More on this book
Kindle Notes & Highlights
Read between
September 27 - October 6, 2021
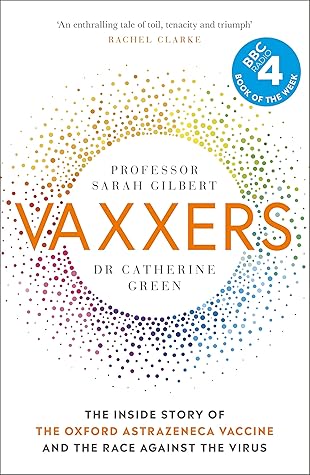
Certainly, fears and doubts often rush in to fill gaps in people’s knowledge. So, we wanted to try to fill in some of those gaps ourselves. What is a vaccine and why do we need them? How do they work? How has it been possible to make them so fast? What is in them? How do we know they are safe?
This book is the story of how two scientists were in the right place at the right time to fight back. We are not ‘big pharma’ or ‘them’. We are two ordinary people who, with a team of other hard-working, dedicated people, did something extraordinary.
At the end of March, just as the entire country went into lockdown for the first time, we heard that my radioactive bid for £2 million from UKRI had been successful. Which was lucky, because we had already spent quite a lot of it.
We were never searching for, hunting for, or, my personal bugbear, finding a vaccine. All year, the papers talked about ‘finding’ a vaccine, as though the thing already existed, maybe in a forgotten freezer somewhere, and our only job was to look hard enough.
we were not completely unprepared: we had been thinking about, and trying to prepare for, Disease X for some time. But one thing we had not thought about was this: how do you fight a pandemic, when you are in a pandemic?
To move quickly, we would still perform all the same tests as usual, we just wouldn’t wait for the results before moving on to the next part of the process. If the starting material failed any of its tests, we would have to throw out anything we had made from it. But that risk – a risk of wasted time and effort and serious money, but not of quality – was one we were prepared to take.
For every vaccine that had ever been developed up until 2020, most of the elapsed development time was spent waiting. In 2020, there were three key factors that enabled us to cut out the waiting and crunch ten years into one: first, the work we had already done; second, changes to the way funding was given out; and third, doing in parallel things that we would normally do in sequence.
Most importantly, we did not need to design, make and test a brand-new vaccine. We had a tried-and-tested platform technology, that we had been working on for years – starting with a flu vaccine back in 2012 and including a vaccine against MERS, another coronavirus. That meant that before we even knew the pathogen’s genome, we knew the design for our vaccine – the gene coding for the SARS-CoV-2 spike protein, plugged into ChAdOx1 – and once we did receive the genome, we were able to design the exact DNA sequence we needed within forty-eight hours.
We were allowed to do a big shop and put all the ingredients we needed in the trolley all at once.
A process that would normally take months – finding the hundreds of volunteers we needed for our first clinical trials – was completed in hours because people were so keen to help. The MHRA prioritised the work they needed to do to review and approve first our trials and later our results, putting us and other Covid vaccines at the front of the queue, bringing in dozens of outside experts to help, and, like us, working long hours, seven days a week.
Before 2020, no one had ever developed a vaccine in a year. But that was not because it could not be done. It was because it had never been tried. We were able to go faster in 2020 not because we cut any corners or took risks with our product. We still did every single thing that needed to be done to develop a vaccine safely. We did not miss out any steps. Nor was any individual task – filling a vial, vaccinating a volunteer, analysing a graph – done with less than the usual care and attention. We went faster because we had to this time – the world needed the vaccine as soon as possible and,
...more
I don’t understand anti-vaxxers. Why would anyone be ideologically opposed to a safe and cost-effective public health measure that saves millions of lives and stops people from having to live with the long-term disabilities that can be caused by diseases such as polio and smallpox – and, it seems, Covid-19?
When using platform technologies such as ChAdOx1 or DNA or mRNA vaccines, rather than starting from the pathogen itself, there is no risk of failing to inactivate the pathogen being vaccinated against (as with the polio vaccine in 1955) or to weaken it sufficiently. The platform technologies increasingly in use in the 2020s are either not live at all, or live but replication-deficient, meaning they can therefore never spread through the body and cause infection and disease.