat the elderberries themselves? Well, cooked are fine, but “consuming uncooked blue or black elderberries can cause nausea and vomiting.”
I found out the hard way, as I explained in an answer to the question, “What was the worst day of your life?” in my London Real interview on my How Not to Die book tour. It turns out elderberry fruits form cyanide, such that eight people had to be medevacked out after someone brought freshly squeezed elderberry juice to a gathering.
Doctor’s Note:
Here’s the London Real interview I mentioned.
What else can we do for the common cold? See the related posts below.
And, speaking of cranberries, Can Cranberry Juice Treat Bladder Infections?. Watch the video to find out.
June 10, 2025
Skip the Salt and Shake on Potassium Chloride?
Worldwide, physical inactivity accounts for more than 10 million years of healthy life lost, but what we eat accounts for nearly 20 times that. As I discuss in my video Fewer Than 1 in 5,000 Meet Sodium and Potassium Recommended Intakes, unhealthy diets shave hundreds of millions of disability-free years off people’s lives every year. What are the worst aspects of our diets? Four out of the five of the deadliest dietary traps involve not eating enough of certain foods—not eating enough whole grains, fruits, nuts, seeds, and vegetables—but our most fatal flaw is getting too much salt. To put things into perspective, our overconsumption of salt is on the order of 15 times deadlier than diets too high in soda.
Our bodies are meant to have a certain balance of sodium and potassium intake, yet many people, including the majority in the United States, get vastly more sodium and far less potassium than the recommended amounts. Indeed, sodium and potassium goals are currently met by less than 0.015 percent of the U.S. population—close to 99.99 percent noncompliance, with only 1 in 6,000 Americans hitting the recommended guidelines.
What’s So Bad About Salt?
Of all the terrible things about our diets, high dietary sodium intake—that is, high salt intake—is the leading risk, estimated to be causing millions of deaths every year mainly through adverse effects on blood pressure and increased risks of stroke, heart attack, and kidney damage. Hypertension, known commonly as high blood pressure, is called the “silent and invisible killer” because it rarely causes symptoms but is one of the most powerful independent predictors of some of our leading causes of death. I discuss this in my video Are Potassium Chloride Salt Substitutes Effective?.
How Much Sodium Is Healthy in a Day?
Our bodies evolved to handle only about 750 milligrams of sodium a day. Nevertheless, the American Heart Association calls for us to stay under 1,500 milligrams, twice that amount. However, we’re consuming more than four times what’s natural, and it’s only getting worse, having increased over the last couple of decades. An eye-opening 98.8 percent of Americans exceed even that elevated 1,500 milligrams threshold.
Daily Potassium Intake
While many of us are consuming too much sodium, we may also be getting too little potassium, a mineral that lowers blood pressure. Less than 2 percent of U.S. adults, for instance, consume the recommended daily minimum intake of potassium based on chronic disease prevention. So, more than 98 percent of Americans may eat potassium-deficient diets.
This deficiency is even more striking when comparing our current intake with that of our ancestors, who consumed large amounts of dietary potassium. We evolved probably getting more than 10,000 milligrams of potassium a day. The recommendation was to get about half that amount, yet most of us don’t come anywhere close.

Why Are So Many of Us Lacking in Potassium?
We evolved consuming a diet very rich in potassium and low in sodium, but, today, this pattern has been reversed. The flip reflects a shift away from traditional plant-based diets high in potassium and low in sodium towards the standard American diet. I’m talking about a shift away from fruits, greens, roots, and tubers to an eating pattern filled with salty, processed foods stripped of potassium.
Why Do We Need Potassium?
Low potassium intake has been implicated in high blood pressure and cardiovascular disease, and several meta-analyses have confirmed that high potassium intake appears to reduce the risk of stroke. It follows that potassium is now considered a “nutrient of public health concern” because most Americans don’t reach the recommended minimum daily intake.
What Is the Best Substitute for Salt?
Potassium chloride, which is often found in zero-sodium salt substitutes. We know from randomized controlled trials that sodium reduction leads to blood pressure reduction and increasing potassium intake can also lower blood pressure. So should we be “salting” our food with potassium chloride instead of sodium chloride?
What Is Potassium Chloride? Is It a Viable (and Tasty) Salt Substitute?
Potassium chloride is a naturally occurring mineral salt, which is obtained the same way we get regular sodium salt. Since we get too much sodium and not enough potassium, this would seem to make potassium chloride a win-win solution. Consider these examples:
In a randomized controlled trial, households had just 25 percent of the sodium chloride salt replaced with potassium chloride. At that level, most people either can’t tell the difference or even prefer the salt with the potassium mixed in. The findings? The use of the salt substitute with one-quarter potassium chloride was associated with cutting the risk of developing hypertension in half.In another study , five kitchens in a veterans’ retirement home were randomized into two groups for about two and a half years. They either salted their meals with regular salt or, unbeknownst to the cooks and the diners alike, a 50/50 blend of potassium chloride. Those in the half-potassium group cut their risk of dying from cardiovascular disease by about 40 percent and lived up to nearly one year longer. The life expectancy difference at age 70 was equivalent to that which would have naturally occurred in 14 years––meaning that just switching to half potassium salt appeared to effectively make people more than a decade younger when it came to risk of death.Side Effects of Potassium Chloride?
As I discuss in my video Potassium Chloride Salt Substitute Side Effects, potassium chloride is “generally regarded as safe” by the U.S. Food and Drug Administration. Healthy individuals don’t have to worry about getting too much potassium because their kidneys excrete any excess in urine, but that’s with potassium in food. What about supplements? No adverse effects have been shown for long-term intakes of potassium supplements as high as 3,000 milligrams a day, and blood levels of potassium are maintained in the normal range by healthy kidneys, even when potassium intake is increased to approximately 15,000 milligrams a day. This isn’t surprising, given that we evolved eating so many healthy plant foods, so many fruits and vegetables, rich in potassium.
The normal range for potassium levels in the blood is between 3.5 and 5.0. There are a small number of individuals who may run into problems, primarily those with severely impaired kidney function. That’s why there’s been such a reluctance to push potassium‐based salt substitutes on a population level. Serious issues may arise if your kidneys can’t regulate your potassium. There may be concern if you have known kidney disease, diabetes (diabetes can lead to kidney damage), severe heart failure, or adrenal insufficiency, or if you’re an older adult or on medications that impair potassium excretion. If you aren’t sure if you’re at risk, ask your doctor about getting your kidney function tested.
Conclusion
National and international health organizations have called for warning labels on salt packets and salt shakers, with messages like “too much sodium in the diet causes high blood pressure and increases risk of stomach cancer, stroke, heart disease, and kidney disease. Limit your use.” So, pass (on) the salt shaker and try some potassium chloride instead.
June 5, 2025
Chemical Safety, Cultivated Meat, and Our Health
More than 95 percent of human exposure to industrial pollutants like dioxins and PCBs comes from fish, other meat, and dairy.
By cultivating muscle meat directly, without associated organs like intestines, the incidence of foodborne diseases “could be significantly reduced,” as could exposure to antibiotics, “pesticides, arsenic, dioxins, and hormones associated with conventional meat.” Currently, the U.S. Food and Drug Administration has approved seven hormone drugs to bulk up the production of milk and meat. “In the European Union, there exists a total ban on such use,” however. Even without injected hormones, though, animal products naturally have hormones because they come from animals. “Eggs, example given, contribute more to the dietary intake of estradiol [estrogens] than beef, whether the animal is legally treated with hormones or not.” After all, eggs come straight from a hen’s ovaries, so, of course, they’re swimming with hormones. But if you’re directly growing just muscle meat or egg white protein, you don’t need to include reproductive organs, adrenal glands, or any of the associated hormones.
“Chemical safety is another concern for meat produced under current production systems.” There are chemical toxicants and industrial pollutants that build up in the food chain, such as pesticides, PCBs, heavy metals, and flame retardants, but there is no food chain with cultivated meat. We could produce all the tuna we wanted, with zero mercury.
When the World Health Organization determined that processed meat was a known human carcinogen and unprocessed meat a probable human carcinogen, it wasn’t even talking about the carcinogenic environmental pollutants. When researchers tested retail meat for the presence of “33 chemicals with calculated carcinogenic potential,” like polycyclic aromatic hydrocarbons (PAHs), organochlorine pesticides like DDT, and dioxin-like PCBs, they concluded that, in order to reduce the risk of cancer, we should limit beef, pork, or chicken consumption to a maximum of five servings a month.
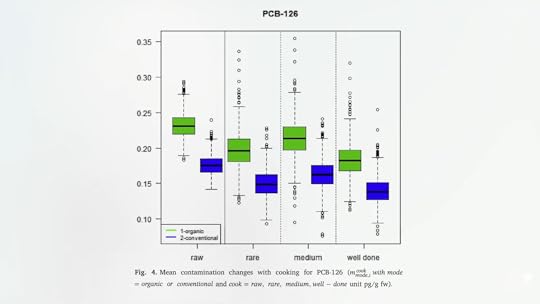
Why cultivate meat at all when you can just buy organic? Surprisingly, “consumption of organic meat does not diminish the carcinogenic potential associated with the intake of persistent organic pollutants (POPs).” A number of studies have recently compared the presence of environmental contaminants in organic meat versus conventional meat, and the researchers found, surprisingly, that organic meat was sometimes more contaminated. Not only organic beef either. Higher levels were also found in pork and poultry.
If you look at the micropollutants and chemical residues in both organic and conventional meat, several environmental contaminants, including dioxins, PCBs, lead, and arsenic, were measured at significantly higher levels in the organic samples. As you can see below and at 2:56 in my video, The Human Health Effects of Cultivated Meat: Chemical Safety, the green is organic meat, and the blue is conventional.

Cooking helps to draw off some of the fat where the PCBs are concentrated, as shown here and at 3:01.
Seafood seems to be an exception. Steaming, for example, generally increases contaminant levels, increasing contaminant exposure and concentrating mercury levels as much as 47 percent, as you can see here and at 3:15 in my video. Better not to have toxic buildup in the first place.

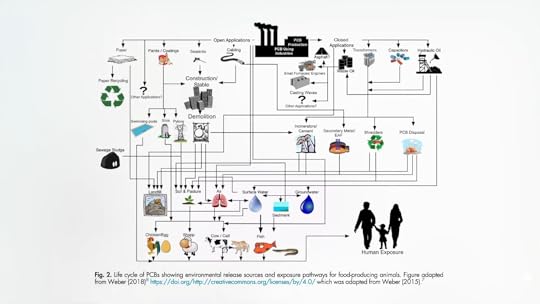
More than 95 percent of human exposure to industrial pollutants like dioxins and PCBs comes from foods like meat, including fatty fish, and dairy, but the pollutants don’t appear magically. The only way the chicken, fish, and other meat lead to human exposure is because the animals themselves built up a lifetime of exposure in our polluted world, from incinerators, power plants, sewer sludge, and on and on, as you can see here and at 3:40 in my video.
Unlike conventional meat production, a slaughter-free harvest would not only mean no more infected animals, but no more contaminated animals either. In terms of pollutants, it would be like taking a time machine back before the Industrial Revolution.
Doctor’s Note:
Cultivated meat means less contamination with fecal residues, toxic pollutants, antibiotics, and hormones; up to 99 percent less environmental impact; and zero pandemic risk. Cultivated meat allows people to have their meat and eat it, too, without affecting the rest of us.
This is the final video in this cultivated meat series. If you missed the first two, check out the videos on Food Safety and Antibiotic Resistance.
I previously did a video series on plant-based meats; see the related posts below.
All videos in the plant-based meat series are also available in a digital download from a webinar I did. SeeThe Human Health Implications of Plant-Based and Cultivated Meat for Pandemic Prevention and Climate Mitigation.
June 3, 2025
Antibiotic Resistance, Cultivated Meat, and Our Health
Medically important antibiotics are being squandered by animal agriculture to compensate for typical factory farming practices.
Cultivating muscle meat directly from cells instead of raising and slaughtering animals would reduce the risk of foodborne illnesses “due to fecal contamination during slaughtering and evisceration of carcasses” because there would be no feces, no slaughter, and no carcasses to eviscerate. In addition, cultivating meat would also reduce the threat from antibiotic resistance.
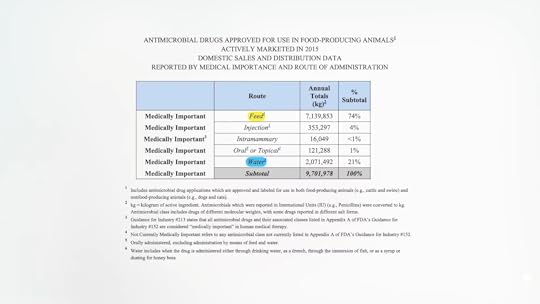
To compensate for overcrowded, stressful, and unhygienic conditions on factory farms, animals are typically dosed en masse with antibiotics. A lot of antibiotics. About 20 million pounds of medically important antibiotics a year, as you can see here and at 0:57 in my video, The Human Health Effects of Cultivated Meat: Antibiotic Resistance.

In the United States, for example, farm animals are given about 2 million pounds of penicillin drugs and 15 million pounds of tetracyclines annually. This is madness.
Antibiotic drugs important to human medicine go right into the feed and water of animals like cows, pigs, and chickens, by the ton and by the thousands of tons, as shown below and at 1:02 in my video. And that is all without a prescription.
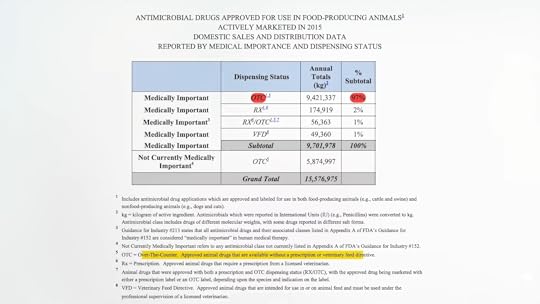
Ninety-seven percent of the tens of millions of pounds of antibiotics given to farm animals in the United States are bought over the counter—without a prescription or even an order from a veterinarian, as seen here and a 1:24. To get even a few milligrams of penicillin, we need a doctor’s prescription, because these are miracle wonder drugs that can’t be squandered. Meanwhile, farmers can just back their trucks up to the feedstore.
Now, half the Salmonella in retail meat—chicken, turkey, beef, and pork—is resistant to tetracycline, as shown below and at 1:50 in my video. About a quarter of the bugs are now resistant to three or more entire classes of antibiotics, including some resistant to “cephalosporins such as ceftriaxone [which] are critically important drugs we use to treat severe Salmonella infections, especially in children.”

Such agricultural applications for antimicrobials are now considered an “urgent threat to human health.” “The link between antibiotic use in animals and antibiotic resistance in humans is unequivocal.”
As shown here and at 2:20 in my video, it all starts with the poop.

Antibiotic-resistant bugs are selected for and then can spread via meat or produce contaminated by poop or they can spread through the wind, the air, or the water, or be carried by insects. There are many pathways by which resistant superbugs can escape. So, even if you don’t eat meat, you can be “put at risk by the pathogens released from stressed, immunocompromised, contaminant-filled livestock” dosed with antibiotics. That’s one of the reasons the American Public Health Association called for a moratorium on factory farms, due in part to all the pollution from concentrated animal feed operations (CAFOs) to the surrounding communities.
Every year, more than five tons of animal manure are produced for every man, woman, and child in the United States. Again, it all starts with the poop. But cultivated meat means no guts, no poop, no fecal infections, and no antibiotics necessary. It also means no fecal or antibiotic residues left in “foodstuffs such as milk, egg, and meat” that can potentially cause a variety of side effects beyond just the transfer of antibiotic-resistant bacteria to humans.
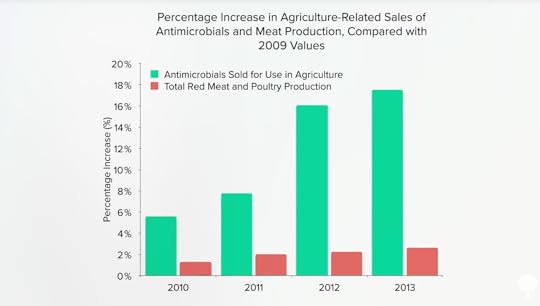
And, as you can see here and at 3:30 in my video, things are getting worse, not better. U.S. animal agriculture is using more antibiotics now than ever.

This isn’t only because more animals are being raised for food, either. Antibiotic sales in the United States are outpacing meat production. Yes, meat production is going up, but there is a serious rise in antibiotic sales for meat production, as shown below and at 3:46.
With the combined might of Big Ag and Big Pharma (who profit from selling all the drugs), it’s hard to imagine anything changing on the political side. The only hope may be a change in the production side.
“The unstoppable rise of super-resistant strains of bacteria is a serious worldwide problem, resulting in 700 000 deaths every year,” and the projections for global antibiotic use in the production of farm animals are “ominous,” estimated to exceed 100,000 tons of antibiotics pumped into animals raised for food by 2030. Quite simply, we may be “on the path to untreatable infections” by using even some of our “last resort antibiotics,” like carbapenems, just to shave a few cents off a pound of meat.
And it’s not just foodborne bacteria. Mad cow disease, swine flu, and bird flu have the potential to kill millions of people. Skeptical? I’ve got a book for you to read, whose author’s “superb storytelling ability makes every page of the book interesting and fascinating for both specialist and layperson.” (Thanks, Virology Journal, for the wonderful book review and calling my book “a must read.”)
Given the threat of the chickens coming home to roost, an editorial in the American Journal of Public Health thought that “it is curious, therefore, that changing the way humans treat animals—most basically, ceasing to eat them or, at the very least, radically limiting the quantity of them that are eaten—is largely off the radar as a significant preventative measure. Such a change, if sufficiently adopted or imposed, could still reduce the chances of the much-feared influenza epidemic…Yet humanity does not consider this option.”
That may be moot, though, because we could cultivate all the chicken we want, without guts or lungs.
It’s hard to stress the importance of that American Journal of Public Health editorial. As devastating as COVID-19 has been, it may just be a dress rehearsal for an even greater threat waiting in the wings—the wings of chickens.
According to the Centers for Disease Control and Prevention, the leading candidate for the next pandemic is a bird flu virus known as H7N9, which is a hundred times deadlier than COVID-19. Instead of 1 in 250 patients dying, H7N9 has killed 40 percent of the people it infects.
The last time a bird flu virus jumped directly to humans and caused a pandemic, it triggered the deadliest plague in human history—the 1918 pandemic that killed 50 million people. That had a 2 percent death rate. What if we had a pandemic infecting billions where death was closer to a flip of a coin?
The good news is that there is something we can do about it. Just as eliminating the exotic animal trade and live animal markets may go a long way toward preventing the next coronavirus pandemic, reforming the way we raise domestic animals for food may help forestall the next killer flu. The bottom line is that it’s not worth risking the lives of millions of people for the sake of cheaper chicken.
If you missed the previous video, see The Human Health Effects of Cultivated Meat: Food Safety. Up next is The Human Health Effects of Cultivated Meat: Chemical Safety.



