Leslie Glass's Blog, page 274
April 21, 2019
The FDA Just Approved The First Generic Nasal Spray To Reverse Opioid Overdoses
The Food and Drug Administration (FDA) on Friday announced that it granted final approval to the first generic naloxone hydrochloride nasal spray, which can be used to reverse opioid overdoses.
The approval is part of the FDA’s wider effort to make tools for stopping or preventing opioid overdoses more accessible and widely used. The agency is also working with drug companies to bring over-the-counter versions of naloxone to market, and is prioritizing the approval of other generic naloxone products.
Friday’s announcement, which makes official a tentative approval previously granted to Teva Pharmaceuticals, means there will soon be a generic alternative to Narcan, the widely used naloxone nasal spray sold by Emergent BioSolutions.
Naloxone can also be delivered by injection. Generic versions of injectable naloxone have been available for years, and can cost as little as $20 to $40. Nasal sprays, however, provide a more user-friendly delivery vehicle that can be used even by those without medical training, such as civilians and loved ones of those struggling with substance use, as well as first responders.
Nearly 50,000 Americans died from an opioid overdose in 2017, according to federal estimates. Heroin and prescription opioids continue to contribute to many deaths, but potent synthetic opioids such as fentanyl have become a rapidly growing problem in recent years, according to federal data.
The list price for a Narcan kit is set at $125, though Emergent runs several programs meant to make Narcan more affordable and accessible for first responders, government agencies and others who need it. Last year, the company offered to distribute Narcan to every public library and YMCA in the country. Narcan can also now be purchased at many major pharmacies, and — although it is not technically an over-the-counter product — state orders often allow it to be purchased without a prescription.
A Teva representative told TIME that details about the generic version’s pricing and release are not yet available.
If the content in ROR has helped you or a loved one, please consider making a donation to keep us going. We need your support to survive and thrive.
The post The FDA Just Approved The First Generic Nasal Spray To Reverse Opioid Overdoses appeared first on Reach Out Recovery.
8 Signs That Coworkers Are Addicted
From USA Today With roughly 23.5 million Americans addicted to drugs or alcohol, and another 22 million in recovery, substance abuse happens often happens on the job.
“It rarely goes unnoticed,” says Lawrence Weinstein, chief medical officer for American Addiction Centers. ”People just don’t know what to do.”
Here are signs a co-worker might be struggling with alcohol or drug addiction:
Falling asleep at work, or constantly appearing to be very tiredSuddenly making frequent mistakesFrequent trips to the bathroom or break roomExtreme mood swingsTheft or disappearance of valuable pieces of company propertyMissed appointments or deadlinesDifficulty concentrating or recalling details, inability to follow instructions or unusual amount of time needed to complete routine tasksChanges in hygiene
If the content in ROR has helped you or a loved one, please consider making a donation to keep us going. We need your support to survive and thrive.
The post 8 Signs That Coworkers Are Addicted appeared first on Reach Out Recovery.
Eminem 11 Years Sober
From PeopleThe rapper, 46, shared his milestone on social media Saturday, posting a photo of the medallion he received for being 11 years sober.
The medallion is stamped with the Roman numeral for eleven, “XI,” and the words “Unity,” “Service” and “Recovery.”
“11 years – still not afraid,” Eminem captioned the photo.
Last year, the rapper, who was born Marshall Mathers, also acknowledged the anniversary of his sobriety, sharing a photo to Instagram in between his headlining sets at Coachella.
“Celebrated my 10 years yesterday,” he wrote alongside the image, in which he held a medallion up to the camera.View image on Twitter

Eminem previously revealed he had a near-death experience from an accidental overdose back in 2007 after his addiction got so bad that he was taking up to 20 pills a day.
The star opened up about his near-fatal overdose on Revival, his ninth studio album that was released in December 2017.
On the 18th track, titled “Castle” featuring Skylar Grey, Eminem writes letters to his 23-year-old daughter Hailie Jade, with the third verse talking about her 12th birthday and recalling how he overdosed on methadone and nearly died.
“Your dad’s at the end of his rope/ I’m sliding down a slippery slope/ Anyway, sweetie, I better go, I’m getting sleepy … Love, Dad, s—, I don’t know,” he raps.R
Then on the 19th and final track of Revival, titled “Arose,” Eminem continues the narrative of “Castle” by speaking directly to his daughter again, this time as final apologies from his deathbed.
“Just heard they’re unplugging me/ And it’s your birthday/ Jade I’m missing your birthday/ Baby girl, I’m sorry,” he says.
However, the end of the verse is noticeably different: “I’m pledging to throw this methadone in the toilet” he says, referring to a new beginning.
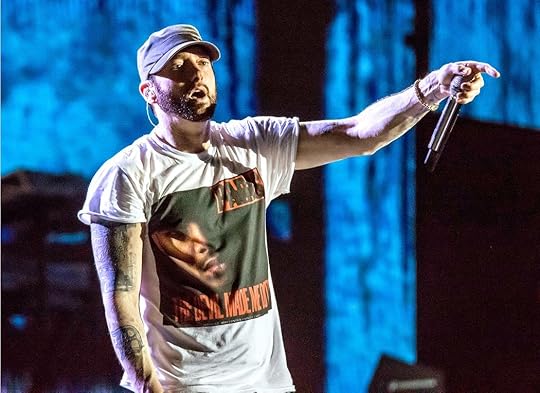
“I used to get pills wherever I could,” the musician told the New York Times in 2011. “I was just taking anything that anybody was giving to me.”
On top of crediting his kids — biological daughter Hailie and his two adopted daughters, Lainey and Whitney — with keeping him sober, he also replaced “addiction with exercise.”R
“When I got out of rehab, I needed to lose weight, but I also needed to figure out a way to function sober,” the rapper told Men’s Journal in 2015. “Unless I was blitzed out of my mind, I had trouble sleeping. So I started running. It gave me a natural endorphin high, but it also helped me sleep, so it was perfect.”
Eminem added, “It’s easy to understand how people replace addiction with exercise. One addiction for another but one that’s good for them.”
The post Eminem 11 Years Sober appeared first on Reach Out Recovery.
April 20, 2019
If You’re Depressed, Reach Out
Tens of thousands of people perish in the US every year from suicide and despair related to substance and alcohol use. We mourn each and every loss of a precious loved one. The lives of so many families will never be the same. It’s sad that our culture doesn’t allow families that suffer losses from addiction or depression to feel the same respect and dignity as those who have lost loved ones to other diseases.
But even in recovery and slowly healing millions of people feel hopeless and alone every day. Isolation is the most painful thing in the world. Do something about it.
Feeling alone, being alone, and unable to engage with others when things are at their worst, are some of the hallmarks not just of addiction, but also of just plain being human. It’s hard to ask for help when you’re down. I wasn’t taught to ask for help, were you? Even though I have the tools to reach out, sometimes I just can’t. When I feel the worst is when I need help the most. And it’s the time I really have trouble picking up the phone.
Why is reaching out and making that call so important?
When you’re lost in your own head, you’re actually lost. You could just as well be in the Gobi desert. Or on Mount Everest. In quicksand up to your ears. Up the creek without a paddle. Doesn’t matter where you are. You’re lost. When you’re lost on the road, GPS can help. When you’re lost in your head, only other people can help. Sometimes just the words, “I understand” can help you turn the corner. Sometimes you need perspective only someone else can give you. Sometimes you need a lot more help than that. If you’re really in trouble, a friend offering to take you to the movies is not enough, or a pull up your socks lecture from a family member could make things a lot worse.
So this is the time when making the choice who to call can make all the difference. This is not the time to call someone who’s mad at you. An aunt who remembers what you did to your mother when you were ten, or the brother whose wedding you ruined with a tantrum, or the ex who harbors a grudge, or any of the people you think may have harmed you. And you may have a long list. These are not the people to call for sympathy, empathy or the path to feeling better.
This is the time to rely on the kindness of genuine friends, people who accept you no matter what, or strangers in safe places. Help is most likely to come from people who won’t use your current misery as an opportunity to call you out or remind you of all the times you may have been a pain in the ass. 12 step fellowships and meeting provide those crucial connections for millions of people. For addiction recovery 12-step programs are often the first place to go.
If the content in ROR has helped you or a loved one, please consider making a donation to keep us going. We need your support to survive and thrive.
For Depression and risk of suicide. The numbers below are trusted sources of help.
Crisis Call Center
800- 273-8255 or text ANSWER to 839863
24 hours a day, seven days a week
http://crisiscallcenter.org/crisisservices-html/
National Suicide Hotline
800-SUICIDE (784-2433)
800-442-Hope (4673)
24 hours a day, seven days a week
National Suicide Prevention Lifeline
800-273-TALK 8255
24 hours a day, seven days a week
http://suicidepreventionlifeline.org
Thursdays Child National Youth Advocacy Hotline
800-USA-Kids (872-5437)
24 hours a day, seven days a week
The post If You’re Depressed, Reach Out appeared first on Reach Out Recovery.
4 Tips For Strategic Holiday Eating
Be strategic about your holiday eating this week. Passover and Easter both signal food, glorious food to us all. We do know the consequences of all that indulgence, but we can prepare for it.
Strategic Holiday Eating Curbs Appetite and Shame
Just the thought of all that luscious food makes my waistband expand. My eyes widen taking in all the delights to eat; and my mouth waters in anticipation of that first bite—the first of many, no doubt! Of course we don’t think of the consequences of stuffing ourselves: weight gain, heartburn, lethargy, gas, and mood swings. Not to mention our feelings of shame and remorse. I can’t believe I ate ALL that food!
Strategic Holiday Eating Includes Enjoyment
Now, I’m about to tell you something you might not expect from a health coach: one day of indulging doesn’t make a huge difference to your health goals and I actually recommend you enjoy yourself. Take a day off! In holiday season time like this week, you can plan for three days. Just avoid gluttony for the days and weeks following your indulgences now.
Unless, you have a health condition that requires you to restrict your diet—such as diabetes, or high blood pressure—then of course, you should heed your doctor’s advice. But in the case of everyone else without a pressing health condition (even those who want to lose weight), I say enjoy yourself and eat the foods you wouldn’t normally.
How Much Does Each Overindulgence Cost Calorically
The reality is that one day of overindulging typically amounts to consuming around 4500 calories. Even if your body stored all of these excess calories as fat, it would only result in a whopping one pound gain. Yep, that’s all. So in the grand scheme of things, it doesn’t really matter.
Track The Treats
My advice doesn’t mean eat everything in sight and snack all day; it means enjoy a treat here or there, and don’t worry about eating more than you normally would. And you certainly don’t have anything to be shameful about by enjoying food with friends and family over counting calories (not that I recommend that either (but that’s another blog, for another day!).
Here’s The Strategy
The way that I plan to enjoy Easter this year is to not buy excesses of indulgent food—because once it is in my home, I will eat it all and much sooner than I had planned! I buy some of what I fancy. On the holiday itself, I’ll eat a reasonably nutritious breakfast, enjoy my Easter meal—and all the treats—and perhaps have a snack later on if I feel like it. I’ll walk or cycle over to my friend’s house—who is hosting—so that afterwards, the walk/cycle back will help with the post-meal lethargy and improve my digestion.
Tips For A Quick Recovery
Know this: if you do overindulge for a few days with all of the leftover food, fear not. There are a few things you can do to get back on track:
Give leftover food to friends and family to take away with them—removing any temptation to snack on them for days after.
Schedule workouts in between the holidays so you commit to keeping up your normal routine. If you know you’ll put them off, sign up for personal training, or arrange to go with a friend—that way, you’re less likely to cancel. Once you exercise, it’s highly likely you’ll make healthier food choices.
Watch your favorite shows—but not for hours on end. I have a tendency to eat the most amount of [mindless] calories in front of the TV—I sometimes can’t believe I’ve eaten the entire plate of food when I look down. Eating in this way is a sure fire way of consuming a lot of excess calories. Try to eat meals at the table or without the distraction of TV. Savor and taste your food—eat slowly and mindfully.
When you plan your grocery list for holiday food, also plan lots of healthy meals to make. That way you’re more likely to commit to getting back on track the day after the holiday because the food is already in your home.
My message is this: enjoy yourself and spend time with loved ones without worrying about eating too much Easter candy. One day, doesn’t have to turn into a whole month of overindulgence.
If the content in ROR has helped you or a loved one, please consider making a donation to keep us going. We need your support to survive and thrive.
The post 4 Tips For Strategic Holiday Eating appeared first on Reach Out Recovery.
April 19, 2019
8 Essential Steps To Addiction Recovery
Is there path to addiction recovery that should be followed? What steps have to be taken, and how long before recovery works? Is just stopping use enough? How about life after rehab or detox, or even sober living? Addiction, now called Substance or Alcohol Use Disorder is confusing. Here’s some of what we know.
30 years of research shows there are many paths to recovery, as cited in the Surgeon General’s 2016 Report on Addiction. But there are some essential steps that can’t be skipped.
The Hunt is On For Protocols That Work
It is a fact that substance and alcohol use alter brain function. No one wants to become a different person, but substance and alcohol use do just that. Addiction is a chronic, relapsing disease of brain reward. When using, people do things they never would have done had they not become addicted.
Old Habits Need Changing
When using stops, however, the negative patterns of behavior do not automatically reverse. People retain the behaviors they learned as substance users, and untreated those behaviors will remain throughout life. This can be confusing for people who long for a quick fix and believe rehab, sober living, or outpatient treatment can reverse the substance user’s survival patterns that no longer work for them. The fact that people don’t automatically return to their previous selves also poses a perplexing problem for researchers. What are the proven treatments that will end both substance use and the behaviors that accompany it? There aren’t any. Recovery is a process.
Necessary Process For Addiction Remission, Thought, and Behavior Change
Stopping useHealing the brainLearning the language of recoveryFollowing a recovery programCreating new habits in a drug-free lifestyle Establishing healthy relationshipsBecoming accountable and honestManaging money and timeWorking at a paying job to restore reliability and trust
8 Steps To Addiction Recovery
Detox in a safe environment.Assessment of substance and alcohol users to determine long term treatment needs. This could be a therapist, physician, psychiatrist addiction specialist, or a combination of providers.Make a treatment plan. After evaluation, a treatment plan should be developed to reflect the length of time it actually takes to learn reliability accountability and life skills. A treatment plan might include being in patient at a rehab, followed by intensive out patient treatment while living in a sober residence. It might include detox, followed by intensive out-patient treatment for six months or longer, followed by weekly therapy and other sessions. It might several years in sober living communities with group and other therapies. Create reasonable goals and expectations.Healing the brain takes several years, so don’t think short term treatment will solve the problem. All treatment programs should include some kind of 12 step group (whether NA, AA, Smart Recovery, Celebrate Recovery, Al Anon, or other group that teaches the language of recovery. Groups don’t not just help people to stop using, they also serve as a guide to behavior and attitude change.Sober living usually has a work requirement so getting and keeping a stress free job is essential.When trust and accountability have been established, work is in place, and healthy relationships are in effect, those in recovery still need ongoing support through the rest of their lives. While treatment may end, and the disease is in remission, it still requires lifelong management.
To learn more about each phase of recovery, use the fly-away menu (often called hamburger) to explore the recovery topics and categories in ROR.
If the content in ROR has helped you or a loved one, please consider making a donation to keep us going. We need your support to survive and thrive.
The post 8 Essential Steps To Addiction Recovery appeared first on Reach Out Recovery.
Can Grants To Study Opioids Reduce Deaths
From Time The National Institutes of Health (NIH) on Thursday announced an ambitious new study that’s meant to reduce opioid-related deaths by 40% in communities that have been hardest-hit by the ongoing epidemic.
The NIH awarded grants to four research sites — the University of Kentucky, Boston Medical Center, Columbia University and Ohio State University — through the three-year, $350 million project, called the HEALing Communities Study. Each site will test the effectiveness of various strategies for combating and preventing opioid addiction in at least 15 communities in those states that are struggling with widespread substance misuse, with the goal of reducing opioid deaths in these areas by 40% over three years, the NIH says.
In 2017, the most recent year with federal estimates available, nearly 50,000 Americans died after overdosing on opioids including heroin, prescription painkillers and the powerful synthetic opioid fentanyl.
The interventions that will be examined in the study include distributing opioid-overdose-reversing naloxone throughout the communities, helping individuals in the criminal justice system find substance abuse treatment and making addiction care part of regular doctor’s visits, according to the announcement.
The announcement did not specify whether more politically controversial techniques, such as needle exchanges and safe injection facilities, would be studied. It did say, however, that research sites would track upticks in medication-based treatment, which can include using drugs to help wean users off of illicit opioids.
Opioid abuse has proved to be an intensifying and persistent public-health issue over the last 20 years, and the problem has evolved over time. While prescription opioid companies have been widely blamed for getting many people hooked on opioids in the first place, synthetic opioids like fentanyl, which often come from outside of the U.S., today pose among the most pressing threats. So many people are dying after using potent synthetic opioids, in fact, that many communities are now targeting their response efforts around these drugs.
The post Can Grants To Study Opioids Reduce Deaths appeared first on Reach Out Recovery.
Crack Pie Is No More As Milk Bar Changes Name Of Famous Dessert
From
From this day forth, Crack Pie is no more. The famous pie, served at the New York-based bakery Milk Bar, will change its name, according to a letter written by the bakery’s founder, Christina Tosi. “We’ve made the decision to stop using the name Crack Pie. Starting today, it will be known as Milk Bar Pie,” Tosi wrote. “While change is never easy, we feel this is the right decision.”
The pie formerly known as Crack Pie, now Milk Bar Pie, from the bakery Milk Bar.Crack Pie is a butter pie with an oat crust. The change comes after continued controversy, with the name’s reported allusion to the addictive nature of crack cocaine, which decimated mostly African-American communities in the 1980s and ’90s. Devra First, food writer for the Boston Globe, wrote a column blasting the name last month. “A bakery would never try to market something called Fentanyl Cake, and the name Crack Pie feels offensively off-key,” she wrote. Other food writers have also written about the name before First’s column. Tosi wrote in her letter that showing respect, having integrity and loving the job were the fuel of her employees whose mission is to “spread joy and inspire celebration.” “The name Crack Pie falls short of this mission,” she wrote. She decided on the name Milk Bar Pie because “it’s been on the Milk Bar menu since day one” and that “the old name was getting in the way of letting the gooey, buttery slice bring happiness— my only goal in creating the thing in the first place.”Crack Pie still shows up on Google searches, but once the link is clicked, Milk Bar’s website says “Milk Bar Pie.” Milk Bar was founded in 2008 by Tosi, an award-winning pastry chef. Tosi was featured on the Netflix docu-series “Chef’s Table” last year.
The post appeared first on Reach Out Recovery.
April 18, 2019
What Is Drunkorexia
From Washington Post By Cara Rosenbloom
Drunkorexia is fasting then drinking and getting very drunk and sick. A very dangerous combination. Imagine this scenario: A female college freshman doesn’t eat anything all day, exercises on an empty stomach, then downs five shots of tequila in less than two hours. Because there’s no food in her system to help slow the absorption of alcohol, those shots affect her rapidly, leading to inebriation and possibly passing out, vomiting or suffering alcohol poisoning. That’s drunkorexia.
Tavis Glassman, professor of health education and public health at the University of Toledo in Ohio, researches drunkorexia and worries about scenarios such as the one described above: “With nothing in her system, alcohol hits quickly, and that brings up the same issues as with any high-risk drinking: getting home safely, sexual assault, unintentional injury, fights, blackouts, hangovers that affect class attendance and grades, and possibly ending up in emergency because the alcohol hits so hard,” he says.
From a medical point of view, Seattle-based registered dietitian Ginger Hultin points out that if alcohol is prioritized over food, it could result in nutrient deficiencies such as calcium, B-vitamins, magnesium, fiber and protein.
“Alcohol can negatively affect the liver or gastrointestinal system, it can interfere with sleep, lower the immune system and is linked to several types of cancers,” Hultin says.
With all of the noted harms, why would a promising college freshman choose this unhealthy pattern? It’s probably not a choice, but mental health and addiction issues mixed together. Studies show that having a preexisting eating disorder or alcoholism are predictors of drunkorexia.
There are no national statistics on the prevalence of campus drunkorexia, and surveys from colleges range widely: One reportconcluded that 34 percent of all students surveyed had engaged in this behavior; another said 81 percent of students who drink heavily had done so. What experts and researchers do agree on is the serious risk posed by the practice. “As soon as this behavior is identified, it could actually be considered a problem,” Hultin says. There’s no safe level of starvation paired with binge drinking.
Glassman and his colleagues are seeking to have drunkorexia — or a more aptly named “alcoholimia” — added as an official diagnosis in the Diagnostic and Statistical Manual of Mental Disorders (DSM), as a subcategory of Other Specified Feeding and Eating Disorders. They hope for guidelines to help practitioners identify the condition in people who engage in high-risk drinking; are very concerned with their body shape; and engage in either laxative use, vomiting, weight control stimulants, meal skipping, food restriction or excessive exercise.
Adding drunkorexia to the DSM would increase the likelihood that a person with this condition can receive insurance coverage for treatment. That’s an important consideration, because treatment may include a costly team approach, including dietitians, psychologists and medical doctors who are able to care for the “dual diagnosis” — involving both an addiction and a psychiatric disorder.
At the University of Toledo, Glassman and his team are trying to prevent drunkorexia with body image education and are raising awareness about the harms of body shaming.
“We try to emphasize that the human body comes in different shapes and sizes, and remind students that when they look at the media, with computer enhancement and airbrushing, even the model may not really look like a model,” Glassman says. “We remind students to value people based on things besides their appearance.”
Their campaign focuses on health factors by reminding students that they only have one body, and it’s time to take care of it instead of abusing or hating or shaming it. “Some students perceive drunkorexia to be harmless when in fact the behavior is extremely dangerous,” Glassman says. “Once they recognize that it’s unhealthy, a lot of students make the decision to change their behavior and get help as necessary.”
Hultin says parents, educators, school counselors and medical professionals can help identify drunkorexia in students, and adds that “if students see friends engaging in this type of behavior, they can intervene and encourage different choices or offer support or resources to address a potential problematic relationship with alcohol and/or food.” Help is always available. An on-campus medical or counseling center is a good place to start.
Registered dietitian Cara Rosenbloom is president of Words to Eat By, a nutrition communications company specializing in writing, nutrition education and recipe development. She is the co-author of “Nourish:
The post What Is Drunkorexia appeared first on Reach Out Recovery.
Media Coverage Of Violent Events Is Found To Fuel A Cycle Of Stress
From the LA Times:
In an era of round-the-clock news cycles and ever-present social media apps, violent events that occur thousands of miles away can feel as though they strike increasingly close to home. So perhaps it should come as no surprise that wall-to-wall media coverage of mayhem can induce post-traumatic stress in those who consume it.
A new study that tracked thousands of Americans after the Boston Marathon bombing in 2013 and the Pulse nightclub shooting in 2016 found that for many who acknowledged initial distress over one of these events, watching lots of news coverage about it was associated with experiencing more post-traumatic stress symptoms six months later.
And that was not the end of their distress. Those who spent more hours engaged with seven different forms of media coverage about one event were more likely to worry over future events. And then, when another national trauma took place, those same people tended to seek out more coverage of it.
The end result of this vicious cycle: deepened levels of distress.
“Distress responses to past large-scale collective traumas (e.g., terror attacks) may sensitize some individuals to media coverage of later collective tragedies, thereby exacerbating distress responses in their aftermath,” the study authors wrote in Wednesday’s edition of the journal Science Advances. “This sensitization process may fuel a cycle of distress.”
And that, the authors added, is a public health issue, since people with post-traumatic stress disorder and chronic distress are more likely to suffer heart attacks, strokes and other cardiovascular problems.
The researchers, from UC Irvine, analyzed the news and social media consumption of 4,165 adults from around the country. They also tracked their psychological states for as long as three years following two major violent events: the Boston Marathon bombings that killed three and injured hundreds, and the mass shooting at Orlando’s Pulse nightclub that left 49 dead and 53 injured.
Six months after the Boston bombings, the amount of media coverage a study participant was exposed to was a good predictor of the number of PTSD symptoms he or she exhibited — including intrusive thoughts or memories about the bombings, hypersensitivity to potentially fearful cues, numbness, and avoidance of reminders. Those with higher levels of media exposure also expressed greater worry about future violent events two years after the bombings occurred.
In turn, after the Pulse nightclub attack, study participants who had high levels of stress and worry about future events were more likely to report both higher levels of media exposure related to the Orlando shooting and more acute stress stemming from the massacre.
It’s widely known that some people are more likely to develop PTSD, including those with a history of depression, anxiety or exposure to violence. But even after accounting for this variation in vulnerability, the UC Irvine team found that more media consumption concerning one event set people up for greater distress, and then for greater consumption of coverage of a later event.
These results are in line with a growing consensus among PTSD researchers, said Dr. David Spiegel, a psychiatrist who directs Stanford’s Center on Stress and Health.
“Exposure to trauma, even at a distance, will elicit the kind of reaction you might have if you are witnessing an event yourself,” he said.
The fact that one is experiencing the events on a screen and is not in immediate danger may mitigate the effects of the sounds, images and vivid accounts of trauma, Spiegel said.
“But we have these big brains that allow us to imagine what it’s like to be there,” he said. When it comes to processing raw images coming across our TVs, laptops and devices, our rich imaginations can conjure very real feelings of immediate danger, he added.
The study authors say their findings hold lessons for news outlets and social media companies, as well as for their audiences.
Media organizations “need to recognize the vital role they can play in broadcasting distress,” they wrote. Amid “pressure to generate clicks and shares,” providers of news-related content should resist the temptations of sensationalism and adopt “a more even-handed” approach, they added.
But news consumers, too, should “understand how they may be putting their long-term mental and physical health at risk by closely following along with collective traumas” as they unfold, the authors added.
Spiegel agreed that news junkies — especially those with a history of trauma — need to be mindful of their propensity to become distressed and limit viewing habits accordingly. And parents should be vigilant about limiting their children’s exposure to the sights and sounds of mayhem.
“Everything in their world is linked to them,” he said. ”So these events get woven into the story of their personal narrative, and that can make it more damaging.”
The post Media Coverage Of Violent Events Is Found To Fuel A Cycle Of Stress appeared first on Reach Out Recovery.





