Aaron E. Carroll's Blog, page 9
May 7, 2024
Qualitative Brief: Better Understanding VA Urgent Care Delivery
Rates of urgent care and emergency department usage have fluctuated over the years, largely increasing. However, as usage has increased, so have costs, and there is significant ongoing research on how to mitigate this trend. This is true within the Veterans Health Administration (VHA) as well. For VHA, understanding how Veterans are referred into urgent care services and emergency departments will help policymakers better understand bottlenecks in non-emergency care services, hopefully reducing costs and improving Veteran access to high quality care.
The Partnered Evidence-based Policy Resource Center (PEPReC) published a policy brief on the qualitative research of one of PEPReC’s doctoral students, examining the roles of and relationship between VHA urgent care clinics and VHA emergency departments. Read the full brief here.
PEPReC, within the Veterans Health Administration and funded in large part by the Quality Enhancement Research Initiative (QUERI), is a team of health economists, health services and public health researchers, statistical programmers, and policy analysts who engage policymakers to improve Veterans’ lives through evidence-driven innovations using advanced quantitative methods.
The post Qualitative Brief: Better Understanding VA Urgent Care Delivery first appeared on The Incidental Economist.May 3, 2024
Does Intermittent Fasting Increase Heart Attack Risk by 91%?
Sigh. Nutrition research is often bad, and how we talk about it is even worse. If you believe the hype from the past several years, intermittent fasting doesn’t only help you lose weight, it may go so far as to prolong your life. So what do we do with new data suggesting it significantly increases your risk for cardiovascular disease?
The post Does Intermittent Fasting Increase Heart Attack Risk by 91%? first appeared on The Incidental Economist.May 2, 2024
Effects of VHA’s Referral Coordination Initiative on Referral Patterns and Waiting Times
Veterans Health Administration (VHA) launched the Referral Coordination Initiative (RCI) in 2019 to assist Veterans in navigating the various care options available to them, improve scheduling timeliness, and reduce administrative burden for referring providers.
The Partnered Evidence-based Policy Resource Center (PEPReC) published a policy brief exploring whether RCI is associated with changes in the proportion of VHA specialty care referrals completed by community providers (rather than VHA providers) and changes to mean appointment waiting times for VHA and community providers. Read the full brief here.
PEPReC, within the Veterans Health Administration and funded in large part by the Quality Enhancement Research Initiative (QUERI), is a team of health economists, health services and public health researchers, statistical programmers, and policy analysts who engage policymakers to improve Veterans’ lives through evidence-driven innovations using advanced quantitative methods.
The post Effects of VHA’s Referral Coordination Initiative on Referral Patterns and Waiting Times first appeared on The Incidental Economist.April 26, 2024
New Obesity Drugs May Impact Mental Health
In mid to late 2023 there was a flurry of news reports about patients taking new weight loss drugs reporting associated mental health concerns, including suicidal thoughts. There’s still a lot of research to be done to fully understand these drugs and their effects, but we take a close look at the research to figure out just what scientists know about GLP-1 drugs and mental health, and some of the evidence is surprising.
The post New Obesity Drugs May Impact Mental Health first appeared on The Incidental Economist.April 22, 2024
Examining Self-Directed Care for the Rural Veteran Population
Rural Veterans face more barriers to health care than those living in urban areas. In addition to having reduced access to health care facilities, providers, and medical transportation services, rural Veterans are more likely to experience lower quality care and greater communication barriers due to less advanced information technology.
The challenges are even greater for those receiving home- and community-based long-term supports and services. Understanding the relative benefits of self-directed services compared to other paid home- and community-based personal care services in rural areas is of particular interest to Veterans Health Administration (VHA) as nearly three million Veterans aged 65 years and older live in rural areas.
An example of a self-directed program, the Veteran Directed Care (VDC) program helps isolated, aging Veterans and their caregivers develop a spending plan and hire people of their choosing (including family members or neighbors) or purchase equipment or home modifications to ensure the Veteran can live independently at home. Home-based workers or paid family members provide assistance with daily activities (e.g., eating, grooming, getting dressed).
New Evidence:
In January 2022, evaluators from the Partnered Evidence-based Policy Resource Center (PEPReC) published a paper titled “Fewer Potentially Avoidable Health Care Events in Rural Veterans with Self-Directed Care versus Other Personal Care Services” in the Journal of the American Geriatrics Society. The objective was to understand whether rural and urban Veterans used less VHA-paid community or in-house nursing home, acute, or emergency department (ED) care following enrollment in VDC, compared to recipients of other VHA-paid personal care services.
Methods:
This retrospective observational study included over 37,000 Veterans receiving VHA-paid home- and community-based long-term care services in fiscal year 2017. Using VHA administrative data on health status and health care use, evaluators compared the differences in outcomes from pre- to post-enrollment in the VDC program and other VHA-paid personal care services programs for Veterans living in rural and urban areas. The baseline period was 12 months prior to service initiation and the outcome period was 12 months after service initiation.
They used logistic regression models stratified by location (rural/urban) to estimate the relationships between VDC receipt and utilization of VHA-paid community or in-house hospital, nursing home, and ED services. Sensitivity analyses also matched Veterans on several covariates (e.g., age, dementia, comorbidities, etc.).
Findings:
The authors found that both rural and urban VDC recipients had fewer VHA-paid community and in-house nursing home admissions, compared to recipients of other VHA-paid personal care services. Rural VDC enrollees had fewer VHA-paid community and in-house acute care admissions and VHA-paid community and in-house ED visits, unlike urban VDC enrollees who had no significant changes in admissions or ED visits before and after service initiation.
In terms of demographics, VDC recipients were younger, had a higher VHA priority status (significant health issues and/or disabilities; high financial need), and were more likely to have sustained a spinal cord injury compared to recipients of other VHA-paid personal care services programs.
Conclusion:
This study had a few limitations. For example, the data did not include non-VHA paid (e.g., paid for out of pocket or by private insurance) long-term care services and evaluators did not compare administrative costs between the VDC program and other VHA-paid personal care services programs. The study was also unable to determine the degree to which improved health outcomes were due to the VDC program or the presence of a strong family caregiver.
This study suggests that the VDC program is an appropriate and beneficial care option for Veterans with multiple chronic conditions and/or cognitive impairment and may be particularly beneficial for Veterans living in rural areas. It also has the potential to reduce use of VHA-paid community and in-house health care more than other VHA-paid personal care services. Future studies should continue to explore the degree to which non-VHA paid care and nursing home admissions change among VDC recipients.
The post Examining Self-Directed Care for the Rural Veteran Population first appeared on The Incidental Economist.April 15, 2024
A Preemptive Strike on Food Allergy Reactions
If you or someone you love has a life-threatening food allergy, you have to remain constantly vigilant for even the slightest exposure to that food, making even an outing to a restaurant an impossibility for some people. It can be exhausting, particularly with children, and there’s no cure for food allergies. However, the FDA recently approved Xolair for the reduction of allergic reactions to food.
The post A Preemptive Strike on Food Allergy Reactions first appeared on The Incidental Economist.April 10, 2024
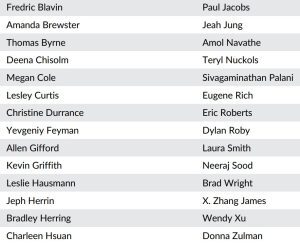
HSR’s outstanding reviewers in 2023
The scholars listed below were rated in the top 5% of reviewers for Health Services Research (HSR) in 2023. Their work, and that of all reviewers, is much appreciated. More here.
April 8, 2024
Measles: The Comeback Kid
Measles is really contagious and can easily spread in pockets of unvaccinated people. In February 2024 a health advisory was issued by the Florida Department of Health in Broward County to warn the public about several confirmed cases of measles at a local elementary school. The Florida Surgeon General made the wrong call on recommendations to parents.
The post Measles: The Comeback Kid first appeared on The Incidental Economist.Evaluation of the Stratification Tool for Opioid Risk Mitigation (STORM)
Veterans are prescribed opioids at higher rates for chronic pain, mental health issues, and substance use disorders than the general United States population. This puts them at increased risk for opioid-related adverse events and opioid use disorder. Responding to concerns for opioid safety, Veterans Health Administration implemented several initiatives including the Opioid Safety Initiative and a mandated case review for all Veterans who are prescribed opioids, facilitated by the Stratification Tool for Opioid Risk Management (STORM). STORM is a web-based dashboard to help assess a Veteran’s risk of experiencing opioid-related adverse events, including death.
The Partnered Evidence-based Policy Resource Center (PEPReC) published a policy brief summarizing the results of their recent STORM evaluation. They found that, for high-risk Veterans, a mandated case review with STORM was associated with a decreased probability of mortality. They also describe the effectiveness of how STORM can be used as a risk mitigation intervention, suggesting the potential of predictive analytic tools to improve patient outcomes. Read the full brief here.
PEPReC, within Veterans Health Administration and funded in large part by the Quality Enhancement Research Initiative, is a team of health economists, health services and public health researchers, statistical programmers, and policy analysts who engage policymakers to improve Veterans’ lives through evidence-driven innovations using advanced quantitative methods.
The post Evaluation of the Stratification Tool for Opioid Risk Mitigation (STORM) first appeared on The Incidental Economist.April 2, 2024
Diversity, Equity, Inclusion, and Justice: Findings and Policy Impacts in PEPReC’s Work
Inspired by the White House’s request to ensure federal agencies equitably serve all eligible individuals and communities, the Partnered Evidence-based Policy Resource Center (PEPReC) developed an initiative to review, incorporate, and uplift a diversity, equity, inclusion, and justice (DEIJ) lens into their center’s work and culture.
Policy analysts at PEPReC drafted a policy brief that shares project-specific evaluation findings related to different health and access outcomes for different Veteran subpopulations and explains how policy changes could improve access to care and mortality risk factors for Veterans with marginalized identities. Read the full brief here.
PEPReC, within the Veterans Health Administration and funded in large part by the Quality Enhancement Research Initiative (QUERI), is a team of health economists, health services and public health researchers, statistical programmers, and policy analysts who engage policymakers to improve Veterans’ lives through evidence-driven innovations using advanced quantitative methods.
The post Diversity, Equity, Inclusion, and Justice: Findings and Policy Impacts in PEPReC’s Work first appeared on The Incidental Economist.Aaron E. Carroll's Blog
- Aaron E. Carroll's profile
- 42 followers



