David Yeung's Blog, page 13
November 8, 2017
Talk on DID in Hong Kong
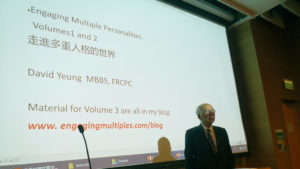
I am in Hong Kong visiting family. While here, I was invited to speak twice this month at the Polytechnic University of Hong Kong about DID. The audience, students working on their masters degree in social work, seemed fully engaged as did the professor who organized the events. I spoke for an hour each time and then answered many questions afterward.
Given that social workers encounter and deal with DID in their profession, it seemed like an important opportunity to bring information about DID to these students. I hope it proves helpful.
The post Talk on DID in Hong Kong appeared first on Engaging Multiple Personalities.
October 19, 2017
Engaging Multiple Personalities Volume 1 in traditional chinese now available
I am very happy to let people know that Volume 1 of Engaging Multiple Personalities is now available in hardcopy and ebook versions.
The hardcopy translation is available at https://www.amazon.com/Engaging-Multi....
The ebook version is available at https://www.barnesandnoble.com/w/enga...
The post Engaging Multiple Personalities Volume 1 in traditional chinese now available appeared first on Engaging Multiple Personalities.
September 24, 2017
Engaging Multiple Personalities Volume 1 now available in Traditional Chinese
I am happy to announce that volume 1 of Engaging Multiple Personalities is available in traditional Chinese through Createspace.com. It should be available through Amazon in the next few days. I hope it is helpful to those who read that language.
走進多重人格的世界
一位華人醫生的臨床手記
The post Engaging Multiple Personalities Volume 1 now available in Traditional Chinese appeared first on Engaging Multiple Personalities.
July 9, 2017
Do Young Alters Need to Age?
A reader of my blog asked me a private question about whether or not alters age (or remain stuck mentally at their age) even though it appears that they are able to do some adult tasks. This is an interesting and important question that I did not address in either Volume 1 or Volume 2 of Engaging Multiple Personalities.
I did not address this question in those volumes because my experience in DID therapy was focused on treating the alters as they presented. My recommendation is always to address the issues that are being presented by the alter or alters that are presenting them. I did not, nor do I recommend, that therapist try to “dig” into the background of a DID patient. In other words, I did not treat each alter as an individual for in-depth psychotherapy. If an alter’s problem was panic with hyper-vigilance, then that was the problem to be treated.
The age of an alter, like the color of a client’s hair, is not a feature we need to focus on. There is no therapeutic advantage in seeking to convert an 4 year old alter into a mature woman of the system’s chronological age, say 40, because the age of the alter is not the problem.
Given that I never sought to help an alter “age” or “mature”, my thoughts on this question are somewhat speculative.
First and foremost, it is quite clear that alters arise as part of the dissociative process in order to allow the system to survive early childhood trauma. However an alter arises, it is tied to that particular trauma. I don’t see why there would be any need for such an alter to age, given that is served and may continue to serve a protective function should the system perceive the same or similar trauma environment. I see every reason for the system to permit the alter to remain as they arose in order to have that mode of dissociative protection available if and when needed.
I do not say that the alters don’t change. It is my experience is that they do change. However, for my patient’s, the alters didn’t change their age. What did change was their ability, with therapy, to remain ever more grounded in the present so as to more properly distinguish danger from the ordinary ups and downs one encounters in life.
In other words, the hyper-vigilance was tamped down. I did not encourage eliminating vigilance as there remain dangers both ordinary and trauma related. It is the hyper-vigilance that was interfering with their life.
Second, I think it is a conceit of those who do not have DID, that have a unitary ego structure, to think that the “correct” or “healthy” result of therapy is that the alters age to the system’s chronological age. It would be far better for therapists to appreciate the brilliance of dissociation as a protective mechanism that arises in the fiery cauldron of early childhood trauma. Knowing its roots in that horrific early childhood trauma, one can have a much deeper appreciation for the strength of the system that enabled survival through dissociation and the consequent alters.
Third, my approach to therapy was always to encourage cooperation among the alters. I think this occurs to some extent all the time, but in times of stress, when unprocessed trauma simply erupts through the appearance of one or more alters, therapy is critical. In DID therapy, we seek to eliminate the internal conflicts that prevent such cooperation. Eliminating the conflicts allows for greater cooperation and a more clear experience of co-consciousness. This limits the hold that the past trauma has on one’s present existence.
In fact, I often encouraged systems to designate alters within that could comfort each other when no therapist is available, to provide an empathetic ear to listen to frightened or angry alters, and to help communicate across amnestic barriers. As cooperation was enhanced, the systems were generally able to use that cooperation as a way to strengthen their ability to remain grounded and healed.”
As their lives become more peaceful (less roller coaster like, and less stormy) the system’s need for different alters to violently seize control, as opposed to cooperatively working with each other, will diminish. We are definitely not asking them to disappear, but they seem to lose the need to insistently take charge. Instead, they will begin to behave in a non-disruptive way.
The post Do Young Alters Need to Age? appeared first on Engaging Multiple Personalities.
June 15, 2017
Resetting the Nervous System after Trauma – Part 2
Levine suggests two very simple physical procedures. One is to ask the client to put one hand in the opposite arm pit, creating a physical sensation of containment of warmth and gentle pressure, directing one’s attention to something immediate, tangible, and palpable in the body. Note that the words are conveying the healing, they are simply directing the client’s attention to feeling their own kinesthetic sense (sense of touch) in their body. Note how much more immediate and real the experience is of such instruction than if a therapist says the words: “try to relax” to the client.
Levine also suggests asking the client to put one hand on their forehead, the other on the chest. Feel the sensation. Or self-tapping their whole body. In general, these techniques help the client to define their bodily boundary which helps them gain a feeling of security.
The practice of tapping, as in the Emotional Freedom Technique, or gently tapping all over the body to provide physical stimulation and redefining physical boundary, creates a gently directed attention to the body in the “here and now” This bypasses the emptiness of words when one is dealing with traumatic memory. Words sound hollow both to the therapist and the client when the therapist speaks to a highly agitated client.
Remember, traumatized clients are on permanent high-alert having been induced to a hyperkinetic state by the traumatic memory. The only way of reaching the psyche of such a client meaningfully is through bringing their attention back to their body.
Alternatively, the therapist could gently push a large cushion against the chest of a client and ask him/her to take a slow deep breath, hold the breath, close the eyes and slowly exhale. Use only a large cushion slowly and gently. This is to ensure that there is no physical miscommunication about the intent of the pushing.
Sometime we therapists overly rely on the use of words. I once used this method on a 59 year old man. It aroused an immediate emotional response and linking to a memory without any verbal intervention on my part. If you can assist a client to get in touch inwards, you don’t have to do a lot of talking in psychotherapy!
If these kinds of exercises are done within a trusting therapeutic relationship, the client cannot escape the physical sensation of gentle pressure against the body. This bodily experience enables them to feel the comfort of relaxation. This is what is meant by grounding, or resetting the nervous system. It is teaching the client the beginnings of re-learning the experiential feelings of comfort and security. The client is induced to re-learn that long lost sensation of good feelings in the body.
I always relied heavily on the therapeutic alliance as a pre-requisite to any procedure in trauma therapy. Then, any instruction was more likely to reach the client physically, rather than merely through words. The simplest way for me to help the client to reach a state of grounding was through that kinesthetic sense, coupled with the attention to the breath.
One key point about breathing is that I never asked my clients to breathe deeply, it seemed too invasive. He/she might end up breathing in too deeply and beginning rapid hyperventilation! If the client was exhibiting agitation, breathing deeply was almost like asking them to breathe back in all the agitation they were putting out into the environment. In fact, they might mistakenly imagine them doing exactly that. The key guidance I chose to give was to ask my clients to breathe “slowly.”
If a therapist is essentially repeating to the client that they need to try to let go and relax, well it simply is not going to work. Give them a path connected to physical sensations they can generate by themselves within their body and you have set them on the course of self-healing. You have given them an understanding of the experience of feeling safe once again – an experience they likely thought would never exist for them again.
I have mentioned aspects of the healing process in various section of my book series Engaging Multiple Personalities. I offer no apology for such repetition because the fundamentals of trauma healing, although quite simple, are very difficult to convey either to novice therapists or to clients.
We must reset the nervous system in relationship to the immediate physical experience of the living body. If we have been grasping a ball tightly, it is not so easy to simply let it go. We have to let go of our grip, muscle by muscle, making sure that we don’t begin to re-grip the ball each time we move to the next muscle. This is what we must teach clients to do with the tight grip with which they are holding their traumatic material. Small step by small step, with ongoing empathy and support, the resetting happens.
The post Resetting the Nervous System after Trauma – Part 2 appeared first on Engaging Multiple Personalities.
Resetting The Nervous System after Trauma Part 1
I have paid close attention to the insights of Peter Levine ever since his book “Waking the Tiger: Healing Trauma” was published. He pointed out that while animals face being hunt down almost on a daily basis, they are virtually immune to traumatic symptoms. With that observation in mind, we have to take a fresh look at trauma healing in human survivors.
Healing involves understanding the role in healing played by bodily sensations, especially in the kinesthetic sensation. Through heightened awareness of these sensations, trauma can be healed. Levine’s approach does not fall into the prevailing practice of over-emphasis on pharmaceuticals even though he considers the problem to be a physical and neurological one.
These are my thoughts concerning his ideas. If there is any confusion or accidental misrepresentation of his work in what I have written, the fault is entirely mine.
The task of the therapist is to help clients by offering them an “island of safety.” It doesn’t have to be a big island, even a very small one is beneficial so long as it is safe. Then, give them a tool so that they can get to that island of safety by themselves. This is accomplished by teaching them self-soothing techniques.
The “island of safety” refers to a palpable, kinesthetic sense of comfort and security; an experience of safety and of being firmly anchored. This must be clearly communicated and demonstrated to the client in therapy so that the therapist conveys the experience, not just the idea.
As survivors of past trauma know, the consequence of the trauma is something that is deeply locked in the body. It is quite different from a conventional understanding of memory, which is narrative. It is unlike the memory of recalling what happened at the ball game yesterday. It is more like a computer that is stuck in a loop and must be re-booted.
“The body keeps the score,” is a phrase emphasized and coined by another trauma specialist, Dr. Bessel van der Kolk. Basically, the body has lost the ability to feel safe. The patient has lost even the memory of what “safe” feels like. This is something that comes up often in therapy.
Therefore, the task in therapy is to help the client to “reset” his or her hyper-alert response. Post trauma, patients are “jumpy” with easily triggered nervous system reactions. With therapy, the patient can realize that it is possible to re-learn and experience safety.
How is this possible? The path to healing is to teach the client that although terrible things did happen in the past, it is possible to experience feelings of safety and joy by living in the present. To a frightened or hurt child, pain and insecurity is felt in the body without narrative memory. The best remedy is to experience the mother (usually but not always) to “physically cradle the child in her loving embrace.”
The cradling by any genuinely protective adult has power. This is how healing is possible. But, as therapists we cannot cradle a patient for reasons that, although obvious, bear repeating:
(1) It is prone to leading to transgressions of the therapeutic boundary.
(2) Our client is not a child, even though the emotional feeling they may express is that of a helpless child.
(3) The therapist, ideally, is teaching the client “to fish” rather than being given a fish as a temporary measure. One aims to teach the client self-healing rather than dependency on the therapist or a pill.
The procedure is teaching the client to generate a sense of self-reliance, of learning what constitutes comfort, security and physical stability. The most immediate goal is to bring the client to the relatively comfortable and secure environment of the here and now through actual experience rather than through words or pharmaceutical intervention.
Words do not create bodily sensations and often run the risk of unknowing retraumatization. I have had patients whose abusers repeatedly used the word “relax” as a prelude to the abuse. For such patients, to suggest that they relax is one of the worst possible thing to say. While retraumatizing words have immediate bodily sensations for the patient, they are the opposite of what you need to convey. They remember the feeling of trauma, they do not remember the feeling of safety. Therefore, mere words are often empty of meaning for patients.
There are medications that can temporarily quell emotional distress. However, there is a clear difference between the actual experience of safety and the experience of suppressing distress through medication. The actual experience is tangible safety. It nourishes the patient and undermines the power of the traumatic events. Quelling the emotional upheaval through medication that suppresses the distress is not the experience of safety. It is simply the apparent absence of upheaval. These are quite different things. I use the term “absence of upheaval” because the distress will re-appear the moment the medication’s suppressive effect weakens.
We must be careful to ensure that our work will not be re-traumatizing, so pre-therapy contracting work is important here. The therapeutic alliance is basic and fundamental to the process. It needs to be cultivated and sustained through empathy, positive regard and congruence.
The post Resetting The Nervous System after Trauma Part 1 appeared first on Engaging Multiple Personalities.
April 17, 2017
Working with Self-Victimization
I received a request from a reader about a major issue encountered by many with DID, self-victimization. In my experience treating DID patients, self-victimization and self-harm seemed to be the rule rather than the exception.
Survivors of early childhood abuse often get attached to successive abusive partners, one after another. It is one of the most unfortunate aspects of the abuse cycle that one goes out to search for an abuser to complete the abuser-victim transaction sketched out in the Karpman Triangle (also known as the Drama Triangle) of the abuser-victim-rescuer socio-gram. Survivors also have similar dynamics within their systems, with different alters playing out similar roles on the inside.
This happens for a variety of reasons, with many different excuses and rationalizations. But rather than respond to the internal logic (or lack of understandable external logic) in the self-harming conduct with arguments, the key point to understand is that healing arises from connecting directly with the alters who are willing to engage, and warmly/gently/kindly inviting others to try to engage.
What does that actually mean? Whether you are seeing a therapist or your have an alter within the system helping out, patiently connecting with a punitive alter (or alters) who wants to inflict pain is critical. Honestly generating empathy for that angry punishing later is key – faking empathy will make things worse. You can generate real empathy by remembering that such alters arose for the same reasons that every other one did – dealing with the direct impact and aftereffects of horrific trauma.
Begin by telling him/her that you understand the feelings of anger, desperation and pain. Be honest if you don’t understand the self-victimization. In that case, you can ask for guidance on how you can better understand his/her view. Gently suggest that the trauma is in the past, but do so by encouraging the alter’s connections with the present. It can be done by identifying the current date. If you are not in the area where the abuse occurred, remind them of where they are right now. My office window overlooked a bridge so I often suggested to my patients that they look at the window and identify that bridge so they could note that the abuse did not occur in this particular city, in this present time.
Physical cues are also helpful. By asking him/her to take a deep breath with you, he/she may then experience even a moment of distance from that traumatic experience. Again, it is encouraging the realization that the trauma can be viewed from a distance in time and space. In other words, it is inviting the experience of safety in the present. It is putting the flashback where it belongs – in the past. It is a memory, not a current experience even though it seems like it is happening now because your body is having the same response of fear, panic, hyper-vigilance and a pounding heart. This is the therapeutic process of disengaging from a flash back.
It is just as important to connect with the alters that are being harmed inside – not just the ones doing the harm. Remember that while some alters seek to do harm, others feel the need to be harmed. It may be phrased by those alters that they deserve to be harmed or that there is no other option. Both need empathy, compassion and understanding as well. Within an environment of understanding, empathy and compassion, the suffering alters will be able to make a shift.
Help those alters in conflict find a safe place to process and heal the wounds. Encourage others in the system to help modulate the conduct of the angry harmful alters, to become their friends. Encourage those that are being victimized inside to connect with other parts of the system that can act as their protectors – not from the point of view of fighting with the other angry alters but rather as a bridge to understanding each alters particular suffering, generating empathy for each other and a spirit of healing teamwork.
For example, the soft and comforting voice of the therapist, or your self-appointed internal therapist, can shift the alter who is still stuck to the past traumatic experience back into the present moment of safety. The pathology is that the particular alter will remain tenaciously stuck to the past trauma. The therapist, no matter from inside or outside, has to persevere to achieve a small, step-by-step separation from the past trauma into the present. It is difficult but this is often the very central central practice in DID therapy.
I want to be quite clear that in this I am directly addressing an alter, treating him/her as my client and giving them my full attention. Some therapists prefer to speak only to the host. In fact, colleagues have criticized my approach as reinforcing the splitting aspect of DID pathology. As I have written elsewhere, fish swim, they are not taught to swim. In that same way, DID individuals dissociate, they are not taught to dissociate. For fish, to swim is instinctual. For DID individuals, to dissociate is similarly instinctual – it is their instinct for self-preservation in the context of massive early childhood trauma.
In my experience, a large part of DID therapy is one-on-one psychotherapy directed to individual alters. If you have an internally appointed self-therapist, working as an adjunct to your therapist or alone because you are unable to find a therapist, one can encourage the same approach of communication between the inner therapist and the self-abuser. Knowing that the self-abuser is acting out unprocessed trauma allows one to communicate always with respect and always with kindness.
[The Karpman Triangle is found on page 126 of Engaging Multiple Personalities Vol 1. It is also displayed by Joan, in Chapter 1, who struggled with this almost every night for months.]
The post Working with Self-Victimization appeared first on Engaging Multiple Personalities.
April 13, 2017
How To Worry Constructively – Part 2
It is clear that some worries are helpful while others are not. Let’s call the first group “constructive” and the second “destructive.” When worrying is helpful, justified in the circumstances, it is constructive. When worrying is not helpful, not justified in the circumstances, it is destructive.
We often cannot separate one from the other. But, we need to distinguish them for our own well-being. So, it is important to learn how to determine whether or not our worry is constructive.
When a patient came to see me about his paralyzing anxiety, I applied the paradoxical intention concept as used in logotherapy, developed by Victor Frankl. I asked him to sit still for a few minutes before telling me all the things that were bothering him. I asked him to prepare himself by organizing his thoughts and reviewing what was bothering him. In other words, I was asking him to allow his worrying to come out without contesting it.
As a result of my request, he gave himself permission to worry. First, appearing somewhat subdued and dull, he sit down. Then, he focused on the issues of concern without the internal turmoil of worrying about the fact that he was worrying. After a few minutes, he opened his eyes and said that what he was worrying about turned out to be of no real significance. To my surprise, he did not even think he needed to tell me about it further! His body language clearly indicated that his mind was lighter, unburdened by the anxiety. Simply allowing his worry to come out in a safe environment had empowered him to solve his difficulty with no other assistance.
Mind you, there were important factors at work in the interaction. Remember, the therapist’s communication in non-verbal language way can carry as much weight, if not more, than the spoken word. So, my body language and verbal communication were in accord with each other – entirely respectful, rather than being dismissive of his concern. It was clear that I took his complaint seriously.
My interpretation of this event was that when he was encouraged to go ahead and explore his concerns in a safe and nurturing environment, he was free from the paralysis of being unable to determine whether he should or should not worry. Without that internal tug of war, without that self-criticism, he was able to focus on and process his concerns without getting in his own way.
Sanjay Gupta, CNN’s chief medical correspondent (and a board certified neurosurgeon) documented the meditation instruction he received on worrying from the Dalai Lama. The Dalai Lama taught him to meditate by focusing on his worry while imagining it isolated in a bubble. He did that for a few months and vouched for it having changed his life in a significant way. This simple and effective instruction may be another practical way to work with worrying about life’s challenges.
http://www.cnn.com/2017/02/15/health/...
The post How To Worry Constructively – Part 2 appeared first on Engaging Multiple Personalities.
How To Worry Constructively – Part 1
In life, one experiences alternating and sometimes mixed emotions of joy and sadness as well as of carefree laughter and deep frowning concerns. While joy and laughter are seldom experienced as problems, when something in your environment triggers an internal alarm, you will start to worry. Worrying can encourage you to focus energy for a task at hand, in problem solving, or in securing a needed level of certainty. However, when worry gets out of control and results in persistent anxiety, loss of sleep and/or ongoing increased blood pressure, it is no longer helpful. At such a point, it no longer helps you achieve a goal. Instead, it self-perpetuates in a seemingly endless loop of stress.
Nowadays, there is a tendency to see every ordinary emotional up and down as a kind of pathological disorder in need of treatment. If you present concerns about your emotions to a busy doctor, it is likely that a magic pill will be prescribed “to take the edge off” whatever worries you.
In DID, worrying can transform into an almost perpetual anxiety, which may then get taken to the extreme of crippling hyper-vigilance. Psycho-active medications can be very helpful when worrying has become incapacitating anxiety. Nevertheless, thoughtlessly employing medication may mean that we miss out on opportunities to mature, to grow stronger and to become more self-reliant. My recommendation was always to include psychotherapy as part of any regimen that included psycho-pharmaceuticals.
But, are all kinds of worrying pathological? No.
If your teenager is going out with friends, you may worry and automatically look for specific danger signals. If the driver has had a couple of beers, then your worry crystallizes – you identified a true predictor of the risk of catastrophe. You may need to actively intervene as a result of this clear and present danger.
Your worry in that example is clearly not pathological. It is a sane response to evaluate known risks of danger. Once we have scrutinized the situation, and ensured that the driver is not drinking then the worry has resulted in reasonable actions of protection. At that point, continuing to worry is a waste of energy.
Having taken reasonable precautions, remaining paralyzed with disabling worries fits into the psychiatric category of “Anxiety Disorder.” If that is the case, then yes, you have an Anxiety Disorder. This leads to follow-up questions, “Are drugs are the only treatment? Are they necessary?”
When necessary, I sometimes prescribed medication but only as an adjunct to psychotherapy. A principal argument against pharmacological treatment alone is that while drugs can ease your mental tension for a short period of time, they take away your autonomy and the possibility of self-empowerment. Taken alone, medications can lead you down the path of chemical dependency.
Training yourself to deal with tension solely with medication does not allow for correcting and refining the balance of your innate alarm system or for modulating your responses to those alarms as appropriate. For example, if you hear a car horn honk some distance away, you notice the sound and scan to identify what is going on. You do not jump and run in a panic. If you are jay-walking and you hear a car horn honk very close, then the appropriate response may indeed be to jump and run out of the way.
Life is full of obstacles for everyone. You will likely meet situations in the future that are similar to what is triggering the anxiety. Relying solely on medication without embarking on the necessary internal re-calibration work of psychotherapy, brings only an even stronger reliance on the drug! It is like starting on sleeping pills to put you back to normal sleeping pattern. Once you find them helpful, you start worrying that you will need them again. But this time the worry is truly justified! Why? Because you have not used the situation to learn about and process the root causes of the obstacle you face. This is the task, this is the essence of the healing journey.
The post How To Worry Constructively – Part 1 appeared first on Engaging Multiple Personalities.
March 29, 2017
Anxiety – Part 3 Meditating on Anxiety
Sanjay Gupta, the CNN Chief Medical Correspondent who is also a neurosurgeon, documented the personal instructions on meditation that Dalai Lama’s gave to him. The Dalai Lama taught him to meditate by focusing on his worry while imagining isolating it in a bubble. He did this as a daily practice of meditation for a few months and vouched for it having changed his life in a significant way. By putting his worries in a bubble, he allowed himself to worry, but in a way that did not generate a vicious self-perpetuating cycle. With this approach, the worry does not get worse. It can either stay the same or get better. If the worry is inappropriate or disproportionate, it will not only get better by having you see it in a more reality based perspective.
http://www.cnn.com/2017/02/15/health/...
One of the worst aspects of anxiety is that it has an all-pervasive quality. So-called “free-floating anxiety” is everywhere which means that one can find it hard to pin-point anything about it. What I sometimes asked my patients to do was to use their imagination to put the anxiety onto some part of their body, such as the chest, or their abdomen. It is like finding a location or a point that enabled them to keep the anxiety in one place. I suggested that they continue, gently but steadfastly, to focus on this point, to look at it and feel it. I encouraged them to keep returning to it if their mind wandered off. I sometimes asked them to move the anxiety just a bit with their breathing; an inch here or there.
Once you’ve localized some anxiety, just breathe and feel it. Treat it like your friend, stay with it through thick or thin. You can even begin to play with it!
Keep breathing, and keep practicing just accepting this feeling of anxiety – kind of like accepting the feeling of the weight of your pillow on your abdomen. If the sensation of anxiety starts to fade, bring it back and accept it. Simply stay with the anxiety instead of trying to get rid of it or fight with it. Treat it as your friend. Eventually, almost everyone ends up having difficulty maintaining the anxiety.
Call it whatever name you like. Some call it “paradoxical intention”, some call it “reverse psychology, some call it “mindfulness practice”. Whatever you call it, it is a way to empower yourself to work with anxiety rather than being disabled by it.
I do not rule out that in special circumstances, medicine may still be justified. However, it must not be given without considering all the alternatives – including using medication as a support for the kinds of self-empowering practices described previously in Part 1 and 2. It is far better to begin to learn how to heal yourself rather than giving up the autonomy which is your own power, and blindly trusting chemicals alone.
The post Anxiety – Part 3 Meditating on Anxiety appeared first on Engaging Multiple Personalities.
David Yeung's Blog
- David Yeung's profile
- 5 followers



