Leslie Glass's Blog, page 406
January 1, 2018
Authorities Are Cracking Down on Opioid-Peddling Doctors
Patients would travel hundreds of miles to see Dr. Andrzej Zielke, eager for what authorities described as a steady flow of prescriptions for the kinds of powerful painkillers that ushered the nation into its worst drug crisis in history.
At least one of Zielke’s patients died of an overdose, and prosecutors say others became so dependent on oxycodone and other opioids they would crowd his office, sometimes sleeping in the waiting room. Some peddled their pills near tumble-down storefronts and on blighted street corners in addiction-plagued parts of Allegheny County, where deaths by drug overdose reached record levels last year.
But Robert Cessar, a longtime federal prosecutor, was unaware of Zielke until Justice Department officials handed him a binder of data that, he said, confirmed what pill-seekers from as far away as Ohio and Virginia already knew. The doctor who offered ozone therapy and herbal pain remedies was also prescribing highly addictive narcotics to patients who didn’t need them, according to an indictment charging him with conspiracy and unlawfully distributing controlled substances.
Zielke denied he was overprescribing, telling AP he practiced alternative medicine and many of his patients stopped seeing him when he cut down on pain pills.
His indictment in October was the first by a nationwide group of federal law enforcement officials that, armed with new access to a broader array of prescription drug databases, Medicaid and Medicare figures, coroners’ records and other numbers compiled by the Justice Department, aims to stop fraudulent doctors faster than before.
The department is providing a trove of data to the Opioid Fraud and Abuse Detection Unit, which draws together authorities in 12 regions across the country, that shows which doctors are prescribing the most, how far patients will travel to see them and whether any have died within 60 days of receiving one of their prescriptions, among other information.
Authorities have been going after co-called “pill mills” for years, but the new approach brings additional federal resources to bear against the escalating epidemic. Where prosecutors would spend months or longer building a case by relying on erratic informants and only limited data, the number-crunching by analysts in Washington provides information they say lets them quickly zero in on a region’s top opioid prescribers.
“This data shines a light we’ve never had before,” Cessar said. “We don’t need to have confidential informants on the street to start a case. Now, we have someone behind a computer screen who is helping us. That has to put (doctors) on notice that we have new tools.”
And Rod Rosenstein, deputy attorney general, told AP the Justice Department will consider going after any law-breaker, even a pharmaceutical company, as it seeks to bring more cases and reduce the number of unwarranted prescriptions.
Attorney General Jeff Sessions has been in lock-step with President Donald Trump about the need to combat the drug abuse problem that claimed more than 64,000 lives in 2016, a priority that resonates with Trump’s working-class supporters who have seen the ravages of drug abuse first-hand. The president called it a public health emergency, a declaration that allows the government to redirect resources in various ways to fight opioid abuse.
But he directed no new federal money to deal with a scourge that kills nearly 100 people a day, and critics say his efforts fall short of what is needed. The Republican-controlled Congress doesn’t seem eager to put extra money toward the problem.
While the effectiveness of the Trump administration’s broader strategy remains to be seen, the Justice Department’s data-driven effort is one small area where federal prosecutors say they can have an impact.
The data analysis provides clues about who may be breaking the law that are then corroborated with old-fashioned detective work — tips from informants or undercover office visits, said Shawn A. Brokos, a supervisory special agent in the FBI’s Pittsburgh division. Investigators can also get a sense for where displaced patients will turn next.
Authorities acknowledge there are legitimate reasons for some doctors to prescribe large quantities of opioids, and high prescribing alone doesn’t necessarily trigger extra scrutiny. What raises red flags for investigators are the dentists, psychiatrists and gynecologists who are prescribing at surprisingly high rates.
The effort operates on the long-held perception that drug addiction often starts with prescriptions from doctors and leads to abuse of more dangerous black market drugs like fentanyl, which, for the first time last year, contributed to more overdose deaths than any other legal or illegal drug, surpassing pain pills and heroin.
But that focus can cause law-abiding physicians to abandon disabled patients who rely on prescriptions, for fear of being shut down, said University of Alabama addiction researcher Stefan Kertesz. Those patients will turn to harder street drugs or even kill themselves, he said.
“The professional risk for physicians is so high that the natural tendency is to get out of the business of prescription opioids at all,” he said.
Another addiction expert, Dr. Andrew Kolodny, founder of Physicians for Responsible Opioid Prescribing, said prosecutors’ emphasis on “drug-dealing doctors” is appropriate but inadequate on its own.
“It’s just not really going to have that much of an impact on an epidemic,” he said. The bigger change will come from a stronger push for prevention and treatment, he said. And, he added, “They should go after the bigger fish…. the legal narcotics distributors and wholesalers who have literally been getting away with mass manslaughter.”
Investigators said Zielke charged $250 a visit and made patients pay in cash. But Zielke said prosecutors unfairly targeted him. Instead of more prosecutions, he said, the government “should promote more alternative therapies,” he said. “And they should find out why so many people have pain.”
A second indictment by the anti-fraud unit involved a cardiologist in Elko, Nevada, accused of routinely providing patients fentanyl and other painkillers they did not need. Justice officials hope to expand the data-driven work nationwide.
Will it work? As Soo Song, who watched addiction warp communities while serving as acting U.S. attorney in western Pennyslvania, put it: “The best measure of success will be if fewer people die.”

The post Authorities Are Cracking Down on Opioid-Peddling Doctors appeared first on Reach Out Recovery.
Recovery Guidance new website for 2018
It would seem that you can find answers for everything on the Internet, but addiction and mental healthcare consumers have been in the dark about the kinds of care they need and where to find it. To fill the void, the Reach Out Recovery founder created a new website, Recovery Guidance, to provide consumers with direct access to all providers of addiction and mental healthcare near them. The new website was designed with both consumers and providers in mind.
Mental Healthcare Joins Addiction Recovery
Recovery Guidance is the only website that lists both mental healthcare providers including therapists, psychiatrists, psychologists, counselors and addiction treatment providers including rehabs, out patient services, hospitals, recovery residents and local programs. Formerly mental healthcare services have been listed on mental healthcare websites where consumers looking for addiction treatment haven’t been able to find them. RG lists mental healthcare providers and and addiction providers together for the first time.
There is an Assess Yourself banner on every page to help people identify what category of providers they should start their search.
Unbiased Reviews Brings Credibility To The Field
In a field with no accountability, Recovery Guidance is the only website that offers consumers of addiction and mental healthcare treatment the opportunity to review their experience of care. You can think of Recovery Guidance as the Yelp or Healthgrades of recovery. While Reach Out Recovery is a 5013c nonprofit information site, Recovery Guidance is a separate company, and for profit listing site, guided by business leaders in the mental healthcare field, Internet developers with expertise in listing sites and traffic generation, and leaders in the addiction and mental health fields including Dr. Tom Mclellan, Founder of Treatment Research Institute, Senior Editor of the Surgeon General’s Report on Addiction (2016). The goal of Recovery Guidance is to bring transparency to the recovery industry and help consumers find the treatments they need to succeed.
Recovery Guidance Is Recovery 2018
As a mom, dealing with teen substance use and addiction years ago, I simply couldn’t find the help my family needed on the Internet. There were dozens of referral sites and ads for rehabs, but they are confusing. I didn’t know who to trust. There were no reliable unbiased reviews, and no outcomes to compare. As experts in the field will tell you, it’s impossible to compare facilities in a field where there is no accountability, no standardization of care, and no published outcomes. As the addiction and opioid epidemic worsened over the last decade, we, at Reach Out Recovery, saw tens of thousands of families losing loved ones* with no idea where to turn. The media keeps showing the end stages of addiction, but the way recovery actually works or where to find it have not been reporting priorities. We knew we had to do something about it.
The Surgeon General’s Report on Addiction was published in November 2016. In it, 30 years of research reveals there is no one kind of treatment that fits everyone, there are many paths to recovery.
Recovery from addiction (Substance Use Disorder) doesn’t happen with only one component, like rehab or medically assisted treatment. Like, heart disease and diabetes that require a life-changing program that includes: medication, diet, and exercise, successful treatment for addiction recovery includes many components.
The Treatments That Brought Our Family Long Term Recovery
Addiction is a chronic brain disease that requires many different kinds of help over a lifetime. In addition, it is a family disease in which everyone is affected. As a mom, I needed therapy and a program for family issues, better communication, financial management, enabling, and co-dependency. Our family has used all of the components below (except bio feedback) to achieve our longterm recovery.
Out-patient treatment over a period of years
Inpatient 30-day rehab
Recovery Residence (sober living for 30 days or many months)
Individual and family therapy with a counselor, social worker, or psychologist
Treatment with a psychiatrist
Bio-feedback
Medications
Group or animal therapy
A wide variety of 12 step programs
Meditation
Diet
Exercise
Acupuncture
Life skills coach
The Only Website That Brings All The Providers To You
We didn’t know we needed so many different kinds of support when we started our journey many years ago. We are proud that we kept at our recovery work. Did you know that addiction is the only disease for which recovery makes you better than you were before? Get better than you ever dreamed with all the help you possibly could need.
50,000 people have already explored Recovery Guidance. Just in time for the New Year, now providers are invited to sign up so that people looking for their services can find them.
Recovery Guidance Features
RG is free for users
RG is a subscription site for providers
RG’s review system allows consumers to review their experience of care and see what others say about providers they consider
Users are invited to review their experience of care even if their provider has not yet signed up and added a profile
Providers can now sign up to get a google map-assisted, full page profile with a list their services, and no fees ever for direct access to the patients and clients looking for them
Happy New Year. We really needed this.
*The CDC estimates that from 1999 to 2015, more than 183,000 people have died in the U.S. from overdoses related to prescription opioids. Opioid prescribing continues to fuel the epidemic. Today, nearly half of all U.S. opioid overdose deaths involve a prescription opioid.
The post Recovery Guidance new website for 2018 appeared first on Reach Out Recovery.
December 30, 2017
Kick Start Your New Year – Day 7
The final step in kick starting our New Year is to get moving. Movement is activity or motion, including unorthodox exercises like:
Washing the car
Painting
Walking the dog
Gardening
Scrubbing the shower
Going up and down the stairs doing laundry
Emptying the dishwasher
Staining the deck
You don’t have to go to the gym to move. Consider that after many outpatient surgeries, post-op instructions include no participation in strenuous activities. In fact, doctors specifically warn against any activity that exercises the core muscles, including vacuuming. Bet you never thought of vacuuming as a strenuous physical activity that exercises the core muscles.
Almost Any Moving Is Exercise
All the typical hobbies and sports that are considered exercise, are merely ways to move the body. Also under the umbrella of movement are household chores and the physical activity required at many jobs. Aerobic activity encompasses an array of motion, choose ones that are most enjoyable for you.
Make movement fun and you will increase your chances of sticking to it. When movement is fun, it becomes playtime. When it becomes playtime, it is prioritized and added to the day as an inevitable occurrence.
Why Moving Matters
Adding movement to stabilize the blood sugar roller coaster helps to circulate nutrients and oxygen, speeds up metabolism, increases energy, reduces the risk of lifestyle diseases, improves weight management, and lifts the mood. Movement creates the possibility of more movement, and having a surplus of energy is a huge benefit.
Create Habit Change Around Movement
Put a chin-up bar in the doorway of the bedroom. Challenge yourself to attempt 3 chin-ups each time you enter or exit the room. Bam! You’ve created a new habit around movement.
Walk or ride a bike to work. Or park in a spot that is far away from the entrance.
Set your alarm for 15 minutes on the hour to get up from the desk and move around.
These suggestions create habit change. Begin creating the lifestyle that you desire by expanding the way you think exercise is supposed to look.
Try New Moves
When’s the last time you did something for the first time? Try on an activity that you find interesting. Be curious and give these a try:
Go to that dance class
Take on kayaking
Hike the State park
Join the flow of the Tai Chi players
Participate in a ceramics workshop
Finish a 5k
Climb the rock wall
Venture to a water park
Learn how to arrange flowers or make wine
Pursue bass fishing
Basically, experiment with life.
Kick Start Your New Year Anytime
Find your balance and energy by revisiting these steps anytime that works for you. Our favorite way to start a healthy year over again is:
Visit a farmers’ market and stroll around checking out the local, whole foods available.
You’re getting movement AND you’re stocking your pantry with healthy, natural foods. You are nourishing your body in two ways with the added benefit of fresh air! By creating a new recipe around the foods you purchased and crowding out the processed, refined foods that were your go-to meals, you add another element of the seven.
Remember, knowledge does not equal habit change. The vortex of transformation is found when you create a possibility and then hold yourself accountable, take action and get on the court … perhaps literally this week!
The post Kick Start Your New Year – Day 7 appeared first on Reach Out Recovery.
Is wine glass size to blame for how much we drink?
From Medical News Today by Ana Sandoiu As you toast a better year, check out the size of the wine glass; whether it’s small, medium, or large, it is still seven times larger than what it was 300 years ago. According to a new study, this increase in size may well be the reason that we drink so much more today.

As the size of our wine glasses increases, so too does our alcohol intake, suggests new research.
A new study published in the Christmas edition of The BMJ looks at the changes in wine glass size over time and the evolution of our drinking habits.
Theresa Marteau, a professor of behavior and health at the University of Cambridge in the United Kingdom, led the research.
As Prof. Marteau and colleagues note in their study, alcohol consumption has increased dramatically in recent decades.
Wine drinking, in particular, increased by nearly four times from 1960 to 1980 and went on to almost double between 1980 and 2004.
Why is that? It is widely accepted that the increased affordability and availability of wine led to an increase in consumption, but the new research suggests that the size and design of wine glasses may also have contributed to this.
In much the same way that larger plates are believed to have led to greater food consumption, so might glass size have triggered a higher wine intake, the researchers hypothesize.
Wine glasses seven times larger today
Using online databases and interviewing antique glassware experts, Prof. Marteau and colleagues collected information on the size of 411 wine glasses between the years 1700 and 2017.
Some of the sources that were used for studying glass size were the Ashmolean Museum of Art and Archaeology at the University of Oxford, the Royal Household, the catalogs of manufacturer Dartington Crystal, and the website of the John Lewis department store.
The analysis revealed that the size of wine glasses has increased by sevenfold in the past 300 years. Specifically, the capacity of the glasses increased from around 66 milliliters in the year 1700 to around 449 milliliters in 2017.
The post Is wine glass size to blame for how much we drink? appeared first on Reach Out Recovery.
Patient uneasiness complicates treatment for stimulant use
Unlike the incoming patient who knows he has a problem with alcohol, or one who thinks she may have a problem with the ambivalence-inducing marijuana, those with a stimulant misuse history “think they absolutely, positively need their Adderall or they can’t survive,” says John Dyben, DHSc. “People come in expecting that we’ll keep them on the stimulant.”
Dyben adds, “You’ll often hear a parent say, ‘You can’t take him off it. His doctor said he needs it.’”
Hanley Center of course does not allow its patients to remain on psychostimulants. But Dyben says this effort requires a great deal of patient education—not to mention support to assist them through a withdrawal period where they are likely to feel tired and restless and have difficulty focusing (“even if they haven’t had attention deficit disorder,” he says).
“It’s about helping them realize there is a goal to this,” Dyben says. He adds that the facility also makes sure to tell patients before they arrive for treatment that they will not be allowed to continue on a psychostimulant, so that there are no surprises at admission.
Use is reinforced
Part of the challenge in treating stimulant addiction, says Dyben, lies in the multiple reinforcers of use of psychostimulants. These influencers range from educators who often practically demand that a young student be prescribed a stimulant, to the simple fact that psychostimulants are so easy for young people to obtain, whether legally with a prescription or illegally from friends or family members.
Dyben believes that amid the opioid crisis that has dominated the addiction field’s attention, the problem of stimulant abuse never really went away. What hasn’t taken hold yet, unlike in the case of the opioid crisis, is widespread scrutiny of physician prescribing patterns that likely are exacerbating the problem, he says.
He adds that while psychostimulant use almost always is observed with other substance use problems, he recently has observed two cases of pure psychostimulant use without other substance use, in patients in their early 20s.

The post Patient uneasiness complicates treatment for stimulant use appeared first on Reach Out Recovery.
Brain recovery from substance use disorder is possible but takes time
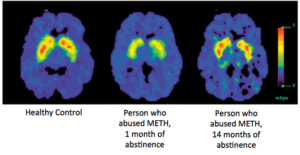
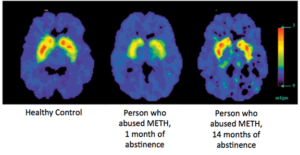
Substance use decreases brain function and changes behavior in ways that those with Substance Use Disorder (SUD) can’t control. With abstinence or Medically Assisted Treatment (MAT) brain recovery is possible. How the brain recovers from addiction is an exciting and emerging area of research. There is evidence that the brain does recover. The image below shows the healthy brain on the left, and the brain of a patient who misused methamphetamine in the center and the right. In the center, after one month of abstinence, the brain looks quite different than the healthy brain; however, after 14 months of abstinence, the dopamine transporter levels (DAT) in the reward region of the brain (an indicator of dopamine system function) return to nearly normal (Volkow et al., 2001).
There is limited research on the brains recovery from alcohol and marijuana use. However, recent studies have shown that some recovery does take place. For example, one study found that adolescents that became abstinent from alcohol had significant recovery with respect to behavioral disinhibition and negative emotionality (Hicks et al., 2012). Lisdahl and colleagues posit that this could mean that some recovery is occurring in the prefrontal cortex after a period of abstinence. Furthermore, other research has found that number of days abstinent from alcohol was associated with improved executive functioning, larger cerebellar volumes and short-term memory.
While promising, this field of research is in its infancy and there have been conflicting results that instead show minimal to no recovery from cognitive deficits. This is especially true for studies evaluating the brains recovery from marijuana use, specifically IQ. On the other hand, some studies have shown that former marijuana users demonstrate increased activation in parts of the brain associated with executive control and attention. Whether this is associated with the compensatory response or brain recovery has yet to be determined.
What is clear is that alcohol and marijuana do have neurotoxic effects and, to some degree, this damage can be reversed. There is minimal evidence on how we can improve brain recovery from substance use, but emerging literature suggests that exercise as an intervention may improve brain recovery. Physical activity has been shown to improve brain health and neuroplasticity. In previous studies of adults, physical activity has improved executive control, cerebral blood flow and white matter integrity. While none of these interventions have been done in adolescent alcohol or marijuana users, this approach is promising and should be investigated further.
The post Brain recovery from substance use disorder is possible but takes time appeared first on Reach Out Recovery.
Addiction is similar to other chronic diseases
Addiction research has clarified the definition of addiction which is now called substance use disorder SUD and considered a chronic brain disease. Over the last 30 years research has brought new understanding about how substances hijack and negatively impact brain function. This new information about the way the brain is affected, can now replace outdated beliefs and improve treatment and outcomes.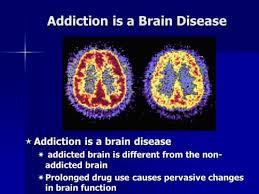
Addiction Research Challenges Outdated Myths
One common outdated belief is that addiction is a weakness that must be managed by abstinence and will power alone. Another common belief is that a stint in rehab (a 30, 60, 90 day program) will arrest substance use and restore normal life. The truth is there are many paths to recovery, and recovery is not a short term undertaking, but rather a life-long pursuit. It can be effectively treated just like any chronic disease. But first SUDs and their impact on the brain must be understood as a chronic illness that requires long-term maintenance and attention.
5 Ways Addiction (SUD) Is Similar To Other Chronic Diseases
Addiction is similar to other chronic diseases, like diabetes and heart disease, in the following ways:
It is preventable
It is treatable
It changes biology
It is progressive and gets worse over time
If untreated, it can last a lifetime, and can even cause death
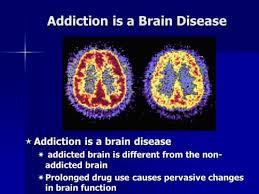
Simply put, addiction (SUDS) changes the brain and impairs the way it works. Just as cardiovascular disease damages the heart and changes its functioning.
Below is an image of the brain (left) and the heart (right).
These images show how scientists can use imaging technology to measure functioning of the brain and heart. Greater activity is shown in reds and yellows, and reduced activity is shown in blues and purples. Both the healthy brain and the healthy heart show greater activity than the diseased brain and heart, because both addiction and heart disease cause changes in function. In drug addiction, the frontal cortex in particular shows less activity. This is the part of the brain associated with judgment and decision-making (NIDA).
The post Addiction is similar to other chronic diseases appeared first on Reach Out Recovery.
New Years resolution about drinking always follows the holidays
From The New York Times by Gabriella Glaser After a season of indulgence, many Americans resolve to drink less in the new year. It’s a common pledge — many of us can recall cringe-worthy texts sent after a raucous night out or a regrettable comment uttered after that third glass of wine.
These intentions are rooted in a stark reality. For all the deserved attention the opioid crisis gets, alcohol overuse remains a persistent public health problem and is responsible for more deaths, as many as 88,000 per year. While light drinking has been shown to be helpful for overall health, since the beginning of this century there has been about a 50 percent uptick in emergency room visits related to heavy drinking. After declining for three decades, deaths from cirrhosis, often linked to alcohol consumption, have been on the rise since 2006.
The pattern has been years in the making. Rick Grucza, an epidemiologist who has been studying alcohol consumption patterns for more than a decade, says the numbers are incontrovertible. Since the early 2000s, according to five government surveys Dr. Grucza has analyzed, binge drinking — often defined as five per day for men and four per day for women — is on the rise among women, older Americans and minorities.
Behind those figures there’s the personal toll — measured in relationships strained or broken, career goals not met and the many nights that college students can’t remember. In researching my 2013 book on women and drinking, and many articles on the topic since, I’ve spoken with hundreds of problem drinkers of all races. Most of the people I’ve spoken to were college-educated; it’s a sad fact that many people learn to drink excessively in college. I found that a lot of people lack physical symptoms of alcohol dependence but they think they are overdoing it, and they are worried.
Having More to Drink
A government survey finds women and older Americans are binge drinking at much greater rates. In this study, binges are defined as five or more drinks on any one occasion for both men and women.

Percentage who reported
binge drinking during
the past month (2013)
Change in number
who binge drink,
2002 to 2013
39%
–4%
All people ages 18-29
33
–2
Men of all ages
29
+10
All people ages 30-49
18
+24
All people ages 50-74
17
+13
Women of all ages
8
+23
All people
ages 65 or older
By The New York Times | Source: analysis of National Survey on Drug Use and Health data by Richard Grucza, Washington University in St. Louis
Many alcohol researchers and substance-use clinicians believe the steady increase in problem drinking arises from a deeply felt sense of despair: “Since the attacks on 9/11, we’ve been in a state of perpetual war, and a lot of us are traumatized by that,” said Andrew Tatarsky, a clinical psychologist who specializes in treating people with substance-use disorders.
The superrich might be making money, Dr. Tatarsky said, but many others are just worried about making ends meet. Uncertainty about tax changes and the cost of health insurance only adds to their burden.
And the culture around drinking, the way we drink, has grown more intense. Epidemiologists say that excessive and binge drinking begins in college, and that for many it continues through early adulthood with after-work happy hours — so much so that Thursdays, in many circles, have become “Little Friday”— code for hitting the bar after (or in some Silicon Valley companies during) work.
Cues from popular culture make alcohol look glamorous and fun: “They send the message that you’re missing out if you are not up on the latest cocktail,” said Carrie Wilkens, also a clinical psychologist treating substance abuse. And as adults age and feel burdened by the responsibilities of family and work, drinking can be an instant stress reliever.
Many who struggle with drinking aren’t getting the help they need, largely because they think that the only way to gain control over alcohol is to abstain. Facing such a severe restriction, they may not try to change unless they hit a mythological “rock bottom.”
Nobody wants to view himself as an addict, and the fact of the matter is most problem drinkers aren’t. Many people are afraid even to discuss the topic with their doctors for fear of being labeled. But in fact, researchers have long shied away from using the term “alcoholic,” because it’s both negative and dated.
In the DSM-V, the new term to describe problematic drinking is alcohol-use disorder — a clunky but more expansive phrase that denotes a spectrum of risky drinking from mild to moderate to severe. Only about 10 percent of the estimated 16 million Americans who abuse alcohol fall into the severe category, according to Reid Hester, a clinical psychologist who has been studying addiction for more than 40 years. While those in the severe category might need to abstain from drinking, the vast majority of others don’t, he said.
Newer treatments embrace an array of techniques and are effective for those with mild and moderate problems. A great deal of research supports the use of anti-craving medications, such as naltrexone, and harm-reduction therapy, which Sheila Vakharia, an assistant professor of social work at Long Island University, says provides practical tools for solving behavioral problems.
Many of the new treatments help people track their drinking — and perhaps most important, understand why they’re imbibing in the first place. Dr. Tatarsky, for instance, teaches patients to learn how to “surf” their urges — taking 15 seconds to notice the emotion that might be causing them, and then substituting healthier behaviors such as breathing exercises. He also teaches strategies: “Before you go to a party, before you set out on your week, it’s useful to have a plan, just like athletes have game plans.”
Others offer web-based methods to curtail drinking, and in some initial research, they have shown promise.
Dr. Hester founded Checkup and Choices, a company that sells a web-based tool for reducing drinking. Since 2003, more than 60 percent of the 22,000 users of the app have been women.
Drinking poses special risks for women, of course. They’re almost twice as likely as men to have anxiety disorders, which they often medicate with alcohol. And biologically, women are more at risk for alcohol’s intoxicating effects.
Because of the stigma associated with alcohol problems, women — especially those with children — are less likely to seek help. Dr. Hester believes that since web-based programs are confidential and available around the clock, women are more likely to turn to them.
The news about our alcohol habits may seem grim, but there’s room for hope. I’ve been inspired by stories of the people I’ve met who’ve overcome drinking problems. One of my favorites is Jane, a Virginia businesswoman who found her drinking spiraling out of control after her company went under in 2009. She used a harm-reduction suggestion of abstaining for 30 days — at first a challenge — and then reintroduced alcohol while chronicling her thoughts, feelings and cognitive abilities after each drink on note cards.
She recognized a stark pattern: She felt happy and lucid after her first and second drinks, but sloppy and maudlin after her third and fourth. She taped the note cards on her refrigerator and kept them up for a year as a reminder of how bad she felt after that third drink. Years on, she still thinks about those notes, especially during these stressful times. More often than not, she switches to water.
“Happiness,” she said, “doesn’t come in a bottle.”
Continue reading the main story
Gabrielle Glaser (@GabrielleGlaser) is the author, most recently, of “Her Best-Kept Secret: Why Women Drink — and How They Can Regain Control.”
The post New Years resolution about drinking always follows the holidays appeared first on Reach Out Recovery.
December 29, 2017
Kick Start Your New Year – Day 6
What, where, when and how to eat are only part of the picture. Lasting transformation happens requires downtime. This is why sleep matters.
Why Does Sleep Matter?
It’s a fact. Good sleep habits make you healthy. According to the Centers for Disease Control and Prevention (CDC), insufficient sleep is a public health problem.
Studies indicate that people who experience a low quality or quantity of sleep are at an increased risk for lifestyle diseases and health problems such as:
Hypertension
Diabetes and obesity
An overall reduced quality of life
Decreased productivity
For some, it encourages eating at night when you should be resting.
How Much Sleep Do We Need?
For the average adult, 7 – 9 hours is considered a sufficient amount to aid the body in its regenerative activities. When sleep is deep and restorative, blood pressure drops, muscles relax, energy is restored and tissue growth and repair occurs. A lot is going on when the mind is at rest. Plus, we’re too busy relaxing to over-eat.
What Keeps Us Awake?
So, you’re getting ready for bed but your brain is wide awake. “I should just keep working, maybe I should clean my desk instead, or unload the dishwasher, or wash that one last load of clothes, or finish writing that paper, or change the oil in my car ….” In that split second when your head hits the pillow and your eyelids become droopy, you snap awake and stare at the ceiling. You pray that tonight the endless chatter in your head will cease. You long for uninterrupted slumber. Know that feeling? We all do.
A Physical Change Occurs
The constant chatter of worry, stress and anxiety that fills your mind at bedtime acts to turn on the hormone, cortisol. Cortisol is counterproductive to a lifestyle of rejuvenation and healing because it is released as part of the fight-or-flight response. When your mind is distracted with excessive thoughts, your body is tense and ready to respond in a manner that is unfavorable to sleep. When you relax and slow down, you stop producing so much cortisol and sleep is yours!
How To Calm Down
Like oral hygiene, sleep hygiene requires a commitment to routine. Avoiding caffeine, alcohol, nicotine and large meals close to bedtime have been shown to improve sleep. Unplugging electronics can take the form of no television in the bedroom or simply powering down a kindle, ipad or smartphone in the hour before bedtime. Your task is to do something of great difficulty: RELAX!
Breathe And Reset Your Thoughts
Silence the chatter with this calming routine:
Connecting to your breath. Breathe in for 4 counts and breathe out for six. Merely counting your breaths gives your mind something calming to do.
Relax your jaw.
Un-crinkle your forehead.
Get comfortable.
Focus on gratitude. Focus on what you have accomplished, not what is left to get done.
Make it a habit to reflect on five things you are grateful for as part of your bedtime routine. When you adopt an attitude of gratitude, you are opening yourself to having more of what you want … like uninterrupted, restorative sleep.
Are personal problems like addiction or family dysfunction keeping you awake? Recovery Guidance provides a free list of therapists and counselors in your area.
The post Kick Start Your New Year – Day 6 appeared first on Reach Out Recovery.
Frostbite: Know the signs and symptoms
From Fox Health News By Dr. Manny When old man winter comes to town, it’s important to make sure you and your family are ready for more than just a heavy snow fall.
Frostbite is a serious medical condition that occurs when the skin and underlying tissues literally freeze.
Since kids lose more heat from their skin than adults, they are at an increased risk for developing the condition. The most common cause for frostbite is exposure to freezing temperatures and wind chills below zero.
According to the National Weather Service’s wind-chill chart, if the temperature is -15 degrees out with a 20mph wind, the temperature will feel like -42 degrees and your child could get frostbite within 10 minutes.
Frostbite typically affects smaller more exposed body parts like- the nose, earlobes, fingers, hands and toes.
Signs and symptoms parents should look out for include:
-A change in skin color- usually to a red, white or pale grayish-yellow color
-A prickly and slightly painful sensation
-Hard or waxy looking skin
-Numbness
-A cold or burning feeling
-Blistering, in severe cases
If you ever suspect your child has frostbite, get him or her indoors and bathe the affected area in lukewarm water – not hot water. If the symptoms worsen, seek medical help immediately.
Here are some helpful tips to keep you and your family safe in cold temperatures:
-Stay updated on the weather forecast and wind chill readings.
-Dress in layers and wear windproof and waterproof outer garments.
-Cover your head with a hat that goes over your ears and wear mittens rather than gloves
-And don’t forget to limit your time outside and change out of any wet clothes or shoes as soon as you or your child comes back indoors.
The post Frostbite: Know the signs and symptoms appeared first on Reach Out Recovery.



