Mathea Ford's Blog, page 42
June 22, 2023
Is Star Fruit Bad For Kidneys
Star fruit is a unique and nutritious snack that can make a flavorful addition to any diet. But if you have kidney disease, star fruit can be dangerous and even deadly.
It looks and sounds like an innocent and tasty option for to add in your fruit basket, fruit salad, or summer drink, but it is actually a very dangerous and toxic substance that can cause a disturbance in patients who have kidney disease.
It's ingestion is prohibited for those who have kidney issues due to the presence of two dangerous and life-threatening neurotoxins and nephrotoxins present in the tropical fruit.
In this article, we'll explore the potential effects and risks of star fruit for individuals with kidney disease. We'll discuss the role of oxalic acid and caramboxin, and the science behind star fruit toxicity, and the common symptoms of star fruit intoxication. We'll also provide information about alternative fruits that are safe for kidney health.
By the end of this article, you'll have all the information you need to make an informed decision about whether or not to include this fruit in your diet.
[feast_advanced_jump_to]Key Takeaways Star fruit contains oxalic and caramboxin acids, which can be fatal if accumulated in the blood of renal patients.Star fruit ingestion is prohibited for those who have kidney disease as it worsens or can cause star fruit induced acute renal failure or acute kidney injury.Apples, pineapples, pears, and citrus fruits are safe alternatives for those with kidney disease.This fruit can cause neurotoxicity and nephrotoxicity in those with damaged kidneys, which can be life-threatening.
Star fruit contains oxalic and caramboxin acids, which can be fatal if accumulated in the blood of renal patients.Star fruit ingestion is prohibited for those who have kidney disease as it worsens or can cause star fruit induced acute renal failure or acute kidney injury.Apples, pineapples, pears, and citrus fruits are safe alternatives for those with kidney disease.This fruit can cause neurotoxicity and nephrotoxicity in those with damaged kidneys, which can be life-threatening.The Intriguing World of Star Fruit: A Brief OverviewFor More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
Star fruit is a bright and interesting fruit that is native to tropical regions of Southeast Asia including Sri Lanka and South America including Brazil. Also known as Averrhoa carambola (A. carambola) or Carambola, it has an edible skin and, when cut into slices, resembles a five-point star. It is sweet, sour, and has a somewhat citrus-like flavor.
They come in yellow or green colors, and are sweeter in their larger variety, with smaller versions of the fruit retaining a sour taste, much like a lemon. While it has gained popularity all over the world for its fun shape and uses, regardless of the type of star fruit, the effects of star fruit can be life-threatening to those with damaged kidneys or those who have trouble filtering out toxins.
While star fruit contains many important nutrients and has a range of culinary uses, it is important to be aware of its potential dangers for those with kidney disease. Star fruit is a good source of fiber and vitamin C, as well as several antioxidant compounds. The ripe fruit is also low in calories, making it a great snack option for those watching their weight.
However, this fruit is also rich in oxalic acid and caramboxin acid, which can be fatal if accumulated in the blood of renal patients. These toxins can be obtained from ripe and unripe star fruit, star fruit juice or carambola juice, star fruit extracts, extract from leaves of star fruit, and other forms of which it may be prepared.
Patients with chronic kidney disease should avoid ingestion of star fruit and consult with their doctor before trying it.
It is also important to remember that star fruit should always be consumed in moderation. excessive consumption can lead to life-threatening neurotoxins and nephrotoxins. For those with healthy kidneys, however, star fruit can be a tasty and healthy addition to their diet.
Potential Risks for Individuals with Kidney Disease: CaramboxinConsuming star fruit can be dangerous for individuals with kidney disease, especially those with chronic kidney disease (CKD). Star fruit contains a harmful substance called caramboxin, which is not properly eliminated by the kidneys in people with kidney problems. This can lead to increased levels of caramboxin in the body, allowing it to affect the brain and nervous system.
The caramboxin toxin can cause excitability, seizures, and damage to the nerves. It interferes with the normal communication between brain cells, leading to problems with brain function. People with kidney disease who eat star fruit may experience symptoms like hiccups, vomiting, confusion, agitation, and even prolonged seizures. In severe cases, it can even be life-threatening.
The risk comes from a toxin in star fruit called caramboxin, which affects the brain and nervous system. The toxin can't be properly eliminated by the kidneys in people with kidney disease, so it builds up in the body and causes harm.
It's important for healthcare professionals, especially nutritionists, to warn patients with kidney disease about the dangers of eating star fruit. Even people with normal renal function should avoid it, as it can still be harmful.
Overall, it's best for individuals with kidney disease to stay away from star fruit completely. The potential risks outweigh any potential benefits. If you have any concerns or questions about your diet and kidney health, it's important to speak with your healthcare provider for personalized advice.
The Role of Oxalic AcidOxalic acid is a substance found in star fruit that can have an impact on kidney health. When we consume this fruit, the oxalate content in it can cause problems for some people. In certain individuals, eating this fruit can lead to issues with the kidneys, known as star fruit nephrotoxicity.
The nephrotoxic effect means that the oxalic acid in star fruit can cause harm to the kidneys leading to acute oxalate nephropathy. It can lead to the deposition of calcium oxalate crystals in the tiny tubes within the kidneys. This can then cause damage to the kidney tissue, leading to conditions like acute kidney damage, acute tubular necrosis, and interstitial nephritis.
Acute tubular necrosis is a condition where the cells in the kidney tubules die, which can disrupt the normal functioning of the kidneys. Interstitial nephritis is inflammation that occurs in the spaces between the kidney tubules. Both of these conditions can affect the kidneys' ability to filter waste products from the blood and maintain the right balance of fluids and electrolytes in the body.
In addition to oxalic acid, star fruit also contains another substance called caramboxin, which can contribute to both kidney and neurotoxicity. Neurotoxicity refers to the harmful effects on the nervous system. In some individuals, consuming star fruit can lead to neurological problems like seizures and confusion.
It's important to note that not everyone will experience these issues when eating star fruit. However, for individuals who already have kidney problems, such as chronic kidney disease, or are at risk of developing kidney stones, it's best to avoid or limit the intake of star fruit. This is because the oxalic acid in star fruit can increase the risk of further kidney damage.
Ultimately, it's important to remember that star fruit ingestion must be consumed in moderation to avoid potential kidney damage. As always, it's best to consult with a healthcare professional before consuming star fruit to prevent any potential side effects.
Understanding the Impact of Star Fruit Consumption on Kidney FunctionUnderstanding the impact of star fruit consumption on kidney function is critical for those with existing renal impairment, as it can cause life-threatening neurotoxins and nephrotoxins. It is important to understand the risks, prevention measures, nutritional benefits, safe alternatives, and medical recommendations for those with or without kidney damage.
The presence of oxalic acid and caramboxin acid in star fruit can accumulate much easier in the blood of CKD patients and can cause rapid deterioration of the brain and kidneys. The table below provides an overview of the risks associated with star fruit consumption:
RisksPrevention MeasuresAcute kidney injury (AKI)Avoid eating star fruitChronic kidney disease (CKD)Consult a healthcare professional firstNeurotoxicity and nephrotoxicityEat in moderationFull renal failureChoose safe alternatives such as apples, pineapples, pears, and citrus fruitsStar fruit can provide nutritional benefits such as vitamin C, fiber, and antioxidants. However, those with kidney damage should avoid star fruit, as even a small amount can cause lethal and toxic effects. Medical professionals should advise patients with CKD or those on dialysis to avoid eating star fruit. Hemoperfusion may be an effective alternative therapy for chronic renal disease patients with severe star fruit poisoning.
Why Renal Health Professionals Advise Against Star FruitStar fruit, also known as carambola, offers several nutrients that can be beneficial for overall health. In a single, medium-sized fruit weighing approximately 91 grams, it provides the following nutrients:
Fiber: There is about 3 grams of fiber in star fruit, which helps support digestive health and can contribute to feelings of fullness.Protein: With 1 gram of protein per medium sized fruit, star fruit is a decent source of protein for the body's need for this essential macronutrient.Vitamin C: Star fruit is particularly rich in vitamin C, providing 52% of the Recommended Daily Intake (RDI). Vitamin C is an antioxidant that supports immune function, collagen synthesis, and iron absorption.Vitamin B5: Star fruit contains 4% of the RDI for vitamin B5 (pantothenic acid), which is involved in energy metabolism and the synthesis of hormones and cholesterol.Folate: With 3% of the RDI for folate, this fruit contributes to DNA synthesis and cell division, making it important for growth and development.Copper: The fruit provides 6% of the RDI for copper, which is involved in the production of red blood cells and the maintenance of healthy connective tissues.Potassium: Star fruit contains 3% of the RDI for potassium, an essential mineral that plays a crucial role in maintaining fluid balance, nerve function, and muscle contractions.Magnesium: With 2% of the RDI for magnesium, star fruit contributes to various physiological processes, including muscle and nerve function, blood sugar regulation, and bone health.Despite these nutritional benefits, renal health professionals advise against star fruit consumption for individuals with kidney disease. As mentioned, star fruit contains oxalic acid and a neurotoxin called caramboxin.
In people with kidney disease, these substances can have harmful effects on the kidneys and nervous system. Oxalic acid can contribute to the formation of kidney stones or worsen existing kidney stone conditions. Caramboxin, when not properly eliminated by impaired kidneys, can accumulate in the body and lead to neurological complications, such as seizures and confusion.
To prioritize kidney health and minimize potential risks, it is recommended that individuals with kidney disease avoid consuming star fruit and consult with healthcare professionals for personalized dietary guidance.
Common Symptoms of Star Fruit Intoxication in Kidney Disease PatientsStar fruit intoxication can lead to various symptoms in individuals with kidney disease. It's important to be aware of these symptoms to recognize and seek medical attention promptly. Some common symptoms of star fruit intoxication in kidney disease patients include:
Hiccups: One of the early signs of star fruit intoxication is persistent hiccups. Kidney disease patients who have consumed star fruit may experience frequent and prolonged bouts of hiccups.Vomiting: Nausea and vomiting are common symptoms that can occur as a result of star fruit toxicity. These symptoms may persist and can be severe in some cases.Mental Confusion: Star fruit intoxication can affect brain function, leading to confusion, disorientation, and cognitive impairment. Kidney disease patients may experience difficulties with memory, concentration, and decision-making.Agitation: Restlessness, irritability, and agitation can be observed in individuals with star fruit intoxication. These behavioral changes may be accompanied by anxiety or a sense of unease.Seizures: Star fruit toxicity can trigger seizures in some cases. Kidney disease patients may experience involuntary muscle contractions, convulsions, and altered consciousness during a seizure episode.Altered Consciousness or Consciousness Disturbance: In severe cases, star fruit intoxication can lead to a decreased level of consciousness or even coma. This can manifest as drowsiness, lethargy, or unresponsiveness.It's important to note that the severity and combination of symptoms can vary among individuals. Some individuals may experience only a few mild symptoms, while others may develop more severe and life-threatening complications.
If kidney disease patients experience any of these symptoms after consumption of star fruit, it is crucial to seek immediate medical attention for proper evaluation, diagnosis, and appropriate management. Prompt recognition and medical intervention are vital to ensure the best possible outcome and prevent further complications associated with star fruit intoxication in individuals with kidney disease.
Star Fruit and Dialysis: A Complex RelationshipThe relationship between star fruit consumption and dialysis is complex. Star fruit contains substances that can be harmful to individuals with kidney disease, particularly those on dialysis. The neurotoxin and high oxalic acid content in star fruit can lead to complications such as oxalic acid intoxication, neurological symptoms, kidney stone formation, and exacerbation of kidney damage.
Due to these risks, individuals on dialysis are typically advised to avoid consumption of star fruit. It is essential for dialysis patients to follow a renal-friendly diet and consult with their healthcare team, including nephrologists and dietitians, for personalized dietary guidance to ensure optimal kidney health.
As a person with kidney disease, you must be aware of this complex relationship between star fruit and dialysis. Here are four key points to keep in mind when managing star fruit toxicity in kidney disease patients:
Dietary alternatives to star fruit should be considered for renal patients. Apples, pineapples, pears, and citrus fruits are safe alternatives.Star fruit ingestion is prohibited for those with kidney disease as it can cause lethal and toxic effects.Hemoperfusion may be an effective alternative therapy for chronic renal disease patients with severe star fruit poisoning.Always consult a healthcare professional first to prevent any star fruit intoxication.Star fruit intoxication can be life-threatening. The buildup of toxins in the blood can cause acute kidney injury, neurological disorders, and death. It's important to understand the risks associated with star fruit consumption and to know the dietary alternatives to avoid intoxication in patients with renal impairment.
Also, it's essential to consult a healthcare professional before consuming star fruit to ensure that it's safe for you to consume. Taking all of these factors into consideration is crucial for managing intoxication by star fruit in kidney disease patients.
Alternative Fruits Safe for Kidney Health: SubstitutesFor those with impaired kidney health, there are numerous alternatives to star fruit that can provide delicious, nutritious snacks without the risk of star fruit nephrotoxicity. Apples, pineapples, pears, and citrus fruits are all safe to consume and provide various nutritional benefits.
Below, we will discuss a few alternatives that have somewhat similar flavors to the fruit, without the unnecessary risk that comes from ingestion of star fruit.
AppleApples are one of the healthiest and most renal-friendly fruits. They are also very diverse and a rich source of protein that can be used in various desserts and paired with things like peanut butter for a protein-rich snack. They have a lighter and sweeter flavor than star fruit, but their versatility makes them the perfect snack.
PineapplesPineapples are quite tropical, like the star fruit, and have a bit of tangy acidity as well. They are a great choice for a similar flavor profile that isn’t in the citrus family, and pineapples make for great additions to smoothies or creating pineapple juice in a juicer.
PearsPears have a much more subtly sweet flavor and are more comparable to apples than the star fruit, but it is an interesting and delicious snack option for those craving a bit of variety among their fruit choices.
Citrus fruitsAre likely the closest on this list in terms of flavor comparisons to the star fruit, but members of the citrus family are safe for CKD patients to consume without worry. Much like the starfruit, grapefruits, oranges, kumquats, and other members of the citrus tree all have a tangy, somewhat sour, and at times bitter quality to their taste which encompasses many of the star fruit flavors as well. So, if you are feeling hungry for star fruit, turn to any of the citrus family instead, and they should definitely fill that void of flavor and promote normal kidney function for those with renal disease.
Frequently Asked QuestionsHow much star fruit can I safely eat if I have kidney disease?If you have kidney disease, it's important to be mindful of your eating habits and make dietary changes to improve your health. Star fruit should be avoided by those with impaired kidney function due to the presence of oxalic and caramboxin acids. Eating even a small amount of star fruit can be dangerous, even deadly, and can cause persistent hiccups, seizures, and death.
To ensure kidney health, it's recommended to avoid star fruit and opt for other alternatives, such as apples, pineapples, pears, and citrus fruits. It's also important to maintain adequate hydration levels and make mindful food choices.
Always consult a healthcare professional to discuss dietary changes and to prevent any star fruit intoxication.
There is currently no specific antidote or treatment for star fruit toxicity. The management of star fruit toxicity involves supportive care and addressing the symptoms experienced by the individual.
In cases of severe toxicity, immediate medical attention is crucial. Medical professionals may provide measures such as intravenous fluids, antiemetics to control vomiting, anticonvulsants for seizures, and supportive measures to maintain kidney function.
Hemodialysis or hemoperfusion may be necessary in severe cases to help remove the toxins from the bloodstream. It is important for individuals who suspect star fruit toxicity or have consumed star fruit and are experiencing symptoms to seek medical assistance promptly for appropriate evaluation and management.
Long-term effects of star fruit consumption can be detrimental for individuals with kidney disease. The oxalic acid and neurotoxin present in star fruit can lead to the formation of kidney stones, worsening of existing kidney stone conditions, and damage to kidney function. Neurological complications, including seizures and cognitive impairment, may also occur.
In severe cases, long-term consumption of star fruit can have a lasting impact on overall kidney health and neurological well-being. Therefore, individuals with kidney disease are strongly advised to avoid star fruit consumption to prevent potential long-term complications and to prioritize their kidney health.
While star fruit is a fruit that individuals with kidney disease should avoid, there are a few other fruits that may need to be limited or avoided due to their potassium content. High-potassium fruits such as bananas, oranges, kiwis, and dried fruits like raisins and prunes are typically recommended to be consumed in moderation for individuals with kidney disease.
However, the exact dietary recommendations may vary depending on the individual's specific condition and the stage of kidney disease. It is essential to work with a healthcare professional, such as a registered dietitian, who can provide personalized dietary guidance based on the individual's needs and kidney function.
Yes, there are other health benefits associated with star fruit consumption. Star fruit is a great source of nutrition, containing high levels of vitamins A and C, as well as potassium and dietary fiber.
In some cultures, star fruit is used for medicinal purposes, such as treating fever and indigestion. There are various ways to cook and prepare star fruit, so it can be a versatile and tasty addition to any meal.
Despite these potential benefits, CKD patients must always be mindful of their consumption of this fruit as the risks may outweigh the benefits.
You have to be careful when it comes to star fruit and kidney health. While it's a nutritious snack with many potential benefits, it can be dangerous for those with kidney disease.
Oxalic acid can cause kidney toxicity and even neurotoxic effects in these individuals. It's best to avoid star fruit if you have kidney disease, and if you must consume it, be sure to monitor your health closely.
There are many other fruits that are safe for kidney health, so you don't have to miss out on the nutritional benefits of star fruit. Remember to always consult with your doctor before eating any new food when you’re on a renal diet.
The post Is Star Fruit Bad For Kidneys appeared first on Renal Diet HQ.
Suggested Reading:
Early Stage Kidney Disease The Importance Of Diet For Stage 3 Chronic Kidney Disease Stage 4 Kidney Disease DietJune 21, 2023
Mindful Eating Tips For A Renal Diet
Are you one of the millions of people with kidney failure who struggle to maintain a healthy diet? The importance of a renal diet cannot be overstated, as what you eat can significantly impact your health and well-being.
Unfortunately, many comfort foods that we turn to in times of stress are often high in sodium, potassium, and phosphorus - all things that can negatively affect people with kidney disease.
But don't despair! There is hope for those looking to improve their renal diet through mindful eating practices.
Mindful eating involves being present and aware while consuming food, which can help you make better choices and avoid emotional eating habits, as well as watch your dietary intake improve through thoughtful decisions about what to eat.
In this article, we will explore the benefits of mindful eating for a renal diet, as well as provide tips on how to incorporate it into your daily routine and maybe even affect your calorie intake.
So let's get started on your journey towards healthier living!
[feast_advanced_jump_to] Key TakeawaysMindful eating can help people with kidney disease focus on the sensory experience of eating and combat mindless eating.Identifying emotional triggers and practicing self-awareness techniques can help avoid unhealthy cravings and emotional eating.Hydration is critical for maintaining healthy kidneys and preventing complications related to chronic kidney disease.Meal planning and preparation in advance, as well as consulting with a registered dietitian who specializes in renal diets, can ensure balanced and nutritious food options that align with health goals.
Key TakeawaysMindful eating can help people with kidney disease focus on the sensory experience of eating and combat mindless eating.Identifying emotional triggers and practicing self-awareness techniques can help avoid unhealthy cravings and emotional eating.Hydration is critical for maintaining healthy kidneys and preventing complications related to chronic kidney disease.Meal planning and preparation in advance, as well as consulting with a registered dietitian who specializes in renal diets, can ensure balanced and nutritious food options that align with health goals.Importance of Renal DietFor More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
If you're living with kidney disease, it's crucial to understand the importance of following a renal diet. This type of diet is designed to help protect your kidney health by managing your dietary restrictions and ensuring proper nutrient balance. Sticking to a renal diet can also help you maintain adequate hydration levels, which is essential for optimal kidney function.
One of the main benefits of following a renal diet is that it helps manage the amount of certain minerals and nutrients in your body. For example, if you have high levels of potassium or phosphorus in your blood, a renal diet can help lower these levels and prevent complications.
However, it's important to remember that this type of diet should be followed under medical supervision to ensure that you're getting all the necessary nutrients while avoiding foods that may be harmful for people with kidney disease.
Another important aspect of a renal diet is hydration. Drinking enough water and fluids is critical for maintaining healthy kidneys and preventing complications related to kidney disease. Your healthcare provider will likely recommend specific fluid intake guidelines based on your individual needs and health status.
It's important to follow these guidelines closely to ensure adequate hydration without overloading your kidneys with excess fluids.
Adhering to a renal diet can be challenging but is essential for maintaining optimal kidney health when living with kidney disease. By focusing on nutrient balance and proper hydration under medical supervision, you can help preserve your kidney function and prevent complications associated with this condition and other chronic disease. Remember to work closely with your healthcare team when designing an appropriate meal plan tailored specifically for your unique needs!
What is Mindful Eating?Mindfulness refers to being in the moment and aware of what is going on. As far as mindful eating, it’s all about paying attention to the foods you are choosing, the portion sizes you are filling up your plate with, and how these foods affect your mind, body, and mood.
When you are eating mindfully, you’ll notice you are making the best decisions for following your renal-friendly diet. You won’t have to worry so much about getting too much potassium or phosphorus – two minerals you need to be careful of when suffering from chronic kidney disease – since you will be choosing the right healthy foods based on the renal diet your doctor has given you.
Unhealthy Comfort FoodsYou may find yourself turning to certain foods for comfort, but it's important to be aware that some of these options can have negative effects on your health. Unhealthy cravings often arise from emotional triggers such as stress, boredom, or anxiety.
Comfort eating habits can lead to overeating and weight gain, which is particularly detrimental in the case of a renal diet. One way to combat unhealthy cravings is by identifying alternative options that satisfy both your taste buds and nutritional needs.
For example, instead of reaching for chips or cookies, try snacking on fresh fruit or vegetables with hummus. Additionally, paying attention to portion sizes can help you maintain a balanced diet while still enjoying the foods you love.
It's important to remember that breaking old habits takes time and effort. Don't be discouraged if you slip up occasionally - it's natural! Instead, focus on incorporating healthier choices into your daily routine and gradually reducing reliance on comfort foods.
With practice and dedication, mindful eating can become second nature and ultimately improve your overall well-being.
Benefits of Mindful EatingImagine savoring every bite of your meal, noticing the flavors and textures, and feeling satisfied with just the right amount - this is the beauty of tuning into your body's hunger and fullness cues through mindful consumption.
Mindful eating is a practice that involves paying attention to what you eat, how you eat it, and why you eat it. It can have numerous benefits for those following a renal diet. Here are three reasons why incorporating mindful eating into your renal diet can be beneficial:
Improved digestion: When we eat mindfully, we take our time to chew our food properly, which aids in digestion. This can help reduce symptoms such as bloating, gas, and constipation.Better food choices: Mindful eating encourages us to choose foods that nourish our bodies rather than simply satisfying cravings or emotional needs. By being more aware of what we're putting into our bodies, we're more likely to make healthier choices.Increased satisfaction: By taking the time to savor each bite and truly enjoy our meals, we feel more satisfied with less food. This can help prevent overeating and promote weight loss.Incorporating mindfulness into your eating habits may also reduce stress levels by allowing you to focus on the present moment rather than worrying about past or future events while eating.
Overall, practicing mindful eating can lead to a happier and healthier relationship with food while keeping your kidneys healthy.
Mindful Eating Tips for Following your Renal DietAssess your mood at mealtime: Comfort foods are likely your renal diet’s worst enemies. They usually aren’t healthy, and more often than not, they are on your food restriction list. These typically include foods that are loaded with carbs and sugar, such as cookies, cake and chocolate.
While these items may be okay in moderation, if you are mindlessly eating them to feel better, forget the sadness, or to reduce stress, you are putting your health at risk. Rather than grab the sweetest item in the store when you are feeling down, find other ways to handle your emotions, including yoga, walking, or talking to someone.
Turn off the television: Eating while you watch your favorite show is the easiest way to eat mindlessly. You won’t realize how much you have eaten, and you can totally blow your renal diet out of the water if you are occupied while you snack. Be sure to put all electronic devices, books, and magazines away while you eat, so you can focus on the task at hand and be more mindful with your eating.
Keep a food journal: Reflect on your meal choices each day. Note the amount of food you are eating, and what ingredients they contain (especially important if you are limiting nutritional intake of sugar, potassium, phosphorus, or other nutrients). This written account of your daily diet will show you where you need to make better choices, or where you need to keep up the good work!
Learn portion control: Many people do not know true portion sizes when it comes to eating meals. They lob spoonfuls of meat and sides onto their plate until it’s full before sitting down to eat. However, portion control is a VERY essential part of mindful eating. When you know how much is “enough,” you’ll be able to better follow your renal diet.
Keep healthy choices on hand: When you don’t have any unhealthy or restricted food in your home, you won’t be breaking your diet rules! Healthy snacks already properly portioned in storage containers or Ziploc bags make it easy to eat mindfully. Preparation is key in following your renal diet!
Risks of Mindless EatingBe aware of the risks of mindlessly consuming your meals, as it can lead to overeating and poor digestion, leaving you feeling sluggish and uncomfortable. Mindless eating occurs when we consume food without paying attention to our body's cues for hunger and fullness. It's often caused by distractions such as watching TV or using electronic devices while eating.
The consequences of mindless eating can be detrimental to your health, especially if you have a renal diet. Overeating can lead to weight gain and high blood pressure, which are risk factors for kidney disease.
To combat mindless eating, try incorporating mindful techniques during meal times. Take time to savor the flavors and textures of each bite, focusing on how the food makes you feel. This will help you become more aware of your body's signals for hunger and fullness. Additionally, practicing mindfulness exercises such as deep breathing or meditation before meals can help calm your mind and improve overall digestion.
Being mindful during meal times is crucial for maintaining a healthy renal diet. Mindless eating poses many risks that can negatively impact both physical health and well-being. By implementing solutions such as mindful techniques and exercises, you can take control of your eating habits and promote better kidney function in the long run.
Avoiding Emotional EatingFeeling overwhelmed or stressed can often trigger emotional eating, which can be detrimental to your renal diet. It's important to recognize and acknowledge your emotional triggers in order to avoid mindless eating.
When you feel the urge to reach for comfort food, take a moment to pause and reflect on what is causing these emotions. Are you feeling anxious? Lonely? Tired? Identifying your emotional triggers can help you find healthier coping mechanisms.
Instead of turning to food as a source of comfort, try incorporating mindfulness practices into your daily routine. Mindfulness involves being present in the moment and focusing on your thoughts and feelings without judgment. This can include meditation, deep breathing exercises, or yoga. By practicing mindfulness regularly, you may be better equipped to deal with stressors when they arise.
Self-awareness techniques are also helpful in avoiding emotional eating. Take note of how different foods make you feel physically and emotionally after consuming them. If certain foods tend to trigger unhealthy behaviors or negative emotions, it may be best to avoid those foods altogether or limit their consumption.
Additionally, finding healthy alternatives that bring you pleasure can also help prevent emotional eating while still satisfying cravings. For example, instead of reaching for sugary snacks when feeling stressed, try snacking on fresh fruit or nuts instead.
Eliminating DistractionsNow that you've got some tips on avoiding emotional eating, let's talk about eliminating distractions during meal times. Mindfulness practices are a powerful tool for people with kidney problems and can help them build a better relationship with food. By practicing mindful breathing, sensory experience, and present moment awareness, you can reduce stress levels and focus on the act of eating.
One way to be more mindful when eating is to eliminate distractions. Turn off the TV, put away your phone or tablet, and sit down at a table without any other distractions that might take your attention away from what you're doing. This will allow you to focus on the task at hand and tune into the sensory experience of eating.
By bringing this level of intentionality to meal times, you'll be able to fully engage with your food and enjoy it as an experience rather than just something necessary for survival.
Keeping a Food JournalKeeping track of what you eat through a food journal can be like taking a snapshot of your daily meals, allowing you to see patterns and make adjustments for better kidney health. Reflection practice is essential in maintaining a renal diet as it helps you stay mindful of what you consume.
By jotting down every meal and snack, you begin to notice which foods work well for your body and which ones cause discomfort. A food diary enables you to track progress towards your dietary goals, motivating you to stay on track.
Identifying triggers is another benefit of keeping a food journal. You may find that certain foods or situations trigger overeating or unhealthy choices. Knowing these triggers allows you to prepare yourself mentally before encountering them again.
Moreover, tracking indulgences provides an opportunity for mindful indulgence rather than mindless snacking. When recording treats or cheat meals, take note of how they affect your mood and energy levels.
Tracking meal timing also plays an important role in maintaining a healthy renal diet. Keeping tabs on when and how much you eat allows for control of blood sugar levels and preventing spikes that could harm the kidneys over time.
Additionally, planning ahead with menu ideas ensures that meals are balanced with proper nutrients in mind. With the help of a food journal, monitoring meal timing becomes easier while making it possible to create healthy habits that last long-term.
Portion ControlControlling your portions is crucial to maintaining a healthy lifestyle and avoiding overindulgence in meals. Meal planning is one way to ensure you're eating balanced meals that are appropriate for your renal diet. By preparing your meals in advance, you can measure out the proper serving sizes and avoid the temptation of going back for seconds.
Measuring tools such as measuring cups, spoons, and food scales can be helpful when it comes to portion control. These tools allow you to accurately measure out the appropriate amounts of food for each meal or snack. When snacking mindfully, it's important to pay attention to portion sizes and choose low-sodium options like fresh fruits or vegetables.
Incorporating mindful eating habits into your daily routine can also help with portion control. Take time to savor each bite of your meal, chew slowly, and put down your fork between bites. This will give your brain time to register when you're full and prevent overeating.
By implementing these tips into your daily routine, you can maintain a healthy balance of nutrients while still enjoying delicious meals that fit within your renal diet restrictions.
Preparation and PlanningBy taking the time to plan and prepare meals in advance, individuals can ensure they're consuming balanced and nutritious food options that align with their health goals.
Grocery shopping is an essential part of this process, as it allows you to choose fresh produce and protein sources that meet your dietary needs. When grocery shopping for a renal diet, it's important to pay attention to food labels and opt for low-sodium options whenever possible.
Meal prepping is also key in mindful eating for a renal diet. By preparing meals ahead of time, you can avoid reaching for unhealthy snacks or fast food when hunger strikes. Recipe research can help inspire new ideas for healthy meal options that support kidney function. Take advantage of online resources or consult with a registered dietitian who specializes in renal diets.
Effective time management and kitchen organization can make meal preparation less stressful and more efficient. Set aside dedicated times each week for grocery shopping and meal prepping, so you always have healthy options on hand. Keep your kitchen organized by labeling foods, storing ingredients properly, and keeping cooking utensils within reach.
With these strategies in place, planning and preparing meals becomes an enjoyable part of your routine rather than a chore.
Assessing Mood and Food ChoicesAssessing your mood can help you make better food choices that support your health goals and overall wellbeing. Your emotional state can significantly impact the foods you crave, leading to unhealthy eating habits.
To avoid this, consider keeping a mood journal where you jot down how you feel before and after meals. This exercise will help you identify patterns in your eating habits and understand how your emotions affect them.
Mindfulness exercises are another effective tool to assess your mood and improve your food choices. Before reaching for a snack or meal, take a moment to pause and breathe deeply. Ask yourself how hungry you truly are and whether the desire to eat is driven by hunger or emotions such as stress or boredom. By taking this mindful approach, you'll be able to differentiate between true physical hunger and emotional triggers that lead to overeating.
Self-awareness techniques such as cognitive behavioral therapy can also aid in assessing your mood and making healthier food choices. This approach helps individuals recognize negative thought patterns that lead them towards unhealthy behaviors such as binge eating or consuming too much sodium-rich foods.
Through therapy sessions, individuals learn self-care techniques that promote positive thinking patterns which ultimately leads to healthy long-term dietary habits. Assessing your mood is an essential part of making mindful food choices on a renal diet plan. Whether through mindfulness exercises, keeping a mood journal or practicing self-awareness techniques like cognitive behavioral therapy- these tools will help you achieve optimal health outcomes while enjoying delicious meals!
Frequently Asked QuestionsCan mindful eating help improve kidney function in individuals with renal disease?Mindful eating techniques can offer several benefits to individuals managing renal disease. While mindfulness alone can't cure the illness, incorporating it into a renal diet and using it as part of a management plan can help improve kidney function.
Mindful eating encourages slowing down and paying attention to hunger cues and the sensations of eating, which can lead to better portion control and less overeating. Additionally, mindful eating promotes choosing nutrient-dense foods that support kidney health, such as fruits, vegetables, whole grains, and lean proteins, and limiting sodium intake.
By practicing mindful eating habits regularly, individuals with renal disease may experience improved overall wellbeing and better manage their condition.
If you have renal disease, there are certain dietary restrictions that you should follow to help manage your condition. Protein intake should be limited as excess protein intake can put extra strain on your kidneys.
Sodium control is also important as excess sodium can lead to fluid retention and elevated blood pressure.
Phosphorus management is another key factor as excessive phosphorus in the blood can cause bone problems.
Potassium limitations are necessary for those with advanced kidney disease, as high levels can affect heart function.
By following these guidelines, you can help improve your overall health and better manage your renal disease symptoms.
It's important to understand that the health benefits timeline for mindful eating and its impact on renal health can vary from person to person.
However, by adopting mindful habits and making positive changes in your eating behaviors, you may start to see improvements in your symptoms within a few weeks or months.
These lifestyle changes, such as paying closer attention to portion sizes or reducing your daily intake of certain foods, can help manage renal disease symptoms and improve overall health.
Remember that consistency is key when it comes to seeing long-term benefits from mindful eating.
To enhance the experience of mindful eating, there are several mindfulness techniques and exercises that can be practiced before meals.
Mindful breathing is a great way to center yourself and focus on the present moment, allowing you to fully enjoy your meal without distractions.
Sensory awareness involves paying attention to the textures, colors, and flavors of your food, which can help you appreciate the taste of food and the nourishment it provides.
Practicing gratitude before a meal can also enhance your mindful eating experience by fostering a positive mindset and appreciation for the food you're about to eat.
Portion control is another key aspect of mindful eating, as it helps you tune in to your body's hunger cues and avoid overeating.
Finally, mindful meal planning involves taking time to plan and prepare healthy meals that align with your dietary needs and preferences so that you can fully enjoy them during mealtimes.
Incorporating these techniques into your daily routine can help you cultivate a more mindful approach to eating while promoting better health outcomes overall.
Emotional triggers and stress levels can significantly impact the effectiveness of mindful eating in managing symptoms of renal disease.
Mindful awareness, coupled with mindful breathing, can help identify emotional triggers before meals and assist in stress management. However, cognitive restructuring may also be necessary to change negative thought patterns that contribute to stress.
By identifying and addressing emotional triggers and utilizing mindfulness techniques such as deep breathing and cognitive restructuring, you can better manage your stress levels and enhance the effectiveness of mindful eating in managing symptoms of renal disease.
Congratulations! You've made it to the end of this article on mindful eating tips for a renal diet. By now, you should know how crucial it is to maintain a healthy and balanced diet when living with kidney disease.
It's easy to succumb to unhealthy comfort foods and mindless eating habits, but by practicing mindfulness in your food choices, you can benefit from improved physical health and emotional well-being.
Remember that being aware of what you eat and how much you eat is crucial for managing your kidney disease. Keeping a food journal, planning your meals ahead of time, and practicing portion control are just some of the ways you can start incorporating mindful eating into your daily routine.
Don't forget to assess your mood before making food choices too, as emotional eating can often lead to unhealthy habits.
In conclusion, incorporating these mindful eating tips into your renal diet will help improve not only your physical health but also promote emotional well-being. Be patient with yourself as making lifestyle changes takes time and effort. With dedication and persistence, you can achieve a healthier lifestyle that supports optimal kidney function.
The post Mindful Eating Tips For A Renal Diet appeared first on Renal Diet HQ.
Suggested Reading:
Renal Vegetarian Diet The Importance Of Diet For Stage 3 Chronic Kidney Disease Early Stage Kidney DiseaseJune 20, 2023
Following a Low Sodium Kidney Diet
Are you living with chronic kidney disease (CKD) or on dialysis? If so, it is important to follow a low-sodium diet.
Sodium is one of the biggest ingredients to avoid. In your body, the kidneys are responsible for filtering out excess sodium and other waste. When the kidneys are not functioning properly, they are not able to properly filter out excess sodium.
A build up in sodium can lead to many serious health problems. Excessive sodium intake can lead to fluid retention, high blood pressure, and swelling – all of which can be very dangerous for those with CKD. Fluid retention can be a very serious matter.
If renal patients are not careful, fluid can build up so much that it floods into the lungs, making it hard to breathe. In this article, we'll explore the importance of following a renal diet and provide tips for grocery shopping and managing sodium intake.
We will also provide delicious low-sodium recipes that are sure to please any palate!
So let's get started on your journey to healthier eating!
[feast_advanced_jump_to]Key Takeaways
- A low sodium renal diet is recommended for patients with renal disease to avoid serious health problems such as fluid retention, high blood pressure, and swelling.
- Fresh or frozen fruits and vegetables are preferred over canned options which may contain added sodium.
- Salt-free seasonings can add flavor without added salt, and cured meats such as bacon, hot dogs, and lunch meats should be avoided.
- Grocery shopping for a low sodium renal diet may require some adjustments but there are many healthy options available, and managing sodium intake is important for those with chronic kidney disease.
Health ImplicationsFor More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
Making the right dietary choices can have a huge impact on your health, especially if you're living with CKD.
High sodium intake can lead to increased blood pressure, which is a major risk factor for kidney disease progression. Elevated blood pressure puts stress on the kidneys and can further damage their vessels.
Excessive sodium intake can cause fluid retention in the body, leading to swelling in the ankles, legs, and other parts of the body.
Following a low sodium kidney diet is essential to managing hypertension risks and fluid retention. The kidneys are responsible for filtering out excess sodium and waste from the body, so any extra sodium intake can lead to serious health complications. Therefore, it's important for individuals with CKD to pay attention to their daily sodium intake.
Restrictions and GuidelinesRestricting sodium intake is critical for those with CKD to maintain proper body function and avoid serious health complications. The recommended daily sodium intake for kidney patients is 1,500 mg/day, but the average American consumes 3,400 mg/day. Meal planning, grocery shopping, dining out and cooking tips can help reduce sodium intake while still enjoying delicious foods.
A low-sodium diet requires careful consideration when it comes to food choices. Fresh or frozen fruits and vegetables are preferred over canned options which may contain added sodium. Cured meats such as bacon, hot dogs, lunch meats should be avoided or limited if possible.
When you are grocery shopping, try to avoid most boxed or processed packaged foods. A lot of them contain a lot of sodium and other preservatives that your kidneys may not be able to process properly. If you must purchase these products, aim for products that have less than 35 mg of sodium per serving, which means that they are very low in sodium.
Low-sodium juices and beverages are best as well as unsalted butter which can remove around 4% of the daily value (DV) of sodium per tablespoon used in recipes compared to salted butter. Sodium-free or very low sodium products are ideal when available. Salt-free seasonings like garlic, cumin, turmeric and sage can add flavor without adding salt to dishes at home or when dining out.
Food OptionsA significant step towards a low sodium diet is to focus on whole, unprocessed foods. Fresh fruits and vegetables are naturally low in sodium and packed with essential nutrients. Apples, berries, cherries, pineapple, lemons, peaches, pears, tangerines, and watermelon are excellent fruit choices for a low sodium renal diet. For vegetables, try asparagus, broccoli, cucumbers, summer squash, and eggplants.
When it comes to protein, opt for fresh meats and fish over processed varieties. Many processed meats are high in sodium, used as a preservative and flavor enhancer. Fresh chicken, fish, and pork loin protein are lower in sodium and can be seasoned with a variety of herbs and spices for flavor.
Speaking of herbs and spices, they are your best friends on a low sodium diet. Swap out salt for flavorful alternatives like garlic, onion, pepper, rosemary, thyme, and other sodium-free seasonings. Mrs. Dash is a popular brand offering a wide range of salt-free seasoning blends that can add a flavor punch to your meals without the sodium.
Grains, pasta, and rice can also be part of a low sodium diet. Opt for whole grain varieties when possible, as they are more nutritious. As a general guideline, you should look for foods with 5% Daily Value (DV) or less of sodium. A DV of 20% or more is considered high. Be mindful of pre-packaged mixes, though, as they often contain added salt. Cooking these items from scratch allows you to control the sodium content.
Now, let's talk about condiments. Many store-bought sauces and dressings are high in sodium. However, you can make your own at home with a few simple ingredients. For example, a homemade salad dressing can be as simple as olive oil, vinegar, and your favorite herbs.
Lastly, don't forget about beverages. Some drinks, like certain sports drinks or sodas, can be high in sodium. Water is always the best choice, but if you're looking for something with a bit more flavor, try fresh juices like apple juice and grape juice, both of which are kidney friendly.
Remember, managing sodium intake doesn't mean you have to sacrifice flavor. With a little creativity and knowledge, you can enjoy a diverse, flavorful diet that supports your kidney health. Always consult with your healthcare provider or a dietitian for personalized advice.
Canned FoodsThe high sodium content in many canned goods can be a real issue, but don't worry, there are plenty of low-sodium options out there that are both tasty and kidney-friendly.
Firstly, let's talk about vegetables. Canned vegetables are a convenient and affordable way to get your daily dose of vitamins and minerals. However, many canned vegetables are loaded with sodium to increase their shelf life. The good news is that many brands offer sodium-free or reduced-sodium versions. These are a great choice for those following a low-sodium kidney diet. Just remember, moderation is key. Even low-sodium vegetables can be harmful to the kidneys if consumed in excess.
Beans and lentils can be fantastic low-sodium canned food options. These nutrient-packed legumes are versatile and can be used in a variety of dishes. However, make sure to check with your doctor or kidney dietitian before incorporating beans into your kidney diet, as they may be unsuitable for some kidney patients because of their potassium and phosphorus contents, especially patients on dialysis.
Reading labels is crucial when choosing low-sodium canned foods. This way, you'll know exactly how much sodium each product contains and can avoid exceeding your recommended dietary limits. It might seem like a lot of work, but with a little practice, it'll become second nature. Pick canned foods labeled "No salt added" or something similar—this can make a difference between a serving of beans being 22% vs 4% of your DV of sodium.
One good tip to follow when using canned vegetables is to rinse them before cooking. Rinsing canned vegetables can reduce salt content by 23%. This makes them a great option for those seeking to incorporate vegetables into their renal diets without compromising taste or health.
Canned fruits can also be a good choice. However, they can be high in sugar, so it's important to choose fruits canned in their own juice rather than syrup. And, as always, check the label to ensure you're making a kidney-friendly choice.
While canned foods can be a convenient and affordable option, it's important to remember that fresh is best. Fresh fruits and vegetables tend to have fewer additives and are often lower in sodium. Frozen produce can also be a good choice, as it's often free from preservatives and additional salt.
Meats and FishNow that you know how to manage the sodium content of canned foods, it's time to turn our attention to meats and fish. Protein sources are important for renal health, and when following a low-sodium kidney diet, making smart choices is key.
Some meats, poultry, and seafood options have added sodium. The good news is that there are still plenty of delicious options available! If the package has a Nutrition Facts label, it’s important to look for products with a 5% DV of sodium or less per serving.
Choose fresh or frozen meats, poultry, and seafood, and instead of processed products. When selecting meats and fish for your meal plan, look for products that don't have added brine or salt solutions—skipping the brine can save over 10% of the recommended DV of sodium per serving.
When cooking these proteins at home, use low-sodium seasonings such as garlic powder or herbs like oregano or basil instead of traditional salt-based seasonings. Be mindful of portion sizes too; adults should aim for 4-6 ounces of meat, poultry or fish per day.
Meal planning can be a great way to ensure you stay on track with your low-sodium kidney diet while still enjoying delicious meals. Try including more plant-based proteins into your menu such as beans and legumes which provide fiber and minerals. With some creativity in the kitchen, you can create flavorful dishes while managing your dietary needs!
Baked GoodsEating baked goods while following a low sodium renal diet doesn't have to be boring or difficult. With some simple substitutions and ingredients, you can enjoy the flavor of freshly-baked desserts and breads without worrying about excess sodium.
When baking at home, consider making low sodium substitutions in your recipes. Unsalted butter is an easy swap for regular butter that can reduce the daily value of sodium per tablespoon by 4%.
If a recipe calls for salt, try using flavorful herbs like garlic and cumin instead. You can also use fruit juices such as apple or orange juice to add sweetness without adding any extra salt. There are many delicious low sodium desserts available if you don't want to bake at home.
Bread is a surprising source of sodium in American diets. Up to 10% of the sodium we get from meals in the United States comes from bread.
Whole grain bread is recommended for kidney diets instead of white bread because of it’s high fiber content. Although whole grain bread may be slightly higher in phosphorus, most of it isn’t absorbed. Some of the best breads for kidney disease include Ezekiel Sprouted Whole Grain Bread, Brownberry Whole Grain Health Nut Bread, and Dave’s Killer Whole Grains & Seeds Bread.
With these tips, it's easy to find flavorful alternatives that won't cause any extra strain on your kidneys!
Condiments and SaucesYou can still enjoy flavorful meals while managing your kidney health with delicious condiments and sauces. Making creative substitutions, DIY options, and sodium-free swaps are all great ways to flavor boost meals without compromising your renal diet.
To begin with, there are many store-bought options that are either low or no sodium, such as mustard, horseradish, garlic, Mrs. Dash herb seasoning blend, lemon juice, jam or jelly, yellow Tabasco sauce, and even vinegar. For those who prefer a DIY approach, you can make your own condiments with fresh ingredients like garlic paste or roasted red peppers blended in a food processor.
When meal planning for the week ahead, it's important to have some of these low-sodium condiments on hand for quick and easy meal preparation. For those looking to add flavor without increasing their sodium intake, there are salt-free herbs and spices like cumin, turmeric, and sage. These work well in many dishes, such as a couscous salad or chili con carne.
With just a few simple changes, you can reduce your overall dietary intake of sodium while still enjoying tasty meals with friends and family at home or while eating out!
RecipesDiscovering delicious, nutritious meals that fit within your dietary restrictions can help you maintain a healthier lifestyle. Following a low sodium kidney diet may seem daunting at first, but with the right recipes and ingredients, it's possible to enjoy hearty meals while managing health.
Here are some tips on how to find great-tasting kidney-friendly recipes:
Kidney-friendly desserts: Desserts don't have to be off-limits! Look for recipes using fruits like apples and strawberries as a sweetener, and try baking with unsweetened cocoa powder instead of sugar. Low-fat Greek yogurt is also an excellent option for those looking for something creamy and delicious that won't add too much sodium.Low-sodium snacks: Instead of reaching for chips or high-sodium pretzels, look into making your trail mix with nuts. Air-popped popcorn is also a great snack that doesn't require any added salt or butter – just sprinkle on some garlic powder if desired!Quick and easy meals: When time is tight, there are plenty of options for quick and healthy meals that will still leave you feeling full without adding extra sodium intake. Try making vegetable stir-fries with fresh vegetables in place of canned ones which often have more salt added; opt for lean proteins such as grilled chicken breast over lunch meats; and use herbs and spices to flavor dishes without having to reach for the salt shaker!Vegetarian options: Plant-based proteins such as beans, lentils, and tofu are naturally low in sodium and will satisfy both taste buds as well as nutrition needs! Also, explore international cuisine such as Indian curries which typically rely heavily on spices rather than salt when flavoring dishes.With these tips in mind, exploring new flavors can be exciting while keeping health goals on track no matter what type of food preferences you have! Whether you prefer creating complex gourmet dishes or prefer simple one-pot dinners – there's something out there that will fit your needs while following a low sodium renal diet.
Frequently Asked QuestionsWhat are the long-term effects of a low sodium renal diet?A low-sodium renal diet can provide several benefits for people with kidney disease. Here are some of the benefits:
1. Blood Pressure Control: A low sodium diet can help lower blood pressure, which is important for individuals with kidney disease. High blood pressure can further damage the kidneys, so reducing sodium intake can help manage blood pressure levels.
2. Fluid Balance: Sodium plays a role in fluid balance in the body. By reducing sodium intake, individuals can help manage fluid retention and prevent swelling or edema.
3. Kidney Function Preservation: A low sodium diet can help slow down the progression of kidney disease and preserve kidney function.
4. Heart Health: Swapping salt with salt substitutes can benefit heart health by reducing the risk of cardiovascular diseases such as heart attack and stroke.
When it comes to renal health, there are some foods that should be avoided on a low sodium diet. Cured meats such as bacon, hot dogs, lunch meats, and processed packaged foods should be limited or avoided due to their high sodium content.
Eating too much sodium can lead to serious health complications such as fluid retention, high blood pressure, and swelling. Instead of using salt or salty seasonings, try using salt-free alternatives like garlic, cumin, turmeric, and sage for flavoring.
Reading nutrition labels is an important part of managing kidney health. When checking the sodium content, look for serving sizes and be aware that sodium can come from many sources. It's important to note that foods labeled as 'sodium-free' or 'low-sodium' may still contain some sodium.
For a more accurate assessment of your intake, read nutrition labels and aim for less than 5% Daily Value (DV) of sodium per serving.
By being mindful of what you eat, you can accurately track your sodium intake and help maintain healthy kidney function.
When it comes to snacking, there are many healthy options available for those looking to make smarter food swaps. Meal planning can be beneficial in finding snacks that contain lower levels of sodium and more nutrient-rich foods.
Nuts, seeds, fruits, vegetables, and whole grains are all great options for snacks that are low in sodium and full of essential vitamins and minerals. Unsalted tortilla chips and unsalted popcorn are also good low sodium snacks. Consider substituting traditional ingredients with sodium substitutes like vinegar or herbs and spices to add flavor without the added salt.
There are also plenty of healthy recipes online that can help you find delicious snacks while keeping your sodium intake low.
It's important to monitor your sodium intake as part of a healthy lifestyle. The recommended daily sodium intake for healthy adults is 2,300 mg/day, but the average American consumes 3,400 mg/day.
However, if you have chronic kidney disease or are on dialysis, it's recommended that your daily sodium intake be less than 1,500 mg.
To limit your sodium intake you should look for low-sodium alternatives and substitutes such as salt-free seasonings like garlic, cumin, turmeric, and sage. Additionally, reduce canned foods with added salt, avoid packaged foods.
Lastly, be mindful of meats without brine and unsalted butter, which can help lower the amount of sodium consumed each day.
You've learned a lot about following a low sodium kidney diet. Not only does it help to reduce fluid retention and high blood pressure, but it can also improve overall health for people with chronic kidney disease.
Eating the right foods and avoiding those that are high in sodium is essential. Be sure to read labels when grocery shopping, manage your intake by reading nutrition facts, and try out some delicious, low-sodium recipes.
By sticking with this diet, you can take control of your health and live a longer, healthier life.
Join my FREE email community and get your free gifts, no credit card required! Click HereThe post Following a Low Sodium Kidney Diet appeared first on Renal Diet HQ.
Suggested Reading:
Renal Vegetarian Diet Renal Diet Sodium Limit Renal Diet Food ListJune 19, 2023
Reading Nutrition Facts Labels With CKD
If you have chronic kidney disease (CKD), it can be overwhelming to navigate nutrient labels while grocery shopping. But don't worry, with the right knowledge on food label, you can make informed choices that support your kidney health.
This article will guide you through everything you need to know about reading nutrient listing with CKD.
Firstly, we'll cover how to understand serving sizes and why they matter for those with kidney disease. We'll then discuss the importance of potassium information on food labels, as well as sodium limits for kidney disease patients.
You'll also learn about total fat and a low-fat diet, total carbohydrates and fiber intake, protein in a balanced diet, hidden phosphorus in ingredients list, fluid intake recommendations, and even some delicious kidney-friendly recipes. With this comprehensive guide from Renal Diet HQ, you'll have all the tools necessary to make healthy food choices that support your overall health and wellbeing.
Let's get started!
[feast_advanced_jump_to]

Understanding Serving SizesFor More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
Let's talk about understanding serving sizes - it's an important aspect to consider when reading nutrition facts labels with chronic kidney disease (CKD). Portion control is vital for managing kidney disease, and the serving size listed on the food packages labeling can help you keep track of how much you're consuming.
It's essential to remember that serving sizes may differ from what your kidney diet plan recommends, so consulting with a renal dietitian is crucial. Caloric intake is another factor affected by serving sizes. The larger the portion, the more calories you consume, which could lead to unwanted weight gain or other health issues.
Understanding serving sizes can also help you identify nutrient-dense foods that provide optimal nutritional value per calorie consumed. This information is particularly helpful for those seeking to manage their caloric intake while ensuring they get all their necessary nutrients. Understanding serving sizes can assist in making food substitutions without compromising your dietary needs.
By comparing similar products' serving sizes and nutritional values, you can choose options that are lower in sodium, potassium or phosphorus levels while still meeting your daily nutrient levels. Nutrition facts panel reading tips include looking at both the actual amount of each nutrient in a single-serving container as well as calculating how much percentage of daily value it contributes towards overall daily consumption goals.
In summary, understanding serving sizes plays a critical role in maintaining optimal nutrition levels needed for CKD management and prevention of further complications associated with this disease state.
Importance of Potassium InformationYou need to pay attention to the potassium content on foods nutrition labels if you have kidney disease, as it's an important nutrient that can impact your health. Potassium helps regulate fluid balance, muscle function, and blood pressure. However, when your kidneys aren't functioning properly, high levels of potassium in the blood can be dangerous and even life-threatening.
Patients living with CKD are at risk for having potassium levels that are either too high or too low. To ensure you're getting enough potassium but not too much, it's important to know the recommended potassium intake for individuals with kidney disease. A daily intake of 2,000-3,000 mg of potassium is recommended for people with kidney disease on a low-potassium diet.
However, this may vary depending on factors such as age and stage of kidney disease. Look for low-potassium foods with no more than 200 mgs of potassium per serving.
There are many high-potassium foods that should generally be avoided while on a low-potassium kidney-friendly diet. Some examples include sweet potatoes, spinach, bananas, avocados, and salmon.
Incorporating more low-potassium meals into your diet doesn't have to mean sacrificing taste or variety. There are many delicious meal ideas available that incorporate low-potassium ingredients such as grilled chicken with roasted green beans or a lettuce salad with cucumber and cranberries. Don't forget about seasoning options either – herbs such as rosemary and thyme add flavor while also being suitable for a low-potassium diet!
For those who struggle to meet their recommended intake through diet alone or have very low levels of potassium in their blood due to medication use or other reasons, high-potassium foods or potassium supplements may be an option. Be sure to talk to your healthcare provider before starting any new supplement regimen.
By paying attention to the levels of nutrients listed on the nutrition labelling and incorporating more high-potassium foods into your meals, you can help support healthy kidney function and overall well-being.
Sodium Limits for Kidney Disease PatientsWhen it comes to managing your kidney disease, it's essential to keep an eye on your sodium intake. High blood pressure and fluid retention are common in people with kidney failure, and consuming too much salt can exacerbate both. The American Heart Association recommends that most adults consume no more than 2,300 milligrams of sodium per day, but for those with kidney disease, the limit may need to be further lowered to 1,500 milligrams.
One way to reduce your sodium intake is to experiment with low-sodium seasoning blends or salt substitutes. These products use herbs and spices to add flavor without adding extra salt. However, some people find them unappealing or too expensive.
Another option is to look for foods labeled 'low-sodium' or 'no added salt.' Be sure to read the nutrition facts label carefully – even foods marketed as healthy options can be high in sodium. Look for products with no more than 6-10% of the recommended daily value of sodium.
It's also important to stay hydrated when you have kidney disease. Drinking enough water can help flush excess wastes out of your system and prevent dehydration, which can lead to a host of other health problems. Talk to your doctor or renal dietitian about how much fluid you should be drinking each day based on your individual needs and medical history.
Total Fat and Low-Fat DietReducing your total fat intake is crucial for managing kidney disease, and a low-fat diet can help you achieve this goal. However, fats are not created equal, and while some types of fat can be harmful to people with kidney disease, others may be beneficial. Foods high in healthy fats include nuts, seeds, fatty fish like salmon or tuna, olive oil, peanut butter, and tofu.
Healthy fats are an excellent source of energy and nutrients that are essential to maintaining good health and may promote kidney health. The other benefits of healthy fats include reducing inflammation, improving brain function and heart health while decreasing the risk of developing chronic illnesses such as diabetes and heart disease.
Cooking techniques for low-fat meals include baking or grilling instead of frying food in oil or butter. Low-fat substitutes like nonfat Greek yogurt or applesauce can replace ingredients like sour cream or oil in recipes.
Paying attention to the amount and type of fat you consume is essential to managing kidney disease effectively. Incorporating healthy sources of fat into your diet while being mindful of portion sizes will improve your overall well-being.
Consulting a renal dietitian for guidance on how to navigate a low-fat diet can take the guesswork out of meal planning while ensuring that you receive proper nutrition.
Total Carbohydrates and FiberIncorporating fiber-rich foods into your diet can help manage kidney disease by promoting digestive health and regulating blood sugar levels. Total carbohydrates include both dietary fiber and sugars, which can affect blood glucose levels. Carb counting is important for those with diabetes or pre-diabetes. The glycemic index measures how quickly a carbohydrate-containing food raises blood sugar levels.
To ensure you are getting enough fiber, aim for at least 25 grams per day for women and 38 grams per day for men, according to the USDA. Fiber sources include fruits, vegetables, whole grains, legumes, nuts, and seeds. Some people may find it difficult to get enough fiber through their diet alone and may benefit from fiber supplements.
When shopping for kidney-friendly foods, look for products that have a good source of fiber with at least 3-5 grams per serving of food. Sugar substitutes such as stevia or sucralose can be used in moderation to sweeten foods while lowering carbs and calories. Remember to always read the nutrition facts label carefully and consult with a renal dietitian about your recommended nutrient needs.
High-Fiber FoodsServing SizeFiber Content (grams)Brussels sprouts (raw)1 cup3.4Black beans (cooked)½ cup7.5Broccoli (cooked)1 cup chopped5Apples1 cup chopped3Raspberries (fresh)1 cup8Quinoa (cooked)15.1Incorporating high-fiber foods into your diet can provide numerous benefits beyond managing kidney disease including reducing risk of heart disease and stroke. By focusing on good sources of dietary fiber while watching carb intake using techniques like carb counting or monitoring the glycemic index, you can help maintain stable blood sugar levels.
Remember to always read the nutrition facts label and ingredient list carefully for hidden sources of sugar or phosphorus intake. By working with a renal dietitian, you can create a personalized eating plan that meets your specific nutrient needs while also promoting overall health.
Protein in a Balanced DietTo maintain a balanced diet, you should aim to include adequate amounts of protein from a variety of sources such as lean meats, poultry, fish, low-fat dairy products and plant-based options like legumes and tofu. Balancing macronutrients is crucial for individuals with CKD because it can help manage symptoms and prevent further complications.
In general, people with CKD may require more or less protein depending on their stage of kidney disease. Here are three important points to keep in mind when considering protein intake:
Protein requirements vary: Individuals with early-stage CKD may need more protein than those in later stages because they are still able to filter waste products effectively. As the disease progresses, however, excess protein can be harmful to the kidneys. It's essential to work with a renal dietitian to determine your individual protein needs.Plant-based proteins are a great option: Plant-based proteins like beans and lentils are low in fat and high in fiber which makes them valuable additions to a renal-friendly diet. They also contain less absorbable phosphorus compared to animal-based proteins which can be beneficial for those with CKD.Be cautious about supplements: Protein supplements like powders and shakes should be used under the guidance of a healthcare professional because they can contain high levels of minerals that can damage the kidneys if consumed in excess. It's always best to meet your protein needs through whole foods whenever possible.Hidden Phosphorus in IngredientsWatch out for hidden sources of phosphorus in your food, as they can be harmful to your kidneys. It’s also important to keep in mind that the nutrition facts labels don’t always list the phosphorus present in a serving.
To avoid consuming excess phosphorus, it's important to read ingredient lists carefully. Look for words that contain "phos," such as phosphoric acid or sodium hexametaphosphate. Additionally, avoid processed foods and opt for fresh fruit and vegetables instead. These whole foods are typically lower in their levels of phosphorus and other harmful minerals.
Nutrition education is key to understanding how to properly manage kidney disease through diet. By learning about hidden phosphorus sources and how to read labels effectively, you can make informed choices that promote kidney health. Consult with a registered dietitian who specializes in renal nutrition for personalized guidance on managing your condition through diet.
Phosphorus SourcesExamplesAdditives/preservativesSodium phosphate, calcium phosphateDairy productsMilk, cheeseDrinksBeer/ale, cocoaProteinBeef/chicken liver, organ meats, sardines.Fluid Intake and Kidney-Friendly RecipesNow that you know how to spot hidden phosphorus in food ingredients, let's talk about fluid intake and kidney-friendly recipes. As someone with CKD, it's important to keep track of your fluid intake as well as finding ways to stay hydrated without overloading your kidneys.
Fluid intake tips include drinking small amounts throughout the day rather than chugging large volumes at once. Sipping on water or other low-sodium drinks like herbal teas can also help with hydration. Additionally, avoiding high-sodium foods and using herbs and spices instead for flavor can reduce thirst.
When it comes to meal planning, incorporating flavorful drinks like infused waters or homemade smoothies can add variety while also being kidney-friendly. Recipe suggestions include a cucumber and mint infused water or a spinach and banana smoothie. Consulting with a renal dietitian can also provide personalized recommendations for staying hydrated while maintaining a kidney-friendly diet.
By implementing these hydration strategies and adding kidney-friendly drinks into your daily routine, you can ensure proper fluid balance while still enjoying delicious beverages. Don't forget to consult with your healthcare team for personalized advice on managing your CKD through nutrition.
Frequently Asked QuestionsWhat are some common misconceptions about food labels and serving sizes for people with CKD?Misconceptions about food labels and serving sizes for patients with kidney disease are common. Many believe that salt alternatives or flavorings can be used freely, but it's important to remember that these still contain potassium and must be used in moderation.
Additionally, some may think that nutrient intake should be restricted, but in reality, a balanced diet is crucial for optimal health. Fluid restriction is also important, but there are creative ways to limit intake while still enjoying flavorful meals.
It's essential to practice label reading and follow a kidney disease diet plan to ensure proper nutrient intake and potassium balance. With the right knowledge and food options, maintaining a healthy lifestyle with CKD is possible.
To ensure dietary balance, CKD patients need to incorporate low potassium options into their diet while also utilizing appropriate cooking techniques and practicing portion control.
Some low potassium options include apples, berries, cucumber, green beans, cauliflower, and cabbage. Leaching by soaking vegetables in warm water can help reduce their potassium content
Portion control is key, so make sure to measure out servings and avoid going back for seconds. Nutritional supplements may also be helpful in meeting nutrient needs without exceeding recommended potassium intake levels. Consult with a renal dietitian to develop an individualized plan that meets your specific nutritional needs while managing your potassium intake.
If you're looking to flavor your food without using table salt, there are several herbal alternatives that can be used. Citrus fruits like lemon and lime can add a tangy taste, while spices and herbs like thyme, basil, and oregano can add a savory flavor. Vinegar-based dressings are also a great option for adding flavor without the sodium.
Additionally, low sodium seasoning blends are available at most grocery stores and can be used in place of traditional seasonings. It's important to talk to your dietitian about incorporating these options into your kidney-friendly diet plan.
If you have CKD and you're looking for high-protein sources, there are a few options you can consider. Good protein sources include lean meats like chicken, fish, or turkey, egg whites, low-fat dairy products like milk and yogurt, beans and legumes, tofu, or tempeh. However, it’s important to not exceed your recommended protein intake, as this can cause waste to build up in your body.
When cooking these proteins, it's important to choose healthier methods such as grilling or baking instead of frying. Portion sizes should also be monitored to ensure that you don't exceed your daily protein requirements.
Meal planning with a renal dietitian can help ensure that you're getting enough protein while still staying within the guidelines of your kidney-friendly diet.
In some cases where additional supplementation is necessary to meet protein needs, your healthcare provider may suggest adding in a protein powder supplement.
To ensure you're getting enough amounts of nutrients while not exceeding your recommended caloric intake with CKD, there are several strategies you can implement.
First, focus on nutrient-dense options such as lean proteins, fruits and vegetables, and whole grains. These foods provide essential vitamins and minerals without adding excess calories to the body.
Additionally, practice portion control by measuring out servings and limiting high-sodium foods.
Finally, look for low-sodium alternatives to your favorite foods and be mindful of hidden sources of sodium in pre-packaged foods.
By incorporating these tips into your diet, you can maintain a healthy balance of nutrients while managing your caloric intake with CKD.
Congratulations! You've now got a comprehensive understanding of how to read nutrition facts labels with chronic kidney disease (CKD). Armed with this knowledge, you can confidently make informed choices about what foods to eat and avoid.
Remember to pay close attention to serving sizes, potassium and sodium information, total fat and carbohydrates, protein levels, hidden phosphorus in ingredients, and fluid intake. By incorporating kidney-friendly recipes into your diet, you can maintain a balanced diet while still enjoying delicious meals.
It may take some time to get used to reading nutrition facts labels with CKD, but it's worth the effort. With practice, you'll become more comfortable navigating food labels and making informed choices that support your kidney health.
By taking control of your diet and lifestyle habits today, you're investing in a healthier future for yourself tomorrow.
The post Reading Nutrition Facts Labels With CKD appeared first on Renal Diet HQ.
Suggested Reading:
Stage 4 Kidney Disease Diet The Importance Of Diet For Stage 3 Chronic Kidney Disease Can You Eat Pasta on a Renal Diet?June 18, 2023
Snacks For CKD And Diabetes
Living with chronic kidney disease (CKD) and diabetes can be a challenge, but with the right approach, you can still enjoy delicious snacks that are suitable for your health conditions. As someone managing both CKD and diabetes, it's important to pay close attention to what you're eating to ensure you're getting the nutrients you need while keeping your blood sugar levels under control.
With the help of a registered dietitian and some planning, there are many options for healthy snacks that will satisfy your cravings without compromising your health.
It's not always easy to know what foods and snacks are safe when you have CKD and diabetes. You may feel overwhelmed by all of the different recommendations and food lists out there. But don't worry - with some guidance, you can find tasty snack options that fit within your dietary restrictions.
In this article, we'll explore some tips for snacking on a kidney-friendly daily diet while also managing diabetes. From fruits and vegetables to low-sugar treats, there are plenty of healthy snack options available that will help keep you feeling satisfied throughout the day. So let's dive in!
[feast_advanced_jump_to] Key TakeawaysSnacking on the kidney diet is okay as long as healthy choices are made.Snack options should be kidney-friendly and low in phosphorus, potassium, sodium, and calcium.Some patients may need to restrict protein in their snacks, and phosphate binders may need to be taken with protein-containing snacks to control phosphorus.Patients with CKD should consult their doctor or dietitian to learn what snack foods are good for their kidney diet.
Key TakeawaysSnacking on the kidney diet is okay as long as healthy choices are made.Snack options should be kidney-friendly and low in phosphorus, potassium, sodium, and calcium.Some patients may need to restrict protein in their snacks, and phosphate binders may need to be taken with protein-containing snacks to control phosphorus.Patients with CKD should consult their doctor or dietitian to learn what snack foods are good for their kidney diet.What is Renal Diabetes?For More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
If you have renal diabetes, also called diabetic kidney disease or diabetic nephropathy, it's important to understand that this condition is a common complication of diabetes that affects the kidneys and can lead to decreased kidney function.
It occurs when high blood glucose levels damage the small blood vessels in your kidneys, reducing their ability to filter waste products from your blood. Symptoms may include fatigue, nausea, vomiting, worsening blood pressure control, and swelling in the hands or feet.
To manage renal diabetes, there are several strategies you can use. One of the most important is proper nutrition. A dietitian can help you create a meal plan that takes into account your specific dietary restrictions and needs.
You may need to limit potassium, phosphorus, protein or sodium contents depending on your individual situation. In addition to dietary changes, medication options such as ACE inhibitors or ARBs may be prescribed by your doctor to slow down the progression of kidney disease.
Lifestyle changes such as quitting smoking or maintaining a healthy weight can help manage renal diabetes. Regular exercise is another key component of managing this condition; aim for 30 minutes of moderate-intensity activity at least three days per week if possible.
With these management strategies in place, many people with renal diabetes are able to lead fulfilling lives without significant complications related to their condition.
Keeping a Food List HandyKeeping a food list handy can be a lifesaver for renal diabetes patients, especially when grocery shopping or dining out. A pocket-sized convenience like a food list can relieve stress and confusion about what to eat. It can also help the family plan meals and make grocery shopping easier.
Digital alternatives are available too, like apps that allow patients to stay on target with their renal diabetes food list. Consulting professionals such as registered dietitians is recommended for creating an effective food list that caters to individual needs. The input of family members also helps in planning healthy meals and keeping track of food choices.
When grocery shopping, having a convenient reference for the recommended nourishing foods and meal plans makes it easier to stick to the diet restrictions. Having the food list easily accessible helps when eating out or at new places too, making it less obtrusive than carrying around bulky lists or feeling embarrassed about asking restaurant staff about suitable options.
Keeping a food list handy is essential for renal diabetes patients in managing their condition. Whether it's through traditional pocket-sized lists or digital alternatives like apps, consulting professionals and involving family members can also help create effective meal plans and make grocery shopping easier.
Getting started is the hardest part for most people. Renal diabetes patients often spend a great deal of time focused on the things they can no longer fail and forget to explore the depths of the foods they can have instead.
Renal dietitians are great for helping you see the possibilities instead of the limitations. That's important as you begin creating a renal diabetes food list that will help you establish healthy eating routines to carry you into the future. The sooner in the process you make an appointment with a qualified registered dietitian; the faster you'll begin to feel better about your menu and food choice options.
You are probably finding that you are confused about what to eat - as someone said the other day to me - "A renal diet is not necessarily a healthy diet for everyone." I interpret that to mean that in many cases we are encouraged to eat high fiber and proteins, and in the case of CKD, whole grains have more potassium and are generally discouraged.
Many times, lower protein is also encouraged. So talking to a qualified registered dietitian who is experienced in teaching people about the ins and outs of a renal diet can release a lot of the stress that you might be feeling about a new renal and diabetes diet.
Print out Full List and Post in Prominent PlaceThe refrigerator is an excellent place to keep your renal diabetes food list. This way it's handy whenever you're making your grocery list, planning your weekly menu, or going for an afternoon snack. There are all kinds of cute magnetic refrigerator frames you can use to make it look neat and tidy, while keeping it handy for regular use.
Having the list handy is a great way to relieve some stress on all the family. At home, even though we do not have renal diabetes, we have a grocery list and a meal list written out for the week. Everyone gets to help choose a couple of meals. We know the foods that are favorites and foods that are not.
When everyone participates, we find that we have less complaints when it's time to eat. Part of having the list is also that it makes going to the grocery store easier - we have a list almost started.
Print a Smaller Copy of the List for PortabilityWhile most meals, snacks, and shopping lists are enjoyed or created at home, there are times when you're out and about when the time for meals comes along. Sometimes you simply leave your grocery list at home. These are the times when you need something handy with you to help you make wise decisions. A small renal diabetes food list in your pocket or purse can help you do just that.
It's especially valuable when you are at a new place to eat, or out with friends and want to enjoy the environment but not mess up your diet. Because you know if you eat too much of something like salt or potassium, you will suffer from it later.
So being able to pull out a short list and ask if certain items are in the recipes can help. As you learn more about what is allowed and what causes you problems, you can make the adjustments easier.
There's an App for ThatIf you own a smartphone, another option is to install an app that helps you keep up with what's a hit and miss for your renal diet needs. Consult with your physician to see if he or she can recommend a good app to help you stay on target with your renal diabetes food list whether you're at home or on the go.
Your renal diabetes food list needs to be packed with food choices and meal plans you'll be happy to eat that will leave you feeling satisfied and not deprived. Try to incorporate meal plans that can be easily prepared ahead of time to help you avoid making convenience choices that aren't exactly wise for your health needs. Freezer cooking and slow cooker (crock-pot) meals are also great ideas if you still lead an active life.
Meal Planning and Convenience ChoicesPlanning ahead is key to maintaining a renal diabetes diet. Meal prep can save time and ensure that you have healthy options readily available.
Start by making a list of meals for the week, including snacks, and then make a grocery list based on those meals. This will help you avoid impulse purchases and stick to healthier options. Always remember to read the nutrition labels to make sure you are avoiding excess sodium levels and excess potassium levels.
When planning your meals, consider healthy swaps for ingredients that may not be suitable for your health needs. For example, instead of using high-potassium fruits, opt for low-potassium fruits like apples or berries or low-potassium veggies for snacks. You can also substitute high sodium condiments with low-sodium alternatives or use herbs and spices to add flavor without adding salt.
On-the-go options are important too, especially if you have a busy schedule or travel frequently. Plan ahead by packing portable snacks like cut-up fruits and vegetables, nuts or seeds, egg white, or low-sodium crackers and cheese. Having these options on hand can help you resist the temptation to grab convenience foods that may not fit with your renal diabetes diet.
By taking the time to plan ahead for meal prep, grocery shopping, and on-the-go options, you can make sure that you always have healthy choices available to support your kidney health needs. With some time management skills and healthy swaps in mind when meal planning, living with renal diabetes limitations doesn't have to be challenging or restrictive.
Snacking on a Kidney DietIndulging in guilt-free and healthy snacks can be a satisfying way to boost your calorie intake and support your kidney health needs. Kidney-friendly snacking is possible with the right choices.
Start by choosing snacks that are low in protein, sodium, phosphorus, and potassium contents. It may also be important to take phosphate binders to control phosphorus levels.
Be sure to avoid high sugar snacks as well if you are diabetic, especially as high sugar can cause further damage to your kidneys. Healthy snack options include kidney-friendly fruits and vegetables as well as unsalted breadsticks, unsalted crackers and tortilla chips, and unsalted pretzels.
Snacks should be compatible with your dietary restrictions but can still provide a tasty treat while supporting your overall kidney health goals.
Healthy Snack OptionsSatisfy your cravings and support your kidney health with these delicious and guilt-free snack options. When it comes to snacking on a kidney diet, choosing the right foods is crucial. You want snacks that are not only tasty but also low in phosphorus, sodium, and potassium while being high in protein.
Here are some kidney-friendly snack options that you can enjoy anytime:
Fresh fruits and vegetables: These are always a good choice for snacking as they are low in calories, high in fiber, and packed with nutrients. Some examples include apples, grapes, berries, plums, cucumbers, and celery.Protein-containing snacks: Consider healthy protein options like hard-boiled eggs or grilled chicken breast or unsalted seafood.Remember to consult with your doctor or dietitian before adding new snacks to your renal diabetes food list. They can help you create a personalized plan tailored to your specific needs so you can still enjoy delicious snacks without compromising your health.
Planning and ModerationWhen planning your meals and snacks, it's important to keep moderation in mind to maintain a balanced renal diet. Portion control is key when it comes to snacking, as overeating can easily lead to consuming too much potassium, phosphorus, or sodium. Instead of snacking throughout the day, try timing your snacks with your meals and choose nutrient-dense options that will leave you feeling satisfied.
In addition to portion control, nutrient balance is essential in creating kidney-friendly snacks. Incorporate a variety of your favorite vegetables and fruits into your snack choices for added fiber and vitamins. Hydration is also crucial for maintaining kidney health, so be sure to include hydrating options like watermelon or cucumber slices in your snack repertoire.
Get creative with your snack ideas by experimenting with new foods and flavors. Low-sodium crackers topped with hummus or guacamole make for a satisfying savory option. For something sweet, try dipping apple slices in almond butter or spreading mashed raspberries on whole-grain toast.
With some planning and creativity, you can enjoy guilt-free snacks while still following a renal-friendly diet.
Eating Out and Travel TipsGoing out to eat or traveling can be challenging for those following a renal-friendly diet, but with the right tips and tricks, it's possible to enjoy delicious meals while still managing kidney disease.
When eating out, look for restaurant options that offer low-sodium, low-potassium dishes. Many restaurants will also allow menu modifications to accommodate dietary restrictions, so don't hesitate to ask your server about making substitutions or leaving off certain ingredients.
If you're traveling, packing portable food options is key. Consider bringing kidney-friendly snacks like sliced fruits and vegetables, unsalted nuts and seeds, low-sodium crackers or rice cakes, and individual servings of hummus or guacamole.
If you'll be on a long flight or road trip where there may not be many healthy food options available, pack a cooler with pre-made meals like salads with lean protein or whole grain wraps with fresh veggies and chicken.
Don't let cultural cuisine deter you from enjoying dining experiences while managing your kidney disease. Research traditional dishes before visiting a new country or trying a new restaurant so you can identify any high-potassium ingredients and make informed choices.
Don't be afraid to ask questions or request modifications – most chefs are happy to accommodate dietary needs in order to create an enjoyable dining experience for their guests.
Getting Enough NutritionStaying healthy while managing kidney disease can be a challenge, but it's crucial to ensure you're getting enough nutrition to keep your body strong and resilient.
A balanced meal plan with the right amount of protein, carbohydrates, and healthy fats is essential for maintaining your health. Protein requirements may vary depending on the stage of your kidney disease and other health conditions you may have. It's important to work with a registered dietitian to determine the appropriate amount of protein for your individual needs.
In addition to eating balanced meals, nutrient supplements may be necessary to ensure you're getting enough vitamins and minerals. Your healthcare team may recommend specific supplements based on your lab results and medical history. It's important to follow their recommendations closely and not exceed recommended dosages.
Hydration is also an important aspect of nutrition for people with kidney disease. Drinking enough fluids helps flush out toxins from the body and keeps organs functioning properly. However, too much fluid intake can be harmful and can cause fluid buildup if you have advanced stages of kidney disease or are on dialysis. Work with your healthcare team to determine your recommended fluid limits.
Overall, it's important to pay attention to calorie intake as well as nutrient content when managing kidney disease. Eating small meals throughout the day can help ensure adequate calorie intake without overeating in one sitting. Snacks can also be a helpful way to boost calorie intake if needed, but make sure they're low in sugar, sodium, and phosphorus and compatible with your kidney health needs.
Frequently Asked QuestionsCan sugary snacks be included in a renal diabetes diet?Sugary snacks can be included in a renal diabetes diet, but it's important to manage cravings and choose alternative options when possible.
These types of snacks can have a significant impact on blood sugar levels, so portion control is key. Balancing macros is also crucial, as sugary snacks are typically high in carbohydrates and low in protein.
However, it's important to consult with your doctor before consuming sugary snacks, especially if you have diabetes.
To help manage cravings and make healthy choices, it's recommended to stick to healthy portion sizes for sugary snacks and drinks. A helpful way to do this is by using a table that outlines the serving sizes of common high-sugar snack options. Here is an example:
High-Sugar Snack Option | Serving Size
Hard Candies | 1 oz (28g)
Jelly Beans | 1 oz (28g)
Chocolate Pudding | ½ cup (110g)
Please note that these are general serving sizes and actual serving sizes may vary based on specific brands or types of snacks.
To satisfy sweet cravings, try incorporating fruits or low-sugar dessert options instead. If consuming sugary snacks, consult with your healthcare provider to ensure they fit within your individual dietary needs and daily limits.
As a CKD patient, it's important to be mindful of the ingredients in snack foods. Some specific ingredients to avoid include high levels of sodium, potassium, phosphorus, and calcium.
Instead, opt for kidney-friendly snack alternatives such as animal crackers, breadsticks, low-sodium crackers and tortilla chips, unsalted pretzels, or fruits and vegetables.
It's also important to maintain nutrient balance and portion control when snacking. Consult with your doctor or dietitian for personalized recommendations on snacks that are appropriate for your specific dietary needs.
Frequent snacking can have benefits for CKD patients on a kidney diet, as long as healthy snack choices are made. Kidney-friendly snack ideas include fruits and vegetables, low-sodium crackers, unsalted pretzels, unsalted breadsticks, and tortilla chips.
Snacks can also provide extra calories for kidney patients with weight management concerns. However, it's important to be mindful of snacking and blood sugar balance in patients with diabetes.
Healthy snacking tips for CKD patients include avoiding added phosphorus, limiting sodium intake, and consulting with a doctor or dietitian to determine appropriate protein intake.
Overall, snacks can be enjoyed in moderation as part of a well-planned kidney diet.
Snacking can be a helpful tool for managing CKD as long as you pay extra attention to nutritional value, portion control, snack timing, low sodium options, and convenience options.
Snacks can help increase your calorie intake if you struggle with poor appetite or unwanted weight loss. However, it's important to watch out for high sugar snacks that may be recommended if losing weight due to poor appetite as these may not be suitable for patients with diabetes.
Planning is required to include snacks on the kidney diet but they should be guilt-free and healthy while still being compatible with your kidney health needs. Patients with CKD should consult their doctor or dietitian to learn what snack foods are good for their specific condition.
If you're looking for protein-rich options that are also kidney-friendly, there are several nutritious nibbles you can choose from. Low sodium snacks like boiled eggs, roasted chickpeas, unsalted nuts or seeds, and low-fat cheese sticks are all examples of foods that can help increase your protein intake while avoiding harmful ingredients.
Kidney-friendly bites such as cottage cheese with fruit, hummus with sliced vegetables, or edamame beans can also add variety to your snack choices and provide additional nutrients like fiber and healthy fats.
Remember to consult with your doctor or dietitian before making any changes to your diet plan.
In conclusion, eating right for chronic kidney disease and diabetes can be challenging when it comes to finding suitable snacks. However, with the help of a registered dietitian and some planning, patients can still enjoy delicious and healthy options that meet their nutritional needs.
It's important to keep a food list handy and plan meals ahead of time for convenience choices. When it comes to snacking on a kidney-friendly diet, there are plenty of healthy options available such as fruits, vegetables, nuts, and low-sugar treats. However, it's also important to be mindful of high-sugar snack options and practice moderation.
Eating out and traveling can also present challenges, but with some preparation and communication with restaurant staff or travel accommodations, patients can still maintain their dietary needs.
Overall, by incorporating these tips and ideas into your routine along with guidance from a healthcare professional or registered dietitian, you can successfully manage both your chronic kidney disease and diabetes while still enjoying tasty snacks.
The post Snacks For CKD And Diabetes appeared first on Renal Diet HQ.
Suggested Reading:
Renal Vegetarian Diet Kidney Friendly Snacks Dietary Protein And The Kidney DietJune 17, 2023
Exercise Mistakes To Avoid With CKD
If you have chronic kidney disease (CKD), exercise is an essential part of maintaining a healthy lifestyle. Regular physical activity can help improve your overall health, reduce the risk of complications associated with CKD, and even slow kidney disease progression.
However, it is important to know how to exercise safely and avoid certain mistakes that could potentially harm you. In this article, we will discuss some common exercise mistakes to avoid if you have CKD, as well as provide tips for safe and effective exercising.
It is crucial to understand that not all exercises are suitable for individuals with CKD. Certain types of physical activities can put too much stress on your kidneys or exacerbate any existing health conditions you may have. Additionally, there are certain circumstances that should be avoided when exercising with CKD such as excessive heat exposure or dehydration.
By learning about these potential pitfalls and following safety guidelines, you can ensure that your exercise routine supports your overall health and well-being while minimizing risks. So let's dive in and explore some key strategies for avoiding exercise mistakes when living with CKD.
[feast_advanced_jump_to] Key TakeawaysJumping into vigorous exercise should be avoided for CKD patientsAvoid doing the same activities repeatedly to prevent boredom and potential injuryExercising after a large meal or before bedtime should be avoidedCKD patients should avoid exercising during the hottest times of the day and take proper precautions to avoid serious issues.
Key TakeawaysJumping into vigorous exercise should be avoided for CKD patientsAvoid doing the same activities repeatedly to prevent boredom and potential injuryExercising after a large meal or before bedtime should be avoidedCKD patients should avoid exercising during the hottest times of the day and take proper precautions to avoid serious issues.Importance of Physical FitnessFor More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
Hey, did you know that physical fitness is super important for everyone, including those with kidney disease?
Regular exercise has many benefits, as it can improve energy levels, strength, blood pressure and even help manage symptoms of chronic kidney disease (CKD).
Here are some specific benefits of exercise that can help individuals with CKD:
Improving endurance: Regular exercise improves cardiovascular health by lowering your risk of heart disease such as coronary artery disease, high cholesterol levels, as well as lowering your risks of heart attack. Exercise also helps increase the strength of your heart and lungs. This means you'll be able to do more activities without feeling tired or out of breath.Managing blood pressure: Exercise has been shown to lower blood pressure in CKD patients. High blood pressure is a common complication of CKD and can lead to further kidney damage if left untreated.Enhancing sleep quality: Exercise has been shown to improve the quality of sleep. A good night's rest is important for overall health as it allows your body time to repair and recharge.Boosting mood: Exercise releases endorphins, which can boost mood by reducing feelings of stress and anxiety. Individuals with CKD may experience depression due to the impact on their daily life, so regular exercise can be an important tool for improving mental well-being.Controlling body weight: Maintaining a healthy weight is important for people with CKD as being overweight or obese puts additional strain on the kidneys. Regular exercise combined with a healthy diet can help you with weight loss.Managing CKD symptoms: Exercise also plays a crucial role in managing chronic diseases such as CKD. By incorporating regular exercise into your routine, you may experience improvements in CKD symptoms such as muscle weakness and joint pain.Incorporating regular physical activity into your routine may seem daunting at first, but starting slow and gradually building up your routine will have long-term benefits for the management of patients living with CKD.
Consultation with a doctor before starting any new exercise program is highly recommended to ensure safe participation based on individual needs and abilities while avoiding potential risks associated with certain exercises or activities that could harm one's well-being over time, especially when done improperly or carelessly without proper supervision from qualified healthcare professionals who know what they're doing.
Remember, taking care of yourself through physical fitness can have long-term benefits for both your physical and mental well-being.
Exercise Mistakes to Avoid with CKDJumping right into vigorous exercise.Once you get your diagnosis of chronic kidney disease, you may feel the urge to sprint up and down your street in order to stay healthy. However, this can put you out of breath quickly, not to mention cause a great deal of pain – and even an injury that could put you out of action for a while.
If you haven't been active much before learning you have CKD, you want to start slow. Do a 5-10 minute warm up before each exercise session, letting your body get used to the activity before ramping up the pace. Increase your exercise duration or intensity a little each week (every 3-4 sessions) so that you don't cause a great deal of shock to your body.
Doing the same activities over and over again.Sure, being active at all is beneficial for your health. However, it's good to mix up your exercises to keep your body from getting too used to the movements. For example, you can do cardio (running, walking, or swimming) one day, then lightweight training the next. Alternating between activities also prevents boredom from setting in!
Forgetting to stretch after exercise.Stretching after exercise has many benefits as it leads to better blood flow and helps with back pain. Start at the top of your body, stretching your neck, shoulders, and arms. Work your way down, stretching your waist, back, and legs. Make sure you are breathing deeply to get oxygen to your spent muscles.
Not being consistent with your exercise.Being active on a sporadic basis isn't going to do much good if you are trying to manage your weight or blood pressure. You must have an exercise plan in place and follow through with it on a weekly basis. Speak to your doctor about developing a plan that works for you and your stage of CKD and also takes into consideration other medical conditions that you may have.
Exercising during the worst times of the day.When deciding the best time to work out, think about the rest of your schedule. You don't want to be active after a large meal or just before bedtime. If you are heading outdoors to exercise, avoid going during the hottest times of the day.
First thing in the morning is a good idea for many, so you can get it out of the way before you begin your day. Plus, it will be cooler during this time of day too!
While exercise is very beneficial to most chronic kidney disease patients, you need to make sure you aren't making any potentially dangerous mistakes when getting active. Have fun with your activities and make sure you are taking proper precautions to avoid any serious issues!
Consulting with a DoctorIt's essential to consult with a physician before starting any new physical activity program, as they can provide individualized recommendations and ensure safe participation based on unique needs and abilities.
Your doctor can help you determine the types of exercises that are best suited for your condition and level of fitness, as well as provide guidelines on how to gradually increase intensity and duration over time.
By consulting with your doctor, you can reduce the risks associated with exercise mistakes and ensure that you take appropriate precautions to avoid injury or other negative health outcomes.
Your doctor may also recommend modifications to your exercise routine based on any underlying health conditions or medications that could affect your ability to engage in physical activity safely.
By working together with your healthcare provider to develop an exercise plan tailored specifically to your needs, you can enjoy the many benefits of regular physical activity while minimizing potential risks.
Planning an Exercise ProgramConsulting with a doctor before starting an exercise program can ensure that you create a personalized plan that will help you feel stronger, more energetic, and better equipped to manage the symptoms of CKD.
When planning your exercise program, it's essential to consider the type of exercise, length of time, frequency, and intensity. Choosing continuous activities that use large muscle groups like walking or cycling are good options. Incorporating low-level strength exercises may also be beneficial but avoid heavy lifting.
In addition to selecting your exercises carefully, it's important to set achievable goals for yourself and track your progress regularly. Aim for at least 30 minutes of exercise per session building up gradually with time. Exercise at least three days a week on non-consecutive days.
Start out slowly and warm up before increasing intensity and cooling down after each session. Do not forget the importance of rest days as well!
Engaging in consistent physical activity is key to improving your health outcomes over time while incorporating variety into your routine can prevent boredom and keep you motivated towards achieving long-term fitness goals.
Types of ExerciseWhen it comes to getting active with CKD, finding a type of exercise that suits your interests and abilities can be key to staying motivated and enjoying the process.
Each type of exercise has unique benefits. Aerobic exercise is the best type of exercise for the heart, but resistance training is also important for people with CKD to prevent muscle weakness and joint pain. Flexibility exercises prevent stiffness and increase mobility, while balance exercises help reduce the risk of falls.
It's recommended that CKD patients aim for at least 30 minutes per exercise session at least 3 days a week. Resistance training should be done using lighter weights or bands if necessary. Modifications can be made to accommodate any physical limitations or health concerns.
Appropriate equipment should also be used, such as comfortable shoes with good support for walking or running.
Monitoring progress is important when starting an exercise program. Keep track of how you feel during and after each workout, as well as any changes in symptoms or overall health.
Incorporating variety into your routine can also help keep things interesting and prevent boredom. Remember that exercising regularly can have many benefits for those with CKD, including increased energy, improved strength and mobility, better blood pressure levels control, and a lower risk of falling.
Frequency and IntensityNow that you know the different types of exercise for people with CKD, let's discuss the frequency and intensity. It's important to start slowly and gradually increase the duration or intensity of your exercise program. A personalized approach is necessary, as each person's needs and abilities are different.
Here are three things to keep in mind when it comes to frequency and intensity:
Gradual Progression: Start with a low level of exercise and gradually increase over time. This will help prevent injury or shock to the body.Personalized Approach: Work with your doctor to develop an exercise plan that fits your individual needs and abilities.Monitoring Progress and Adjusting Intensity: Monitor how your body responds to exercise, such as heart rate, blood pressure, fatigue levels, etc. Adjust the intensity accordingly to ensure safety during physical activity.Remember to take safety precautions while exercising, such as warming up before starting any activity, stretching after finishing an activity, staying hydrated throughout the day, wearing appropriate clothing and footwear, avoiding extreme temperatures when possible (hot/cold), etc.
By following a safe approach with gradual progression and monitoring progress regularly with adjustments where necessary, you can help improve physical capacity without risking injury or complications from CKD symptoms like fatigue or joint pain!
Avoiding Certain CircumstancesTo ensure your safety while improving physical capacity, it's important to be aware of certain circumstances when you shouldn’t exercise. If you're experiencing fatigue or joint pain, it's best to consult with your doctor before engaging in any exercise program.
They can help you adapt your routine to suit your physical limitations and avoid causing further harm. Additionally, you should avoid exercising when you have a fever or when the weather is too hot and humid before consulting with your doctor.
Avoiding certain circumstances when exercising is crucial for CKD patients looking to improve their physical capacity safely. Consult with a healthcare professional if you're managing fatigue or experiencing joint pain, adapt your routine according to any physical limitations, and take extra precautions if pregnant.
Consider incorporating aquatic exercises into your routine for a low-impact workout that can provide many benefits for overall health.
Concerning SymptomsIt's important to pay attention to any concerning symptoms while engaging in physical activity, such as chest pain, difficulty breathing or leg cramps that prevent future exercise sessions. Managing these symptoms is critical for individuals with CKD, as they may be more prone to experiencing them due to their condition. Exercise modifications may be necessary depending on the severity of the symptom, such as reducing intensity or duration.
Monitoring progress during exercise is also essential for individuals with CKD. Keeping track of how you feel during and after an exercise session can help determine if adjustments need to be made in intensity or frequency. If symptoms persist or worsen despite making modifications, it's important to seek medical attention from a healthcare provider who understands your specific needs and limitations.
Adjusting the intensity of physical activity is another way to manage concerning symptoms. Gradual increases in intensity can help build endurance and strength over time without causing undue stress on the body. It's crucial not to push yourself too hard, especially when just starting an exercise program. By taking things slow and listening to your body, you can ensure that you're getting the most out of your workout while staying safe and healthy.
Exercising with a PartnerPartnering up with someone can make working out more enjoyable and help provide motivation to stick with a regular exercise routine. Here are some partner benefits, motivation tactics, communication strategies, workout variations, and fun activities to consider when exercising with a partner:
Partner Benefits: Working out with a partner can provide accountability and encouragement. It can also make exercising more social and increase the enjoyment of physical activity.Motivation Tactics: Set achievable goals together, celebrate progress, and encourage each other during workouts. Consider creating friendly competitions or challenges to keep things interesting.Communication Strategies: Openly communicate about fitness goals, concerns, and schedules to ensure both partners are on the same page. Provide feedback that's constructive and helpful.Workout Variations & Fun Activities: Mix up your workouts by trying new exercises or activities such as hiking, dancing, or yoga classes together. This will keep things fun while challenging your body in new ways.Overall, partnering up with someone for exercise has many benefits including increased motivation and enjoyment of physical activity. By setting achievable goals together, communicating openly about fitness goals and concerns, trying new workout variations, and fun activities – you can stay motivated while having fun!
Other Facts to ConsiderConsidering other factors, staying physically fit can help CKD patients with necessary tasks and still have energy for other activities. However, there are some exercise misconceptions that may prevent CKD patients from reaping the full benefits of physical activity. One common misconception is that exercise puts too much strain on already weakened muscles and bones. In reality, regular exercise can actually improve muscle and bone health in people with CKD.
Another important aspect of exercise that is often overlooked is its impact on mental health. Exercise has been shown to improve mood and reduce symptoms of depression and anxiety in people with chronic illnesses like CKD. Additionally, regular physical activity can help alleviate symptoms of fatigue commonly experienced by CKD patients.
Motivation for exercise can sometimes be challenging for anyone, but especially for those living with a chronic illness. It's important to remember that there are many different types of exercises available, so finding something you enjoy doing is key. Additionally, proper nutrition plays a crucial role in supporting an active lifestyle. Eating a special diet designed for kidney patients can provide the fuel your body for exercise without compromising your safety.
By incorporating regular exercise into your routine and making healthy food choices, you can take control of your health and improve your overall well-being as a person living with CKD.
Exercise MisconceptionsFactsExercise puts too much strain on weakened muscles/bonesRegular exercise improves muscle/bone health in people with CKDExercise does not benefit mental healthExercise improves mood/reduces symptoms of depression/anxietyMotivation for exercise is difficultFinding enjoyable activities & proper nutrition supports an active lifestyleFrequently Asked QuestionsWhat are some specific exercises that should be avoided for CKD patients?As a CKD patient, it's important to choose low impact exercise options that won't put undue stress on your cardiovascular system. Avoid exercises that involve high intensity or sudden movements, as well as those that require heavy lifting.
Additionally, take precautions by incorporating strength training modifications such as using lighter weights or resistance bands. Flexibility exercises, such as yoga and stretching, can also be beneficial for improving mobility and reducing the risk of injury.
Remember to always consult with your doctor before beginning any exercise program and monitor for any cardiovascular risks during activity.
Exercise benefits people with CKD by improving their physical function, energy levels, and blood pressure control. However, it is important to consult with a doctor before starting an exercise program and to take precautions to avoid worsening symptoms.
Gradually increasing exercise frequency and intensity, choosing recommended activities, taking breaks when feeling tired or short of breath, and staying hydrated are all important measures to take. It is also important to avoid exercising during times of illness or after changes in medication schedules.
Consistency is key for reaping the benefits of exercise for CKD patients, but it should be done with caution and proper guidance from healthcare professionals.
When exercising with CKD, it's important to follow certain dietary restrictions and recommendations. Recommended foods include lean proteins, fruits, vegetables, whole grains, and low-fat dairy products.
People with CKD often need to limit their protein intake, as excessive protein can put strain on the kidneys. However, protein is still important for muscle repair and during recovery.
It is recommended to consume moderate amounts of high-quality protein sources, such as lean meats, fish, and poultry. However, you should avoid protein supplements like protein powders, shakes, and protein bars unless they have been approved by your doctor or dietitian.
Hydration is also crucial, as dehydration can worsen kidney function. It's recommended to drink water before, during, and after exercise. However, you may have to avoid excess fluids with advanced kidney disease. You should also avoid sports drinks as they contain sodium and potassium.
Supplements may be necessary for some individuals with CKD to ensure they're getting enough nutrients. Timing considerations should also be taken into account - it's best to wait at least an hour after a meal before exercising and avoid exercising close to bedtime.
Pre-workout snacks should consist of easily digestible carbohydrates such as fruit or crackers. Consult with a doctor or dietitian for personalized recommendations based on individual needs and preferences.
Regular exercise is important for people with kidney disease as it can improve energy levels, increase strength, lower the risk of falls, and improve blood sugars and blood pressure.
The benefits timeline for a regular exercise program varies from person to person depending on the individual's health status and exercise frequency and intensity levels. It typically takes a period of time between several weeks to months to see significant improvements in health.
It's important to consult with a doctor before starting an exercise program and develop personalized routines with medical supervision. Starting slowly and gradually increasing intensity levels while avoiding overexertion is crucial for preventing injury or complications.
With consistent effort, CKD patients can experience improved physical function and overall quality of life through regular exercise.
When considering team sports or high-impact activities with CKD, it's important to conduct a thorough risk assessment and consult with your healthcare team. Modifications to equipment may be necessary, such as wearing protective gear or using appropriate footwear. Gradual progression is key, starting at a low intensity and gradually increasing over time.
Hydration management is also crucial during exercise, as dehydration can exacerbate kidney function issues. Communication with your healthcare team is essential for monitoring any potential changes in your condition and adjusting your exercise plan accordingly. While these activities can be enjoyable, safety should always come first for those with CKD.
Congratulations! You've learned about the importance of exercise for those with chronic kidney disease (CKD) and common exercise mistakes to avoid. It's important to consult with your doctor before starting any new exercise program and to plan an appropriate routine based on your individual needs.
Always choose exercises that are low-impact and avoid certain circumstances such as exercising in extreme temperatures. Be aware of concerning symptoms such as chest pain or shortness of breath, and consider exercising with a partner for added safety.
To reap the benefits of exercise while avoiding potential harm, follow these guidelines. By safely incorporating physical activity into your daily routine, you can keep your kidney healthy and improve your overall health and wellbeing.
Remember that physical fitness is crucial for maintaining a healthy lifestyle, particularly if you have CKD. Regular exercise can help manage CKD symptoms, reduce the risk of complications associated with the disease, and improve quality of life. So get moving today!
The post Exercise Mistakes To Avoid With CKD appeared first on Renal Diet HQ.
Suggested Reading:
Exercise For CKD Patients Exercise For Healthy Heart Early Stage Kidney DiseaseJune 16, 2023
Questions About The Kidney Disease Diet
If you or a loved one has been diagnosed with chronic kidney disease (CKD), you may be wondering how diet plays a role in managing the condition. The truth is, what you eat can have a significant impact on your kidney function and overall health.
With so much information available online, it can be overwhelming trying to navigate the dos and don'ts of a kidney-friendly diet. In this article, we will address some common questions about the kidney disease diet and provide evidence-based answers to help guide you on your journey towards healthy kidneys.
You might be wondering: How does diet affect CKD? Can a vegetarian diet help manage CKD? Is protein harmful for CKD patients? Are nuts and seeds safe to eat?
These are just some of the many questions that individuals with CKD may have when it comes to their dietary choices. It's important to note that there is no one-size-fits-all approach to nutrition for those living with CKD, as each person's needs may vary based on factors such as stage of the disease, age, gender, and other medical conditions.
However, by working closely with your healthcare team and following evidence-based recommendations, you can make informed decisions about what foods to include or avoid in your daily meals.
[feast_advanced_jump_to]Key Takeaways A low-protein diet may help slow the progression of CKD, and plant-based proteins like beans, lentils, and tofu provide an excellent source of nutrition.Specific diet restrictions may be recommended based on individual needs, such as limiting high-potassium or high-phosphorus foods.Healthy lifestyle changes such as quitting smoking, regular exercise, and maintaining a healthy weight can help manage CKD.Consulting with a registered dietitian who specializes in renal nutrition can help ensure meeting nutritional needs and creating a personalized meal plan that meets your nutrition guidelines while also incorporating your favorite foods.
A low-protein diet may help slow the progression of CKD, and plant-based proteins like beans, lentils, and tofu provide an excellent source of nutrition.Specific diet restrictions may be recommended based on individual needs, such as limiting high-potassium or high-phosphorus foods.Healthy lifestyle changes such as quitting smoking, regular exercise, and maintaining a healthy weight can help manage CKD.Consulting with a registered dietitian who specializes in renal nutrition can help ensure meeting nutritional needs and creating a personalized meal plan that meets your nutrition guidelines while also incorporating your favorite foods.How Does Diet Affect Chronic Kidney Disease (CKD)?For More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
You'll need to be mindful of what you eat, as each bite can either help or harm your kidneys - think of your diet as a tool for managing CKD.
Dietary restrictions are essential in managing CKD. Your doctor may recommend limiting foods that are high in sodium, potassium, and phosphorus. You should also limit your intake of protein since too much protein can cause damage to the kidneys.
Nutrient intake is crucial when following a kidney-friendly diet. You'll want to focus on consuming foods that are low in sodium, potassium, and phosphorus while still getting enough nutrients to support your overall health.
Meal planning can help ensure you're eating the right foods in the right amounts. Work with a registered dietitian who specializes in renal nutrition to develop a meal plan that meets your individual needs.
Fluid management is another critical aspect of a kidney-friendly diet. For early stage kidney disease, it may be recommended to drink 8 glasses of water each day to keep your kidneys working well. However, your doctor may recommend limiting extra fluids if you have fluid retention or if you're on dialysis.
Lifestyle changes such as quitting smoking, exercising regularly, and maintaining a healthy weight can also help manage CKD. By making these changes and following a healthy eating plan, you can improve your overall health and reduce symptoms associated with CKD.
Can diet reverse CKD?Eating certain foods and making lifestyle changes can potentially improve kidney function in those with chronic kidney issues. While diet can't cure CKD, it can help manage the condition and slow kidney disease progression. Nutritional therapy is a crucial aspect of disease management for individuals with CKD.
Dietary restrictions are necessary for those with CKD to avoid putting more stress on their kidneys. A diet low in sodium, potassium, and phosphorus is typically recommended.
Consuming foods high in these minerals can lead to complications such as high blood pressure levels and bone problems. Additionally, limiting protein intake may also be necessary to reduce the workload on the kidneys.
In addition to dietary restrictions, lifestyle changes can also improve kidney function. Maintaining a healthy weight through regular exercise can not only benefit overall health but also reduce the risk of further decline of kidney function.
Managing blood sugar levels if you have diabetes is also crucial since uncontrolled diabetes can cause further damage to the kidneys. Quitting smoking and controlling blood pressure are other lifestyle changes that can help slow down the progression of CKD.
Who needs to make dietary changes for CKD?Any person that has been diagnosed with any stage of chronic kidney disease should start making dietary changes immediately. The sooner you make changes and start living a healthy lifestyle, the better your overall health and well-being will be. In fact, the earlier you start the easier it is to stop or slow the progression of kidney failure. You could effectively stop your illness in its tracks and avoid end-stage kidney disease by acting now.
Is protein harmful for CKD patients?Protein can be harmful for individuals with chronic kidney issues, potentially leading to further damage and complications. The kidneys are responsible for filtering waste products from the bloodstream, including excess protein.
When kidney patients consume too much protein, their kidneys may not be able to filter it properly. This can lead to a buildup of waste products in the blood, which can cause further damage to the kidneys over time.
It's important for those with CKD to find a nutritional balance that meets their dietary restrictions while providing adequate protein intake. Recommended daily protein intake levels vary based on individual factors such as age, sex, and activity level. However, most patients with CKD should aim for a lower protein diet than what is typically recommended for healthy people.
There are several alternatives to traditional high-protein sources such as meat and dairy that can help patients manage their protein intake. Plant-based proteins like beans, peas, lentils, and tofu provide an excellent source of nutrition without putting added strain on the kidneys.
Additionally, working closely with a registered dietitian or healthcare provider can help ensure that individuals with CKD adhere to proper dietary guidelines and avoid potential complications related to excessive protein intake.
Can a vegetarian diet help manage CKD?A plant-based approach to managing chronic kidney issues can be a healthy and flavorful way to support your body's needs. A vegetarian diet can provide numerous benefits, including keeping your kidney disease from getting worse and reducing the risk of complications associated with kidney disease.
Additionally, plant-based diets are often rich in fiber, vitamins, and minerals that can help reduce inflammation and protect against chronic diseases. If you choose to adopt a vegetarian diet for managing your chronic kidney issue, it's important to pay attention to protein sources.
While meat is a common source of protein in many diets, there are plenty of plant-based options available such as beans, lentils, tofu, and quinoa. These foods contain high-quality proteins that can help maintain muscle mass and support overall health.
However, it's important to note that nutrient deficiencies are possible on a vegetarian or vegan diet if meal planning is not done properly. It may be necessary to supplement certain vitamins or minerals such as vitamin B12 or iron.
Consulting with a registered dietitian who specializes in renal nutrition can help ensure that you're meeting all of your nutritional needs while following a plant-based diet for managing CKD.
Can a low-protein diet slow the progression of CKD?Limiting intake of protein may help slow the progression of chronic kidney issues. This type of diet reduces the amount of protein that your body needs to metabolize, which can ease the workload on your kidneys.
However, it is important to note that not all patients with CKD need to follow a low-protein diet, and the specific guidelines for protein intake will depend on individual factors such as stage of CKD, age, sex, and activity level.
To determine if a low-protein diet is right for you, it is important to consult with a registered dietitian who specializes in kidney disease nutrition. They can provide personalized guidance on how much protein you should be consuming each day. In addition, they can offer tips and recipes for incorporating protein alternatives into your meals. Some sources of plant-based proteins include beans, lentils, tofu, nuts and seeds.
While reducing protein intake has been shown to have benefits for slowing the progression of CKD, it is also important to consider potential drawbacks such as muscle loss. Maintaining adequate muscle mass is important for overall health and quality of life. Therefore, it is recommended that individuals following a low-protein diet also engage in regular physical activity to prevent muscle loss and consume enough calories from other food sources to meet their energy needs.
By working closely with a healthcare team and following personalized guidelines for protein intake and physical activity levels, individuals with CKD may be able to slow the progression of their condition while maintaining optimal muscle mass and overall health.
Protein Intake GuidelinesStage 1-2: < 0.8 grams/kgStage 3-5: < 0.6 grams/kgTable: Recommended daily protein intake guidelines based on stage of CKD. Source: National Kidney Foundation.
Is a low-carb diet safe for someone with CKD?Following a low-carb diet may not be safe for individuals with chronic kidney issues, as it can put additional strain on the kidneys. This is because when you consume fewer carbohydrates, your body produces ketones, which are acidic substances that need to be excreted by the kidneys. If your kidneys are already damaged, they may struggle to handle this extra workload and lead to further complications.
However, there are still low-carb options available for those with CKD. You can opt for healthy, low-carb foods such as non-starchy vegetables, nuts, and seeds, and lean protein sources like fish or chicken. Additionally, alternative diets such as the Mediterranean diet or DASH have shown benefits in managing CKD without putting undue stress on the kidneys.
It's important to keep in mind that any dietary restrictions should be discussed with your healthcare provider or a registered dietitian who specializes in kidney disease. They can provide you with individualized meal planning strategies that meet your specific nutritional needs while taking into account any potential risks associated with certain diets.
By following a well-balanced and personalized meal plan, you can effectively manage CKD while maintaining good overall health.
How does weight loss affect CKD?If you have CKD, weight loss can have significant benefits. Losing weight can improve blood pressure, reduce the risk of heart disease, and slow the progression of kidney disease. However, it is important to approach weight loss with caution and under medical supervision.
Following a kidney-friendly eating plan is crucial for managing CKD. Your healthcare provider may recommend specific diet restrictions based on your individual needs. For example, they may advise limiting foods high in potassium or phosphorus. It is also important to maintain adequate protein intake while reducing calorie consumption for weight loss.
In addition to dietary changes, exercise recommendations may be made by your healthcare provider. Regular physical activity can help with weight loss and improve overall health outcomes for those with CKD. Incorporating lifestyle changes such as healthy eating habits and exercise into your daily routine can help manage symptoms and improve quality of life. Remember that any changes should be made under medical supervision to ensure safety and effectiveness.
Benefits of Weight LossDiet RestrictionsExercise RecommendationsImproves blood pressureLimiting high-sodium or high-phosphorus foodsIncorporate regular physical activityReduces risk of heart diseaseMaintaining adequate protein intake while reducing caloriesFollow healthcare provider's recommendationsSlows progression of kidney diseaseMaintaining adequate potassium intakeExercising for at least 150 minutes per weekOverall, if you have CKD and are considering weight loss as part of your treatment plan, it is important to work closely with your healthcare provider to determine the best course of action for you. A combination of dietary changes, exercise recommendations, and medical supervision can lead to better outcomes in managing symptoms and improving quality of life.
By incorporating these lifestyle changes into your daily routine, you can take control of your health journey and serve yourself in the best way possible.
Are there any drinks I should avoid with CKD?Steering clear of certain beverages is crucial for those with CKD to manage their condition effectively. Here are some drinks that you should avoid when dealing with CKD:
Soda: Carbonated drinks can lead to an increase in blood phosphorus and sugar levels, which can be harmful to your kidneys.Alcohol: Drinking alcohol can cause many harms, including dehydration and disruption of electrolyte balance in your body, in addition to leading to further kidney damage.Herbal teas: While many herbal teas have health benefits, some may contain high levels of potassium or other minerals that could harm your kidneys. Be sure to talk to your doctor before consuming any herbal teas.Energy drinks: Similar to soda, these beverages often contain large amounts of phosphorus and sugar, both of which can stress your kidneys and contribute to further damage.Staying hydrated is important for managing CKD, but it's also important to choose hydrating beverages wisely. Opt for water or kidney-friendly fruit juices instead of sugary sodas or energy drinks. If you do choose a sports drink, make sure it doesn't contain too much potassium or phosphorus.
Avoiding certain beverages is essential for managing CKD effectively. Consult with your kidney doctor about the best beverage choices for you based on the current stage of your CKD and follow these tips above to help keep yourself hydrated and healthy!
How much sodium should I consume if I have CKD?To effectively manage your condition and promote kidney health, it's important to limit your daily sodium intake to a certain amount if you have CKD. Sodium is an essential mineral that helps regulate blood pressure and fluid balance in the body, but excess water can cause fluid buildup for people with kidney problems.
The recommended daily sodium intake for individuals with CKD is less than 1,500 milligrams per day.
Fluid intake management is also crucial when it comes to managing CKD. Consuming too much sodium can cause excessive thirst and lead to increased fluid retention in the body, which can put more strain on the kidneys.
To help maintain a healthy fluid balance, aim to drink enough fluids throughout the day while also limiting your sodium intake. You may also need to monitor your potassium levels and adjust your meal planning accordingly.
It's important to note that dietary restrictions may vary depending on the stage of CKD you're in and any other underlying health conditions you may have. Your healthcare provider or registered dietitian can help you develop a personalized meal plan that takes into account your individual nutritional needs and limitations.
By following a balanced diet that includes appropriate amounts of sodium, managing fluids properly, and staying hydrated, you can help support your overall kidney function and improve your quality of life.
How much potassium should I consume with CKD?You should aim to consume a moderate amount of potassium if you have chronic kidney problems, as it plays an important role in maintaining healthy heart and muscle function. However, too much of this mineral can be harmful, leading to hyperkalemia or high levels of potassium in the blood. It's essential that you monitor your potassium intake and follow any restrictions set by your healthcare provider.
Hyperkalemia can cause symptoms such as muscle weakness, tingling, numbness, heart palpitations, and shortness of breath.
Potassium can be found in many foods such as fruits, vegetables, dairy products, and meats. Some examples of potassium-rich foods include bananas, oranges, spinach, sweet potatoes, tomatoes, and salmon. While these foods are generally considered healthy for most people, those with CKD may need to limit their intake due to their increased risk for developing hyperkalemia.
Your healthcare provider may also recommend taking potassium supplements if your diet alone doesn't provide enough of this mineral. However, it's crucial to follow the prescribed dosage carefully as taking too much can cause serious health complications.
Regular monitoring of your potassium levels through blood tests is also necessary to ensure that they remain within a safe range while on a kidney disease diet plan.
How much phosphorus is safe for me to consume with CKD?Consuming too much phosphorus can be harmful for those with chronic kidney problems, as it can lead to bone and heart complications. Safe phosphorus intake is important for individuals with CKD, as the kidneys are not able to filter excess amounts of this mineral from the body.
High phosphorus foods such as dairy products, meat, fish, and whole grains should be limited or avoided altogether. Phosphorus binders may also be prescribed by a healthcare provider to help manage dietary phosphorus levels. These medications work by binding with excess phosphorus in the digestive tract before it is absorbed into the bloodstream. However, it's still important to follow a low-phosphorus diet even when taking these medications.
Regular testing of phosphorus levels is also recommended for individuals with CKD. This allows healthcare providers to monitor how well dietary interventions and medication management are working in controlling blood phosphorus levels. Overall, managing dietary phosphorus intake is crucial for those living with CKD in order to prevent complications and maintain overall health.
Are nuts and seeds harmful for someone with CKD?Nuts and seeds can be problematic for individuals with CKD due to their high phosphorus content. These foods are often touted as healthy snacks due to their high nutrient content, but they can also contain a significant amount of phosphorus. This mineral is important for bone health, but it can accumulate in the blood when kidney function is impaired, leading to complications such as bone disease and cardiovascular problems.
To maintain nutritional balance while managing your kidney disease diet, it's important to practice portion control when consuming nuts and seeds. Stick to small servings and avoid eating them on a daily basis. You can also try soaking or roasting these foods before consumption to decrease their phytate content, which is a storage form of phosphorus.
Additionally, hydration management is crucial for individuals with CKD, so make sure you're drinking enough water throughout the day to help flush out excess minerals.
While nuts and seeds may pose some challenges for those with CKD, they do offer many health benefits if consumed in moderation. They are rich in heart-healthy fats, fiber, vitamins, and minerals that play an important role in overall health. To optimize nutrient absorption from these foods, consider using food preparation techniques such as grinding or blending them into smoothies or spreads rather than consuming them whole.
With careful planning and attention to your food plan, you can still enjoy the many benefits of nuts and seeds while managing your kidney disease.
What types of fats should I eat with CKD?Optimizing your fat intake with CKD involves choosing the right types of fats that can help promote heart health and overall well-being. Healthy fats, like omega 3 sources, are essential for maintaining a nutrient balance and reducing inflammation in the body.
Omega 3 sources include fatty fish such as salmon, mackerel, and sardines, as well as flaxseed oil or chia seeds. It's also important to pay attention to cooking methods when consuming fats.
Opt for healthy oils like olive oil or avocado oil which have anti-inflammatory properties. Additionally, keeping portion control in mind is crucial; even healthy fats should be consumed in moderation to avoid weight gain which can lead to further complications.
Incorporating healthy fats into your diet can be beneficial for those with CKD by reducing inflammation and promoting heart health. Choosing the right sources of omega 3s along with mindful cooking methods and portion control can help maintain a balanced diet while managing kidney disease symptoms. Consult with a registered dietitian specialized in kidney disease management for personalized recommendations on optimizing your fat intake with CKD.
How can a dietitian help with my CKD diet?Working with a registered dietitian can be incredibly helpful in managing your CKD nutrition plan, as they can provide personalized recommendations and support to help you achieve optimal health. Here are some benefits of working with a dietitian:
Personalized Plan: A dietitian can create a proper nutrition plan that is tailored specifically to your needs, taking into account your medical history, lifestyle, and food preferences. This personalized approach ensures that you're getting the nutrients you need without compromising on taste or convenience.Meal Preparation: A dietitian can also help with meal planning and preparation, making it easier for you to stick to your nutritional goals. They can provide recipes and cooking tips that are kidney-friendly and easy to prepare at home.Grocery Shopping: Knowing what foods to buy at the grocery store can be challenging when following a CKD diet. A dietitian can teach you how to read food labels and identify ingredients that may be harmful to your kidneys. They can also recommend healthy alternatives that'll keep you feeling satisfied.In addition to these benefits, working with a dietitian may also involve lifestyle changes such as increasing physical activity or reducing stress levels. By taking a holistic approach to your health, a registered dietitian can help you manage CKD more effectively and improve your overall quality of life. So if you're struggling with your CKD nutrition plan, consider reaching out for professional support from a registered dietitian today!
Are there any kidney-friendly recipes available for CKD patients?Looking for tasty recipes that are healthy and safe for your kidneys? You're in luck! There are plenty of kidney-friendly cuisine options to choose from.
When it comes to recipe ideas, it's important to keep in mind the dietary restrictions that come with CKD. This means limiting foods high in phosphorus, potassium, and sodium.
Meal planning is key when following a CKD diet. A registered dietitian can help you create a personalized meal plan that meets your nutrition guidelines while also incorporating your favorite foods. They can also provide you with kidney-friendly recipe ideas and cooking tips.
Some popular options include roasted vegetables with herbs, grilled chicken or fish with lemon and garlic seasoning, and quinoa salad with fresh veggies.
When it comes to kidney-friendly cuisine, there are many delicious and nutritious options available. By working closely with a dietitian and experimenting with new recipes, you can still enjoy flavorful meals while maintaining a healthy diet that supports your kidney health.
So why not try something new today? Your taste buds - and your kidneys - will thank you!
Check Out Our Meal Plans For People With Chronic Kidney Disease (CKD)A Kidney Diet Is Essential To Manage Kidney DiseaseIn conclusion, managing your diet is crucial in the management of chronic kidney disease (CKD). Your diet should be tailored to meet your specific needs and goals by a registered dietitian.
Eating a balanced diet rich in fruits, vegetables, and whole grains while limiting sodium, protein, and phosphorus intake can help slow down the progression of CKD. However, it's important to note that no one diet fits all when it comes to CKD management.
Vegetarian diets may also be beneficial for those with CKD as they're naturally low in protein levels and have been shown to prevent or delay the onset of kidney disease.
In addition, incorporating healthy fats such as olive oil and nuts into your diet can provide numerous health benefits without compromising the level of kidney function.
By working closely with a registered dietitian and making mindful food choices, you can improve your overall health and quality of life while managing CKD.
The post Questions About The Kidney Disease Diet appeared first on Renal Diet HQ.
Suggested Reading:
Stage 4 Kidney Disease Diet The Importance Of Diet For Stage 3 Chronic Kidney Disease Dietary Protein And The Kidney DietJune 15, 2023
How Quickly Will My Chronic Kidney Disease Progress To Dialysis
Are you worried about how quickly your chronic kidney disease (CKD) will progress to dialysis? It's a valid concern, but the progression of CKD can actually vary greatly from person to person.
Your lifestyle, genetics, and other factors all play a role in how fast your renal function declines. In this article, we'll explore the different stages of kidney disease, the indicators and predictors of progression, and lifestyle changes that can help slow down decline.
By understanding more about how your CKD may progress and taking steps to manage it proactively, you can feel more confident in your ability to serve others while living with this condition.
[feast_advanced_jump_to] What Are The Stages of CKD?
What Are The Stages of CKD?As you go through the stages of chronic kidney disease (CKD), it's important to understand the changes happening in your body and how they can affect your overall health.
There are five stages of CKD, with stage one being the mildest and stage five being end-stage renal disease (ESRD). In the earlier stages, you may not experience any symptoms, but as your kidneys continue to decline in function, symptoms may arise, such as fatigue, swelling in the legs or feet, dry skin, and itching.
In stages one and two of CKD, there's a mild loss of kidney function and some signs of kidney damage. While you may still not experience any noticeable symptoms of kidney disease during this stage, it's important to make lifestyle changes such as eating a healthy diet low in sodium to slow down CKD progression.
Stage three is when kidney function drops significantly and patients may begin experiencing symptoms such as high blood pressure or anemia.
Stage four is when kidney function has declined severely and dialysis or a kidney transplant may be necessary soon. It's essential to work closely with your healthcare team during this time to manage complications and prepare for treatment options.
Understanding these stages can help you take charge of your health by making informed decisions about lifestyle modifications that can help slow down progression towards dialysis.
Factors Affecting ProgressionFor More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
Understanding the factors that impact the advancement of kidney disease can be crucial for those worried about its potential effects. There are several factors that can affect how quickly your chronic kidney disease progresses to dialysis.
These may include underlying health conditions, such as high blood pressure or diabetes, which can worsen kidney function over time. Additionally, certain lifestyle choices and habits, such as smoking or not following a proper diet, can also contribute to a faster progression of the disease.
Other factors that play a role in the progression of CKD include age and genetics. As you get older, your kidneys naturally begin to lose function, making it more difficult for them to filter waste products from your blood properly. Similarly, if you have a family history of kidney disease or other related conditions, you may be at higher risk for developing CKD yourself.
It is essential to keep these factors in mind when monitoring your kidney function and working with your healthcare provider to manage any underlying conditions.
While there is no way to predict exactly how quickly your chronic kidney disease will progress towards dialysis, understanding the various factors that impact its advancement can help you take steps towards managing the disease effectively. By staying on top of any underlying health concerns and making positive lifestyle changes where necessary, you may be able to slow down or even halt the progression of CKD altogether.
Remember that early detection and treatment are key when it comes to managing this condition successfully.
Indicators of ProgressionTo effectively monitor the progression of your kidney disease, it's important to be aware of the various indicators that can signal a decline in kidney function.
One key indicator is a decrease in your estimated glomerular filtration rate (eGFR), which measures how well your kidneys are filtering waste from your blood. A drop in eGFR may suggest that your condition is worsening and may indicate the need for closer monitoring or more aggressive treatment.
Another indicator of progression is an increase in proteinuria, which means there's an abnormal large amount of protein in your urine. This can be a sign that your kidney damage has increased and that you're at higher risk of heart disease, stroke, and other complications. Your kidney doctor may recommend additional tests or medication to help manage this symptom and slow down further damage.
Finally, high blood pressure can also be an indicator of worsening kidney function. Over time, high blood pressure can cause damage to the tiny blood vessels in the kidneys, leading to decreased function and eventually dialysis or transplant. It's important to work with your healthcare team to manage hypertension through lifestyle changes and medication if necessary, as this can significantly slow down the progression of chronic kidney disease.
Difficulties in PredictionPredicting the future of your kidney health can be a real headache, with no surefire way to tell what might happen next. While there are some indicators that doctors can use to estimate how quickly your CKD will progress to dialysis, these predictions aren't always accurate.
One difficulty is that every patient's experience with CKD is unique. Even if two people have the same stage of CKD and similar medical histories, their rates of progression may differ. This means it's difficult to create one-size-fits-all guidelines for predicting CKD progression.
One of the reasons why it’s difficult to predict how quickly CKD will progress is that multiple factors can influence the speed of progression. Some of these factors include the following:
Overall Health: Your overall physical and mental wellness will play a role in how quickly your kidney function declines.
Medications: Certain medications like ACE inhibitors or ARBs can slow down the rate at which kidneys deteriorate, while others can cause further damage to the kidneys.
Blood Pressure: High blood pressure puts extra strain on kidneys leading them towards damage.
Blood Sugar Levels: Poorly controlled diabetes accelerates the rate of kidney damage.
Proteinuria: Increased amounts of protein in urine indicate increased kidney damage.
Additionally, factors such as age, sex, race, and other health conditions can all affect how rapidly CKD progresses.
Another challenge in predicting CKD progression is that symptoms don't always match up with the severity of the disease. For example, someone with advanced-stage CKD may not have any noticeable symptoms at all. On the other hand, someone with early-stage CKD may experience swelling or other symptoms that suggest more advanced disease than they actually have.
Finally, it's worth noting that while dialysis is often seen as the ultimate endpoint for those with severe CKD, it's not always necessary or appropriate for everyone. Depending on your overall health and goals of care, you may be able to manage your kidney disease without ever needing dialysis. So even if your doctor predicts rapid progression to end-stage renal disease (ESRD), there is still hope for managing your condition effectively without undergoing dialysis treatment.
In summary, predicting how quickly your CKD will progress to dialysis can be challenging due to the unique nature of every patient's experience with the disease. Symptoms may not always match up with severity, and factors such as age, sex, race, and other health conditions can all affect the progression rate.
However, by working closely with your doctor and paying attention to indicators such as overall health, medication use, systolic blood pressure, and sugar levels, you can take steps towards slowing down or even stopping its progression. Remember that while dialysis is often seen as a last resort for those with severe CKD, it may not be necessary or appropriate for everyone.
Lifestyle ChangesIf you want to take control of your kidney health, making lifestyle changes can be a great place to start. It's important to remember that CKD progresses slowly over time, and making positive lifestyle changes can help slow down its progression. A healthy diet rich in fruits, vegetables, and lean meats can improve blood pressure and maintain kidney function.
Another important lifestyle change to consider is regular physical activity. Exercise promotes overall health by maintaining a healthy weight, reducing stress levels, and lowering your risk of cardiovascular disease. However, it's important to consult with your healthcare provider before starting any new exercise regimen or if you have other medical conditions that may affect your ability to exercise.
Finally, quitting smoking and limiting alcohol consumption are also crucial steps in managing CKD. Both smoking and excessive alcohol intake can worsen kidney function by increasing blood pressure and damaging blood vessels in the kidneys.
Taking small steps towards a healthier lifestyle can make a big difference in slowing down the progression of CKD and improving overall health outcomes.
Follow The Correct Meal Plan To Stop The Progression Of Kidney DiseaseDialysis can be a very scary endpoint to look forward to and I completely understand your desire to prevent placement on dialysis. Regardless of how much protein you have in your urine or what stage of kidney disease you are in, as long as it's pre-dialysis, you can slow the progression through the implementation of a healthy diet.
If you're in stages one or two of pre-dialysis kidney disease, you should work hard to control your blood pressure, diabetes, and any sort of heart disease that you have. If you need meal plans to help you prepare nutritious yet delicious meals, you can check out our meal planning program for Free 7 Day Meal Plan. Stage 1 kidney disease diet is really just eating more fruits and vegetables as well as less sodium and managing your weight.
If you've progressed to stages three or four of pre-dialysis kidney disease, you should look into our meal plans that we have on the renaldiethq.com website to help you manage the low-protein and diabetes meal plan that you need to also have nutritious and delicious meals. Your stage is often affected by many things and you can be in chronic kidney disease stage IIIB which is a little higher priority and a little stricter than the diet for CKD Stage 1. Stage III kidney failure means you really need to start working to control protein and sodium in your diet in addition to making it a priority to maintain excellent blood pressure control.
Medication and DiscontinuationIn addition to following a kidney-friendly diet, you can also manage your kidney health with medication and by discussing options for discontinuing medications that may harm your kidneys.
Medications are commonly used to treat the complications associated with CKD, such as high blood pressure, anemia, and bone disease. Taking these medications as prescribed can help slow down the progression of CKD, which may delay the need for dialysis or a kidney transplant.
However, it's important to note that some medications can actually harm your kidneys and worsen CKD. That's why you should discuss all of your medications with your healthcare provider, including over-the-counter drugs and supplements.
Your provider may recommend changing or stopping certain medications to prevent further damage to your kidneys. It's crucial to follow their recommendations carefully.
To effectively manage your kidney health through medication, here are three tips:
Take all prescribed medications exactly as directed by your healthcare provider.Discuss all of your current medications with your provider to identify any that might be harmful to your kidneys.Be aware of potential side effects and report any new symptoms or changes in how you feel to your healthcare provider immediately.Remember that managing CKD requires a comprehensive approach that includes lifestyle changes, regular medical care, and taking prescribed medication. By being proactive about managing both the benefits and risks of medication use in CKD, you can take control of this aspect of your health journey and make progress towards preserving kidney function for as long as possible.
Risk Factors for Rapid DeclineManaging your kidney health with medication is vital, but it's also important to be aware of the risk factors for rapid decline.
Chronic kidney disease can progress quickly in some individuals, leading to a higher likelihood of needing dialysis. Some of the factors that contribute to this include age, genetics, and underlying medical conditions such as high blood pressure or diabetes.
Age is a significant factor when it comes to the progression of chronic kidney disease. As we age, so do our kidneys. Typically, people above the age of 60 are more likely than not to develop CKD. Additionally, genetics play an important role in determining how quickly your kidneys will deteriorate over time. If you have a family history of chronic kidney disease or other related conditions such as polycystic kidney disease, it's essential to monitor your kidney function regularly.
Underlying medical conditions like high blood pressure and diabetes can also increase your risk for rapid decline in kidney function. It's critical to manage these conditions carefully by taking medications as prescribed by your doctor and making lifestyle changes like adopting a healthy diet and exercising regularly. By doing so, you may be able to slow down the progression of chronic kidney disease and avoid dialysis altogether.
In conclusion, understanding the risk factors for rapid decline in chronic kidney disease is crucial for managing your overall health effectively. Age, genetics, and underlying medical conditions all play a role in determining how quickly your kidneys will deteriorate over time.
By staying informed about these factors and taking care of yourself through proper management techniques like medication adherence and lifestyle changes, you may be able to slow down or even prevent further damage from occurring.
Predictors of Fast CKD ProgressionKnowing the predictors of fast CKD progression can help you take proactive steps to protect your kidney health. Firstly, high blood pressure is a significant predictor of rapid decline in kidney function. Therefore, it's essential to keep your blood pressure under control with medication and lifestyle changes such as exercise and a healthy diet.
Secondly, proteinuria or the presence of excess protein in urine is also a strong indicator of fast CKD progression. Some studies also suggest that the presence of protein in urine accelerates kidney damage by increasing inflammation and scarring in the kidneys. You can reduce proteinuria by limiting your intake of animal proteins, especially red meat, and taking medication prescribed by your doctor.
Lastly, smoking has been found to be a crucial factor in accelerating CKD progression. It increases oxidative stress on the kidneys and causes inflammation that damages them further. Quitting smoking can significantly slow down the rate of decline in kidney function and improve overall health outcomes.
By knowing these predictors, you can take action towards preserving your kidney function for longer periods before dialysis becomes necessary. Make sure to consult with your doctor regularly about any changes in kidney function or other risk factors that may affect its health. With proper care and management, you have the power to make a positive impact on your overall well-being.
Managing Accelerated Decline in Kidney FunctionIf your kidney function is declining more rapidly than expected, it's important to work with your healthcare team to identify potential causes and develop a treatment plan.
They will likely perform a series of tests to determine the underlying cause and assess the extent of kidney damage. These tests may include blood tests, urine tests, imaging studies, and possibly a kidney biopsy.
Once the cause is identified, your healthcare team will develop a personalized treatment plan. This plan may involve lifestyle modifications, such as adopting a healthy diet low in salt and saturated fats, exercising regularly, and quitting smoking. Medications may also be prescribed to control blood pressure, manage diabetes, or treat any underlying conditions contributing to kidney damage.
In some cases, more aggressive interventions may be necessary. For example, if a blockage or narrowing of the blood vessels in the kidneys is causing the accelerated decline, a procedure called angioplasty may be performed to open up the blocked vessels. In severe cases, dialysis or a kidney transplant may be required.
It's important to remember that everyone's experience with chronic kidney disease is unique. While some people may progress quickly towards dialysis or transplantation, others may have a slower decline in kidney function.
By working with your healthcare team and following a kidney-friendly diet plan, you can help improve the health of your kidneys and potentially slow down their decline over time.
Frequently Asked QuestionsHow does race and ethnicity affect the progression of CKD?If you're curious about how race and ethnicity can impact the progression of chronic kidney disease (CKD), there's evidence to suggest that certain populations may be more at risk for developing end-stage kidney disease.
Studies have shown that individuals who identify as Black, Hispanic, or Native American may be up to three times more likely to develop end-stage renal disease compared to those who identify as White. This may be due in part to disparities in access to healthcare, socioeconomic factors, and genetic predispositions.
However, it's important to note that every person's experience with CKD is unique, and it's crucial to work closely with your healthcare team to monitor your individual progression and make informed treatment decisions.
Stress and mental health can indeed impact the progression of chronic kidney disease (CKD). Studies have shown that people with kidney disease experience high levels of stress and anxiety, which can worsen their condition.
Stress activates the sympathetic nervous system, leading to increased blood pressure, which in turn damages the kidneys. Additionally, depression has been linked to an increased risk of CKD progression and mortality.
Therefore, it's crucial for individuals with CKD to manage their stress levels and seek help if experiencing symptoms of depression or anxiety. Some effective strategies include exercise, meditation, therapy, and support groups.
By prioritizing your mental health alongside medical treatment, you may be able to slow progression of your CKD.
You might think of exercise as an investment in your health, and it turns out that this investment can pay off for those with chronic kidney disease (CKD).
Research shows that regular physical activity can help slow down the progression of CKD. Exercise helps your kidneys function better. It also lowers blood pressure and reduces inflammation throughout the body, both of which are important factors in slowing CKD progression.
So, if you're looking for a way to take control of your health and potentially improve your kidney function, adding exercise to your routine could be a good place to start.
If you're looking for alternative treatments or therapies that can slow or reverse the progression of chronic kidney disease (CKD), there are several options available. One approach is to focus on managing underlying health conditions that may contribute to CKD, such as high blood pressure and diabetes. This may involve lifestyle changes like modification of diet and exercise, as well as medication management.
Additionally, some studies suggest that certain supplements and herbs, such as omega-3 fatty acids and Chinese herbal medicine, may have a beneficial effect on kidney function. It's important to speak with your healthcare provider about these potential treatments and determine the best course of action for your individual needs.
Did you know that age is a significant factor in the progression of chronic kidney disease (CKD)? According to recent studies, patients over the age of 65 have a higher likelihood of developing end-stage renal disease (ESRD) and requiring dialysis.
In fact, adults over the age of 65 account for more than one third of all CKD cases in the United States. While there are undoubtedly other factors at play in CKD progression, including underlying health conditions and lifestyle factors, your age can play a critical role in determining your risk level.
If you're concerned about the potential need for dialysis as your CKD progresses, it's essential to talk with your doctor about proactive steps you can take to protect your kidney function and manage any underlying conditions that may be contributing to the problem.
You now have a better understanding of the factors that affect the progression of your chronic kidney disease (CKD) and how to slow it down. While there's no guaranteed timeline for when you'll need dialysis, taking steps to control your blood pressure and diabetes, maintaining a healthy kidney-friendly diet plan, and avoiding harmful substances can make a significant difference in slowing the decline of your kidney function.
Some may argue that making these lifestyle changes can be difficult or burdensome. However, it's important to remember that even small changes can have a big impact on your health.
Seeking support from healthcare professionals, family members, or friends can also help you stay motivated and accountable towards achieving better health outcomes. Remember that you're not alone on this journey. With proper self-care and medical attention, you can take charge of your CKD and live a healthier life.
The post How Quickly Will My Chronic Kidney Disease Progress To Dialysis appeared first on Renal Diet HQ.
Suggested Reading:
CKD Progression Early Stage Kidney Disease The Importance Of Diet For Stage 3 Chronic Kidney DiseaseJune 14, 2023
CKD Grocery List
Eating a healthy diet is essential for people with chronic kidney disease (CKD). Meal planning and grocery shopping can be challenging, but it is important to make healthy food choices in order to protect your kidneys.
In this article, we will discuss the importance of creating a CKD-friendly grocery list and provide tips for building a healthy meal plan that meets your nutritional needs while still pleasing your palate. We'll also cover how online grocery shopping can help you stick to a kidney friendly food list and maintain a family-friendly kidney diet.
So let's get started!
[feast_advanced_jump_to] Key TakeawaysCreating a CKD-friendly grocery list is essential for individuals with CKD.Shopping for CKD-friendly foods can be challenging, but reading nutrition labels and focusing on low sodium, potassium, phosphorus, protein, saturated fat, and cholesterol options can help.Meal planning and portion control are crucial in managing nutrition while living with CKD.Small adjustments to diet, such as using herbs and spices as substitutes for salt and incorporating frozen fruits and vegetables without added sauces or seasonings, can have significant impacts on health.
Key TakeawaysCreating a CKD-friendly grocery list is essential for individuals with CKD.Shopping for CKD-friendly foods can be challenging, but reading nutrition labels and focusing on low sodium, potassium, phosphorus, protein, saturated fat, and cholesterol options can help.Meal planning and portion control are crucial in managing nutrition while living with CKD.Small adjustments to diet, such as using herbs and spices as substitutes for salt and incorporating frozen fruits and vegetables without added sauces or seasonings, can have significant impacts on health.Renal Diet EssentialsFor More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
A renal diet, also known as a kidney diet, is a specialized eating plan designed to support the overall health of individuals with chronic kidney disease. It focuses on managing the intake of certain nutrients, particularly protein, potassium, sodium, and phosphorus. Proper planning and grocery shopping play crucial roles in maintaining a balanced kidney diet.
Restricting amounts of protein consumed is a key aspect of a renal diet. High-protein options can increase the workload on the kidneys, leading to further kidney damage. It is suggested to consumed 0.55–0.60 grams of protein per kilogram per day.
Therefore, patients with CKD are often advised to limit their protein intake. Sources of protein like lean meats, poultry, fish, and eggs can still be included but in moderate portions. Plant-based proteins such as beans, lentils, and tofu are also good alternatives.
Controlling levels of potassium is also important because impaired kidneys may struggle to eliminate excess potassium from the body. Elevated potassium levels can disrupt the normal functioning of the heart and muscles. Hence CKD patients are often advised to adhere to a low potassium diet.
Foods high in potassium, such as bananas, oranges, tomatoes, potatoes, and beans, should be consumed in limited amounts. Instead, lower-potassium options like apples, berries, cucumbers, and rice can be chosen.
Sodium restriction helps control blood pressure and fluid balance. High sodium intake can lead to fluid retention and hypertension, which can further damage the kidneys. Processed foods, fast food, canned foods, and condiments often contain high levels of sodium and should be avoided. Instead, fresh fruits, vegetables, lean meats, and whole grains should be preferred.
One should also be careful of excess sodium additives in the form of sodium hexameta-phosphate, sodium tripolyphosphate, and tetrasodium pyrophosphate that may appear on food ingredients lists.
Phosphorus restriction is necessary because impaired kidneys may struggle to regulate phosphorus levels in the blood. Excessive phosphorus can weaken bones and contribute to cardiovascular complications. It is wise to be cautious of phosphorus additives as well.
Dairy products, nuts, seeds, whole grains, and processed foods are often high in phosphorus and should be limited. Foods with lower phosphorus content, such as rice, bread, apples, carrots, bean sprouts, and green beans, are better options.
Good planning when it comes to grocery shopping is essential for maintaining a balanced kidney diet. It allows individuals to select appropriate foods, control portion sizes, and avoid impulsive purchases.
Prioritizing fresh produce, lean proteins, and low-sodium and low-phosphorus alternatives is beneficial. Reading food labels for sodium and phosphorus content can also guide decision-making. Additionally, meal prepping can help ensure adherence to dietary guidelines and prevent reliance on convenience or processed foods.
A renal diet involves protein restriction, potassium, sodium, and phosphorus control. Planning grocery shopping effectively enables individuals with CKD to make informed choices, maintain a balanced kidney diet, and support their overall health and well-being.
Consulting with a registered dietitian who specializes in renal nutrition can provide personalized guidance and ensure optimal dietary management of chronic kidney disease.
Understanding the Importance of Meal Planning in CKDPlanning meals for CKD can be a huge challenge, but it's essential to managing the condition and staying healthy! Taking into account the individual's dietary restrictions and nutrient needs while still ensuring that meal planning is convenient and enjoyable are important considerations.
When creating a list of kidney friendly goods, look for foods that are low in sodium, potassium, phosphorus, protein, saturated fat, and cholesterol. Avoiding processed foods and fast food options is also recommended. Frozen fruits and vegetables without added sauces or seasonings can be great additions to a renal diet grocery list as they provide convenience without sacrificing nutrition.
Eating out should also be avoided when possible due to the lack of control over ingredients used in restaurant dishes. However, if it cannot be avoided, make sure to research food menu information offered by the restaurants or let your servers know that you have special dietary accommodations.
When shopping for groceries with CKD in mind, portion control is key. It's important not to buy too much food at once as this can lead to waste or overeating which could have negative health consequences.
Cost considerations are also an important factor when choosing foods; fresh produce may cost more than pre-packaged items but will typically offer more nutritional value than processed foods.
To reduce costs without compromising nutrition, it is usually safe to buy canned or frozen fruits instead of fresh ones - most canned fruit does not contain added sugar so it can make a great snack option if portioned correctly!
Additionally, look into making recipe substitutions such as using whole wheat pasta instead of white pasta or opting for leaner cuts of meat like chicken breast instead of red meat.
Meal planning may seem daunting at first but by focusing on nutritious ingredients that fit within your dietary restrictions, you'll soon find yourself creating delicious meals that everyone in your family will enjoy! Don't forget about snacks either: many nuts and seeds provide plenty of nutrition without being overly high in sodium or other nutrients you need to limit with CKD.
With some creativity and careful consideration, you'll be able to create an ideal renal diet grocery list tailored specifically towards your own health needs! No matter what stage of kidney disease you're in, being aware of how to prepare your list of foods for shopping can help support your diet.
The Role of Grocery Shopping in CKD ManagementMaintaining a healthy diet that is appropriate for kidney disease comes down to effective meal planning and grocery shopping. Most people go to the grocery store and just choose items that they think look good and that is how they plan their menu for the week. For people with chronic health issues like kidney disease, you need a bit more planning and an effective grocery store strategy.
Strategizing a trip to the grocery store might sound like overkill to you know, but you will come to understand how effective shopping for kidney disease can not only ensure healthier groceries, but it can also help save you time and money.
Knowing what part of the store holds the healthiest groceries and what places you go to to get the best items that are appropriate for your diet are how you grocery shop to suit your health situation.
The first step in grocery shopping for CKD is to plan out what meals you want to make throughout the week. This allows you to determine exactly what ingredients you need in your shopping list so that you don't buy too much or too little.
Knowing which items are good for CKD is also important when planning meals and going through the grocery store aisles. For example, whole grain breads provide complex carbohydrates compared with white breads which contain simple carbohydrates, however, they also tend to contain more phosphorus. Be sure that you are guided by a healthcare provider such as a renal dietitian to decide these matters.
Grocery shopping requires some thoughtfulness but doesn't have to be a chore if done correctly! By understanding how different foods affect your health and nutrition goals - such as controlling blood glucose levels or maintaining a healthy weight – you can create a personalized meal plan that best suits your lifestyle and helps manage CKD symptoms.
So, get creative and enjoy your next trip to the grocery store!
Creating a CKD-Friendly Grocery ListCreating a personalized renal diet grocery list that's tailored to your dietary needs and health goals can make shopping trips fun and stress-free! Whether you've recently been diagnosed with chronic kidney disease or are managing advanced kidney disease for years, understanding what foods are best for maintaining kidney health should be at the top of your list.
Reading nutrition labels on food packaging will help you determine which items contain high levels of sodium, sugar, and other important nutrients. Be sure to practice portion control when selecting items such as canned goods, pre-packaged snacks, and frozen meals. Additionally, it's wise to choose fresh fruits and vegetables for snacking options throughout the day.
When creating your grocery list for CKD management, focus on ingredients that are low in potassium and phosphorus. It's also beneficial to select dry foods that can be stored easily like nuts, seeds, oats, quinoa, etc. so you can have easy access when meal planning or craving a snack.
You may want to consider incorporating some simple kidney-friendly recipes into your meal plan such as grilled chicken with steamed vegetables or baked salmon served over a bed of wild rice.
Grocery shopping can be an enjoyable experience if you take the time to plan ahead according to your dietary needs and health goals. Making smart choices while reading nutrition labels and stocking up on nutrient-dense foods will go a long way when it comes to maintaining optimal kidney function!
Avoiding Impulse Buys: Sticking to Your CKD Grocery ListSticking to your personalized dietary needs and health goals while grocery shopping can help you avoid costly impulse buys! To do so, it's important to stock up on the staples that you need for a healthy CKD diet.
Here are a few things to keep in mind:
Plan It OutFirst of all, every effective meal plan and grocery shopping trip starts with a little organization and planning. You should put a healthy meal plan together based on healthy recipes that you want to eat each day. Make a list of the items you plan to eat for each meal as well as the ingredients you need to make these meals, including snacks. Based on that list, make your grocery list.
Don't StrayDo not stray from your list when you shop and avoid impulse buys at all costs. This will help you avoid unhealthy buys and save you money. One way to avoid impulse buying is to grocery shop online which can make it less satisfying to put unhealthy items in your cart.
You also have the benefit of being able to fully analyze your cart and easily remove impulse items before you checkout. If you plan on using any online savings schemes such as Target coupons, remember not to stray from your list, as it can be very easy to buy more than you need to take advantage of such a deal.
Another way to avoid impulse buys is to never go grocery shopping hungry. If you are hungry you are more likely to make impulse buys, specifically snack items that aren't good for you or your kidney disease.
Stick To The Outer AislesIn almost every grocery store, the outer aisles are where you will find the healthiest grocery items. The produce section, of course, is where you should be finding most of your groceries. In most grocery stores, the "health food" section is in the aisles nearest to the fresh foods section, and this is where you will find more unprocessed food items.
Meat and dairy items are also typically on the outer aisles, so you should be able to avoid the inner aisles. If you do find the need to venture into these aisles, try not to browse and only go for what is on your list. All of those easy processed foods are hard to turn down in a pinch.
Market FreshOne of the best places to grocery shop is at your local farmer's market. Not only will you find the freshest and most delicious produce there, but you will help your local economy. You will also likely save a lot of money because most farmer's markets are cheaper than the produce section in your favorite grocery stores.
The Benefits of Online Grocery Shopping for CKD PatientsFinding the perfect balance between convenience and nutrition can be challenging for CKD patients, but online grocery shopping offers a great solution. With the tap of a few buttons, CKD patients can access their favorite groceries without leaving home.
Shopping apps like AmazonFresh or Instacart allow users to search specific items or browse entire stores in order to compare prices and find the best deal on quality products. Home delivery is also available with some services so that those with limited mobility can still reap the benefits of online grocery shopping.
Online grocery stores make it easier to control portion sizes and stay within nutritional guidelines by providing detailed nutritional information about each product. Price comparison tools help shoppers stick to their budget while ensuring they are buying healthy foods that fit into their meal plan.
CKD patients no longer need to worry about long lines and navigating crowded store aisles; online grocery shopping provides all the same benefits as traditional options with added convenience.
From price comparison tools and detailed nutritional information to home delivery services and helpful apps, online grocery shopping offers plenty of advantages for CKD patients looking for an easy way to manage their diet while staying safe at home.
Navigating the Grocery Store: Outer Aisles vs. Inner AislesYou can make the most of your grocery shopping trip by taking advantage of the differences between outer aisles and inner aisles. Outer aisles tend to contain more fresh, unprocessed foods such as fruits, vegetables, and lean proteins like seafood or poultry.
Inner aisles are often stocked with pre-packaged convenience items like frozen meals, condiments, canned goods, and cereals. Both areas have their advantages for CKD patients:
Outer Aisle Benefits:
Reading nutrition facts labels is key to understanding what you're buying and making healthy choices. Unprocessed items on the outer aisle don't come with nutrition labels so they're easier to identify as healthier options.The produce section offers many salt substitutes that can be used in cooking instead of table salt. This can help reduce sodium intake significantly without sacrificing flavor.Buying produce from the outer aisle means you get to decide portion sizes which gives you greater control over calorie consumption as well as added convenience since no additional preparation is needed when it comes time to eat them.Inner Aisle Benefits:
Pre-made meals offer quick dinner solutions if you're short on time but still want something nutritious that fits within your dietary restrictions for CKD management.Canned vegetables and fruits provide easy access to healthy snacks even during busy times when there isn't enough time for meal prep or baking from scratch.Low sodium alternatives like reduced-salt broths can replace regular broths if lower sodium content is desired while still providing flavor in recipes or soups without having to substitute ingredients too much or sacrifice taste entirely.Both sections of the grocery store have their uses depending on what kind of meal planning needs arise throughout the week, giving CKD patients more kidney-friendly options to meet their health needs without compromising flavor or convenience at mealtimes.
The Importance of Fresh Produce in a CKD DietNow that you know what to look for when navigating the grocery store, it's important to focus on the importance of fresh produce in a CKD diet. Eating fresh fruits and vegetables can help manage potassium levels and portion control.
When selecting produce, it is recommended to look for food labels and read them carefully. Focus on the serving size listed on the label and note how much potassium is contained in each serving size. This will help you determine which foods are safe to consume within your CKD diet plan.
As potassium is one of the nutrients that people with kidney disease must watch out for, here is a table outlining the amounts of potassium in selected produce:
Food & Serving SizePotassium (mg)Strawberries, 1 cup (152g)54 mgApple, 1 large (242g)195 mgBroccoli, ½ cup cooked (78g)42 mgBanana, 1 medium (118g)422 mgBy understanding your dietary needs through label reading and food swaps, you can ensure that your meals contain enough essential nutrients while controlling your potassium levels. With this knowledge, you can easily pick out the best healthy options when it comes to fresh produce for your renal diet!
Exploring Local Farmers Markets for CKD-Friendly FoodsShopping from local farmer markets can offer numerous benefits for patients with chronic kidney disease (CKD) who are following a renal diet.
Here are some advantages of choosing farmer markets for CKD-friendly foods:
Freshness and Quality: Farmer markets often offer fresh, locally sourced produce. Fresh fruits and vegetables are rich in essential nutrients and lower in sodium and phosphorus compared to processed or canned alternatives. The quality and flavor of freshly harvested produce can greatly enhance the taste and enjoyment of meals.Seasonal Variety: Farmer markets showcase a wide range of seasonal produce. Eating a variety of fruits and vegetables ensures a diverse nutrient intake while adding culinary excitement. Local farmers can provide guidance on the best produce options for CKD patients, ensuring they choose items that are low in potassium and phosphorus.Organic and Pesticide-Free Options: Many farmer markets prioritize organic farming practices, offering a selection of pesticide-free and sustainably grown produce. Organic foods can reduce exposure to potentially harmful chemicals, which is particularly important for individuals with CKD who need to minimize toxin buildup in their bodies.Community Support: Shopping at farmer markets supports local farmers and the community. It promotes sustainable agriculture and helps strengthen the local economy. Engaging with farmers and other shoppers can create a sense of belonging and connection, fostering a supportive environment for individuals managing CKD.Access to Specialty Foods: Farmer markets often feature unique and specialty items that may be beneficial for CKD patients. These can include low-sodium sauces, herbal teas, low-phosphorus baked goods, and other homemade products that cater specifically to dietary restrictions.Education and Awareness: Farmer markets offer an opportunity for individuals to learn more about the food they consume. Farmers and vendors are often knowledgeable about their products and can provide valuable insights into nutritional content, cooking techniques, and recipe ideas that align with a renal diet.By shopping at local farmer markets, CKD patients can access fresh, seasonal, and nutrient-dense foods that align with their dietary needs. The direct connection with local farmers and the community enhances the overall experience and contributes to a healthier, more sustainable lifestyle.
Building a Healthy Meal Plan for CKDCreating a healthy meal plan for people with CKD doesn't have to be difficult – you just need to know where to start! Meal planning is an important part of managing the dietary needs associated with CKD.
Preparing meals ahead of time can help you reach your nutritional goals and make sure you're getting the necessary vitamins and minerals without exceeding sodium intake guidelines.
Creating a healthy meal plan for a CKD patient on a renal diet involves several key steps:
Consult with a healthcare professional: It's crucial to consult with a registered dietitian or healthcare professional who specializes in renal nutrition. They can assess the patient's individual needs, medical history, and lab results to provide personalized dietary recommendations.Understand dietary restrictions: Gain a thorough understanding of the dietary restrictions associated with CKD, including protein, sodium, potassium, and phosphorus restrictions. This knowledge forms the foundation of the meal plan.Plan balanced meals: Design meals that incorporate a balance of nutrients while adhering to the recommended restrictions. Include adequate high-quality protein sources such as lean meats, poultry, fish, and eggs, while controlling portion sizes to limit protein intake. Choose low-potassium fruits and vegetables and limit high-potassium foods like bananas, oranges, tomatoes, and potatoes. Similarly, control sodium intake by avoiding processed foods and using herbs and spices for flavoring instead.Monitor phosphorus intake: Restrict phosphorus intake by choosing low-phosphorus foods like rice, bread, and pasta over higher-phosphorus alternatives like whole grains and dairy products. Limiting portion sizes of high-phosphorus foods is also essential.Consider fluid restrictions: In advanced stages of CKD, fluid intake may need to be restricted. Take into account the recommended fluid allowance when planning meals and beverages.Incorporate variety and taste: Make the meal plan enjoyable by including a variety of flavors, textures, and colors. Experiment with herbs, spices, and low-sodium seasoning blends to enhance taste without relying on salt. Explore different cooking methods like grilling, baking, or steaming to add variety to meals.Monitor and adjust: Regularly monitor the patient's lab results and consult with the healthcare professional to assess the effectiveness of the meal plan. Adjustments may be necessary based on individual needs and changing health conditions.By following these steps and working closely with a healthcare professional, a CKD patient can develop a personalized, healthy meal plan that supports kidney function and overall well-being.
Tips for Shopping for Kidney DiseaseShopping for and preparing meals with kidney disease can be tricky, but there are tips to help you make smart decisions at the grocery store. First, menu planning is a great way to ensure that you're getting all of the nutrients your body needs while limiting foods that may cause harm.
Before going to the store, plan a week's worth of meals ahead of time, so you know exactly what ingredients you need. Secondly, portion control is key when managing CKD. Make sure to balance your plate with half non-starchy vegetables, one quarter proteins (alternative proteins such as fish or tofu are recommended) and one quarter carbohydrates such as whole grains or legumes.
Lastly, when shopping for beverages look out for ones that are low in sugar and sodium; label reading is also essential when it comes to avoiding unwanted additives in processed food products.
Stay away dark-colored sodas, certain diet sodas, and cream sodas as they not only raise blood sugar levels, may also contain phosphoric acid additives that can raise phosphorus levels.
TipsDescriptionMenu PlanningPlan weekly meals before shoppingPortion ControlBalance plate with non-starchy vegetables, proteins & carbsAlternative ProteinsTry fish or tofu instead of red meat/poultryHydration StrategiesAim for 8 glasses water/day; avoid sugary drinks & high sodium foodsLabel ReadingCheck labels on processed foods for unwanted additives & preservativesIt can be overwhelming navigating grocery stores nowadays due to the wide variety of options available - try sticking with whole foods such as fresh fruits and veggies which don't require label reading!
Remember: eating healthy doesn't have to be complicated. With these simple tips in mind you will soon find yourself making smart choices at the grocery store while still enjoying delicious meals!
Low Sodium Choices: A Key Consideration for CKD Grocery ListsWhen managing a chronic condition like CKD, it's important to consider low sodium choices when preparing meals. Knowing which foods contain the least amount of salt is a critical part of any grocery list for people with kidney disease.
Eating out can be difficult, as many restaurants add large amounts of salt to their dishes. To ensure you're making the healthiest decisions possible, always read nutrition labels prior to purchasing pre-made meals or snacks. Portion control also plays an important role in regulating your sodium intake; make sure that you're not eating too much food at one time.
Eating a balanced diet is also essential for overall health and wellness; choose fresh fruits and vegetables whenever possible, and stay away from processed meats and other high-sodium items like canned soup or frozen dinners.
Small adjustments to your diet can have big impacts on your health – so take some time each week to plan out healthy meals that are low in sodium content!
Maintaining a Family-Friendly Kidney DietMaintaining a kidney-friendly diet with family members in mind can be challenging, but it doesn't have to be difficult. The key is to make small adjustments while still providing delicious and nutritious meals for everyone.
Portion control, sodium substitutes, cooking techniques, grocery budgeting, and meal prepping are all helpful strategies that can help you create meals that are tailored to the needs of those with CKD.
For example, if a family member has dietary restrictions due to CKD, it's important to plan ahead when shopping for groceries. Look for foods low in sodium and try using herbs and spices as sodium substitutes instead of salt.
Meal prepping can also help save time during busy weeknights by making larger batches of food which will last throughout the week. This helps cut down on added stress when trying to accommodate different dietary restrictions within the household.
Grocery budgeting is another way to help maintain a healthy kidney diet while accommodating other family members' dietary needs. Consider stocking up on items like frozen vegetables or canned beans since they tend to be less expensive options than fresh produce.
Making sure everyone at home is getting their nutritional needs met without breaking the bank can help make meal planning easier and less stressful for everyone involved!
Frequently Asked QuestionsWhat foods should be avoided when following a CKD diet?When following a CKD diet, it is important to avoid certain foods that can worsen kidney function. These include high-protein foods like red meat, processed meats, and high-fat dairy products. Foods high in potassium, such as bananas, oranges, tomatoes, and potatoes, should be limited.
Sodium-rich foods like processed snacks, canned soups, and fast food should be avoided to manage fluid balance. Foods with high phosphorus content, such as dairy products, nuts, seeds, and whole grains, should also be restricted. It is crucial to consult with a healthcare professional or registered dietitian for personalized recommendations based on individual needs and stage of CKD.
When following a chronic kidney disease (CKD) diet, it's important to prioritize foods that are kidney-friendly and support overall health. Here are some essential items to consider for your kidney friendly food list:
1. Low-potassium fruits: Include apples, berries, grapes, and pineapples while limiting high-potassium fruits like bananas and oranges.
2. Vegetables with lower potassium content: Opt for cauliflower, green beans, cabbage, and peppers, while moderating intake of high-potassium veggies such as potatoes and tomatoes.
3. Lean protein sources: Choose skinless poultry, fish, eggs, and tofu as excellent sources of high-quality protein with less phosphorus.
4. Low-phosphorus grains: Incorporate rice, pasta, and white bread, avoiding whole wheat products that are higher in phosphorus.
5. Low-fat dairy or alternatives: Include skim milk, low-fat yogurt, and unsalted cheese to maintain calcium intake while minimizing phosphorus.
6.Limited sodium foods: Select fresh herbs, spices, and low-sodium seasoning blends instead of salt to reduce sodium intake.
Remember to consult with a registered dietitian to customize your CKD diet according to your specific needs and to ensure optimal kidney health.
You can save money while following a CKD diet by being cost-effective in your grocery shopping. Start by developing a budget plan and sticking to it, then shop with that in mind.
Meal planning is also important for saving money and time when grocery shopping. Read labels carefully to make sure you're getting what you need at the best price, and look for local sources of ingredients as they can often be cheaper than buying from larger stores.
With some careful consideration of cost effectiveness, label reading, budget planning, meal planning, and local sources, you can save money while still eating healthily on a CKD diet.
When shopping for a CKD diet with a family, it's important to plan ahead. Look at the meal plan and create a grocery list that reflects all of the items you need.
Be sure to read nutrition labels carefully and look for organic options when possible. Convenient alternatives such as pre-cut vegetables or frozen meals can save time while still sticking to your diet goals.
Lastly, consider smart swaps like substituting whole grain crackers for chips or swapping high-fat sauces for lower-fat alternatives, which will help balance out the nutritional content of your meals.
Yes, there are ways to shop for CKD-friendly foods without going to a grocery store. You can use online delivery services to have the food you need delivered right to your door.
Meal planning is helpful in this situation so you can make sure that any items purchased fit into the CKD diet and ensure portion sizes are correct. Reading labels carefully and staying within budget are important as well.
With online delivery services, meal planning, portion size control, label reading, and budgeting skills, you can easily shop for CKD-friendly foods without leaving your home.
Making smart grocery choices is an essential part of managing chronic kidney disease. It doesn't have to be overwhelming to create a CKD-friendly grocery list. With tools like online shopping and healthy meal plans, you can make the process easier and keep your kidney friendly food list focused on low-sodium, nutrient-rich foods.
By sticking to your renal diet grocery list and avoiding impulse buys, you'll be able to maintain a balanced diet that meets your nutritional needs while keeping your family happy. The key is planning ahead and making smart decisions in the store, so you don't have to worry about what's in your cart when you get home.
The post CKD Grocery List appeared first on Renal Diet HQ.
Suggested Reading:
Renal Vegetarian Diet The Importance Of Diet For Stage 3 Chronic Kidney Disease Low Potassium Side DishesJune 13, 2023
Hyperparathyroidism Diet Restriction
If you're living with both hyperparathyroidism and chronic kidney disease (CKD), you may be wondering what dietary restrictions are necessary to keep your condition in check. It's important to know that diet plays a significant role in managing these conditions, and understanding the relationship between the two can help you create a balanced diet plan that works for you.
In this article, we'll look at how to create an appropriate diet plan for hyperparathyroidism and CKD, as well as lifestyle changes that can help support it. We'll also provide tips on monitoring and adapting your diet over time with these two conditions.
[feast_advanced_jump_to] Key TakeawaysLimit foods high in calcium, phosphorus, and sodium to reduce symptoms associated with hyperparathyroidism and chronic kidney disease.Pay attention to nutrient intake, including calcium, phosphorus, vitamin D, protein, sodium, potassium, and magnesium.Dietary adjustments can improve overall health by including anti-inflammatory foods like fruits, vegetables, legumes, and fish.Mindful tracking of food intake can help identify areas where dietary modifications are needed for effective management of hyperparathyroidism and chronic kidney disease.
Key TakeawaysLimit foods high in calcium, phosphorus, and sodium to reduce symptoms associated with hyperparathyroidism and chronic kidney disease.Pay attention to nutrient intake, including calcium, phosphorus, vitamin D, protein, sodium, potassium, and magnesium.Dietary adjustments can improve overall health by including anti-inflammatory foods like fruits, vegetables, legumes, and fish.Mindful tracking of food intake can help identify areas where dietary modifications are needed for effective management of hyperparathyroidism and chronic kidney disease.Understanding Hyperparathyroidism and Chronic Kidney Disease (CKD)For More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
If you have hyperparathyroidism and CKD, understanding how the two conditions affect each other can help you make dietary changes that'll support your health. Hyperparathyroidism is caused by an overactive parathyroid gland, leading to increased calcium levels in the blood. Symptoms include fatigue, bone loss, and kidney stones.
Chronic Kidney Disease (CKD) is a progressive decrease in kidney function due to damage. It can be caused by infection, injury, or certain medical conditions.
Diagnosis and testing for both hyperparathyroidism and CKD involve physical exams, blood/urine tests, and imaging scans. Treatment for hyperparathyroidism may include medication or surgery to remove part of the abnormal tissue.
For those with CKD, treatment may involve lifestyle changes such as diet restrictions or dialysis treatments. Risk factors for developing either condition include age, family history, diabetes mellitus type 2, and hypertension.
It's important to take steps towards emotional support when dealing with these conditions, as depression and anxiety are common side-effects. Finding someone who understands what you're going through can be incredibly helpful in managing stress levels.
The key takeaway is that having hyperparathyroidism with chronic kidney disease requires careful consideration when making dietary choices. Understanding how they interact is essential when determining what food options best suit your individual needs within a healthy eating plan. This supports overall wellbeing through proper nutrition while reducing risk factors wherever possible.
The Connection Between Hyperparathyroidism and CKDYou're probably wondering how kidney disease and parathyroid issues are connected. Hyperparathyroidism is a condition in which the body produces too much of the hormone parathyroid hormone (PTH).
First, let me explain what SHPT (secondary hyperparathyroidism) is. Your parathyroid glands are responsible for keeping your bones and calcium levels in your blood at a healthy range. They are located in your neck on the back of your thyroid gland.
Most of the time, you don't even know they are there. They are near your thyroid gland, but work separately and produce PTH (Parathyroid hormone). PTH is responsible for maintaining the correct amount of calcium in the blood and bones, as well as ensuring optimal gastrointestinal absorption of calcium, and finally controlling urinary calcium excretion (That is the connection to kidney disease).
The amounts of other minerals that are part of bone growth - phosphorus and Vitamin D - are also critically important to the parathyroid. Doctors measure the amount of PTH as an indicator of bone disease.
Secondary Hyperparathyroidism (SHPT) as related to kidney disease is an overactive parathyroid hormone secretion. This is caused by renal insufficiency affecting other mineral levels in the blood and causing the body to overproduce PTH. In persons with CKD starting in stage 3, damage to the kidney affects the functioning of the kidney and causes these changes to possibly occur.
So, what causes the body to produce more PTH?
While that is a complicated question, I would like to answer it in a way that is easier to understand. Please remember - I am not your doctor!
Initially, your functioning kidney mass is decreased. This happens because of the damage over time to the nephrons in your kidneys. Your doctor may have told you a percentage of your kidneys that are still functioning. Once the amount of your kidneys that are working is decreased beyond a certain level (not exactly clear how much and it varies by individual), 2 things happen:
Kidneys are responsible for activating the Vitamin D in our body so it works. With less functional kidney, lower amounts of vitamin D3 are available in the bloodstream.Kidneys also excrete the phosphorus in our bodies, and with a lower capacity to produce urine, phosphorus builds up in the bloodstream.Those two events that happen together bring about a decrease in serum (blood level) calcium. A decrease in the amount of calcium, plus a decrease in the amount of Vitamin D3 and an increase in the amount of phosphorus in the blood cause your body to think you need more PTH (because it needs to increase the amount of calcium in your bloodstream to a normal level).
It's essential to have regular check-ups with your doctor if you suffer from CKD or hyperparathyroidism so that potential complications can be identified early on. Keeping track of changes in symptoms and adjusting lifestyle accordingly will improve quality of life and help prevent long-term damage caused by this condition.
Importance of Diet in Managing Hyperparathyroidism and CKDTaking control of your nutrition is essential in managing the symptoms of both chronic kidney disease and hyperparathyroidism, so don't ignore the importance of diet. Managing your dietary intake can help you to better manage your phosphorus levels and maintain an optimal lifestyle even with a chronic condition.
By following dietary guidelines and keeping track of what you eat, you can make sure you're getting all the essential nutrients while avoiding those that could aggravate your symptoms.
When it comes to managing hyperparathyroidism and CKD, there are some important dietary restrictions to take into consideration.
It's recommended to limit foods high in phosphorus such as dairy products, nuts, beans, lentils, dark-colored soft drinks and beers as well as processed foods like ready meals or fast food.
Additionally, high sodium intake should be avoided since it increases the risk of fluid retention which can worsen CKD-related health problems like swelling in legs or ankles.
Adopting a healthy lifestyle with a proper diet is key for symptom management when living with these two conditions. Making small changes such as reducing salt intake or limiting unhealthy snacks will help you get on top of your nutrition needs while managing hyperparathyroidism and CKD simultaneously.
Nutrients to Monitor in a Hyperparathyroidism and CKD DietStruggling with a chronic condition can be overwhelming, but monitoring your nutrient intake is an essential part of managing hyperparathyroidism and CKD.
To do this effectively, it's important to keep tabs on calcium supplementation, phosphorus control, vitamin D intake, protein sources, and sodium regulation.
Levels of calcium should be monitored closely since it helps regulate the parathyroid hormone levels in those with hyperparathyroidism.Phosphorus control is another important factor to pay attention to when managing both conditions as it can cause complications if left unchecked. This means avoiding processed foods and high-phosphorus animal proteins like organ meats and shellfish.Vitamin D intake is also key since it helps reduce the risk of developing fractures due to bone loss caused by hyperparathyroidism or CKD-associated osteoporosis. For people who lack sufficient sunlight exposure, supplements may be necessary for adequate doses of vitamin D.Lastly, protein sources should be selected carefully as too much protein can worsen kidney disease symptoms such as fatigue and nausea while not enough can lead to muscle wasting in people with CKD. Additionally, individuals must keep an eye on their sodium intake as high amounts are often associated with increased blood pressure which exacerbates both diseases' symptoms in some cases.It's not always easy to stay on top of managing a chronic condition like hyperparathyroidism or CKD but getting into the habit of monitoring one's nutrient intakes can help make life more manageable over time - even if small changes are made every day towards healthier eating habits that comply with these guidelines!
With guidance from healthcare providers and support from family & friends alike, anyone struggling with these ailments will soon find themselves equipped with the knowledge they need to manage their dietary requirements more effectively for greater overall health outcomes down the road!
Calcium and Phosphorus Balance in Hyperparathyroidism and CKD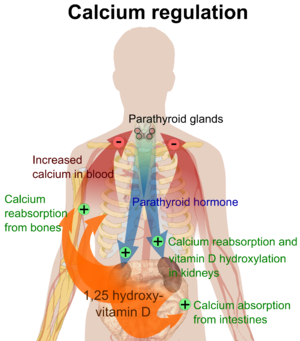 English: Overview of calcium regulation (See Wikipedia:Calcium in biology).
English: Overview of calcium regulation (See Wikipedia:Calcium in biology).Maintaining a healthy blood calcium levels and phosphorus balance is essential when managing hyperparathyroidism and CKD, so it's important to track your intake of these nutrients.
When the estimated Glomerular Filtration Rate (eGFR) decreases to less than 60 ml/min, your ability to remove phosphorus from your blood via your kidneys becomes altered.
The part of your nephrons that are still working compensate by increasing the removal of phosphorus because your blood levels are increased. This helps to maintain normal phosphorus levels in your bloodstream.
Once you progress further in kidney disease, your nephrons eventually become unable to excrete enough phosphorus to compensate, and that is when you start to notice hyperphosphatemia (elevated levels of blood phosphorus).
So, as the amount of phosphorus increases in your blood, PTH is secreted to compensate. Calcium can bind with phosphorus (if they are out of balance) in the blood stream and form particles that then are deposited in organs and blood vessels.
As phosphorus levels increase, this risk is higher, so your body reacts by breaking down bones and increasing serum calcium level. This causes the bones to weaken over time, and calcium particles (those bound with phosphorus) to deposit in areas of the body such as the heart.
Dietary interventions are key to keeping your levels in check since some foods can interfere with phosphorus absorption or mineral deficiencies can cause an imbalance. If you're having trouble getting enough calcium through diet alone via intestinal calcium absorption, consider taking a supplement to help support bone health.
Making sure you get the right amount of both minerals is important for preventing complications associated with hyperparathyroidism and CKD.
It's essential that you monitor your calcium consumption and dietary phosphate intake on a daily basis. Understanding how much of each nutrient is in various food sources will help you create meals that promote balance between them. Pay attention to portion sizes as well, as too much of one nutrient can throw off the delicate equilibrium required for optimal health outcomes.
Consider talking to a nutritionist or medical professional who specializes in hyperparathyroidism and CKD diets if you need extra assistance creating meal plans tailored for your specific needs.
Knowing which supplements to take can be tricky, especially when dealing with two separate conditions at once. Speak with your doctor about any recommended products they suggest for maintaining balance of calcium and phosphorus levels, such as multivitamins or individual minerals like iron or magnesium.
They may also suggest switching up your existing medications if there could be possible interactions with other components within them causing an imbalance between these two nutrients.
Vitamin D and its Role in Hyperparathyroidism and CKDYou can't overlook the importance of Vitamin D for managing both hyperparathyroidism and CKD. It's essential for keeping your levels in check and improving your overall health. Without adequate levels, your body won't be able to properly absorb minerals like calcium and phosphorus, which are necessary for bone health.
PTH works to "normalize" your serum calcium concentrations or the amount of calcium available in your bloodstream. Calcium is used for many things in your body, and it needs to be available to your cells. So, an increased amount of PTH will cause your bones to be broken down more quickly to makes its calcium content available in your bloodstream.
Vitamin D3 happens to be very important in the actions and levels of PTH in our body. You may be aware that our bodies can "make" vitamin D by exposing our skin to sunlight for 10-20 minutes every day. That vitamin D our skin makes has to be transported to the kidney to be changed into the "active" form our body uses. It keeps us from overdosing on Vitamin D with too much sunlight.
Once vitamin D becomes activated, it can work in our bodies. It stimulates some other hormones that tell the parathyroid we have enough PTH. It also decreases PTH indirectly by increasing the amount of calcium we absorb in our "gut" through our gastrointestinal tract.
This increases the amount of calcium in our blood stream, and keeps the amount of PTH at a normal level. But once you have a decreased level of vitamin D in your body, it does not work to increase the level of calcium in your bloodstream as efficiently (you don't absorb as much) so your body starts increasing the amount of PTH to accommodate your calcium needs.
When it comes to treating hyperparathyroidism and CKD, Vitamin D supplementation is often recommended as part of dietary guidelines. Here are a few ways you can make sure you're getting enough:
Spend more time outside in direct sunlight – UV rays from sunlight help form Vitamin D3Incorporate foods rich in Vitamin D into your diet such as fatty fish (e.g., salmon), egg yolks, fortified milk products, certain mushrooms, and organ meats like liver.Take a supplement if needed – sometimes doctors will recommend a Vitamin D supplement if dietary sources aren't enough or if there's an underlying medical issue causing deficiencies.It's easy to see why maintaining healthy levels of Vitamin D is so important when managing conditions like hyperparathyroidism and CKD. If you think you might be deficient or have any questions about how much you should be getting each day, talk to your doctor right away!
Management And Treatment of PTH and SHPTKDOQI guidelines have recommended target ranges for PTH and calcium levels in renal patients with Stage 3 - 5 kidney disease. Based on those target ranges, the first course of action to improve the health of a patient with SHPT and suppress the levels of PTH is thought to be Vitamin D therapy.
As vitamin D plays such a role in our absorption of calcium, if a person can take in and absorb appropriate amounts of "active" vitamin D (doesn't have to be processed by the kidneys), their calcium absorption rate should also improve.
In addition to Vitamin D, dietary therapy includes reduction of high phosphate foods. Foods that are high in phosphate content include dairy products, meats, beans, dark sodas, beer and nuts. Many of these foods are great sources of protein, so it is important to be cautious when eliminating foods. You should focus on removing foods that are high in phosphate yet lower in protein, such as dark colas, cheese, milk, ice cream and beer.
You have to be careful about sources of protein because that can lead to malnutrition which affects outcomes once people start on dialysis. Also, dietary phosphate restriction may not be adequate since most of our food contains phosphates. Many doctors also recommend the use of phosphate binders as well.
Phosphate binding agents are taken with foods, up to 3-4 times per day, and attach to phosphate in the foods we eat causing it to remain in the digestive system and be excreted through stool. They have to be taken with food or they don't work effectively, yet it is difficult for people to be consistent and remember to take the medications.
Sometimes doctors use several different types of binders to achieve success. Some phosphate binders can be found over the counter such as calcium carbonate and aluminum hydroxide. But, you should talk to your doctor about it prior to initiating any additional intake.
Protein Intake: A Key Consideration in Hyperparathyroidism and CKDManaging your protein intake is essential for keeping hyperparathyroidism and CKD in check, so it's important to be mindful of how much you're consuming each day. To do this, it's important to understand the sources of dietary protein as well as the dietary guidelines that must be followed for hyperparathyroidism and CKD.
Protein SourcesDietary GuidelinesLean meats, poultry, fish, eggs, dairy products, legumes, nuts/seedsLimit saturated fat intake; Choose low-fat options; Avoid processed foods; Eat more fruits & vegetables; Incorporate nutritional supplements such as vitamin D & calcium into diet if neededWhen having hyperparathyroidism and CKD together, diet modifications are key. Making smart food choices while focusing on lean proteins is recommended in order to ensure proper nutrition.
In addition to dietary changes like limiting unhealthy fats and avoiding processed foods, adding nutritional supplements such as vitamin D or calcium can help maintain balance between healthy eating habits and necessary nutrients. Remember though that supplements should only be taken after consulting with a medical professional first.
Considering all these factors is vital when managing your protein intake while living with both hyperparathyroidism and CKD. Eating a balanced diet full of nutrient-rich proteins can help keep symptoms at bay while still providing enough energy throughout the day for everyday activities.
Sodium and Fluid Restrictions in Hyperparathyroidism and CKD DietWhen living with both hyperparathyroidism and CKD, it's essential to keep a watchful eye on sodium and fluid intake in order to maintain balanced levels. For those with kidney disease and hyperparathyroidism, the right balance of sodium is especially important as too much can cause fluid overload, while too little can lead to dehydration.
Keeping an eye on sodium sources such as table salt, processed foods, and canned goods is key for maintaining proper sodium levels in the body. Additionally, keeping track of water consumption throughout the day is also necessary.
In addition to monitoring sodium intake for those with both hyperparathyroidism and CKD, making sure that there is enough potassium and magnesium in the diet is also important. Potassium helps regulate electrolyte balance in cells while magnesium helps activate enzymes related to energy production.
What Should I Do About My SHPT?First of all, discuss what it means with your doctor. Develop that relationship so you can ask. If you cannot, consider finding another doctor who will work with you. If you need to make a longer appointment, you should tell the person booking the appointment that you have a lot of questions and request a longer appointment time. That will keep your physician from feeling rushed.
At this point - if you have CKD Stage 3, it is recommended that you work with a nephrologist. They are experts and will manage your kidney disease very well. You may also want to find a local dietitian or check into a meal plan that meets your nutritional needs.
Decreasing the amount of phosphate in your diet, in addition to treatment with an active vitamin D medication can provide a great deal of improvement and reduce your risk of bone and cardiac complications.
Creating a Balanced Diet Plan for Hyperparathyroidism and CKDCreating a balanced diet plan for your hyperparathyroidism and CKD can be an important step in managing your health. With the right modifications to your habits, you can ensure that you are getting the nutrition you need while avoiding any potential complications.
It is important to make sure that you are following guidelines from both your healthcare team and dietician when creating this plan. A wide variety of food should be included in order to ensure that all of your nutritional needs are being met.
Food GroupsFoods to IncludeFruits & VegetablesApples, Bananas, Carrots, SpinachGrains & StarchBreads, Rice, Potatoes, OatmealProtein FoodsChicken Breast, Fish Fillet, Eggs, LegumesDairy ProductsMilk, Yogurt Cheese cubes/slices/shreddedIt is important to keep track of what foods you eat and drink throughout the day so that you can make sure that all food groups as listed above are covered. You may also want to take into account portion sizes as well as how often each type of food is consumed in order to have a more balanced diet overall.
By making small changes over time and following these dietary guidelines it will become easier for you to create healthy eating patterns and maintain them long term.
Lifestyle Changes to Support a Hyperparathyroidism and CKD DietTaking charge of your lifestyle can help you manage hyperparathyroidism and CKD, so it's important to make small changes that support a balanced diet. The good news is there are many ways to do this without feeling overwhelmed or deprived.
Tracking food intake, making dietary adjustments, and incorporating lifestyle changes are all effective tools for managing the condition. Food tracking involves keeping a record of what you eat as well as the quantity and quality of nutrients consumed daily.
This helps you gain insight into your eating habits, identify areas where improvements can be made, and monitor how foods affect your symptoms. Additionally, tracking kidney function with lab tests such as creatinine levels will help gauge diet compliance over time.
Making dietary adjustments may also improve overall health in those with hyperparathyroidism and CKD by promoting nutrient balance from whole foods rather than relying solely on supplements.
Eating anti-inflammatory foods like fruits, vegetables, legumes, and fish; avoiding processed foods; maintaining adequate hydration; and limiting salt intake could all help reduce symptoms associated with the condition while supporting kidney function.
Small lifestyle changes such as reducing stress levels through yoga or meditation can also benefit overall health by improving emotional wellbeing, which may directly impact physical health outcomes over time.
Monitoring and Adapting Your Diet Over Time with Hyperparathyroidism and CKDMonitoring and adapting your diet over time is crucial when managing hyperparathyroidism in renal patients. When dealing with hyperparathyroidism and CKD, it is important to limit certain nutrients in your diet. Phosphorus, for example, needs to be restricted as impaired kidney function can lead to its buildup in the bloodstream.
Foods high in phosphorus, such as dairy products, legumes, and processed foods, should be limited or avoided. Calcium intake should also be monitored. Choosing calcium-rich foods with low phosphorus content, like leafy greens, is beneficial. However, caution on potassium intake must be kept in mind when consuming green leafy vegetables.
Moreover, monitoring protein intake is crucial for individuals with CKD. Restricting protein can help reduce the burden on the kidneys and manage uremic symptoms. High-quality protein sources, such as lean meats, fish, and poultry, should be consumed in moderation. Additionally, sodium intake should be limited to control blood pressure and fluid balance.
Vitamin D plays a vital role in calcium metabolism, but individuals with hyperparathyroidism and CKD often have vitamin D deficiencies. Supplementation may be necessary under the guidance of a healthcare professional.
Regular monitoring of blood levels is essential to assess the effectiveness of dietary modifications. Blood tests can evaluate calcium, phosphorus, parathyroid hormone, and other relevant parameters. Collaborating with a registered dietitian who specializes in renal nutrition can provide valuable guidance in managing your diet effectively.
As the conditions progress, dietary adjustments may be needed. Personalized dietary plans may involve more restrictive phosphorus and protein limits, depending on the severity of kidney dysfunction and parathyroid hormone levels. Adapting to these changes is crucial to maintain the best possible nutritional status and prevent complications.
Frequently Asked QuestionsWhat are the potential complications of hyperparathyroidism with CKD?Hyperparathyroidism in the presence of chronic kidney disease (CKD) can lead to various potential complications. Firstly, hyperparathyroidism can cause an imbalance in calcium and phosphorus levels, leading to the development of mineral and bone disorders.
High levels of parathyroid hormone can cause the bones to release calcium, leading to decreased mineral bone density, weakened bones and an increased risk of fractures. Excessive phosphorus levels can also contribute to bone mineral loss.
Additionally, hyperparathyroidism with CKD can exacerbate cardiovascular complications. Elevated parathyroid hormone levels are associated with increased vascular calcification, which can lead to cardiovascular disease, including heart attacks and strokes.
Furthermore, hyperparathyroidism can impact kidney function. The overproduction of parathyroid hormone can contribute to the progression of CKD, leading to further decline in kidney function.Other complications may include muscle weakness, fatigue, joint pain, and impaired immune function.
It is important for individuals with hyperparathyroidism and CKD to work closely with their healthcare team to manage and monitor these potential complications, through medication, dietary modifications, and other appropriate interventions. Regular check-ups, blood tests, and imaging studies are often necessary to assess the progression of the conditions and to identify and address any complications that may arise.
If you've been diagnosed with hyperparathyroidism and chronic kidney disease (CKD), your doctor may recommend a specific diet to manage your condition. How long to follow the diet depends on individual factors, but it's important to maintain compliance for as long as possible.
This means making attitude changes, managing stress healthily, and adjusting your lifestyle to get the right minerals from food. By following your doctor's recommended diet with dedication and ongoing symptom monitoring, you can improve your quality of life with both conditions.
When following a diet for hyperparathyroidism and chronic kidney disease (CKD), there are several foods that are generally recommended to be avoided or limited. These include:
. High-phosphorus foods: Dairy products, legumes, nuts, seeds, processed meats, and carbonated beverages should be restricted as they are rich in phosphorus, which can accumulate in the blood.
. High-calcium foods with high phosphorus content: Foods like milk, cheese, and yogurt are high in both calcium and phosphorus, so they should be consumed in moderation.
. Sodium-rich foods: Processed and packaged foods, fast food, canned soups, and salty snacks should be limited to control fluid balance and blood pressure.
. Potassium-rich foods (if necessary): Some individuals with advanced CKD may need to restrict potassium. Examples of high-potassium foods include bananas, oranges, potatoes, tomatoes, and certain vegetables.
. Foods high in oxalates (if necessary): Oxalates can contribute to the formation of kidney stones. Spinach, rhubarb, beets, nuts, and chocolate are examples of high-oxalate foods that may need to be limited.
Remember that individual dietary recommendations may vary based on the severity of CKD and other factors. It's crucial to consult with a registered dietitian who specializes in renal nutrition to create a personalized diet plan tailored to your specific needs.
It is generally advisable to limit or avoid alcohol consumption when following a diet for hyperparathyroidism and chronic kidney disease (CKD). Alcohol can have negative effects on kidney function and can interfere with the body's ability to maintain proper mineral and fluid balance.
Alcohol can also interact with medications that may be prescribed for managing hyperparathyroidism or CKD, potentially causing adverse effects or reducing their effectiveness. Furthermore, alcohol can contribute to dehydration and high blood pressure, which are concerns for individuals with CKD.
However, it is important to consult with your healthcare provider or a registered dietitian to determine if moderate alcohol consumption may be acceptable for your specific situation. They can provide personalized guidance based on the severity of your condition, overall health, and any other medications or treatments you are undergoing. It is crucial to prioritize your kidney health and follow the recommendations provided by your healthcare team.
Kidney transplantation can have a positive impact on secondary hyperparathyroidism, but it may not completely cure the condition in all cases. SHPT often develops as a result of end stage renal disease and the associated disturbances in levels of calcium, phosphorus, and vitamin D mineral metabolism.
Kidney transplantation can restore kidney function, leading to improved regulation of these metabolic processes. As a result, many individuals experience a reduction in parathyroid hormone levels after transplantation. However, some individuals may still require ongoing monitoring and management of SHPT, even after kidney transplantation. Some patients even develop tertiary hyperparathyroidism after transplant, which can be even more challenging.
Factors such as the severity of SHPT prior to transplantation, the health of the transplanted kidney, and individual variations in response to the transplant can influence the outcomes. Close follow-up with healthcare providers, including nephrologists and endocrinologists, is necessary to monitor and manage SHPT post-transplantation and ensure optimal outcomes.
In conclusion, managing hyperparathyroidism and chronic kidney disease (CKD) requires careful attention to diet and lifestyle choices.
Dietary restrictions, such as limiting foods high in calcium, phosphorus, and sodium, can help alleviate symptoms associated with these conditions. Monitoring nutrient intake, including calcium, phosphorus, vitamin D, protein, sodium, potassium, and magnesium, is crucial for maintaining overall health.
Adopting a diet rich in anti-inflammatory foods, such as fruits, vegetables, legumes, and fish, can improve well-being. It is important to understand the connection between hyperparathyroidism and CKD and how they interact.
Regular check-ups, emotional support, and professional guidance are essential for effective management. By taking control of nutrition, monitoring nutrient intake, and balancing calcium and phosphorus levels, individuals can better manage their conditions and improve their quality of life.
The post Hyperparathyroidism Diet Restriction appeared first on Renal Diet HQ.
Suggested Reading:
Phosphorus In Your Body Phosphorus In Milk Questions About Chronic Kidney Disease


