Mathea Ford's Blog, page 35
August 25, 2023
Can Kidney Disease Be Reversed
You're concerned about kidney disease, aren't you? It can be a silent predator, often undetected until it's advanced. But here's the question: Can it be reversed?
Let's explore this matter together, examining causes, symptoms, and possible lifestyle changes. We'll decipher the role of diet and early detection while unveiling helpful tools for managing this condition.
Whether you're curious about this diet and have a healthy kidney or you have acute kidney failure or even Chronic Kidney disease, there are lots of questions to be answered.
[feast_advanced_jump_to] Key TakeawaysKidney disease can be caused by various factors such as genetic influence, hormone imbalances, high blood pressure, and lifestyle choices like alcohol consumption.Dietary changes, including controlling fluid intake, limiting certain nutrients, and adopting a plant-based diet, can have a significant impact on managing kidney disease.Lifestyle changes such as staying hydrated, managing stress, getting sufficient sleep, and avoiding excessive alcohol consumption are important for kidney health.Regular check-ups and early detection of kidney disease are crucial for timely intervention and implementing necessary lifestyle changes to slow down or halt disease progression.
Key TakeawaysKidney disease can be caused by various factors such as genetic influence, hormone imbalances, high blood pressure, and lifestyle choices like alcohol consumption.Dietary changes, including controlling fluid intake, limiting certain nutrients, and adopting a plant-based diet, can have a significant impact on managing kidney disease.Lifestyle changes such as staying hydrated, managing stress, getting sufficient sleep, and avoiding excessive alcohol consumption are important for kidney health.Regular check-ups and early detection of kidney disease are crucial for timely intervention and implementing necessary lifestyle changes to slow down or halt disease progression.Understanding Kidney Disease: Causes and SymptomsFor More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
You're about to dive into the causes and symptoms of kidney disease, so you can better understand what's going on. Knowledge is power, especially when it comes to health matters.
Kidney disease is a complex condition with various triggers. The kidney structure itself plays a significant role in its vulnerability. Composed of tiny units called nephrons that filter waste products from your blood, any damage to these can lead to kidney disease.
Genetic influence is another major factor. Certain inherited conditions, like polycystic kidney disease, significantly increase your risk. It's crucial to know your family history and inform your healthcare provider about any relatives with kidney issues.
Hormone imbalances also play a part in developing this ailment. Diabetes, for instance, results in high glucose levels that over time can damage the kidneys. Conditions like hypothyroidism may also contribute due to their impact on renal functions.
Blood pressure effects are not to be overlooked either. High blood pressure forces your kidneys to work overtime leading to wear and tear over time, a perfect setup for chronic kidney disease.
Lastly, lifestyle choices such as alcohol consumption have been linked with kidney diseases by numerous studies. Alcohol dehydrates the body which forces the kidneys into overdrive filtering out toxins, a state they aren't designed for long-term.
Symptoms vary but generally include fatigue, reduced urine output or change in coloration, puffiness around eyes or swelling of hands and ankles (due to fluid build-up), unexplained shortness of breath or even an unusual sense of coldness.
Remember, knowledge equips you to better serve yourself and others facing this challenging illness.
The Role of Diet in Managing Kidney DiseaseIt's important to realize that what you eat can significantly impact the management and progression of your condition. Dietary modifications are crucial in managing kidney disease, especially concerning fluid intake, nutrient limitations, plant-based diets, and protein consumption.
In managing kidney disease, the role of a water-soluble diet can't be understated. By controlling your fluid intake, you're helping your kidneys not to overwork themselves. It's equally vital to consider nutrient limitations; excess sodium or phosphorus can lead to further complications.
Switching to a plant-based diet could be beneficial as well. These diets are rich in fiber and antioxidants which aid in reducing inflammation and managing blood pressure, two key factors when it comes to kidney health.
Protein consumption is another area requiring careful attention. Overconsumption can put more strain on your kidneys but too little may result in malnutrition. Balancing protein intake according to medical advice is key.
To evoke emotion for better understanding, here's a table showing how dietary changes affect kidney health:
Dietary AspectImpact on Kidney HealthFluid IntakeHelps prevent overworking of kidneysNutrient LimitationsPrevents complications from excess nutrients like sodium & phosphorusPlant-Based DietsReduces inflammation & manages blood pressureThe Impact of Lifestyle Changes on Kidney HealthAside from diet, there's a strong correlation between lifestyle changes and improved health of your renal system. A key aspect of the kidney diet is the importance of hydration.
Drinking plenty of water ensures that your kidneys can effectively clear toxins from your body. Aim for at least eight glasses a day, more if you're active or live in a hot climate.
Stress management also plays an integral role in maintaining kidney health. Chronic stress can indirectly lead to kidney damage by increasing blood pressure and triggering harmful behaviors like unhealthy eating or excessive alcohol consumption. It's crucial to find healthy ways to cope with stress, such as regular exercise, meditation, or talking things out with someone you trust.
Speaking of sleep patterns, getting sufficient rest is vital for overall health including that of your kidneys. Lack of sleep can lead to high blood pressure and diabetes, two major risk factors for kidney disease. Try to get seven to eight hours each night and maintain regular sleep-wake cycles during this diet plan and understanding kidney health.
You should reconsider alcohol consumption too as it poses significant risks to your kidneys when consumed excessively. It dehydrates the body and forces the kidneys to work harder than necessary which could result in long-term damage.
Lastly, controlling blood pressure is fundamental in preventing kidney disease progression since hypertension is one of its leading causes. Maintaining an optimal level through medication adherence (if prescribed), regular monitoring, balanced diet, and physical activity becomes pivotal.
In essence, prioritizing these lifestyle changes not only supports better renal function but contributes significantly towards holistic well-being - something worth striving for! While you may not be able to completely reset kidney health, these tips can help!
The Importance of Regular Check-ups and Early DetectionDon't underestimate the value of regular check-ups with your healthcare team for early detection of potential issues, as they can be a lifesaver when it comes to maintaining your overall health, acute kidney failure or not. When you prioritize preventive measures such as health screenings, you're enabling medical professionals to detect any signs of disease progression at an early stage.
Early diagnosis is particularly vital in managing kidney disease. Why? Because this condition often progresses silently and can reach advanced stages before symptoms become apparent. Here are four critical reasons why routine checks matter:
Detecting Problems Early: Regularly scheduled health screenings allow doctors to catch problems before they escalate. Diagnostic methods such as blood tests and urine tests can identify kidney damage even before you notice any symptoms.Halting Disease Progression: If detected early, lifestyle changes and medication can significantly slow down or halt disease progression.Preventing Complications: Managing kidney disease from an early stage helps prevent complications like high blood pressure, heart disease, or stroke.Providing Patient Support: A timely diagnosis equips patients with the knowledge and resources needed to manage their condition effectively.Other things to keep in mind to keep kidneys healthy with regular check-ups and early detection:
Consume as many heart-healthy foods as possible.Talk to your doctor about any underlying conditions you may have! Understand your own personal risk for kidney disease. There are many types of kidney failure. Blood clots, excess fluid, extra fluid, and alcohol, are all part of what people with kidney disease have to deal with. Medication Management: What to Take and What to AvoidYou've got to know that managing your prescribed medication, understanding what to take and what to avoid, plays a crucial role in maintaining overall health. Being aware of potential drug interactions is key, as some types of medication can either enhance or reduce the effectiveness of others when taken together. Misunderstanding these interactions could lead not only to ineffectiveness but also to severe medication side effects.
Prescription adherence is another vital aspect of proper medication management. You're not alone if you occasionally forget a dose or skip it due to side effects.
But consistency is essential for many medications, especially those treating chronic conditions like kidney disease. If skipped doses become frequent, it may result in suboptimal treatment outcomes.
Over-the-counter (OTC) medicines are often perceived as harmless because they don't require a prescription. However, OTC risks are real, as excessive use or misuse can cause serious health problems.
For instance, prolonged use of non-prescription pain relievers may harm kidney function. A good example is blood pressure medication, a proper doctor has to monitor you to help you reset kidney health.Â
The Role of Exercise and Maintaining a Healthy Weight in Kidney HealthWhile managing medication is crucial for kidney health, let's now turn our attention to the significant role of regular exercise and maintaining a healthy weight.
You might ask, 'How do these factors play into kidney health?' Here's what you need to know:
Exercise Benefits: Regular physical activity can help control high blood pressure and lower your risk for type 2 diabetes, two key factors in preventing kidney disease. It doesn't have to be strenuous; even brisk walking or light jogging can make a difference.Weight Monitoring: Keeping an eye on your weight is equally important as excess weight increases the strain on your kidneys. By achieving and maintaining a healthy weight, you're not only protecting your kidneys but also improving overall health.Fitness Regimens: The type of exercise matters too! A balanced mix of cardio and strength training could work wonders for your body, including your kidneys. Remember, it's essential to start slow and gradually increase intensity based on your comfort level.Hydration Importance: While hydration is vital for everyone, those with kidney issues need to monitor their fluid intake carefully. Over-hydration can cause problems like swelling or high blood pressure whereas dehydration could lead to acute kidney injury.Beyond physical well-being, don't underestimate the power of stress management in preserving kidney health. High-stress levels may lead to unhealthy coping mechanisms such as smoking or overeating, habits detrimental to both kidneys and overall wellness. The risk of kidney disease is great but there are lots of things you can doÂ
The Dangerous Effects of Smoking on Kidney HealthIt's vital to understand that smoking greatly affects your overall health. Notably, it can cause serious damage to your body's filtering system. Tobacco toxins are harmful substances that directly influence the functioning of your kidneys.
They increase blood pressure and heart rate, reducing blood flow in the kidneys and narrowing the blood vessels. This accelerates kidney disease progression.
But there is hope with smoking cessation. Quitting this habit can significantly reduce the risk of developing kidney disease or slow its progression if already present.
Nicotine replacement therapy (NRT) such as patches, gum, or inhalers can be an effective part of a plan to leave this damaging habit behind. These products provide controlled doses of nicotine to help ease withdrawal symptoms.
Equally important is behavioral therapy, which focuses on learning new coping skills and breaking those habitual ties associated with smoking. It provides strategies like mindfulness practices to deal with cravings or social situations where you might feel tempted to smoke.
Remember too, not just smokers suffer the ill effects; secondhand smoke also poses a threat to others' kidney health by inhaling these tobacco toxins involuntarily. So, your decision towards quitting benefits not only you but also those around you.
Pain Management Strategies for Kidney Disease PatientsManaging your pain effectively becomes crucial when dealing with chronic health issues. Many people report all kinds of pain from headaches down to abdominal pain. As a kidney disease patient, you're no stranger to discomfort, but there are strategies you can use to improve your well-being.
These include alternative therapies and non-pharmacological interventions that aim at altering your pain perception and boosting psychological coping during the different stages of kidney failure.Â
Mind-body techniques: This involves practices like meditation, progressive muscle relaxation, and guided imagery designed to enhance the mind's capacity to affect bodily functions and symptoms.Physical Therapy: Regularly participating in exercises tailored for kidney patients can help alleviate pain by strengthening muscles around the kidneys.Alternative Therapies: Acupuncture or massage therapy may prove beneficial in addressing the physical origins of your pain.Psychological Coping Mechanisms: Cognitive behavioral therapy can be used to help you deal with stressors related to chronic illness and manage emotional responses linked with painful experiences.These methods aren't one-size-fits-all solutions, so it's important you work closely with healthcare providers to tailor an approach that best addresses your unique circumstances. Remember, managing chronic pain goes beyond just dulling the sensation, it also entails promoting overall wellness.
Incorporating these approaches into your routine could significantly improve your quality of life as a kidney disease patient. By focusing not only on physical treatment but also on mental resilience, you're better equipped to handle the trials brought about by this condition, not just surviving, but thriving amidst adversity.
The Progression of Chronic Kidney Disease: Can It Be Slowed?You're probably wondering if the progression of your chronic condition can be slowed down, and the answer is yes, with the right treatment plan and lifestyle modifications. Chronic kidney disease, while often influenced by genetic predisposition, can be managed effectively.
One important aspect to consider is dialysis effectiveness. Dialysis works as an artificial kidney when your own kidneys are no longer functioning adequately. However, it's not a cure-all, it's critical to maintain a balanced diet and healthy weight alongside regular dialysis treatments.
Genetic PredispositionLifestyle ModificationsAffects how quickly CKD progressesCan slow progressionMay necessitate earlier transplant considerationMay delay need for transplantationTransplant consideration should always be on your mind. If you've reached end-stage renal disease (ESRD), receiving a kidney transplant could significantly improve your quality of life and long-term health outcomes.
Psychological impact cannot be ignored either. Living with chronic disease can take a toll on mental health, seeking support from professionals or support groups could prove beneficial in managing stress and anxiety.
Lastly, explore alternative treatments too. Some patients have found relief through acupuncture or herbal remedies (with medical consultation). These alternatives may complement conventional treatments rather than replace them but could help manage symptoms more holistically.
Helpful Tools and Resources for Managing Kidney DiseaseWhile slowing the progression of kidney disease is vital, it's equally critical to manage your condition effectively. You're not alone in this journey, and there are numerous resources available that can help you navigate these challenging waters.
Disease Education: Educate yourself about kidney disease. Understanding your condition will empower you to make better decisions regarding your health. Numerous online platforms provide accurate medical information, such as the National Kidney Foundation or Mayo Clinic websites.Support Groups: It's important for maintaining your mental health that you don't feel isolated during this difficult time. Connect with others who are on similar journeys through support groups both locally and online. Sharing experiences and coping strategies can be immensely beneficial.Advanced Treatments: Keep abreast of advancements in treatment options for kidney disease by regularly consulting with your healthcare provider or doing independent research online. New treatments are continually being developed thanks to technology advancements in medicine, often offering improved patient outcomes and quality of life.Technology Advancements: Utilize technology to manage your kidney disease more efficiently, from mobile apps that track symptoms or aid medication management, to wearable devices that monitor vitals real-time.Remember, managing a chronic illness like kidney disease goes beyond just addressing physical symptoms. It also involves taking care of your emotional well-being and equipping yourself with knowledge through continuous education about the condition.
These tools and resources could significantly improve how you handle the challenges brought by chronic kidney diseases. Empowering you not only survive but thrive despite having this condition.
Whether you struggle with kidney transplantation, mild kidney damage, normal kidney function, or reduce kidney function, there are so many options for treatment of kidney disease.
Frequently Asked QuestionsWhat Are the Genetic Factors That Can Contribute to Kidney Disease?Certain genes can raise your chances of kidney disease and your risk of kidney damage, especially adult kidneys. Genetic testing can reveal these inherited risks, helping you understand your disease progression.
Mutations in specific genes like PKD1 or PKD2 often lead to polycystic kidney disease. Gene therapy is a potential future treatment to correct defective genes.
Consulting with genetic counseling services, you'll gain valuable insights about your genetic predispositions and how they might impact your health. It's important for serving not just yourself but also your family's health needs.
Yes, mental stress and emotional health problems can potentially impact your kidney health. It's crucial for your overall well-being, including kidney health, to effectively manage stress and build emotional resilience.
Anxiety and depression may indirectly affect kidneys by influencing behaviors detrimental to kidney function. So, maintaining mental well-being goes hand in hand with physical health. It's not a direct cause but a contributing factor that you shouldn't overlook.
Survival rates for advanced kidney disease vary. Dialysis effectiveness and transplant possibilities, as well as nutrition influence, exercise impact, and medication advancements, all play a role. If you're on dialysis, your lifespan could be extended by years.
A successful transplant could mean many more years of life. A healthy diet and regular exercise also contribute positively to survival rates. Medication advancements continue to improve outcomes too.
In conclusion, you can't fully reverse every type of kidney disease, but you can slow its progression. By adjusting your diet, making lifestyle changes, and having regular check-ups, you'll stand a better chance.
Quit smoking and manage your medication wisely too. Remember to monitor pain levels effectively to avoid even more loss of kidney function.
There are ample resources available for managing kidney disease, make the most of them! No matter what stages of kidney disease you're in, there is a kidney-friendly diet out there for you! The history of kidney disease has been a rough one, but there are plenty of options out there for those with Chronic Kidney Failure.Â
The post Can Kidney Disease Be Reversed appeared first on Renal Diet HQ.
Suggested Reading:
What Is Chronic Kidney DiseaseChronic Illness and CKDDiabetic Renal Diet Meal PlanAugust 23, 2023
How Much Sodium per Day for Renal Diet
Sodium is a mineral that is found in many foods. Many processed foods and prepared foods have added amounts of sodium to preserve the contents.
You may be steadily decreasing the fat in your diet but not realize how much sodium you take in and how it is affecting your kidneys.

Sodium can be linked to increased blood pressure, and increased blood pressure levels cause damage to your kidneys over time whether you're aware of your blood pressure being high or not. Sodium can also make you feel dehydrated.
You're eager to better manage your chronic kidney disease (CKD) and you've heard sodium intake plays a big part in the dietary management aspect. But how much is too much?
It's time you understood the ins and outs of a renal-friendly diet, especially when it comes to sodium. Let's decode food labels, highlight hidden sodium culprits, and help you make healthier choices.
[feast_advanced_jump_to]Key TakeawaysSodium plays a crucial role in maintaining optimal bodily function and overall wellbeing.Extra sodium intake can lead to high blood pressure and heart disease.Balancing sodium intake is crucial for individuals with kidney disease.Hidden sodium in processed foods and restaurant meals should be avoided.Understanding the Role of Sodium in the BodySodium is a fundamental electrolyte vital for human survival, playing a crucial role in various physiological processes. Here, we delve into the significance of sodium in the body, exploring its profound impact on health.
We will also unravel the intricate mechanisms by which the body regulates sodium levels, shedding light on the delicate balance between dietary sodium intake and overall well-being. Understanding sodium's role is essential in renal health.
Role of Sodium in Normal Body FunctionsFor More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
Sodium is a crucial electrolyte with a vital role in maintaining normal body functions. It primarily functions in conjunction with potassium to regulate fluid balance, nerve function, and muscle contractions.
Sodium helps transmit nerve impulses by facilitating the movement of electrical signals across cell membranes. It also plays a key role in muscle contraction, including the beating of the heart. Additionally, sodium is vital for maintaining proper hydration levels in the body, as it helps regulate fluid balance by controlling water distribution between cells and the bloodstream.
Without adequate sodium, our bodies would struggle to maintain blood pressure, nerve function, and muscle coordination, emphasizing its indispensable role in overall health and wellbeing.
However, it's essential to strike a balance, as excessive dietary sodium intake can lead to health problems like high blood pressure and cardiovascular issues.
Sodium Regulation in BodyThe body has intricate mechanisms to regulate sodium levels, crucial for maintaining overall health. One of the primary regulators is the renin-angiotensin-aldosterone system (RAAS). When blood sodium levels drop, specialized cells in the kidneys release renin, which initiates a cascade leading to the release of aldosterone. Aldosterone signals the kidneys to reabsorb sodium, preventing excessive loss in urine.
Another crucial regulator is the hormone atrial natriuretic peptide (ANP), which opposes aldosterone's effects. When blood pressure rises or the heart's atria stretch due to increased blood volume, ANP is released, prompting the kidneys to excrete sodium and reduce blood volume and pressure.
Furthermore, the sensation of thirst can be triggered when sodium levels are too high, encouraging increased fluid intake to help dilute sodium concentrations.
This intricate system of hormonal and neural controls maintains the delicate balance of sodium in the body, ensuring that it remains within a narrow and vital range for optimal physiological function.
Sodium's Impact on HealthSodium plays a dual role in health, with both essential benefits and potential risks. On the positive side, sodium is crucial for maintaining proper fluid balance, nerve function, and muscle contractions. Adequate dietary sodium intake is necessary for overall bodily function, especially in regulating blood pressure, which is essential for cardiovascular health.
However, excessive sodium consumption, often associated with a high-salt diet, can have detrimental effects on health. It is a leading contributor to high blood pressure (hypertension), a major risk factor for heart disease, stroke, and kidney problems. High sodium intake can also lead to fluid retention, which may exacerbate conditions like congestive heart failure.
Balancing dietary sodium intake is essential. It involves not only reducing the consumption of highly processed, sodium-laden foods but also ensuring an adequate intake of potassium, which counteracts sodium's effects.
Monitoring dietary sodium intake can help individuals maintain their health by striking the right balance and preventing the adverse consequences of excessive sodium consumption.
Sodium Limits for Those With Kidney DiseaseIn individuals with Chronic Kidney Disease, understanding the importance of sodium limits is paramount. Here, we look into the critical reasons behind the necessity of restricting sodium intake for CKD patients. We explore the potential consequences of excess sodium on kidney function and overall health. Discovering the delicate balance between sodium consumption and kidney health is crucial for managing CKD and enhancing the quality of life for those affected by this condition.
Why Sodium Is Controlled in CKDControlling dietary sodium intake is crucial in Chronic Kidney Disease due to the impaired kidney function characteristic of the condition. As CKD progresses, the kidneys' ability to filter waste products and regulate electrolytes, including sodium, diminishes. This can lead to sodium retention in the body, resulting in elevated blood pressure, fluid retention, and swelling, further burdening the already compromised kidneys.
High sodium levels can also disrupt the balance of other essential electrolytes, like potassium and calcium, potentially leading to dangerous imbalances. Moreover, excessive sodium intake can exacerbate proteinuria, a condition where the kidneys leak valuable proteins into the urine, accelerating kidney damage.
By controlling dietary sodium intake, CKD patients can help manage blood pressure, reduce the strain on their kidneys, and maintain a more stable internal environment, ultimately slowing the progression of the disease and enhancing their overall well-being.
Determining Safe Sodium LevelsSafe sodium levels for individuals with Chronic Kidney Disease are significantly lower than the average American intake.
While the Dietary Guidelines for Americans suggest limiting intake to less than 2,300 milligrams of sodium per day for most adults, CKD patients, especially those with advanced stages, are often advised to aim for even stricter limits, typically around 1,500 milligrams of sodium per day.
This reduced sodium target is essential because impaired kidney function in CKD makes it challenging to excrete excess sodium efficiently. High dietary sodium intake can lead to fluid retention, elevated blood pressure, and increased strain on the kidneys, potentially accelerating the progression of kidney damage.
Being able to limit sodium intake can help mitigate these risks, manage blood pressure, and slow CKD progression, thereby enhancing the quality of life and long-term outcomes for individuals battling this chronic condition.
It's crucial for CKD patients to work closely with healthcare professionals to establish personalized dietary guidelines based on their specific health needs.
Effects of Excess SodiumExcessive salt intake in Chronic Kidney Disease patients can exacerbate their condition and lead to a range of complications and clinical implications. High dietary sodium levels can contribute to fluid retention, elevated blood pressure, and a heightened risk of cardiovascular events, all of which are particularly concerning for individuals with compromised kidney function.
Furthermore, excessive salt can directly harm the kidneys by increasing proteinuria and oxidative stress, accelerating the progression of CKD. It may also disturb electrolyte balance, potentially causing hyperkalemia or hyponatremia, further jeopardizing renal health.
Additionally, salt-induced hypertension can strain the already weakened kidneys, amplifying proteinuria and kidney damage. These complications underscore the importance of strict dietary sodium restriction in the diet of CKD patients to mitigate the adverse effects on their already vulnerable renal and cardiovascular systems.
Complications of Excessive Salt Intake in CKD Patients:
ComplicationDescriptionFluid RetentionExcess sodium can lead to fluid buildup, exacerbating edema and increasing blood pressure.HypertensionHigh salt intake is a major contributor to elevated blood pressure, elevating the risk of cardiovascular events.Cardiovascular EventsElevated blood pressure and sodium-related damage increase the likelihood of heart problems and stroke.Kidney DamageExcessive salt may directly harm the kidneys, accelerating proteinuria and oxidative stress.Electrolyte ImbalancesSodium imbalance can lead to hyperkalemia or hyponatremia, further compromising renal function.Proteinuria ExacerbationHigh dietary sodium intake worsens proteinuria, worsening kidney damage in CKD patients.Decoding Nutritional Information on Food PackagingIn this article section, we delve into the critical aspects of Understanding Sodium Content Labels and Comparing Sodium in Products. We will break down the intricacies of interpreting sodium information on food labels, helping you grasp its significance in your diet.
Additionally, we'll provide practical guidance on how to effectively compare sodium levels among different food items, enabling you to make informed choices that align with your dietary sodium restrictions.
Understanding Sodium Content LabelsInterpreting sodium or salt labels is crucial for making informed dietary choices. These labels convey the sodium content and can greatly impact your health:
Sodium per Serving: This indicates the amount of sodium in one serving of the product. It's essential to check serving sizes to avoid underestimating your dietary sodium intake.Low Sodium: Foods labeled as "low sodium" contain a relatively small amount of sodium per serving. This is generally defined as 140 milligrams or less of sodium per serving.Lite (or Light): This label may suggest a reduced sodium content but doesn't always guarantee it. Check the nutrition facts to confirm the actual sodium levels.No Salt (or Salt-Free): These products should contain virtually no added salt. Be cautious as they may still have natural sodium from ingredients.Less Sodium: Foods labeled as "less sodium" should have at least 25% less sodium compared to the regular version of the product.To maintain a heart-healthy diet, focus on products with lower sodium per serving and be vigilant about serving sizes and label claims.
Comparing Sodium in ProductsComparing sodium levels in different food products is essential for making informed dietary choices, especially for individuals aiming to reduce their dietary sodium intake. Here's how to effectively compare sodium in products:
Check Serving Sizes: Always compare sodium content based on the same serving size for accurate assessments.Read Nutrition Labels: Review the Nutrition Facts labels on packaging. Look for the "Sodium" or "Salt" content, typically measured in milligrams (mg) per serving.Use Percent Daily Value (%DV): This percentage helps you see how much a serving contributes to your daily sodium limit (usually around 2,300 mg for healthy adults). Aim for products with lower %DV for sodium.Compare Similar Items: When choosing between similar products, opt for the one with the lower sodium content.Consider Unprocessed Foods: Whole, unprocessed foods generally contain less sodium compared to their processed counterparts, making them a healthier choice.Be Cautious of "Light" Claims: "Light" doesn't always mean lower sodium. Check the label for confirmation.By diligently comparing sodium levels, you can make choices that align with your dietary goals and reduce the risk of health issues associated with excessive dietary sodium intake, such as high blood pressure and cardiovascular disease.
Unmasking Hidden Sodium in Everyday FoodsYou might be surprised to learn about the hidden sodium lurking in many of your favorite processed foods, often in amounts that can significantly impact your daily intake.
But don't worry, there are alternatives such as sodium substitutes that you could consider to help manage and reduce your sodium consumption.
However, it's important to understand that these alternatives aren't without their own set of risks and potential side effects which we'll explore in detail.
Sodium in Processed FoodsSodium plays a multifaceted role in processed foods, serving as a preservative, flavor enhancer, and texture modifier. Its preservative properties help extend the shelf life of products, preventing spoilage.
Beyond sodium chloride (table salt), various sodium additives are prevalent in processed foods, including sodium bicarbonate (baking soda), sodium benzoate, sodium citrate, and sodium nitrate/nitrite. These additives serve diverse functions, such as regulating acidity, enhancing flavors, and preserving color and texture.
However, excessive dietary sodium intake from processed foods can lead to health concerns, particularly high blood pressure and an increased risk of cardiovascular disease, especially for patients with kidney disease.
It's essential for consumers to scrutinize food labels for anything with the word “sodium,” opt for products with lower sodium content, and limit their consumption of heavily processed items.
Sodium Substitutes and RisksSalt substitutes are often used as alternatives to traditional table salt (sodium chloride) to reduce dietary sodium intake, which can be beneficial for individuals with hypertension or other health concerns. Common salt substitutes include potassium chloride, magnesium-based salts, and blends of various herbs and spices.
Potassium chloride, a primary salt substitute, can help lower blood pressure by balancing sodium-potassium ratios. However, it should be used cautiously, as excessive potassium intake can be harmful, especially for those with kidney problems. High potassium levels can lead to muscle weakness, irregular heart rhythms, and in severe cases, cardiac arrest.
Magnesium-based salts can be another substitute but should be monitored, as excessive magnesium intake may lead to diarrhea and stomach discomfort.
Blends of herbs and spices can enhance flavor without adding sodium or potassium, making them a healthier option. Nevertheless, individuals should be cautious with any salt substitute, especially if they have underlying health conditions, and consult with a healthcare professional for guidance on their specific dietary needs.
Practical Suggestions for Lowering Sodium ConsumptionHere, we discuss how to have a healthier, tastier diet even when reducing your salt consumption. In this section, we explore the art of flavor enhancement through herbs and spices, allowing you to savor your meals without excess sodium.
Additionally, we unveil smart meal planning techniques that make reducing dietary sodium intake a breeze. Striking a balance between sodium restriction and having flavorful meals is essential in starting a kidney friendly eating plan that you can enjoy without compromising your health.
Adding Flavor Without Adding SaltMaximizing flavors through herbs and spices is an essential culinary strategy for those on a salt-restricted renal diet. Such diets are crucial for managing chronic kidney disease and maintaining overall health. By reducing sodium, the risk of fluid retention and high blood pressure is mitigated, alleviating strain on the kidneys.
However, this dietary restriction need not result in bland, unappetizing meals. Herbs like basil, thyme, and rosemary, as well as spices like cumin, paprika, and turmeric, offer a treasure trove of flavors without compromising sodium levels. They add complexity, aroma, and depth to dishes, making them not only kidney-friendly but also delicious.
This approach empowers individuals to embrace a flavorful, satisfying, and health-conscious culinary journey while adhering to their salt-restricted renal diet.
Meal Planning StrategiesManaging a low salt diet is essential for individuals with chronic kidney disease to protect kidney function and overall health. Effective meal planning is a cornerstone of this dietary approach. Here are key strategies to reduce salt and processed foods while maximizing flavor with herbs and spices:
Whole, Fresh Ingredients: Prioritize fresh fruits and vegetables, lean proteins, and whole grains. These items are naturally lower in sodium and provide essential nutrients.Label Reading: Scrutinize food labels for sodium content. Opt for products with lower sodium levels or choose those labeled as "low sodium" or "sodium-free."Home Cooking: Preparing meals at home allows you to control ingredients and sodium content. Avoid canned or pre-packaged foods, which often contain high levels of sodium.Spice It Up: Embrace the world of herbs and spices to infuse flavor into dishes. Basil, oregano, cumin, bay leaf, and garlic powder can elevate your meals without sodium.Limit Processed Meats: Reduce consumption of processed meats like bacon, sausages, and deli meats, as they are high in sodium and additives.Fresh Herbs and Citrus: Incorporate fresh herbs like cilantro and parsley, and use citrus fruits like lemon and lime to add zing to salads and proteins.Low-Sodium Broths: Choose low-sodium or homemade broths for soups and stews such as chicken noodle soup instead of their high-sodium counterparts.Ditch the Salt Shaker: Avoid adding table salt during cooking or at the dining table. Allow natural flavors to shine through.Experiment: Don't be afraid to experiment with different herb and spice combinations to find your favorite flavor profiles.Meal Prep: Prepare your custom meal plans in advance to ensure a well-balanced, low salt diet. This helps you avoid impulsive choices that may be high in salt.By implementing these strategies, individuals on a low sodium renal diet can create a menu that's not only kidney-friendly but also delicious and satisfying. It's about reimagining the role of herbs and spices as the stars of the show in your culinary journey, making every meal a flavorful and health-conscious experience.
Identifying High-Sodium Foods to AvoidYou might not realize it, but your daily sodium intake could be higher than you think, especially if you're regularly consuming processed foods and restaurant meals. It's important to understand that these types of foods often contain a significant amount of hidden sodium, which can have adverse effects on your health.
Processed Foods' Sodium ContentIn a renal diet, avoiding high-sodium processed foods is crucial to manage chronic kidney disease effectively. High sodium intake can lead to fluid retention, elevated blood pressure, and worsen kidney function. Here are common high-sodium processed foods to steer clear of:
Canned Soups: Many canned soups contain excessive salt, with some brands exceeding your daily recommended dietary sodium intake in a single serving.Processed Meats: Bacon, sausages, hot dogs, and deli meats are loaded with sodium and often contain additives that are harmful to kidneys.Canned Vegetables: Canned vegetables are often preserved in salty brines, significantly increasing their sodium content.Frozen Meals: Convenience frozen meals, including pizzas, burritos, and TV dinners, can be extremely high in sodium to enhance flavor and shelf life.Fast Food: Fast-food items like burgers, fries, and fried chicken are notorious for their sodium content due to added salt and processed ingredients.Condiments: Soy sauce, ketchup, barbecue sauce, and salad dressings can be sodium-rich condiments. Opt for low-sodium or make homemade versions.Snack Foods: Chips, pretzels, and salted nuts are often drenched in sodium to satisfy cravings.Canned and Processed Cheese: Cheese spreads and processed cheese products are high in sodium.Packaged Sweets: Baked goods, cakes, and cookies can contain hidden sources of sodium in baking powder or soda.Salty Seasoning Blends: Seasoning packets, bouillon cubes, and some spice blends can be excessively salty.Avoiding these high-sodium processed foods is essential for preserving kidney function and overall health in a renal diet. Instead, focus on fresh, whole foods and flavor enhancement through herbs and spices to maintain a well-balanced, kidney-friendly diet.
Sodium in Restaurant MealsWhen following a low salt diet, it's essential to be cautious about restaurant meals that can be excessively high in salt, as excessive sodium intake can lead to health issues like hypertension and heart disease. Several restaurant dishes are notorious for their sodium content and should be avoided or consumed sparingly.
Firstly, fast food options like burgers, fries, and fried chicken tend to be laden with salt, both in the meats and the accompanying condiments. Similarly, many Asian dishes, such as soy sauce-heavy stir-fries or sushi with soy sauce dipping, can be sodium bombs.
Mexican cuisine can also be problematic due to the use of salty cheeses, sauces, and processed meats in dishes like nachos, tacos, and burritos. Additionally, canned soups, broths, and gravies used in various restaurant recipes can contain excessive sodium.
To maintain a low sodium diet while dining out, opt for grilled or steamed dishes, request sauces and dressings on the side, and inquire about low-sodium menu options if available. Being mindful of these high-sodium culprits can help you make healthier choices when dining in restaurants.
Seeking Out Low-Sodium AlternativesIn this section, we look at real-world tips on how to seek out low sodium alternatives. By adopting mindful grocery shopping and preparing meals at home, we'll uncover how small changes in our daily choices can lead to significant health benefits, especially for people with kidney disease.
Low-Sodium Shopping StrategiesFor individuals with Chronic Kidney Disease (CKD), managing sodium intake is crucial to prevent fluid retention and maintain kidney health. Here are some essential low-sodium shopping strategies:
Read Labels: Scrutinize food labels for sodium content. Look for products with "low-sodium," "sodium-free," or "no salt added" labels.Fresh is Best: Choose fresh foods over processed options. Fresh fruits, vegetables, lean meats, and unprocessed grains are naturally lower in sodium.Limit Canned Goods: Canned foods often contain added salt for preservation. If using canned items, rinse them thoroughly to reduce sodium content.Select Low-Sodium Alternatives: Opt for low-sodium or sodium-free versions of condiments like soy sauce, broth, and canned soups.Herbs and Spices: Enhance flavor with herbs, spices, and salt-free seasoning blends instead of salt.Dairy Choices: Select low-sodium or sodium-free dairy products like yogurt and cheese.Plan Meals: Plan menus in advance to control sodium intake and avoid last-minute high-sodium choices. Make sure to bring a comprehensive shopping list to prevent impulse purchases.Consult a Dietitian: Seek guidance from a registered dietitian who can tailor a low-sodium diet to your specific CKD stage and dietary requirements.Home Cooking BenefitsHome cooking offers numerous advantages for individuals aiming to maintain a low sodium diet:
Control Over Ingredients: When you cook at home, you have complete control over what goes into your meals, allowing you to choose low-sodium alternatives and fresh ingredients.Portion Management: Home-cooked meals enable you to manage portion sizes, reducing the risk of overeating and excessive sodium intake.Flavor Customization: You can experiment with herbs, spices, and salt-free seasonings to enhance flavors without relying on excessive salt.Reduced Processed Foods: Cooking at home minimizes reliance on processed and fast foods, which often contain hidden sodium.Healthier Cooking Techniques: You can employ healthier cooking methods like grilling, baking, steaming, and sautéing, which inherently reduce sodium content compared to frying or deep-frying.Personalized Diet: Home cooking allows you to tailor meals to specific dietary needs or restrictions, ensuring a low sodium diet that aligns with your health goals.Cost-Efficiency: Cooking at home can also be cost-effective and may promote better overall nutrition.Incorporating home-cooked meals into your routine empowers you to make informed choices and maintain better control over sodium intake, promoting better health and quality of life, even with CKD.
The Impact of Controlled Sodium Intake on Renal HealthWhen you keep your sodium intake under control, you'll not only support healthier kidneys but also enjoy overall health benefits. These benefits include better blood pressure control and minimized risk of heart disease.
Sodium's Role in Renal HealthControlled sodium intake significantly benefits kidney health in several ways:
Blood Pressure Regulation: High sodium consumption can lead to elevated blood pressure, increasing the strain on the kidneys. By reducing sodium intake, blood pressure can be better managed, preventing kidney damage.Slower Progression of CKD: In individuals with Chronic Kidney Disease, limiting sodium intake can slow down the progression of the disease, preserving kidney function over time.Reduced Risk of Kidney Stones: Lower sodium levels in the diet help minimize the formation of kidney stones, which are often composed of salts and minerals.Prevention of Edema: Controlling sodium intake helps prevent fluid retention (edema) in the body, which can strain the kidneys and exacerbate kidney problems.By maintaining a balanced and low-sodium diet, individuals can promote kidney health, reduce the risk of kidney-related complications, and enhance overall well-being.
Controlled Sodium Intake BenefitsControlling sodium intake offers a multitude of health benefits:
Management of Blood Pressure: Reduced sodium intake helps regulate blood pressure, lowering the risk of hypertension and related cardiovascular diseases.Heart Health: Lower sodium levels contribute to a healthier heart, reducing the risk of heart attacks, strokes, and other heart-related conditions.Kidney Function: Managing sodium can alleviate strain on the kidneys, preserving their function and reducing the risk of kidney disease or worsening existing kidney conditions.Bone Disease: High sodium diets can lead to calcium loss from bones, increasing the risk of osteoporosis. Lower sodium intake helps maintain bone density.Reduced Fluid Retention: Controlling sodium levels minimizes fluid retention, easing discomfort for individuals with conditions like edema or congestive heart failure.Digestive Health: Lower sodium intake can alleviate symptoms of certain digestive disorders, such as acid reflux and gastritis.Overall Well-being: A balanced sodium intake supports overall health, providing more energy, better sleep, and improved quality of life.By managing sodium intake, individuals can enjoy improved health and reduce the risk of various chronic diseases, ultimately leading to a longer, more vibrant life.
Sample Low Sodium Diet Meal PlanBreakfast: Scrambled Egg Whites with Vegetables (Sodium: 90 mg)
2 egg whites scrambled with bell peppers.A slice of whole-grain toast (check for low-sodium bread).Fresh fruit salad (berries, banana, and apple).Lunch: Quinoa and Chickpea Salad (Sodium: 280 mg)
A generous portion of quinoa mixed with low-sodium chickpeas, cucumber, red onion, and parsley.Dress with a homemade vinaigrette using olive oil, lemon juice, and salt-free herbs and spices.Sliced carrots and celery sticks for added crunch.Snack: Greek Yogurt with Berries (Sodium: 45 mg)
A serving of plain, low-sodium Greek yogurt.Top with fresh berries and a drizzle of honey.Dinner: Baked Lemon Herb Chicken (Sodium: 240 mg)
Skinless chicken breast or lean chicken strips marinated in lemon juice, garlic, and a blend of salt-free herbs and spices.Baked sweet potato with a sprinkle of fresh herbs.Steamed broccoli with lemon zest.Snack (if needed): Almonds (Sodium: 0 mg)
A small handful of unsalted almonds for a satisfying crunch.Day's Total Sodium: 655 mg
This sample low-sodium meal plan keeps salt intake well below the recommended 1500 milligrams of sodium per day for individuals on a restricted sodium diet. It also avoids high potassium and high phosphorus ingredients, making it suitable for those with kidney concerns.
Adjust portion sizes and ingredients to fit personal dietary requirements and consult a healthcare professional or dietitian for personalized guidance on managing sodium intake, especially if you have specific medical conditions or dietary restrictions.
Frequently Asked QuestionsWhat Are the Potential Side Effects of Consuming Too Little Sodium?Consuming too little sodium can lead to several potential side effects, including muscle cramps, weakness, nausea, vomiting, dizziness, and headaches. Extremely low sodium levels, known as hyponatremia, can be life-threatening, causing confusion, seizures, and, in severe cases, coma. It's important to strike a balance in sodium intake, as excessive restriction can disrupt the body's electrolyte balance. It's crucial to consult with a healthcare professional or registered dietitian to determine an appropriate sodium intake level based on individual health needs and conditions.
How Does Sodium Intake Affect Blood Pressure in Individuals With Kidney Disease?In individuals with kidney disease, sodium intake can significantly impact blood pressure. The kidneys play a vital role in regulating sodium levels in the body. When kidney function is compromised, excess sodium can accumulate, leading to fluid retention and elevated blood pressure. High blood pressure can further damage the kidneys, creating a vicious cycle. Therefore, limiting sodium intake is crucial for managing blood pressure and slowing the progression of kidney disease. Medical guidance and personalized dietary recommendations from a healthcare provider or dietitian are essential for individuals with kidney disease to maintain optimal sodium levels and protect their kidney health.
Check Out Our Meal Plans For People With Chronic Kidney Disease (CKD)Avoiding Sodium Avoids ComplicationsManaging your sodium intake is crucial for kidney health. By understanding food labels, avoiding high-sodium foods, and choosing low-sodium alternatives, you can make informed choices that support your renal diet.
Remember, balancing sodium isn't just about restriction; it's about making smarter decisions every day, and maximizing strategies such as the use of herbs and spices and being vigilant about food labels.
Adjusting to a low sodium diet may be difficult when you’re used to consuming salty foods on a regular basis, but this restriction is necessary not only to improve your health but also to maintain your well being and avoid complications.
The post How Much Sodium per Day for Renal Diet appeared first on Renal Diet HQ.
Suggested Reading:
What Is Chronic Kidney DiseaseDiabetic Renal Diet Meal PlanFoods To Avoid With Kidney DiseaseAugust 22, 2023
Renal Failure Diets
You're on a mission to help those with renal failure live healthier lives. Understanding the role of diet is key, and we've got you covered.
We'll discuss crucial dietary restrictions, sodium control, protein management, heart-healthy choices, and more.
You'll develop strategies for effectively managing phosphorus and potassium intake too.
Itâs time to discover how a balanced renal failure diet can make all the difference.
 [feast_advanced_jump_to]Key TakeawaysDiet plays a crucial role in managing renal failure and can either strain or support kidney function.Nutrient-rich foods like watermelon and kidney beans can support kidney function due to their high water content, essential nutrients, fiber, and low sodium levels.Controlling nutritional intake, including limiting sodium and protein intake, is essential for managing kidney health in those with impaired functionality.Sodium management is important for maintaining overall health and supporting kidney health. It is crucial to avoid processed foods and incorporate fresh fruits and vegetables to control sodium intake effectively.Understanding the Role of Diet in Renal Failure
[feast_advanced_jump_to]Key TakeawaysDiet plays a crucial role in managing renal failure and can either strain or support kidney function.Nutrient-rich foods like watermelon and kidney beans can support kidney function due to their high water content, essential nutrients, fiber, and low sodium levels.Controlling nutritional intake, including limiting sodium and protein intake, is essential for managing kidney health in those with impaired functionality.Sodium management is important for maintaining overall health and supporting kidney health. It is crucial to avoid processed foods and incorporate fresh fruits and vegetables to control sodium intake effectively.Understanding the Role of Diet in Renal FailureYou're about to delve into an insightful discussion that explores the significant impact of diet on kidney health. Specifically, we'll focus on how nutritional control can manage renal failure.
Engaging with evidence-based findings, we'll investigate how certain dietary choices can either strain or support your kidneys' function.
We'll also unravel the potential of nutritionally controlling renal failure, offering a holistic perspective on this critical health issue at any stage of kidney disease.
Diet's Impact on KidneysFor More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
It's crucial to understand how diet directly impacts kidney health, particularly for those with renal failure. You can optimize your' health by focusing on three main dietary aspects:
Kidney Hydration: Encourage increased water intake. It helps flush out nephrotoxic substances and maintains kidney function.Detoxifying Herbs: Promote herbs like parsley and dandelion root that have a diuretic effect to help cleanse the kidneys.Nutrient-Rich Foods: Recommend foods like watermelon and kidney beans which are high in essential nutrients beneficial for the kidneys.Watermelon benefits include its high water content aiding in hydration and providing important vitamins. Kidney beans, apart from being heart-healthy, also support kidney function due to their fiber content and low sodium levels for people with kidney disease.
There are a few simple things that you should avoid like orange juice, white bread, and heavy convenience foods. Try to stick to a healthy meal as often as you can. Frozen meals and premade meals can get in the way of your health and contain excess phosphorus and excess amounts of sodium.
Controlling Renal Failure NutritionallyControlling nutritional intake can significantly impact kidney health, especially in those dealing with impaired functionality. Kidney-friendly recipes and vegan renal diets are essential tools for managing your condition. These diets limit proteins, phosphorus, and sodium while providing necessary nutrients.
Hydration importance cannot be overstated; adequate water intake helps kidneys clear sodium, urea, and toxins from the body.
Exercise plays a vital role too! It aids in maintaining healthy blood pressure levels which directly influences kidney health. However, you've to be aware of medication interactions, as certain drugs might affect nutrient absorption or cause damage when combined incorrectly.
Always consult your healthcare provider, before making dietary changes, or starting new medications to ensure safety. You're not just what you eat, but how you manage what you consume.
Crucial Dietary Restrictions for Kidney HealthWhen managing kidney health, it's crucial that you understand the significance of limiting your sodium and protein intake, as well as balancing potassium consumption.
Studies have found that excessive sodium can exacerbate hypertension and cause further damage to the kidneys, while overconsumption of protein may lead to a buildup of waste products in your bloodstream.
On the other hand, maintaining an appropriate balance of potassium is key for nerve function and muscle control, but too much can be harmful, if your kidneys aren't fully functional.
Pay attention to ingredient labels, ingredient list, diet plans, and talk to your health professional if you have any questions.
Limiting Sodium and ProteinYou'll need to be mindful of your sodium and protein intake to manage your renal failure effectively. Protein alternatives, like tofu or lentils, can provide essential nutrients without overloading your kidneys. Sodium substitutes are another vital component, opt for herbs and spices instead of salt to flavor foods.
Diet Optimization - A balanced diet is crucial for maintaining health, while managing kidney disease.Nutrient Absorption - Consuming the right nutrients in the correct amounts helps your body function optimally.Fluid Management - This doesn't just mean water, monitor intake of other fluids like coffee or juice too.Balancing Potassium IntakeIt's important to strike a balance with your potassium intake, as too much can be hard on the kidneys. A diet filled with kidney friendly fruits and low potassium snacks is crucial for maintaining health. Potassium rich recipes might be tempting, but they could pose a risk, especially when combined with potassium supplements.
Food TypeExamplesPotassium ContentFruitsApples, BerriesLowSnacksRice cakes, PopcornLowSupplementsRisks outweigh benefitsHighPotassium level monitoring becomes important for those in service to others who have renal diseases. Be cautious about supplements as the risk of consuming high potassium can lead to serious health issues. In essence, balance is key, not too much or too little will ensure optimal kidney function.
The Importance of Sodium Control in Renal DietsAs you get deeper into the complexities of renal diets, it's crucial to understand sodium's key role in this context. Sodium management is not just essential for maintaining overall health, but it's particularly vital when caring for your kidneys.
Drawing from evidence-based findings, we will discuss how sodium affects kidney function and provide detailed strategies for effective sodium control tailored to support kidney health.
Sodium's Role in Renal DietsSodium's crucial in a renal diet because it helps control your body's fluid balance. Understand the sodium sources and ensure hydration importance to maintain this balance.
Processed foods, a major source of dietary salt, should be avoided as they often contain high levels of sodium which can lead to health implications such as hypertension, heart disease, and kidney damage.
Consider these steps:
Incorporate fresh fruits and vegetables into your meals.Choose unprocessed lean proteins.Read food labels carefully for sodium content.Managing Sodium for KidneysYou've got to manage your sodium intake effectively to ensure good kidney health. Sodium intake awareness is critical, too much sodium can damage your kidneys over time.
Hydrating responsibly goes hand in hand with this, as water helps flush out excess sodium. Reading food labels becomes second nature when you're committed to maintaining kidney health; keep an eye out for hidden sodium sources.
Opt for kidney-friendly snacks like fresh fruits and vegetables instead of processed foods. Processed foods avoidance not only reduces your sodium consumption, but also other harmful substances such as preservatives and artificial flavors.
In short, managing your diet thoughtfully can make a significant difference in the longevity and functionality of your kidneys.
Advantages of Following a Renal Failure Meal PlanAs you dig deeper into the world of renal failure diets, it's crucial to understand the significant health benefits a well-structured meal plan can provide.
Not only does it promote better kidney health, but it also aids in maintaining overall wellness and mitigating disease progression.
A dietitian plays an indispensable role in this planning process, utilizing evidence-based findings to customize a nutritional plan that fits your specific needs and preferences. All this while ensuring your body receives all necessary nutrients for optimal function.
You may also know that individuals with kidney disease do refer to kidney failure as different names. Advanced kidney disease, following a kidney-friendly diet, chronic diseases, may be all things that people with kidney failure deal with.
Health Benefits of Meal PlansIncorporating this meal plan can significantly improve your health by reducing strain on your kidneys. It emphasizes the importance of hydration, meal timing, managing cravings, the role of fiber, and the usage of probiotics. Each of these factors plays a crucial role in ensuring you stay healthy while dealing with like as a person with kidney failure.
Hydration Importance: Adequate fluid intake keeps your kidneys functioning optimally.Meal Timing: Regular meals prevent sudden spikes or drops in blood sugar, helping to manage cravings.Role of Fiber and Probiotics Usage: Fiber aids digestion, and probiotics ensure a healthy gut environment.Dietitian's Role in PlanningWorking with a dietitian can help you tailor your meal plan to meet your specific needs and preferences. A dietitian's expertise lies in interpreting lab results, therapeutic communication, patient education, and individualized meal planning. They translate complex medical jargon into understandable information for you.
Dietitian's RoleImpactInterpret Lab ResultsUnderstand the implications of your health dataTherapeutic CommunicationEstablish trust and openness for effective treatmentIndividualized Meal PlanningTailor nutritional advice to personal circumstancesA dietitian guides you through understanding your renal failure dietary requirements. Their professional advice is based on evidence-based findings that are proven to work. As someone who desires serving others, their goal is not just about providing information but also ensuring understanding and application of this knowledge for better health outcomes.
Strategies for Reducing Sodium in Your DietYou've likely heard about the importance of monitoring sodium intake for overall health, but you may be unsure about how to go about it in your daily cooking.
This discussion will delve into evidence-based strategies that can help you control sodium levels in your meals, focusing on sodium-free seasoning alternatives that can enhance flavor without adding unnecessary salt.
We'll also explore practical techniques for managing sodium content during cooking, helping you to create healthier and more balanced dishes.
Sodium-Free Seasoning AlternativesIt's important to explore sodium-free seasoning alternatives when managing a renal failure diet. This not only helps protect your kidneys, but also enhances the flavor of your meals without the harmful effects of salt. Here are some options you can consider:
Herb Infusions: Fresh or dried herbs such as basil, rosemary, and thyme can infuse dishes with rich flavors.Spice Combinations: Try blends like turmeric and black pepper or cumin and coriander for an explosion of taste.Aromatics Usage: Ingredients like garlic, onions, and bell peppers add depth to any dish.Umami Enhancers: Mushrooms or nutritional yeast create savory notes.Vinegar Varieties: A splash of balsamic or apple cider vinegar can brighten flavors.Embrace these alternatives; they're not just healthier choices but also opportunities to elevate your culinary skills while serving others well.
Controlling Sodium in CookingBuilding on sodium-free seasoning alternatives, let's delve into the broader topic of controlling sodium in cooking.
You can make use of sodium detection techniques to monitor your food's salt content effectively. Understanding these methods will help you regulate your intake, which is crucial for kidney health.
Additionally, homemade sodium substitutes such as herbs and spices can be excellent options for flavor without adding any harmful amounts of salt.
While diuretics play a role in managing fluid balance, they're not a solution to a high-sodium diet.
Cooking without salt may seem challenging initially, but with practice and creativity, it becomes manageable and rewarding.
Also, consider low sodium beverage options to complement your meals - an integral part of maintaining a healthy renal diet.
The Role of Protein in a Renal Failure DietAs you navigate the complexities of a renal failure diet, understanding protein consumption guidelines is crucial. You'll learn that not all proteins are created equal - the source matters, often boiling down to a comparison between animal and plant proteins.
Drawing on evidence-based findings, this discussion will provide detailed insights into which types of protein may be most beneficial for your health and how to integrate them into your daily meals effectively.
Protein Consumption GuidelinesYou'll need to monitor your protein intake carefully when managing renal failure. This involves understanding Protein Sources, exploring Protein Alternatives, and practicing Protein Moderation. You should also be aware of any Protein Misconceptions and consider the use of Protein Supplementation if necessary.
Protein sources - Not all proteins are created equal. It's vital that you choose high-quality protein from lean meats, fish, and poultry.Protein alternatives - Don't forget about plant-based proteins! Foods like lentils, black beans, and quinoa can provide essential amino acids without overloading your kidneys.Protein moderation - Even too much of a good thing can be harmful in renal failure. Monitor your portions to avoid exacerbating kidney damage.Remember: managing renal failure isn't just about restrictionâit's about making informed choices for better health.
Animal Vs Plant ProteinIn the battle between animal and plant protein, it's essential to understand that they're not all created equal. When comparing protein sources, you should consider a variety of factors, such as nutrient density and potential health implications.
Plant-based benefits include lower risks of heart disease and obesity. Vegan diet implications may involve deficiencies in certain nutrients if not properly planned; yet, smart choices can offer a rich spectrum of nutrients beyond just protein.
Conversely, some animal proteins carry dangers like high saturated fat content which can lead to cardiovascular issues. Non-dairy alternatives are excellent sources of plant protein too â quinoa and lentils being prime examples.
It's critical for you to make informed decisions about protein intake considering your unique health needs.
Making Heart-Healthy Choices for Renal HealthAs you navigate the complexities of maintaining renal health, it's crucial to make heart-healthy choices that take into account your cooking methods and dietary intake.
Studies show that choosing cooking methods wisely, such as grilling or steaming instead of frying, can significantly reduce the risk of further kidney damage by limiting saturated fats intake.
It's not just about what you eat but also how you prepare your meals; this approach helps in managing your overall calorie consumption and contributes to improved cardiovascular health - a key aspect for individuals dealing with renal failure.
Choosing Cooking Methods WiselyChoosing cooking methods wisely can significantly impact the success of a renal failure diet. Steaming benefits include retention of nutrients and elimination of added fats - an ideal choice for kidney care.
Grilling imparts flavor without unhealthy additives, while slow cooking allows for tender meals without excess sodium or fats. Microwave usage can be a quick, healthy option when used to steam vegetables or reheat prepared dishes. Stir frying techniques provide quick, high heat cooking that seals in flavors and nutrients with minimal oil.
When preparing meals:
Consider the nutritional impact of your cooking method.Choose techniques that preserve natural flavors and nutrients.Avoid methods that require excessive salt or fat.Limiting Saturated Fats IntakeYou'll want to limit your intake of saturated fats, as they can negatively impact your overall health. Fats identification is crucial in making dietary decisions. Instead, choose healthy oils such as olive or avocado oil, known for their unsaturated fats sources and numerous health benefits.
Avocados are particularly beneficial due to their high monounsaturated fat content which can help lower bad cholesterol levels when used instead of saturated or trans fats.
Furthermore, you should try to incorporate more omega-3 fatty acids into your diet due to Omega 3 importance in supporting heart health and reducing inflammation.
Remember that while all fats are high in calories, not all are created equal â so make smart swaps where possible for the sake of those you serve and care for.
How to Manage Phosphorus Intake EffectivelyYou might be surprised to learn about the prevalent presence of phosphorus in many packaged foods you're consuming daily, and its potential impact on your renal health.
It's essential to understand not only where this hidden phosphorus comes from but also how you can manage it effectively.
This includes discussing the usage of phosphate binders, a treatment option that's proven to control the levels of phosphorus in your body.
Phosphorus in Packaged FoodsIt's important to watch out for hidden phosphorus in packaged foods when managing a renal failure diet. Packaged food labeling can be deceiving, so you must keep an eye on phosphorus-rich ingredients and hidden sources. Phosphorus absorption becomes a significant concern with renal failure, requiring careful dietary selection.
Here are three steps to guide you:
Always scrutinize the labels of packaged foods. Even seemingly non-phosphorus alternatives may contain hidden sources.Educate yourself about common phosphorus-rich ingredients present in many pre-packaged foods.Opt for fresh produce over processed items whenever possible, to control your phosphorus intake more effectively.Phosphate Binders UsagePhosphate binders can be a real lifesaver when used properly to control phosphorus levels. However, you must be aware of the potential side effects, such as constipation or nausea. The key is in the timing of binder administration - it's best taken with meals to maximize their effect.
Understanding phosphorus food labeling is vital too, as managing your intake can decrease the need for high doses of binders. There are different types of binder medications, including calcium-based and non-calcium-based ones. Choosing the right one depends on your specific needs.
The binder's role in dialysis is significant; it helps maintain appropriate serum phosphorus levels, reducing potential heart risks. Remember, phosphate binders aren't a standalone solution but part of a broader strategy to manage kidney health.
Tips for Balancing Potassium Intake in Renal DietsAs you continue on your journey to effectively manage your renal diet, it's critical for you to consider potassium management strategies.
It's well-documented that an overabundance of potassium can lead to serious health issues, especially for those with kidney conditions.
Therefore, understanding and avoiding high-potassium foods is not just a dietary convenienceâit's an essential part of maintaining your overall health. If you have any questions, you can speak to your renal dietitian.
What kind of cheese can be added to this diet with ease?Cottage cheeseFeta cheeseLight cream cheesePotassium Management StrategiesManaging potassium levels effectively is vital in renal failure diets. You need to be mindful of the foods you consume, especially with potassium-rich recipes. It's crucial to consider medication interactions and the role they can play in your diet. Herbal supplements may seem harmless, but they too can affect your potassium levels adversely.
Start by incorporating kidney-friendly fruits into your diet - these are low in potassium but high in essential nutrients.Pay attention to how exercise influences your body's ability to regulate potassium; staying active helps maintain balance.Educate yourself on potential medication interactions that could derail your carefully planned meals.Avoiding High-Potassium FoodsYou'll need to be careful about avoiding high-potassium foods in your daily meals, as they can disrupt the balance of nutrients in your body. For instance, potassium-rich fruits like bananas and avocados should be consumed sparingly. Even mineral water may pose dangers if it's naturally high in potassium.
Herbal supplements are not always benign either; some contain substantial amounts of this mineral, thereby posing risks for those needing a low-potassium diet.
Dairy products require consideration. While they provide essential calcium, their potassium content can be problematic. Figuring out a kidney-friendly eating plan is important.
FAQs for Renal Failure DietsWhat Are Some Common Symptoms of Renal Failure That Can Indicate a Need for Dietary Changes?You may need to adjust your diet if you're experiencing symptoms of kidney problems. These can include fatigue, changes in urine output, trouble sleeping, and a loss of appetite.
It's crucial to recognize these symptoms early for effective dietary adjustments. This involves nutrient monitoring, fluid regulation, and maintaining electrolyte balance.
Yes, adhering to dietary restrictions can significantly slow down disease progression. By focusing on kidney health and understanding the dietary impact, you're supporting your body's natural systems.
It's not just about what you eat, but also how these foods interact with your body. A well-managed diet acts as a support system for your kidneys, potentially delaying the need for more aggressive treatments.
Changing your diet can certainly impact your emotional and mental health. It's not unusual to experience dietary depression or mood swings when adjusting to new food restrictions.
However, with strong emotional coping strategies and mental resilience, you'll manage these changes more effectively. Stress management techniques can also aid in navigating this new lifestyle.
Yes, exercise can assist in managing renal failure. Exercise benefits include improved physical function and quality of life.
However, the impact on dialysis treatment must be considered. You should tailor training intensity to your individual capacity and take necessary precautions.
Consult with healthcare professionals for activity recommendations that suit your condition.
In conclusion, managing your renal health through diet is crucial. Restricting sodium, balancing protein, and controlling phosphorus and potassium intake can significantly improve kidney health.
Heart-healthy choices also play a key role. By following a structured renal failure meal plan, you'll not only enhance your kidney function but also boost overall wellness.
You can still enjoy things like BBQ sauce, marinara sauce, homemade soups, cola drinks, roast beef, and beet greens. You have to be able to homemade meals portion under control as well! A kidney support diet can help support end-stage kidney disease and help avoid kidney infections.
Remember, every step taken towards a healthier diet is a stride towards better renal health. Portion size and proper blood sugar levels are both vital parts of renal failure diets.
The post Renal Failure Diets appeared first on Renal Diet HQ.
Suggested Reading:
Diabetic Renal Diet Meal PlanFoods To Avoid With Kidney DiseaseCKD Diet GuidelinesAugust 21, 2023
Low Potassium Smoothies
You're on a mission to serve up health-conscious, delicious smoothies without the potassium overload. It's not as hard as you might think!
With careful fruit selection and some clever additions like protein powders or silken tofu, you can create low potassium smoothies that are both kidney-friendly and incredibly tasty.
Let's dive into the world of low potassium fruits, discover pre-made options, and explore strategies for controlling volume in your blends. Whatever you choose to consume, low potassium smoothies can help you have a balanced meal and enjoy your favorite flavors.Â
[feast_advanced_jump_to]Key Takeaways[image error]Low potassium smoothies can be a beneficial addition to a low potassium diet for individuals with kidney disorders, as they can help maintain fluid balance and manage blood pressure.When making low potassium smoothies, it is important to carefully select ingredients, opting for low potassium fruits and vegetables, and choosing liquids that are low in potassium.It is crucial to be aware of the risks and precautions associated with high potassium fruits, as well as the symptoms and complications of potassium overdose. Consulting with healthcare professionals about dietary choices is recommended.Low potassium smoothies can provide a balanced combination of essential nutrients, hydration, and aid in detoxification and digestion, contributing to overall health and well-being.Understanding the Importance of Low Potassium DietFor More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
You've probably heard about the importance of potassium for your overall health. But did you know it plays a crucial role in kidney function? It's true. This essential mineral helps your kidneys filter out waste from the blood, maintain fluid balance, and manage blood pressure.
However, managing your dietary intake of potassium is key. Too much or too little can lead to serious health problems.
Potassium's Role in KidneysDon't underestimate the importance of potassium for your kidneys. It's vital in maintaining fluid and electrolyte balance.
Potassium regulation: Your kidneys control the amount of potassium in your body. Too much or too little can cause problems.Renal disorders: Diseases like chronic kidney disease disrupt this regulation, often leading to high levels of potassium.Dietary modifications: To combat this, people with renal disorders are recommended to follow a low-potassium diet.Managing Dietary Potassium IntakeIt's crucial for you to understand how to manage dietary intake of specific minerals, especially if you're caring for someone with kidney disorders. Potassium regulation plays a vital role in maintaining a healthy sodium potassium balance and preserving kidney function. Dietary planning is key here - too much potassium can cause problems, but so can too little.
You should consider incorporating low-potassium foods into meals, while avoiding high-potassium ones. Don't forget to monitor the person's overall diet and take note of any changes in their condition.
If needed, consult a doctor about potassium supplements; they can provide an extra boost without overloading the kidneys. Always remember that your goal is not just managing symptoms, but also promoting long-term health through careful dietary choices.
The Role of Smoothies in a Kidney-Friendly Diet
You're about to delve into the nutritional impact of smoothies and how strategic ingredient selection can enhance your health.
It's not just about blending fruits and veggies; there's a science behind it that you'll find intriguing. Understanding this will help optimize your daily intake, making every sip count towards a kidney-friendly diet.
Smoothies' Nutritional ImpactUnderstanding the nutritional impact of your smoothies, particularly their potassium content, can significantly improve your dietary choices. Smoothies offer a wealth of nutrients that promote health and wellness. They provide:
Nutritional balance: Ensuring you're getting an array of essential nutrients.Vitamins: Vital for overall health.Minerals: Like magnesium and calcium for bone health.Smoothie detoxification: Helps rid your body of toxins.Dietary fiber content: Aids in digestion and removal of waste.Smoothie hydration properties: Keeping you hydrated throughout the day.Water content: Mostly from fruits or vegetables used.Antioxidant benefits: Protects cells from damage.From fruits like berries and pomegranates.Smoothie Ingredient SelectionChoosing the right ingredients for your smoothie can greatly affect its nutritional value and taste. Prioritize ingredient freshness, fresh fruits and vegetables not only enhance flavor but also increase your detox smoothies' efficacy. Opt for low-potassium options, if you're managing potassium levels.
Consider liquid selection carefully too, unsweetened almond milk or coconut water can add hydration without excess sugars. Even your blending techniques matter - blend longer for smoother textures, less time if you prefer some chunkiness.
Ultimately, crafting a delicious, health-conscious smoothie is about balance - balancing flavors, nutrients, and even textures. You're not just making a drink, you're serving health in a glass! So, experiment with different combinations, until you find what serves your body best.
What's my sweetener options, just make sure you're choosing in the best interest of your blood sugar levels?
Alternative sweetenerVegan sweetenerTablespoon honey Agave nectarJust make sure you watch any excess sodium intake, caffeine intake, and excess sugar intake. You can also add your favorite peanut butter or nut butter.
Selecting Low Potassium Fruits for SmoothiesWhen managing kidney health, it's important to make smart choices about the fruits you consume. You need to consider not only their general nutritional value but also their potassium content.
Choosing Kidney-Friendly FruitsYou'll want to opt for fruits like apples, berries, and grapes that are low in potassium for your smoothies. These kidney-friendly vegetables make great additions, too.
However, fruit acidity and ripeness impact the overall nutritional value of these smoothie ingredients.
Fruit Acidity: Citrus fruit selection is crucial as their acidity can affect your kidneys. Choose lemons or limes over oranges.Ripeness Impact: Ripe fruits have more sugar but less potassium than their unripe counterparts.Tropical Fruit Considerations: Although appealing, most tropical fruits rank high in potassiumâstick with pineapples or guavas.Potassium Content in FruitsIt's crucial to understand that bananas, apricots, and oranges are examples of fruits with high potassium content. These tropical potassium powerhouses can be a boon or a bane depending on the health needs of those you're serving. For instance, if you're dealing with renal issues, unripe bananas can offer lower potassium levels.
Seasonal variety is another factor to consider; local seasonal fruits often have differing nutrient profiles. Dried fruits typically pack more potassium per serving due to their concentrated nature. So, moderation is key here!
Also, note that certain cooking techniques could reduce the potassium content in these fruits. By understanding these aspects, you can make informed decisions in preparing nourishing meals or concoctions for those under your care.
Eating a frozen banana, orange juice, and frozen blueberries are all common ingredients in a delicious breakfast of the classic smoothie.
Fruits to Avoid for Low Potassium SmoothiesYou might be surprised to learn that not all fruits are created equal when it comes to their potassium content. In fact, there's a potential risk involved with consuming too many high-potassium fruits, particularly for those with certain health conditions.
Let's dive into how you can identify these potentially dangerous fruits and the risks they pose for your health and your daily diet.
High Potassium Fruit RisksWhile there's no denying the health benefits of high potassium fruits, they can pose risks if you're dealing with certain health conditions. Your body needs a balance; too much potassium can lead to Hyperkalemia, and issues in Potassium absorption regulation can cause other complications.
Consider these important points:
Potassium Overdose Symptoms: These include palpitations, muscle weakness, breathing difficulties.Educate yourself and others on how to recognize these signs early.Hyperkalemia Prevention: Limit high-potassium foods and be wary of dietary supplements as they could have hidden dangers.Encourage those at risk to discuss their diet with healthcare professionals.High Potassium Complications: These range from irregular heart rhythms to kidney failure.It's crucial to raise awareness on the importance of maintaining balanced potassium levels.Stay mindful of your intake for healthy living.
Identifying Dangerous FruitsLet's now delve into identifying fruits that might pose a risk due to their high potassium content. You're likely aware of the dangers of fruit toxicity, especially when certain harmful fruit combinations are consumed in large amounts. Although they are creative blends, frozen fruit, or fruity blends, it's important to know what you're putting in your fruit smoothie!
For instance, bananas and oranges, though healthy, can cause harm if over consumed due to their high potassium content.
Moreover, you must be mindful of dangerous antioxidants that could affect your health. Some fruits may contain pesticides which present additional risks if not properly washed off before consumption.
Besides these factors, overconsumption effects can also come into play with any fruit; moderation is key.
In serving others with dietary restrictions or health concerns, it's vital to understand the potential hazards associated with certain fruits, so you can provide safe and nutritious options for all. Stay informed and take care! One of the best things about fruit per portion is the fiber from fruit!
Exploring Smoothie RecipesExploring different smoothie recipes can be a fun and tasty way to include more fruits and veggies in your diet and help you get more servings per recipe. Consider green smoothies for their detoxification benefits, packed with leafy greens like spinach or kale. They're not only vibrant but also rich in nutrients.
Superfood inclusion is key to boosting the nutritional value of your smoothies. Adding ingredients like chia seeds, flaxseeds, or goji berries can offer a significant health boost. If you're sensitive to dairy or just looking for something different, there's an array of dairy alternatives such as almond milk, coconut water, or soy milk that you can use.
A delicious smoothie recipe consistency matters too, whether you prefer it thick like a shake or light and refreshing is totally up to you. Enjoy discovering new combinations, even if you just enjoy a regular smoothie recipe, these are worth trying!
Orange Banana SmoothiePina Colada SmoothieApple Juice SmoothieBlueberry SmoothieHealthy Apple SmoothieProtein SmoothiesApple Cinnamon Smoothie RecipeStrawberry SmoothieFeel free to explore sodium smoothie recipes and any vegan smoothie recipe you like! Incorporating Lower Potassium Fruits in SmoothiesYou're keen on maintaining a healthy lifestyle, and part of that involves keeping your potassium levels in check. Choosing low potassium fruits for your smoothies is an excellent way to do this.
In the following discussion, there are specific fruits to pick and how you can adjust your smoothie recipes to keep them delicious while reducing their potassium content.
Choosing Low Potassium FruitsWhen picking out fruits for your smoothie, it's important to choose those with low potassium content. This is particularly crucial if you're concerned about potassium and hypertension. Too many potassium-rich foods can be dangerous!
Consider diuretic foods such as cucumbers or watermelon. They not only add flavor but also help flush excess potassium from the body.
Instead of using high-potassium fruit juices, opt for alternatives like almond milk or coconut water. This is an amazing smoothie alternative.
Be mindful of adding potassium rich vegetables like spinach; instead use lettuce or kale. In no time, you'll have a smoothie regimen that you enjoy. If you need a vegetarian smoothie recipe or a smoothie without milk products than this is for you!
Remember that potassium balancing supplements can be a useful addition too. Always ensure what you put in your smoothie aligns with the dietary needs of those you're serving.
It's all about creating a health-conscious blend that suits everyone's nutritional requirements! Without a doubt, a happy smoothie can help you enjoy the effects of drinking smoothies and even more so, enjoying kidney-friendly smoothies.
Smoothie Recipes AdjustmentsIt's vital to know how to adjust your smoothie recipes based on dietary needs and personal preferences. You can modify the smoothie consistency by adding more liquid or fruit. Consider ingredient alternatives like low-potassium fruits, non-dairy milk, or natural sweeteners if you have dietary restrictions.
Allergen considerations are also important. If a recipe calls for an allergenic food, substitute it with something you're not allergic to without compromising taste or nutritional value.
Remember, fresh smoothies are best consumed immediately after preparation. If you must store it, refrigerate it in a sealed container and consume within 24 hours to retain maximum nutrients.
Satisfying everyone's tastes and health requirements takes planning and flexibility but it's achievable with these tips.
Benefits of smoothies:
Flavorful drinks with various flavor profiles. Delicious drinks for your current diet, even a diet for dialysis patients. Can be a complete meal replacement Mega flavor, extra flavor, flavor pairings, flavor of choice. You can avoid a gritty artificial-tasting drink by following these diet tips and tricks for smoothies.Choosing the Right Protein Powders for Your Smoothies, Guide to SmoothiesYou're well on your way to mastering the art of smoothie making, but have you considered the impact your protein choices may have on your kidney health?
It's not just about selecting a protein powder or alternative that tastes good; it's also about being mindful of their kidney-friendly properties.
You can make informed decisions when choosing between protein powders and their alternatives for your smoothies. Whey protein powder can be a positive thing when you're on a CKD diet.
Selecting Kidney-Friendly ProteinsChoosing kidney-friendly proteins for your low-potassium smoothies isn't as hard as it may seem. By focusing on plant-based proteins, not only are you promoting protein absorption, but you are also enhancing kidney health. Here's a list to help guide your selection:
Pea Protein: It's easy to digest and helps with kidney detoxification. Ideal in green smoothies.Hemp Protein: A complete protein that supports kidney function. Perfect for fruit-based blends.Rice Protein: Gentle on the digestive system, aiding in protein digestion. Great for any type of smoothie.Protein Powder Vs. AlternativesNow that you're equipped with knowledge on selecting kidney-friendly proteins, let's shift our focus to protein powders and their alternatives.
Protein sources are abundant, but it's essential to consider factors like protein absorption and digestibility. Traditionally, many have turned to whey protein for its efficiency in these areas. However, if you're seeking whey alternatives due to dietary restrictions or personal preferences, there are several options available.
Vegan proteins derived from peas, hemp, rice and other plant-based sources can be as effective while offering additional fiber benefits. These vegan options often provide a complete amino acid profile necessary for optimal health and muscle recovery.
Remember though, each individual absorbs protein differently based on various factors including age, metabolism rate and gut health. So, make sure you choose what best suits your unique needs!
The Benefits of Adding Silken Tofu to Your SmoothiesYou've heard about the benefits of protein in your diet, but have you considered boosting your intake with tofu? Specifically, silken tofu can be a great addition to your smoothies, offering a healthful way to ramp up protein levels.
Let's dive into the unique blending techniques that make it easy and tasty to incorporate this nutrient-packed ingredient into your daily routine.
Protein Boost With TofuAdding tofu to your smoothie isn't just a great way to boost its protein content, it also helps keep your potassium levels low. Tofu provides numerous health benefits, while serving as an excellent source of vegan protein. However, be mindful if you have soy allergies, always opt for allergy-friendly alternatives such as cup tofu.
The varieties of tofu available are plenty:
Silken tofu: Ideal for blending into smoothies.Sub-list 1: It's soft and creamy.Sub-list 2: Lower in fat and calories than other types.Firm or extra-firm tofu: Excellent for cooking with.Sub-list 1: Holds up well in stir-fries and grills.Sub-list 2: Higher in protein but also higher in fat.Silken Tofu Blending TechniquesBlending silken tofu into your meals couldn't be easier, and it's a versatile ingredient that works well in a variety of recipes. Among the multiple tofu varieties, silken tofu is soft and creamy, making it perfect for blending into smoothies or sauces.
Rich in vegan protein and low in fat, tofu nutrition benefits are vast. However, be mindful if serving someone with soy allergies as tofu is a soy-based product. Always check dietary restrictions before introducing new foods.
Proper tofu storage extends its shelf life. Keep unopened packages in the fridge. After opening, submerge any leftover piece in water inside an airtight container; change the water daily to maintain freshness.
Strategies for Controlling Volume and Fluid Intake in SmoothiesYou've mastered the art of creating delicious and healthy smoothies, but now it's time to tackle portion control strategies.
It's important to remember that even good things should be consumed in moderation for optimal health benefits.
Did you know you can also freeze your smoothies for later? This not only helps with portion control but also ensures that you have a ready-to-go, nutritious treat whenever you need it.
Portion Control StrategiesIt's important to measure your ingredients accurately, when making low potassium smoothies to ensure portion control. Here are some strategies that can help you:
Meal Planning: Plan your meals in advance, incorporating a variety of fresh whole foods. This not only helps manage your diet, but also ensures you're getting all the nutrients you need.Mindful Eating: Be aware of what you're eating and how much. Savor each bite and pay attention to your hunger cues.Visual Cues: Use visual cues like smaller plates or bowls for portion control.Regular Exercise: Incorporating regular physical activity into your routine boosts metabolism, helping maintain healthy weight levels.These strategies keep you conscious about the portions you consume while promoting holistic health through regular exercise and mindful eating. Remember, it's not just about quantity, but quality too!
Freezing Smoothies for LaterStoring your freshly made smoothies in the freezer for later is an excellent way to ensure you've got a healthy snack on hand anytime. Smoothie preservation isn't complicated, but it requires some knowledge about optimal freezing temperature and defrosting methods.
You're aiming for 0°F (-18°C) as your freezer's setting; this halts bacterial growth and maintains the smoothie's nutritional value.
When it comes to containers, opt for glass or BPA-free plastic smoothie storage containers that are airtight to prevent oxidation. You might also consider ice cube trays usage; they allow you to portion out your smoothie effectively.
To defrost, leave them in the fridge overnight or immerse sealed containers in warm water for quicker results.
Enjoying nutrient-rich low potassium smoothies has never been more convenient!
FAQs for Enjoying Low Potassium SmoothiesCan I Still Enjoy a Variety of Flavors While Maintaining a Low Potassium Smoothie Diet?Absolutely! You can enjoy a variety of flavors in your smoothies. Your fruit selection plays a key role. Choose fruits lower in potassium like apples and berries.
The consistency of your smoothie can be managed by adding low-potassium liquids or ice. Include supplements that fit into your dietary needs. There are also yogurt alternatives that you can use for your smoothie.Â
You can also switch up the yogurt options. Green yogurt, vegan yogurt, almond yogurt, Greek yogurt, coconut yogurt and whatever else type of yogurt that you wish to enjoy
You're looking for natural ways to sweeten your smoothies. Great choice! Just as a smoothie is a healthy breakfast choice, it's alsoÂ
Stevia benefits include zero calories and no potassium, making it an excellent option.
Honey alternatives like agave syrup can also provide a delicious sweetness without the extra potassium.
Don't forget about cinnamon uses, it's not just a spice, but a natural sweetener too.
Mixing these into your drinks can create yummy, health-conscious concoctions that taste as good as they make you feel! You can also add a little unsweetened rice milk if that makes sense for your situation, you'll notice it adds a creamy texture to your smoothie.Â
You can include low potassium smoothies in your meal plan with a few tweaks. Consider meal prep ideas like prepping ingredients ahead of time.
Use smoothie ingredient swaps, such as low potassium fruits, to maintain flavor while controlling intake. These additions to smoothies are smart. You can learn to make extra smoothies and even more flavorful smoothies than to low potassium options.
Portion control tips also help manage the amount you consume daily, plus you get a fuller flavor!Â
The nutritional benefits of these smoothies contribute to overall health, making this an attractive option for anyone wanting to serve nutritious meals to loved ones.
Absolutely, you can use dairy milk alternatives in your smoothies! If you are not doing a juice diet plan, that's okay because you can still enjoy low potassium smoothies on a sodium kidney diet.Â
Almond milk benefits from being low in potassium and high in calcium. However, soy milk's drawbacks include a higher potassium content.
Oat milk provides good nutrition with fiber and protein. Rice milk is suitable for those allergic to nuts or soy, while coconut milk is rich but higher in fat.
Remember to read labels as additives can vary the nutritional profiles of these milks. Getting your daily vitamin in through a balanced smoothie is a good idea. A cup smoothie has so much nutrition in it, that is may even become a sort of vegetable choice over other options.Â
You can pair this smoothie with pasteurized egg whites and see major success! Delicious flavor combinations are available by enjoying a healthy kidney-friendly smoothie.Â
So, now you've got the scoop on low potassium smoothies. Remember, careful selection of fruits and protein powders is key in maintaining a kidney-friendly diet. Even if you're not a breakfast eater or are looking for breakfast for dialysis patients.
Not to mention, you're going to start feeling that fullness with meals, which is always welcome when enjoying a friendly drink for people with kidney disease.Â
Always keep an eye out for pre-made options that fit your needs. And don't forget silken tofu, it's a great addition to any smoothie!
Stay mindful of volume and fluid intake too. Think about what are some of your favorite smoothie additions. Pay attention to exercise levels, hydration levels, cholesterol levels, and so much more when you're enjoying these smoothies.
You're going to get essential vitamins and a boost of vitamins from these balanced nutrition smoothies. Here's to your health!
The post Low Potassium Smoothies appeared first on Renal Diet HQ.
Suggested Reading:
Low Potassium Side DishesDiabetic Renal Diet Meal PlanAre Berries High In Potassium?August 20, 2023
Managing Renal Diet Limits
Like most things in life, living with renal diet limitations is largely what you make it out to be. Some people consider this diet highly restrictive. However, if you take a few moments to explore your options, you just might discover that there are many food options still available to you.
More than you may have realized at first glance. Don't give up on eating for pleasure. It's still very much possible despite perceived renal diet limitations. These tips will help you make the most of the renal diet limitations you are faced with, so that you can enjoy food as part of your daily routine.
[feast_advanced_jump_to] 79Key TakeawaysEstablishing a routine is vital for managing food restrictions, medication, and water intake in a renal diet.Use fresh ingredients to add flavor and nutrition while avoiding grazing and drinking during meal prep.Maintain a positive mindset by focusing on exploring new food options and recipes rather than dwelling on limitations.Consistency is key in sticking to a renal diet, helping you gradually adjust to healthier eating habits.Look for renal diet-friendly versions of your favorite foods to continue enjoying your meals within the limitations of the diet.
79Key TakeawaysEstablishing a routine is vital for managing food restrictions, medication, and water intake in a renal diet.Use fresh ingredients to add flavor and nutrition while avoiding grazing and drinking during meal prep.Maintain a positive mindset by focusing on exploring new food options and recipes rather than dwelling on limitations.Consistency is key in sticking to a renal diet, helping you gradually adjust to healthier eating habits.Look for renal diet-friendly versions of your favorite foods to continue enjoying your meals within the limitations of the diet.Renal Diet BasicsFor More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
Understanding the fundamentals of a renal diet is foundational in managing Chronic Kidney Disease. Here, we provide a comprehensive overview of CKD, shedding light on why a renal diet is essential in the context of this disease.
We'll delve into the intricacies of this specialized diet, exploring its critical role in mitigating complications and preserving kidney function. From dietary restrictions to nutrient optimization, these insights will empower you to make informed choices for a healthier life while living with CKD.
Chronic Kidney Disease OverviewChronic Kidney Disease is a progressive medical condition characterized by the gradual deterioration of kidney function over time. It is typically a silent disease, with symptoms often not manifesting until the disease has advanced significantly. CKD can result from various underlying factors, including high blood pressure, diabetes, autoimmune diseases, and genetic predisposition.
The kidneys' primary role is to filter waste and excess fluids from the blood, regulate blood pressure, and maintain electrolyte balance. As CKD progresses, these functions become compromised, leading to a buildup of toxins in the body and imbalances in essential bodily functions.
Effective management of CKD involves early detection, lifestyle modifications, medication, and, in severe cases, dialysis or kidney transplantation. Regular monitoring and adherence to a renal diet are crucial for preserving kidney function and overall well-being.
Why Is Renal Diet Necessary?A renal diet is essential for individuals with Chronic Kidney Disease because it plays a crucial role in slowing disease progression, managing symptoms, and preventing complications. CKD impairs the kidneys' ability to filter waste and regulate fluid and electrolyte balance effectively.
Without dietary adjustments, waste products can accumulate in the blood, causing complications like high blood pressure, fluid retention, and electrolyte imbalances. A renal diet helps control these issues by limiting the intake of specific nutrients such as sodium, potassium, and phosphorus. Additionally, it manages protein intake to reduce the burden on the kidneys.
Properly managed, a renal diet can help delay the need for dialysis or kidney transplantation due to kidney failure, improve overall health, and enhance the quality of life for individuals living with CKD.
Understanding Sodium Restrictions in Renal DietSodium or salt is linked to kidney disease and hypertension. This could also lead to fluid retention in the body, thus causing your blood pressure to shoot up and your extremities to swell.
In your CKD diet, you need to limit your sodium intake to 1500 milligrams per day. Avoid using extra salt in your renal diet, and also avoid processed foods because they are very high in sodium.
Sodium in Packaged FoodsPackaged and processed foods are notorious for their high sodium content, posing a significant challenge for individuals on a renal diet that requires strict sodium limitation, such as those with Chronic Kidney Disease.
It's crucial to shop smartly by carefully examining food labels. Avoid or minimize foods like canned soups, instant noodles, processed meats (e.g., bacon, ham, sausages), frozen meals, canned vegetables, and salty snacks (chips, pretzels).
Sauces and condiments like soy sauce, ketchup, and salad dressings can also be sodium culprits. Carbonated drinks, including colas, are sodium-laden and should be avoided.
Instead, prioritize fresh fruits and vegetables, lean meats, poultry, and fish, and choose sodium-free or low-sodium versions of canned goods. Cooking from scratch with herbs, spices, and sodium-free seasonings allows for greater control over sodium intake. Gradually reducing salt while gradually acclimating taste buds to lower sodium levels is essential for effective sodium management on a renal diet.
Reducing Sodium in CookingReducing sodium in cooking is essential for individuals on a renal diet, particularly for those managing conditions like Chronic Kidney Disease. Here are strategies to cut down on sodium while maintaining flavor:
Use Fresh Ingredients: Start with fresh fruits and vegetables, lean meats, poultry, and fish, which naturally contain lower levels of sodium compared to processed counterparts.Limit Salt: Gradually reduce the amount of salt used in recipes. Over time, your taste buds will adjust to lower sodium levels.Rinse Canned Foods: Rinse canned vegetables, beans, and other high-sodium foods under running water to remove excess salt.Choose Sodium-Free Seasonings: Opt for herbs, spices, garlic, ginger, lemon, and vinegar to enhance flavor without sodium. Experiment with various combinations for creative, tasty dishes.Homemade Broths and Sauces: Prepare homemade broths, stocks, and sauces to control sodium content. Use unsalted or low-sodium varieties.Read Labels: When using packaged ingredients, select low-sodium or sodium-free versions and carefully read food labels to identify sodium content.Avoid High-Sodium Condiments: Be cautious with condiments like soy sauce, ketchup, and salad dressings, as they can contribute significant sodium. Choose low-sodium alternatives or make your own.By adopting these practices, individuals on a renal diet can enjoy flavorful meals while effectively reducing sodium intake, promoting kidney health, and preventing complications associated with excess sodium consumption.
Adjusting Protein Consumption for Kidney HealthThe body needs protein in order to build muscles, repair tissues, and fight infections. However, when the body breaks down protein, it also releases urea, a waste product that usually goes out in the urine. Since your kidneys are no longer functioning well, there is a danger that urea might not be properly excreted by the body.
Therefore, a CKD diet will help prevent urea overload in the kidneys. You need to limit your protein intake by cutting down high protein foods such as fish, meat, poultry, dairy, and eggs. Your nutritionist will tell you how much protein your condition warrants in your CKD diet.
Balancing Animal and Plant-ProteinsBalancing animal and plant proteins is crucial when managing protein intake for non-dialysis Chronic Kidney Disease patients. Animal proteins provide complete amino acids but are often higher in phosphorus and potassium, necessitating moderation.
Choose lean cuts of meat, skinless poultry, and fatty fish for high-quality animal protein sources. Dairy products should be low-fat or fat-free to limit saturated fat and phosphorus.
Plant proteins, like beans, lentils, and tofu, are lower in phosphorus and potassium but may lack some essential amino acids. Combining different plant protein sources can help fill these gaps. Focus on variety to maximize nutrient intake.
Also, monitor portion sizes to avoid overconsuming phosphorus and potassium. Balancing animal and plant proteins allows people with kidney disease to maintain protein intake while effectively managing potential complications associated with renal disease.
Protein Portion Size ImportanceIt's not just what type of protein you eat, but how much you consume that plays a crucial role in maintaining your health. Consuming protein-rich foods in moderation is key, especially if you're on dialysis. Too much can be burdensome on your kidneys.
Your aim should be diet sustainability, incorporating enough proteins without causing harm. It's important to understand portion sizes and the impact they have on your overall health. Nutritional counseling can provide guidance appropriate for your specific needs.
Considerations for those undergoing dialysis are more complex due to their differing needs since the dialysis process may cause protein losses. Achieving balance may seem challenging at first glance, but with proper knowledge and consultation, it becomes attainable.
Managing Phosphorus Intake in Renal DietsPhosphorus can build up in your blood, and your kidneys might not be able to get rid of it. This may cause your bones to lose calcium and weaken. Foods that are high in phosphorus content and should be limited in your CKD diet include dairy products, nuts, whole grains, beer, cocoa, and cola drinks.
Avoiding Phosphorus-Added Packaged FoodsAvoiding phosphorus additives in packaged foods is essential for individuals with Chronic Kidney Disease to manage their phosphorus intake effectively. Many processed and packaged foods contain phosphorus additives, often listed on ingredient labels as "phos" or "phosphate." These additives are used for various purposes, including as preservatives, stabilizers, and leavening agents.
To reduce phosphorus intake:
Read Labels: Carefully inspect ingredient labels when shopping. Look out for phosphorus-containing additives like sodium phosphate, calcium phosphate, and phosphoric acid.Choose Fresh Foods: Opt for fresh, whole foods whenever possible, as they are naturally lower in phosphorus. Fruits, vegetables, and lean meats are excellent choices.Limit Processed Foods: Minimize the consumption of processed and convenience foods, which are more likely to contain phosphorus additives.Cook from Scratch: Preparing meals from scratch allows you to have better control over ingredients and reduce phosphorus additives' presence in your diet.By being vigilant about phosphorus additives, CKD patients can better manage their phosphorus levels and reduce the risk of complications associated with excessive phosphorus intake.
Choosing Low-Phosphorus FoodsSelecting low-phosphorus foods is crucial for individuals with Chronic Kidney Disease to manage phosphorus levels and minimize strain on their kidneys. Some examples of low-phosphorus foods include:
Fresh Fruits: Most fresh fruits like apples, berries, and grapes are naturally low in phosphorus.Vegetables: Opt for vegetables such as broccoli, cauliflower, kale, and cabbage, which have lower phosphorus content.Lean Proteins: Choose lean cuts of chicken, turkey, and fish like salmon or trout. Egg whites are another phosphorus-free protein option.Bread and Grains: Look for low-phosphorus bread and grains like white rice, white bread, and pasta.Dairy Alternatives: Consider phosphorus-free dairy alternatives like almond milk or rice milk.Cooked Rice and Pasta: Cooking rice and pasta can reduce their phosphorus content, making them better choices for CKD patients.Herbs and Spices: Use herbs, spices, and low-sodium seasonings to flavor dishes instead of high-phosphorus condiments.By incorporating these low-phosphorus foods into their diet, individuals with CKD can better manage their condition and minimize the risk of complications associated with elevated phosphorus levels.
Regulating Potassium Levels in Renal DietWithout a healthy kidney, potassium can build up in your body, causing irregular heartbeats or arrhythmias. Foods that are high in potassium and should be limited in a CKD diet include fruits and vegetables like potatoes, tomatoes, beans, bananas, pumpkins, spinach, mushrooms, and dried peas.
Potassium Rich Foods To AvoidFor individuals on a kidney-friendly diet, it's crucial to be aware of potassium-rich foods that should be limited or avoided, particularly when dealing with Chronic Kidney Disease. High levels of potassium can pose risks, including heart arrhythmias. Foods to restrict include:
Bananas: Renowned for their potassium content, bananas should be consumed in moderation.Oranges and Orange Juice: These are high in potassium and should be limited.Potatoes: Baked potatoes, potato chips, and French fries are rich in potassium and best avoided.Tomatoes and Tomato-Based Products: Tomato sauce, ketchup, and even certain soups contain significant amounts of potassium.Spinach and Leafy Greens: While nutritious, these are high-potassium foods and should be consumed in small portions.Dried Fruits: Raisins, prunes, and dried apricots have concentrated potassium levels and should be restricted.Nuts and Seeds: Almonds, peanuts, and sunflower seeds are potassium-rich snacks to limit.By avoiding or limiting these high-potassium foods and carefully monitoring their intake, individuals with CKD can better manage potassium levels and reduce the risk of complications.
Draining Canned Fruits, VegetablesDraining canned fruits and vegetables is a simple yet effective strategy for reducing potassium intake, especially for individuals on a renal diet. Canned foods often contain excess potassium due to the liquid they are packed in. By thoroughly rinsing and draining these foods under running water, a significant portion of the potassium is removed, making them more kidney-friendly.
For example, canned beans, a common source of plant-based protein, can have high potassium levels. Rinsing and draining them can help lower their potassium content. Similarly, canned fruits like peaches or pears in syrup can be high in potassium, but draining them reduces the potassium load.
This practice allows individuals with Chronic Kidney Disease to enjoy a more varied diet while better controlling their potassium intake, promoting kidney health and preventing complications associated with elevated potassium levels.
Incorporating Heart-Healthy Foods for Renal DietIncorporating heart-healthy foods into a renal diet is not just a matter of culinary choice; it's a necessity, particularly for individuals dealing with Chronic Kidney Disease. Cardiovascular complications, including heart disease, are the leading cause of mortality among CKD patients. Thus, embracing a diet that supports both kidney and heart health is paramount.
This section explores the vital intersection of renal and heart health, offering insights into how CKD patients can make dietary choices that nurture their kidneys while safeguarding their cardiovascular well-being.
Heart Healthy Foods To IncludeIn a renal diet, it's crucial to incorporate heart-healthy foods, given that cardiovascular complications are a leading cause of mortality in Chronic Kidney Disease patients. Balancing both renal and heart health requires careful dietary choices.
First, fatty fish like salmon, mackerel, and trout are excellent options as they are rich in omega-3 fatty acids that support heart health without overloading on phosphorus, making them a valuable protein source. Berries, such as blueberries, strawberries, and raspberries, are low in potassium and high in antioxidants, offering protection against heart disease.
Olive oil, with its monounsaturated fats, can replace saturated fats in cooking, promoting heart health. Whole grains like brown rice, quinoa, and whole wheat bread provide essential nutrients and fiber, supporting cardiovascular well-being while being mindful of potassium levels. Lean proteins like skinless poultry, lean cuts of meat, and egg whites are low in saturated fat and phosphorus, making them heart-healthy protein options.
Red bell peppers are low in potassium but rich in vitamins, contributing to heart protection. Finally, garlic, renowned for its cardiovascular benefits, can be used to flavor dishes.
Incorporating these heart-healthy foods into a renal diet can help CKD patients strike a balance between maintaining kidney function and reducing the risk of heart-related complications, promoting overall well-being.
Choosing Low-Fat ProteinsChoosing low-fat proteins isn't just beneficial for weight management, but it's also gentler on your kidneys and blood vessels compared to high-fat alternatives. When you switch to protein alternatives like vegan proteins or lean seafood selection, you're doing your body a great service. Check out this table with some healthy protein options:
Protein SourceProtein (g) per 100gFat (g) per 100gSkinless Chicken Breast313.6Tofu84.8Salmon Fillet2013Lentils (cooked)90.4Developing a Routine for Effective Dietary ManagementMost people discover that even more than the renal diet limitations on food, the need for medications coupled with the restrictions on water require a little proper planning. Once you develop a routine, it all comes together like clockwork. Getting there, though, takes a little time and a lot of planning on your part.
It takes a while to create new habits and live within your renal diet limitations. At first, you may need to set a few alarms to keep it all straight.
Pillboxes, notes on refrigerators, and charts are great tools for keeping it all together too. Food prep, however, is one of the fundamental changes you're going to have to make in your life.
Planning for Dietary RestrictionsIncorporating dietary restrictions into one's daily routine is a crucial aspect of managing chronic conditions like Chronic Kidney Disease. The key to success lies in careful planning and gradual adjustments.
Start by educating yourself about the specific dietary restrictions and recommendations provided by your healthcare provider or dietitian. Then, create a meal plan that aligns with these guidelines, emphasizing foods that support your health goals while avoiding those that could exacerbate your condition.
Consistency is paramount; therefore, establish a routine for meal preparation, consumption, and medication management. Use tools like pillboxes, calendars, and grocery lists to stay organized. Make adjustments slowly, allowing your taste buds to adapt to new flavors and textures over time.
Enlist the support of your family and friends to create an encouraging environment. By making dietary restrictions a routine part of your life, you can effectively manage your condition, enhance your overall well-being, and reduce the risk of complications.
Maintaining Consistent Healthy HabitsMaintaining consistent healthy habits, including regular exercise and adequate sleep, plays a significant role in managing Chronic Kidney Disease. Exercise, when tailored to an individual's condition, can improve cardiovascular health, control blood pressure, and enhance overall well-being. It also helps with weight management and may alleviate some CKD-related symptoms.
Adequate sleep is equally vital, as it promotes kidney function and overall health. Poor sleep patterns can contribute to increased inflammation and elevated blood pressure, both of which can exacerbate CKD.
To incorporate these habits effectively, establish a routine that includes regular exercise sessions, prioritizes sleep hygiene, and manages stress through relaxation techniques like meditation.
Consulting with healthcare providers and specialists can help design an exercise plan that is safe and beneficial for your CKD stage, while also addressing any sleep issues. By consistently adhering to these healthy habits, individuals with CKD can actively contribute to the management of their condition and improve their quality of life.
Sustaining Long-Term SuccessSustaining long-term success in managing renal diet limits is crucial for individuals with Chronic Kidney Disease. To achieve this, it's essential to cultivate a balanced and sustainable approach to dietary restrictions.
First and foremost, continued communication with healthcare providers and registered dietitians is key. Regular check-ups and consultations can help adjust the diet plan as needed and ensure it aligns with the evolving needs of the individual's CKD stage.
Furthermore, education plays a vital role. Understanding the reasons behind dietary restrictions, the impact of various foods on kidney health, and the potential consequences of non-compliance can motivate individuals to adhere to their dietary guidelines.
Incorporating variety into the renal diet can also contribute to long-term success. Exploring new recipes, experimenting with different food combinations, and seeking out kidney-friendly alternatives to favorite dishes can make the diet more enjoyable and sustainable.
Lastly, involving family and friends in the journey can provide crucial support, making it easier to navigate the challenges of long-term dietary restrictions and maintain a healthier lifestyle.
The Challenge of Starting a New Renal DietStarting a new renal diet is a pivotal step in managing Chronic Kidney Disease. It entails breaking old eating habits and embracing a diet tailored to kidney health.
The journey begins with understanding the dietary restrictions and their importance. However, sustaining consistency with these new dietary guidelines can be a challenge.
In this article section, we'll explore strategies to initiate this transformative process, overcome the hurdles of ingrained eating habits, and maintain steadfast adherence to the renal diet, promoting better kidney health and overall well-being.
Breaking Old Eating HabitsBreaking old eating habits isn't easy, especially when managing a renal diet. You may find yourself grappling with emotional eating, but remember that change is possible with mindful consumption.
Emotional Eating: It's crucial to identify triggers and seek healthier ways to cope. Stress management techniques can help you avoid using food as comfort.Mindful Consumption: Pay attention to what you eat and why you're eating it. This helps curb mindless snacking. Food Journaling: Keep a record of what you consume daily. It aids in identifying unhealthy patterns and tracking improvements.Junk Food Alternatives: Opt for kidney-friendly alternatives like fresh fruits, vegetables, lean proteins instead of the usual junk food.Stay committed! Remember, every small step towards healthier choices positively impacts your renal health.
Maintaining Dietary Routine ConsistencyMaintaining dietary routine consistency when embarking on a new renal diet is essential for successfully managing Chronic Kidney Disease. As individuals transition to this specialized diet, they often encounter the need to break old eating habits and embrace unfamiliar food choices. To achieve and sustain dietary consistency, a few key steps are vital.
These include thorough education about the renal diet's principles, seeking guidance from registered dietitians or healthcare providers, meticulous meal planning, and the gradual integration of kidney-friendly foods into daily routines. Patience and perseverance are crucial, as change takes time. By establishing a consistent dietary routine that aligns with CKD recommendations, individuals can better manage their condition, reduce the risk of complications, and enhance their overall quality of life.
Embracing Positivity in Managing Renal Diet LimitsIf you spend all your time focusing on renal diet limitations, instead of exploring new food options, new recipes, and a new way of enjoying your food, you're going to end up feeling cranky, deprived, and negative. If, instead you choose to focus on what an adventure it might be to learn a new way of cooking and eating at this stage in life, you'll find that you're much fonder of the foods you prepare and happier you are in general.
Adventure in New RecipesExploring new recipes can be a fun adventure, even when you're dealing with dietary restrictions. Recipe experimentation allows you to play with taste preferences while considering nutritional needs. Adapting cultural cuisine can introduce exciting flavors and keep meal planning engaging.
Now, here are four techniques to make your renal diet journey more thrilling:
Experiment with various recipes that align with your dietary needs.Identify your taste preferences and incorporate them into your meals.Explore cultural cuisine adaptations as they offer a wide array of flavors.Consider the usage of approved dietary supplements to bolster nutrition.Maintaining Positive Dietary MindsetAdopting a positive mindset, you'll find that meal planning can be a delightful process rather than a chore. Incorporating mindful eating into your daily routine will not only help manage renal diet restrictions but also reduce emotional eating. Remember, it's about savoring each bite, appreciating the food's nutrients and how they support your health.
Utilize positive affirmations to reinforce your efforts. Say things like 'I am making healthy choices for my body' and believe in them. This simple act aids stress reduction, boosting your overall mood and wellbeing.
Lastly, remember to practice self-compassion. It's okay if you slip up or face challenges along the way; what matters is getting back on track. Your dietary journey should always be filled with kindness towards yourself.
Frequently Asked QuestionsWhat Are Some Delicious Kidney-Friendly Recipes I Can Try?There are several delicious kidney-friendly recipes to try:
1. Lemon Herb Grilled Chicken: Marinate chicken breasts in a mixture of lemon juice, herbs, and olive oil, then grill to perfection.
2. Cauliflower Mashed Potatoes: Replace traditional potatoes with cauliflower for a lower-potassium alternative.
3. Salmon with Dill Sauce: Baked or grilled salmon topped with a creamy dill sauce made from low-phosphorus ingredients.
4. Black Bean and Quinoa Salad: A protein-packed salad with black beans, quinoa, fresh vegetables, and a citrus vinaigrette.
5. Vegetable Stir-Fry: Load up on kidney-friendly vegetables and tofu or lean protein, stir-fried with a low-sodium sauce.
These recipes are both delicious and suitable for a renal diet, providing a variety of flavors while adhering to dietary restrictions.
It's advisable for individuals managing renal diet limits to exercise caution with alcohol consumption. Alcohol can affect kidney function and interact with medications. Moderation is key, and it's essential to consult with a healthcare provider or dietitian to determine the safe limit based on individual health and medications.
Some low-potassium and low-phosphorus alcoholic options, like certain wines or light beers, may be better choices. However, it's crucial to monitor how alcohol affects one's condition and make informed choices to protect kidney health.
Managing a renal diet while dining out or traveling requires careful planning. Research restaurants in advance to find those with kidney-friendly options. When ordering, ask for modifications to suit your dietary needs, such as requesting sauces or dressings on the side and opting for grilled or steamed dishes.
Bring low-phosphorus snacks for travel and stay hydrated. Pack medications and dietary supplements, and inform travel companions about your dietary restrictions. Flexibility and communication are key; don't hesitate to discuss your needs with restaurant staff or accommodations when traveling to ensure a successful renal diet away from home.
Supplements and vitamins should be taken under the guidance of a healthcare provider or registered dietitian when managing a renal diet. Common supplements for CKD patients include vitamin D and iron, but their usage should be determined based on individual needs and lab results. Phosphate binders may also be prescribed to manage phosphorus levels.
It's crucial not to self-prescribe supplements, as excessive intake can lead to complications. Regular monitoring and consultation with a healthcare professional are essential to tailor supplement usage to specific renal diet requirements.
Handling cravings for foods not included in your renal diet can be challenging but manageable. Firstly, acknowledge your cravings and understand the importance of dietary restrictions for your health. Seek kidney-friendly alternatives or recipes that mimic the flavors you crave.
Distract yourself with enjoyable activities, practice portion control if occasional indulgence is safe, and stay hydrated to reduce cravings. Connecting with a support group or dietitian can provide valuable strategies for managing cravings while adhering to your renal diet for better kidney health.
Managing renal diet limits requires a positive approach and practical strategies. While initially restrictive, exploring kidney-friendly foods can make the journey enjoyable.
Understanding its importance for Chronic Kidney Disease is vital. CKD often lacks symptoms until advanced stages, making a renal diet essential.
Sodium restrictions are crucial due to their link to kidney disease and hypertension, especially with packaged foods' high sodium content. Balancing animal and plant proteins, avoiding phosphorus additives, limiting potassium-rich foods, and draining canned items can tailor the diet. Incorporating heart-healthy foods is crucial, given cardiovascular risks in CKD.
Breaking old habits and maintaining consistency can be challenging but rewarding. Through positivity and these strategies, you can manage renal diet limits effectively.
The post Managing Renal Diet Limits appeared first on Renal Diet HQ.
Suggested Reading:
CKD Diet GuidelinesWhat Is Chronic Kidney DiseaseFoods To Avoid With Kidney DiseaseAugust 19, 2023
Meal Planning for Families With CKD
At any stage of chronic kidney disease (CKD), meal planning is one of the most important factors to a healthy lifestyle. What you eat and drink has major implications to your health and comfort.
If you are cooking to feed a family and not just yourself, you want to be able to make kidney safe meals that your whole family can enjoy. After all, you do not want to have to cook separate meals for yourself and your family. Not only that, but it is always a good idea to start your family eating healthier, especially with a history of illness in the family.
In this article, weâll talk about strategies on how to plan meals for the family when a member needs dietary modifications for a renal diet.
[feast_advanced_jump_to] Kidney-safe-meals-the-whole-family-can-enjoyKey TakeawaysA well-planned kidney-friendly diet is crucial for managing CKD in families.Choosing foods low in sodium, potassium, and phosphorus is important for maintaining kidney health.Consulting with a dietician and monitoring mineral intake, fluid levels, and potassium levels in the diet is essential for families with CKD.
Kidney-safe-meals-the-whole-family-can-enjoyKey TakeawaysA well-planned kidney-friendly diet is crucial for managing CKD in families.Choosing foods low in sodium, potassium, and phosphorus is important for maintaining kidney health.Consulting with a dietician and monitoring mineral intake, fluid levels, and potassium levels in the diet is essential for families with CKD.Understanding the Importance of a Kidney-Friendly DietFor More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
A kidney-friendly diet plays a pivotal role in managing Chronic Kidney Disease by mitigating the strain on these vital organs. Understanding the fundamentals of a renal diet is essential for people with kidney disease, as it involves specific restrictions to optimize kidney function and overall health. Here, we delve into the key principles and restrictions of a renal diet, shedding light on its profound impact on CKD management.
Kidney Diet's Role in CKDThe role of a renal diet in the management of Chronic Kidney Disease cannot be overstated. CKD is characterized by the gradual loss of kidney function, leading to a buildup of waste and excess fluids in the body. A well-designed renal diet is tailored to alleviate the strain on the kidneys, slow disease progression, and improve overall health.
First and foremost, a renal diet aims to regulate the daily intake of protein, phosphorus, potassium, and sodium. Protein restriction is essential to reduce the burden of waste products that the kidneys must filter, while controlling phosphorus and potassium helps maintain proper mineral balance in the blood. Sodium moderation aids in managing blood pressure, a crucial factor in CKD.
Moreover, adequate calorie intake is crucial to prevent malnutrition, a common concern in CKD patients. Hence, a balance must be struck intake of nutrients and calories. Hydration is also monitored, as excessive fluid intake can lead to edema and high blood pressure.
A renal diet plays a pivotal role in CKD management by alleviating the workload on the kidneys, preserving kidney function, and promoting overall well-being in individuals with this chronic condition. Consulting a registered kidney dietitian is essential to create a personalized renal diet plan tailored to an individual's specific needs and stage of CKD.
Dietary Restrictions in CKDMeal planning for families dealing with Chronic Kidney Disease necessitates careful consideration of dietary restrictions to support the health of affected individuals. Key restrictions include:
Protein Control: Reducing protein intake, particularly animal proteins, helps minimize the buildup of waste products in the blood. High-quality, lower-protein sources like fish, poultry, and plant-based options are preferred.Phosphorus Management: CKD often leads to elevated phosphorus levels in the blood, which can weaken bones. Limit phosphorus-rich foods like dairy, nuts, and processed foods with additives.Potassium Moderation: Elevated potassium levels can pose risks to heart health. High potassium foods, such as bananas, potatoes, and oranges, must be monitored and restricted.Sodium Restriction: Controlling sodium intake helps manage blood pressure and fluid retention. Processed foods, canned soups, and high-sodium condiments should be minimized.Fluid Monitoring: Fluid intake should be regulated to prevent fluid overload and edema. This includes accounting for liquid from foods like soups and fruits.Caloric Balance: Maintaining a healthy weight and preventing malnutrition is crucial. Calorie intake must be adequate while accounting for nutrient restrictions.Medication Interactions: Some foods can interact with medications, affecting their effectiveness. Knowledge of these interactions is vital.Overall, meal planning for CKD involves balancing nutritional needs with these restrictions, promoting kidney health, and supporting the well-being of the entire family. Consultation with a registered dietitian is invaluable in creating customized meal plans that address individual needs and CKD stages.
Implementing and Adapting Your Kidney-Friendly Eating PlanYou've learned the importance of a kidney-friendly diet, but now it's time to put that knowledge into action. Adapting your eating habits for chronic kidney disease isn't as daunting as it may seem and we're here to guide you every step of the way.
Let's delve into how you can implement a kidney-friendly meal plan that not only benefits your health, but also suits your lifestyle and personal tastes.
Adapting Diet for CKDAdapting typical family meals to a kidney-friendly diet for CKD patients involves making conscious and health-conscious choices. Start by reducing the protein content, especially animal-based sources, and focusing on lean cuts or plant-based sources of protein like tofu or black beans.
Be vigilant about phosphorus and potassium levels, opting for low potassium fruits and vegetables while limiting high-phosphorus foods like dairy products. Cutting back on salt and using herbs and spices for flavor can help control dietary intake of sodium.
Portion control is essential, particularly with high protein foods. Balancing meals with the guidance of a registered dietitian ensures that necessary nutrients are not compromised while adhering to dietary restrictions.
Involving the whole family in these changes can make mealtimes more inclusive, supportive, and healthy for everyone, aligning with the needs of CKD patients without sacrificing flavor or enjoyment.
Implementing Kidney-Friendly PlanAdopting a kidney-friendly diet can make a big difference in your overall well being. This means understanding dietary restrictions, reading food labels carefully during grocery shopping, practicing portion control, and tracking intake of nutrients.
Here's a simple guide to help you:
Dietary RestrictionsGrocery ShoppingPortion Control & Nutrient TrackingAvoid high-sodium foodsChoose fresh low potassium fruits and vegetablesUse measuring cups or a digital scaleLimit protein intakeBuy lean meatsKeep daily logs of food consumptionReduce phosphorus-rich foodsChoose low phosphorus vegetablesMonitor potassium, sodium, and protein levelsFollowing this plan will not only support your kidneys but also promote healthier lifestyle choices. Remember to consult your healthcare provider before making any major dietary changes.
Important Factors in a Kidney-Friendly DietIn the realm of kidney health, a well-structured renal diet is a cornerstone of management. In this section, we delve into the crucial factors that constitute a kidney-friendly diet. From the meticulous control of sodium intake to the delicate balance of protein, potassium, and phosphorus restrictions, understanding these elements is essential for individuals with kidney-related concerns.
Let's explore how each component plays a pivotal role in nurturing kidney health and overall well-being.
Managing Sodium IntakeManaging sodium intake in a family meal plan for a renal diet is of paramount importance in Chronic Kidney Disease management. Excess sodium can lead to elevated blood pressure and fluid retention, placing additional strain on the kidneys. To effectively control sodium:
Read Labels: Scrutinize food labels for sodium content and choose low-sodium or salt-free products.Cook from Scratch: Preparing meals at home allows you to control sodium levels by using fresh ingredients and avoiding high-sodium additives.Limit Processed Foods: Minimize processed, canned, and fast foods, as they often contain hidden sodium.Use Herbs and Spices: Enhance flavor with herbs, spices, lemon juice, or vinegar instead of salt.Rinse Canned Goods: Rinse canned vegetables, beans, or other canned items to reduce sodium.Portion Control: Be mindful of portion sizes to avoid excessive sodium consumption.By adhering to sodium restrictions in a renal diet, you help regulate blood pressure and fluid balance, which are critical for slowing the progression of CKD and maintaining overall health.
Choosing Healthy ProteinsSelecting healthy high quality proteins is a crucial aspect of meal planning for a family following a renal diet. In Chronic Kidney Disease, it's essential to balance protein intake to reduce the burden on the kidneys while still meeting nutritional needs.
Opt for lean high protein foods like skinless poultry, fish, and plant-based options such as tofu, legumes, and beans. Limit or avoid high-phosphorus protein sources like dairy and red meat, which can be detrimental to kidney health. Proper portion control is vital to ensure protein intake aligns with dietary recommendations.
Collaborating with a registered dietitian can help create balanced and delicious meals that cater to the entire family's protein requirements while supporting the dietary restrictions necessary for people with kidney disease.
Balancing Potassium in DietRestricting potassium in meal planning for families dealing with Chronic Kidney Disease is essential to manage potassium levels in the blood, which can otherwise become dangerously high. Here are some strategies:
Choose Low-Potassium Foods: Focus on low potassium fruits and vegetables. Opt for apples, berries, green beans, and cauliflower over high-potassium options like bananas, oranges, and potatoes.Cooking Techniques: Certain cooking methods, like boiling, can leach potassium from foods. Rinse and boil vegetables before consumption to reduce their potassium content.Portion Control: Be mindful of portion sizes, as even low-potassium foods can contribute to high intake if consumed in large quantities.Limit High-Potassium Ingredients: Avoid or minimize high-potassium ingredients such as avocados, dried fruits, and tomatoes in recipes.Processed Foods: Reduce the consumption of processed foods, as they often contain added potassium-based additives.Consult a Dietitian: Work with a registered dietitian to create customized kidney disease meal plans that balance potassium restriction with essential nutrient needs for the entire family.By implementing these measures, families can effectively manage potassium intake while still enjoying nutritious and satisfying meals that align with the dietary needs of CKD patients.
Managing PhosphorusManaging phosphorus intake is crucial when meal planning for families dealing with Chronic Kidney Disease as high phosphorus levels can lead to complications such as bone and heart problems. Here's how to restrict phosphorus:
Limit High-Phosphorus Foods: Reduce or eliminate foods rich in phosphorus like dairy products, nuts, seeds, and whole grains. Opt for lower-phosphorus alternatives.Watch for Additives: Be cautious of food additives like phosphates (often found in processed foods and sodas) that can significantly increase phosphorus intake.Choose Fresh Meats: Select fresh meats like chicken, turkey, and fish over processed or cured meats, which tend to have higher phosphorus levels.Dairy Alternatives: Substitute high-phosphorus dairy with non-dairy options like almond or rice milk, which are typically lower in phosphorus.Cooking Methods: Some cooking techniques like boiling can reduce phosphorus content. Pre-soak and rinse beans and grains before cooking to lower their phosphorus levels.Portion Control: Be mindful of portion sizes, as even lower-phosphorus foods can contribute to high intake if consumed excessively.Consult a Dietitian: Collaborate with a registered dietitian to create balanced kidney disease meal plans that meet the dietary restrictions of CKD while providing adequate nutrition for the entire family.By incorporating these strategies into family meal planning, it's possible to effectively manage phosphorus intake and support the health of CKD patients.
Mindful Fluid ConsumptionManaging fluid intake is critical when planning meals for families with members who have Chronic Kidney Disease to prevent fluid overload and maintain proper fluid balance. Here's how to effectively manage fluid intake:
Know Individual Needs: Understand the specific fluid restriction guidelines for each family member with CKD. These recommendations are typically personalized based on the stage of CKD and individual health.Limit High-Fluid Foods: Be cautious with high-fluid foods like soups, broths, and foods with high water content like watermelon and cucumbers. Portion control is key.Monitor Beverage Choices: Encourage family members with CKD to choose beverages carefully. Limit sodium rich and high-potassium drinks like sports drinks, colas, and some fruit juices.Use Ice Chips: Offer ice chips or frozen fruit pieces as a way to provide a sense of hydration without excessive fluid intake.Limit Salt: Reducing sodium intake helps control thirst. Cook with less salt, and avoid high-sodium condiments and processed foods.Consult a Dietitian: Collaborate with a registered dietitian who can develop healthy eating plan and fluid restrictions tailored to the individual needs of family members with CKD.Effectively managing fluid intake is essential in preventing complications like fluid retention and high blood pressure, promoting kidney health, and enhancing overall well-being for families dealing with CKD.
The Significance of Meal Planning in Managing CKDMeal planning takes on heightened importance when a family member is diagnosed with Chronic Kidney Disease. Proper nutrition and dietary restrictions play vital roles in managing and minimizing progression of kidney disease. In this section, we delve into the significance of a healthy eating plan especially when a family member is dealing with a medical conditions especially a chronic illness.
From understanding dietary restrictions to optimizing nutrient intake, we explore how strategic meal planning can not only support the health of the CKD-afflicted family member but also foster an environment of wellness and unity within the family.
Benefits of Meal PlanningMeal planning for a family member on a renal diet due to Chronic Kidney Disease offers numerous benefits that extend beyond just managing the condition.
Disease Management: A well-structured renal diet helps slow the progression of kidney disease, reduces complications like high blood pressure, and minimizes the strain on the kidneys, ultimately improving the patient's overall health.Nutritional Balance: Careful meal planning ensures that the patient receives essential nutrients while adhering to dietary restrictions. It prevents malnutrition and promotes better energy levels and overall well-being.Family Involvement: Inclusive meal planning encourages the whole family to adopt healthier eating habits. It fosters empathy, support, and unity among family members.Cost-Efficiency: Planning meals in advance reduces food waste and encourages cost-effective shopping, making it a budget-friendly approach.Stress Reduction: Knowing what to prepare in advance reduces mealtime stress and ensures that the patient consistently follows the prescribed diet.Improved Compliance: By accommodating the patient's dietary needs within family meals, adherence to the renal diet becomes easier and more sustainable.Overall, meal planning for a family member with CKD not only contributes to their health but also creates a nurturing and supportive environment that benefits the entire family.
Meal Planning ChallengesMeal planning for families with a member requiring a renal diet due to Chronic Kidney Disease (CKD) can be challenging due to various dietary restrictions. Here are common challenges and possible solutions:
ChallengeSolutionLimited Food ChoicesSeek a registered dietitian's guidance to identify alternative ingredients and creative recipes within dietary constraints.Balancing NutrientsCollaborate with a dietitian to ensure meals meet nutritional needs while adhering to sodium, potassium, phosphorus, and protein limits.Taste and VarietyExperiment with herbs, spices, and flavor-enhancing techniques to make renal-friendly meals more appetizing and diverse.Family PreferencesFind compromise by modifying family-favorite recipes to meet renal diet requirements or identify shared dishes that align with restrictions.Meal Planning FatigueDevelop a weekly meal plan with rotating recipes to reduce monotony and streamline grocery shopping.Budget ConstraintsPlan budget-friendly meals by focusing on local, seasonal produce and affordable protein sources, and buying in bulk when possible.Time ConstraintsUtilize meal prep techniques like batch cooking to save time during the week, and involve family members in cooking to distribute the workload.These solutions can help families overcome challenges in meal planning for individuals with kidney conditions, making the process more manageable and supportive of the patient's dietary needs.
Exploring Salt-free Seasoning Options for Tastier MealsAs you navigate your journey with managing CKD, it's essential to explore the world of salt-free seasoning and healthier options for tastier meals.
Let's delve into how using herbs and spices can not only enhance the flavor of your dishes but also offer health benefits.
Alternative seasonings are more than just substitutes for saltâthey're a key part of creating delicious, kidney-friendly meals.
Herbs and Spices UsageUsing herbs and spices to flavor meals is a smart and delicious strategy when preparing family meals for a member on a kidney diet due to Chronic Kidney Disease. It's especially important because reduced salt consumption is a key aspect of managing CKD.
Herbs like basil, oregano, thyme, and rosemary, along with spices such as cumin, paprika, and turmeric, add layers of flavor without the sodium overload of salt. Fresh herbs like cilantro, parsley, and chives provide a burst of freshness to dishes. Citrus zest and juice can also enhance taste.
By embracing these natural flavor enhancers, families can maintain the appeal of their favorite recipes while accommodating the dietary restrictions of the CKD patient. Moreover, it encourages healthier eating habits for the entire family, promoting a balanced and kidney-friendly diet.
Alternative Seasoning BenefitsOpting for seasonings, spices, and herbs over salt in a family-friendly renal diet plan offers a multitude of benefits. Firstly, it supports the management of Chronic Kidney Disease by reducing sodium intake, thus helping to control blood pressure and fluid retention, common issues in CKD.
Secondly, these natural flavor enhancers introduce diversity and depth of taste to meals, making them more enjoyable and appealing. This encourages family members to embrace a healthier, kidney-friendly eating pattern.
Additionally, using herbs and spices promotes creativity in the kitchen, allowing for culinary experimentation and the discovery of new, delicious recipes. By reducing reliance on salt and emphasizing these flavorful alternatives, families not only support the dietary needs of the CKD patient but also cultivate a broader appreciation for wholesome, nutritious, and satisfying meals that benefit everyone's health.
The Benefits of Choosing Fresh Ingredients Over Canned OnesIt should come as no surprise that fresh vegetables, beans, and more taste so much better than canned. Your whole family will notice the difference when the food on their plate is fresh and delicious, and your health will fare better for it too.
When you cannot find what you are looking for fresh, you can also turn to frozen as most of the vitamins and nutrients are preserved in freezing, and there are no extra preservatives like there are in canned. Whatever you can get that is the freshest, the better off you will all be.
Nutritional Value DifferencesThe nutritional value of fresh healthy foods far surpasses that of canned foods, making fresh ingredients the preferred choice for family-friendly and kidney-friendly meals.
Fresh foods are rich in essential vitamins, minerals, and antioxidants because they haven't undergone the high-heat canning process that can degrade these key nutrients. Fresh produce is also lower in sodium compared to canned counterparts, crucial for kidney health.
Moreover, fresh foods offer superior flavor and texture, making meals more appealing to both adults and children. This encourages the consumption of a wider variety of nutritious foods, which is essential in crafting well-rounded and kidney-friendly family meals.
While canned options may be more convenient, prioritizing fresh ingredients when meal planning ensures that the family receives the best possible nutritional support, especially when considering the dietary restrictions often associated with Chronic Kidney Disease.
Preservatives and Health ImpactsPreservatives in canned and processed foods can have significant health implications, particularly for individuals with Chronic Kidney Disease. Many processed foods are high in sodium-based preservatives like monosodium glutamate (MSG) or sodium benzoate, which can lead to elevated blood pressure and fluid retention, both detrimental to kidney disease patients.
Additionally, canned foods may contain phosphorus-based preservatives, further exacerbating the phosphorus imbalance common in CKD. Furthermore, certain preservatives can have adverse effects on overall health, potentially increasing the risk of other chronic conditions that often coexist with CKD, such as heart disease.
Therefore, for CKD patients, minimizing the consumption of processed and canned foods with high preservative content is crucial in managing the disease, preserving kidney function, and maintaining overall well-being. Opting for fresh, whole foods and cooking from scratch is the healthiest approach.
Discovering Delicious and Kidney-Safe Substitutes for Favorite FoodsYou're probably wondering how to keep meals flavorful while also ensuring they're safe for your kidneys. In our next discussion, we'll delve into exploring kidney-safe substitutes for your favorite foods. We'll also cover how to enhance flavor naturally, giving you the ability to enjoy meals that are both delicious and beneficial for your health.
Exploring Kidney-Safe SubstitutesKidney-safe substitutes for meal staples are essential for individuals with Chronic Kidney Disease who need to adhere to a renal diet. Here are some key substitutions:
Protein: Replace high-phosphorus meats like beef and pork with lean cuts of chicken or turkey. For plant-based options, consider tofu or tempeh.Dairy: Swap dairy milk for lower-phosphorus alternatives like almond milk or rice milk. Use low-phosphorus cheeses or nutritional yeast sparingly.Grains: Choose white rice or pasta over whole grains like brown rice, wild rice, or whole wheat pasta, which contain higher phosphorus levels.Bread: Opt for white bread instead of whole grain or whole wheat bread, which have more phosphorus.Salt: Use herbs, spices, and low-sodium seasonings instead of salt for flavor enhancement.Potatoes: Substitute white potatoes for sweet potatoes or cauliflower, which are lower in potassium.Tomato Products: Replace tomato-based sauces and products with low-sodium or homemade alternatives.These kidney-safe substitutes help individuals with CKD manage their dietary restrictions while still enjoying satisfying and flavorful meals. Consulting a registered kidney dietitian can provide personalized guidance on the best substitutions for specific dietary needs and CKD stages.
Enhancing Flavor NaturallyIncorporating herbs and spices into your dishes can naturally enhance their flavor without jeopardizing kidney health. Flavorful marinades, for instance, can be prepared using healthy condiments and homemade broths.
Don't shy away from using citrus - it's fantastic for livening up a dish. Roasting vegetables brings out their natural sweetness while also adding depth to your meals. Steamed vegetables with minimal seasoning is also a great option.Â
Here are some suggestions:
MethodIngredientsBenefitsFlavorful MarinadesHerbs, Spices, CitrusEnhances TasteHealthy CondimentsTurmeric, GarlicLowers InflammationHomemade BrothsVegetables, HerbsPacked with NutrientsUsing CitrusLemon, LimeAdds ZestRoasting VegetablesCarrots, PotatoesCaramelize Natural SugarsRemember to experiment with different combinations. It's about keeping meals tasty and kidney-friendly!
Creating and Enjoying Kidney-Safe Family Meals TogetherCatering to the dietary needs of a member with Chronic Kidney Disease while ensuring kid-friendly healthy options can be a delicate balance. In this part, we explore the art of creating kidney-safe meal plans that not only support the health of CKD patients but also delight the taste buds of the little ones.
Discover how to strike the perfect harmony between nutritional requirements and family-friendly flavors, making mealtime a joyous and wholesome experience for everyone.
Kidney-Safe Meal PlanningKidney-safe meal planning that accommodates the health needs and preferences of every family member is a delicate yet achievable balance. To create harmonious family meals:
Consult a Dietitian: Seek guidance from a registered dietitian who specializes in renal nutrition. They can craft customized meal plans that meet the dietary restrictions of the CKD patient while ensuring balanced nutrition for all.Modify Family Favorites: Adapt beloved recipes to align with renal diet requirements. For instance, use lower-phosphorus dairy or reduce sodium content.Incorporate Variety: Introduce a wide range of kidney-safe ingredients to keep meals exciting. Experiment with herbs, spices, and flavorful low-sodium sauces.Family Involvement: Involve family members in meal preparation to foster a sense of participation and understanding of dietary restrictions.Delicious Options for Kids: Incorporate appealing, renal-friendly dishes that cater to the tastes of children. Consider dishes like grilled chicken skewers, vegetable stir-fries, or fruit salads.By emphasizing communication, creativity, and collaboration, kidney-safe meal planning can nurture both the health and happiness of every family member, making mealtimes a source of unity and well-being.
Kid Friendly and Kidney Friendly MealsMeal planning for kidney-friendly meals that cater to children in the family requires a careful and balanced approach. Begin by consulting with a registered dietitian who specializes in renal nutrition to create a foundation that meets the specific dietary restrictions of the CKD patient while ensuring kid-friendly options.
When selecting ingredients, prioritize fresh fruits, vegetables, lean proteins such as chicken or turkey, and whole grains. Limit foods high in phosphorus and potassium, which are often restricted in a renal diet.
To enhance flavor without relying on salt, use a variety of herbs, spices, and low-sodium seasonings. Gradually reduce salt in recipes to acclimate taste buds to lower sodium levels.
Adapt family-favorite recipes to align with renal diet restrictions. For instance, prepare a kidney-friendly pasta dish using ingredients suitable for both the patient and children.
Additionally, make meals visually appealing and colorful to pique the interest of children. Engage them in meal planning and preparation to foster a sense of involvement and curiosity about healthy eating.
For snacks, offer healthier options like sliced fruits, yogurt, crunchy vegetables, or low-sodium crackers that are suitable for both the CKD patient and the kids. By striking this balance, you can ensure that meals are both nutritious for kidney health and enjoyable for the entire family.
Frequently Asked QuestionsWhat Are Some Easy, Kidney-Friendly Recipes for a Busy Weekday?For busy weekdays, quick and kidney-friendly recipes are essential. Try dishes like a simple grilled chicken breast with steamed broccoli and a side of quinoa. Another option is a stir-fry with lean protein (chicken, tofu) and a mix of low-potassium vegetables, served over brown rice.
You can also make a kidney-friendly pasta salad using whole wheat pasta, diced cucumbers, and cherry tomatoes with a lemon-herb vinaigrette. These recipes are easy to prepare, low in sodium, and can accommodate dietary restrictions for those with kidney concerns.
Maintaining a healthy diet while dining out or traveling requires careful planning. Before your trip, research restaurants that offer renal-friendly options, and check their menus online. When dining out, communicate your dietary restrictions to the server, and don't hesitate to request modifications to suit your needs.
Managing portion sizes is essential, so consider splitting meals or taking leftovers with you. Avoid high-risk foods like those high in sodium, potassium, or phosphorus. To stay prepared, carry kidney-friendly snacks for on-the-go.
Hydration is crucial, but be mindful of fluid intake within the recommended limits. Don't forget to pack your medications and adhere to prescribed doses while monitoring your potassium and phosphorus levels. These strategies will help you enjoy your outings or travels while maintaining your kidney-friendly diet.
Just because you are living with kidney disease or illness does not mean that you have to eat separately, or that you and your family cannot enjoy your meals together. There are plenty of kidney safe, family friendly meals that you can make. It all starts with a little planning.
Managing CKD in your family starts with a kidney-friendly diet. Monitor potassium, phosphorus, and fluid levels for optimal health. Explore salt-free seasonings and fresh ingredients to make delicious meals. Try kidney-safe substitutes for favorite foods and enjoy creating family meals together.
A well-planned meal is crucial in dealing with CKD effectively. Remember, you're not just eating right; you're enhancing the quality of life for your loved ones too!
The post Meal Planning for Families With CKD appeared first on Renal Diet HQ.
Suggested Reading:
Foods To Avoid With Kidney DiseaseCKD Diet GuidelinesWhat Is Chronic Kidney DiseaseAugust 18, 2023
CKD Diet Guidelines
When you have chronic kidney disease or CKD, you need to follow a special type of diet to ensure that your body will continue to function well despite your kidney disease. A CKD diet or renal diet will control the amount of protein, phosphorus, calcium, sodium, and potassium in your diet, since your kidneys can no longer remove the toxins and waste products in your body.
If you have CKD, you need to have a CKD diet in order to decrease the workload of your kidney and maintain its function. You will need a nutritionist to help you plan your CKD diet. But for the meantime, here are the guidelines that you need to remember if you are planning to have a CKD diet.
[feast_advanced_jump_to] Key TakeawaysManaging nutrition in CKD, including protein balance, phosphorus, potassium, sodium, and fluid control, is crucial for kidney health.Proper CKD nutrition can slow disease progression, control blood pressure, and alleviate symptoms while preventing complications.The renal diet emphasizes protein restriction, mineral control, sodium reduction, and balanced nutrition, tailored to CKD stages.Dialysis patients have higher protein needs but must still manage minerals, sodium, and fluid, while the DASH diet offers heart-healthy principles.Plant-based diets can benefit CKD patients, but they require careful planning, carbohydrate management is vital, and consulting healthcare professionals is essential.
Key TakeawaysManaging nutrition in CKD, including protein balance, phosphorus, potassium, sodium, and fluid control, is crucial for kidney health.Proper CKD nutrition can slow disease progression, control blood pressure, and alleviate symptoms while preventing complications.The renal diet emphasizes protein restriction, mineral control, sodium reduction, and balanced nutrition, tailored to CKD stages.Dialysis patients have higher protein needs but must still manage minerals, sodium, and fluid, while the DASH diet offers heart-healthy principles.Plant-based diets can benefit CKD patients, but they require careful planning, carbohydrate management is vital, and consulting healthcare professionals is essential.Understanding the Role of Nutrition in CKDFor More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
In the complex landscape of Chronic Kidney Disease, understanding the pivotal role of nutrition is paramount. This section looks into the intricate interplay between diet and CKD, shedding light on common nutritional challenges faced by individuals with this condition.
From the delicate balance of protein intake to the management of phosphorus, potassium, and sodium, we explore the nuanced world of renal nutrition. Moreover, we unveil the profound benefits of a well-structured diet in CKD management, showcasing how proper nutrition can be a powerful ally in preserving kidney health and enhancing overall well-being.
Nutritional Issues in CKDChronic Kidney Disease presents a range of nutritional challenges that require careful management.
One primary concern is protein intake. CKD patients often need to restrict protein to lessen the burden on compromised kidneys, but inadequate protein can lead to malnutrition and muscle wasting.
Phosphorus control is equally vital. Damaged kidneys struggle to excrete excess phosphorus, leading to elevated levels in the blood, which can weaken bones and harm cardiovascular health.
Potassium regulation is another issue. High potassium foods like bananas and potatoes can be problematic, as hyperkalemia (high potassium levels) can disrupt heart rhythm.
Sodium restriction is crucial to manage fluid balance and blood pressure, so avoiding foods high in sodium is paramount.
Additionally, CKD patients must pay attention to fluid intake, vitamin and mineral deficiencies, and caloric intake to prevent weight loss or gain.
Balancing these nutritional issues is key to managing CKD effectively and slowing disease progression. Regular monitoring and guidance from healthcare professionals and dietitians are essential for tailored dietary plans.
Balancing Diet With CKDA proper diet plays an important role in managing Chronic Kidney Disease (CKD) and offers numerous benefits for individuals grappling with this condition:
Slowed Disease Progression: A well-structured renal diet can slow down the progression of CKD, preserving kidney function over time.Blood Pressure Control: Proper diet helps manage blood pressure, a common complication in CKD. Reduced sodium intake and balanced nutrition support better blood pressure regulation.Phosphorus and Potassium Control: Dietary modifications help maintain optimal levels of these minerals in the blood, preventing complications such as bone disease and heart arrhythmias.Protein Balance: Proper protein intake helps prevent muscle wasting and malnutrition, two issues CKD patients are vulnerable to. It ensures that the body receives essential amino acids without overburdening the kidneys.Symptom Management: A suitable diet can alleviate CKD symptoms like edema (fluid retention), fatigue, and anemia, leading to an improved quality of life.Prevention of Other Health Complications: A well-managed diet can lower the risk of complications like cardiovascular disease and diabetes, which often accompany CKD.In essence, a proper diet tailored to individual needs is an essential tool in managing CKD, enhancing overall health, and improving the patient's quality of life. Consulting with a healthcare provider or dietitian is critical to create a personalized dietary plan.
Overview of Diets for CKDNavigating the dietary landscape with Chronic Kidney Disease involves a spectrum of tailored nutritional approaches. This article section delves into four specific diets crucial in CKD management: the renal diet, designed to alleviate the strain on compromised kidneys; the dialysis diet, fine-tuned for those undergoing renal replacement therapy; the DASH diet, renowned for its heart-healthy principles; and the plant-based diet, which offers a sustainable approach to renal nutrition.
Exploring the nuances of these CKD-specific diets unveils a diverse toolkit for individuals seeking optimal kidney health and overall well-being.
Renal DietThe renal diet, also known as the kidney diet, is a specialized nutritional plan designed to support individuals with Chronic Kidney Disease. Its primary goal is to alleviate the workload on the kidneys while maintaining overall health. Key principles of the renal diet include:
Protein Restriction: Limiting high-protein foods to reduce the production of waste products, such as urea and creatinine, which damaged kidneys struggle to filter.Phosphorus and Potassium Control: Managing intake of foods rich in these minerals, as elevated levels can harm bone health and heart function.Sodium Reduction: Lowering sodium to regulate blood pressure and fluid balance.Fluid Management: Monitoring fluid intake to prevent fluid overload and edema.Balanced Nutrition: Ensuring adequate calorie intake and intake of essential vitamins and minerals to prevent malnutrition.Regular Monitoring: Ongoing assessment and adjustment of the diet based on kidney function and individual needs.A well-structured renal diet helps slow CKD progression, manages complications, and enhances the overall quality of life for those with kidney disease.
Dialysis DietThe Dialysis diet is a specialized nutritional plan tailored for individuals undergoing renal replacement therapy, such as hemodialysis or peritoneal dialysis.
It differs significantly from the pre-dialysis renal diet due to the additional challenges and considerations brought about by dialysis.
In the Dialysis diet:
Increased Protein: Dialysis removes protein waste products, so protein intake is often higher compared to the pre-dialysis renal diet to prevent muscle wasting.Phosphorus Control: Dialysis is less effective at removing phosphorus, so strict phosphorus restriction continues, along with the use of phosphate binders.Potassium Management: Dietary potassium may be less restricted than in pre-dialysis, but careful monitoring is essential.Sodium and Fluid Control: Sodium and fluid intake are still regulated to manage blood pressure and prevent fluid overload.Caloric Needs: Dialysis may increase calorie needs due to metabolic changes.The Dialysis diet is more flexible regarding protein but still focuses on controlling phosphorus, potassium, sodium, and fluid, tailored to individual patient needs.
DASH Diet BenefitsThe DASH (Dietary Approaches to Stop Hypertension) diet is a heart-healthy eating plan with potential benefits for individuals with Chronic Kidney Disease, particularly those managing hypertension, a common complication of CKD. The DASH diet emphasizes:
Sodium Reduction: It prioritizes a lower sodium intake, which helps control blood pressure, a key concern in CKD.Rich in Fruits and Vegetables: The diet encourages ample consumption of fruits and vegetables, which provide essential nutrients and antioxidants, supporting overall health.Moderate Protein: While not specifically designed for CKD, the DASH diet includes moderate protein intake, aligning with general renal diet recommendations.Whole Grains: It promotes whole grains, which are beneficial for sustained energy and dietary fiber.Limitation of Processed Foods: DASH advises against processed and high-sodium foods, which is consistent with CKD dietary guidelines.While not explicitly designed for CKD, the DASH diet's focus on heart-healthy, whole foods aligns with many renal diet principles and can be adapted to support kidney health in individuals with CKD, especially those with hypertension.
Plant-Based Diets ImpactPlant-based diets, such as vegetarian or vegan diets, have gained recognition as viable options for individuals with Chronic Kidney Disease. These diets emphasize:
Lower Protein Content: Plant-based diets naturally contain less protein compared to animal-based diets, which can be beneficial for CKD patients who need to restrict protein intake.Reduced Phosphorus and Potassium: Many plant-based foods are lower in phosphorus and potassium, which are critical considerations in CKD to manage mineral imbalances.Heart Health: Plant-based diets can improve cardiovascular health, a significant concern for CKD patients, by reducing blood pressure and cholesterol levels.Antioxidants and Fiber: They are rich in antioxidants and dietary fiber, supporting overall health and potentially reducing inflammation.However, a plant-based diet requires careful planning to ensure adequate protein intake and prevent nutritional deficiencies.
CKD patients considering this diet should work closely with a dietitian to create a balanced and kidney-friendly plant-based eating plan tailored to their specific needs.
The Importance of Carbohydrate Management in CKDNow, letâs delve into the often-overlooked yet critical aspect of carbohydrate intake in the context of Chronic Kidney Disease and renal diabetes management.
Carbohydrates play a pivotal role in the nutritional well-being of CKD patients, impacting blood glucose control, energy levels, and overall health. Understanding the intricacies of carbohydrate intake and learning how to control it effectively is essential for individuals navigating the complex terrain of CKD, particularly those with renal diabetes.
Discover how thoughtful carbohydrate management can be a powerful ally in optimizing kidney health and enhancing the quality of life for those facing these multifaceted challenges.
Importance of Carbohydrate Intake in CKDBalanced carbohydrate intake is of paramount importance in the management of Chronic Kidney Disease for several reasons.
Firstly, carbohydrates are a primary source of energy, crucial for overall well-being and maintaining energy levels, which CKD patients often struggle with due to fatigue.
Secondly, controlling carbohydrate intake helps regulate blood glucose levels. Many CKD patients also have diabetes or are at risk of developing it, making blood sugar management critical to prevent further kidney damage and complications.
Furthermore, well-distributed carbohydrates can help prevent muscle wasting and malnutrition, which are common concerns in CKD.
Balancing carbohydrates also involves choosing the right types, favoring complex carbohydrates like whole grains, fruits, and vegetables over simple sugars. This supports heart health and minimizes the risk of cardiovascular complications, which often accompany CKD.
Managing carbohydrate intake in CKD ensures energy, blood sugar control, muscle preservation, and overall health, making it a fundamental aspect of renal nutrition and disease management.
Carbohydrate Counting BenefitsCarbohydrate control is particularly crucial in the renal diet, especially for individuals with Renal Diabetes (or Diabetic Kidney Disease). This specialized dietary approach focuses on managing blood glucose levels to prevent further kidney damage while also addressing the unique nutritional needs of CKD patients.
Carbohydrates from high-fiber sources like whole grains, fruits, and vegetables are encouraged as they have a gentler impact on blood sugar levels. Portion control and consistent carbohydrate intake throughout the day help stabilize glucose levels, reducing the risk of hyperglycemia.
Monitoring carbohydrate intake, along with phosphorus, potassium, and sodium content, is vital in managing renal diabetes. A registered dietitian can help individuals with CKD and Renal Diabetes create a personalized meal plan that balances carbohydrates while supporting kidney function and blood glucose control, optimizing overall health outcomes.
Managing Protein Intake in CKDManaging protein intake is a pivotal aspect of Chronic Kidney Disease management. Protein plays a dual role as a necessary nutrient and a potential burden on compromised kidneys. Understanding the impact of protein, and the differing requirements for pre-dialysis and dialysis patients.
Let us discover the nuanced world of protein management in CKD, providing insights into how tailored approaches can support kidney health and overall well-being for individuals at different stages of their renal journey.
Protein's Impact on KidneysProtein's impact on the kidneys is a critical consideration for individuals with Chronic Kidney Disease. While protein is essential for growth, repair, and overall health, its metabolism produces waste products, including urea and creatinine, which healthy kidneys efficiently eliminate.
However, in CKD, impaired kidney function can hinder the clearance of these waste products, leading to their accumulation in the bloodstream. Excessive protein intake can exacerbate this issue, overloading the kidneys and accelerating the progression of CKD.
On the other hand, inadequate protein intake can result in malnutrition and muscle wasting. Therefore, striking the right balance in protein intake is essential, often requiring careful monitoring and personalized guidance from healthcare professionals to support kidney health effectively.
Non Dialysis Chronic Kidney Disease Protein RequirementsProtein intake limits vary depending on the stage of Chronic Kidney Disease (CKD) to mitigate its impact on kidney function.
For individuals in CKD stages 1 and 2, the recommendation is to restrict dietary protein to no more than 0.8 grams per kilogram of their ideal body weight. This conservative approach aims to reduce the burden on the kidneys while maintaining overall health.
As CKD progresses to stages 3, 4, and 5 (Non Dialysis-CKD), the 2020 KDOQI guidelines advise further protein reduction, with recommended intake ranging from 0.55 to 0.60 grams per kilogram per day for stable patients. These lower limits are designed to slow the advancement of kidney disease and minimize the accumulation of waste products in the bloodstream.
Individual protein requirements may still vary, emphasizing the importance of personalized dietary plans and regular monitoring under the guidance of healthcare professionals to manage CKD effectively.
Dialysis Protein NeedsFor individuals undergoing dialysis, whether peritoneal dialysis or hemodialysis, protein intake recommendations are notably different compared to those with Non Dialysis Chronic Kidney Disease. The dietary guidelines suggest a higher protein intake ranging from 1.0 to 1.2 grams per kilogram of body weight per day.
This elevated protein allowance is essential because dialysis effectively removes waste products, including urea and creatinine, from the bloodstream. Consequently, dialysis patients experience higher protein loss and an increased risk of malnutrition and muscle wasting.
By increasing protein intake within this range, patients can help counteract these effects, supporting muscle maintenance, overall nutrition, and a better quality of life. However, precise protein requirements may vary among individuals, warranting personalized dietary plans and ongoing monitoring to optimize their health during dialysis treatment.
Controlling Phosphorus Intake for CKD PatientsControlling phosphorus intake is a critical component of managing Chronic Kidney Disease. Here, we delve into the intricacies of dietary phosphorus management for CKD patients, emphasizing the importance of limiting high-phosphorus foods.
Excessive phosphorus can disrupt mineral balance, particularly calcium, which may weaken bones and contribute to renal osteodystrophy, a common complication of advanced CKD. Understanding how to navigate phosphorus-rich dietary choices and the potential consequences of excessive phosphorus on bone health is essential for individuals seeking to preserve their overall well-being while dealing with the challenges of CKD.
Limiting High-Phosphorus FoodsLimiting high-phosphorus foods is a fundamental dietary strategy for managing Chronic Kidney Disease.
In CKD, impaired kidney function leads to difficulties in excreting excess phosphorus from the body, resulting in its accumulation in the bloodstream. This excess phosphorus can disrupt calcium balance, weakening bones and potentially causing vascular calcification, a serious cardiovascular risk.
To address this issue, CKD patients are typically advised to limit their daily phosphorus intake to a specific range, often falling between 800 to 1,000 milligrams. This involves avoiding or minimizing foods rich in phosphorus, such as dairy products, nuts, seeds, processed meats, and dark colored sodas and other carbonated beverages.
Instead, patients are encouraged to opt for lower-phosphorus alternatives and to carefully read food labels for phosphorus content.
Balancing phosphorus intake plays a crucial role in preserving bone health, minimizing the risk of vascular calcification, and supporting overall well-being for individuals with CKD, making it an integral part of renal nutrition. Regular monitoring and guidance from healthcare professionals or dietitians are vital for effective management.
Phosphorus Impact on BonesPhosphorus is a mineral vital for bone health, but its balance in the body is delicate. In Chronic Kidney Disease, impaired kidney function leads to difficulty in excreting excess phosphorus, and elevated blood phosphorus levels can have severe consequences for bones, often resulting in a condition called renal osteodystrophy.
Excess phosphorus disrupts the body's calcium-phosphorus balance, prompting the release of calcium from bones into the bloodstream. Over time, this leaching of calcium can weaken bones, causing them to become brittle and prone to fractures.
Renal osteodystrophy encompasses a range of bone abnormalities, including osteoporosis (reduced bone density), osteitis fibrosa (bone softening), and vascular calcification (calcium buildup in blood vessels).
Managing phosphorus intake and adhering to prescribed phosphorus binders are critical for CKD patients to prevent or mitigate the impact of renal osteodystrophy on bone health and overall well-being. Regular monitoring and guidance from healthcare professionals are essential components of effective management.
Reducing Sodium Intake for Better Kidney HealthThe effects of sodium on kidney function are profound, particularly for individuals with Chronic Kidney Disease. Sodium plays a crucial role in regulating fluid balance and blood pressure, both of which are critically important for kidney health. However, excessive sodium intake can lead to elevated blood pressure and fluid retention, increasing the strain on already compromised kidneys.
In your CKD diet, you need to limit your sodium intake to 1500 milligrams per day. Letâs now tackle the intricate relationship between sodium and CKD, emphasizing the benefits of a low-sodium diet.
Discover how reducing sodium intake can alleviate stress on the kidneys, support blood pressure control, and enhance overall renal well-being for individuals navigating the complexities of CKD.
Sodium's Impact on KidneysSodium, a crucial electrolyte, significantly impacts kidney function and overall health, particularly in the context of Chronic Kidney Disease. The kidneys play a central role in regulating sodium levels in the body. Excessive sodium intake can have detrimental effects on kidney health.
In CKD, compromised kidneys struggle to filter excess sodium from the bloodstream, leading to sodium retention and fluid buildup. This can result in edema, hypertension (high blood pressure), and increased cardiovascular risk. Elevated blood pressure, in turn, accelerates the progression of CKD, creating a vicious cycle.
Moreover, high sodium intake is associated with an increased risk of heart disease and stroke, which are common comorbidities in CKD. Reducing sodium intake is essential for CKD patients to manage blood pressure, alleviate the strain on the kidneys, and reduce the risk of fluid overload.
A low-sodium diet is a key component of renal nutrition and plays a pivotal role in preserving kidney function and overall well-being in CKD.
Implementing Low-sodium DietsImplementing low-sodium diets for individuals with Chronic Kidney Disease is essential to manage hypertension, minimize fluid retention, and support kidney health. Here are key steps in implementing such diets:
Consultation with a Dietitian: CKD patients should work closely with a registered dietitian specializing in renal nutrition. A dietitian can assess the patient's specific needs, develop a tailored meal plan, and provide ongoing guidance.Limit Processed Foods: Processed and restaurant foods often contain high sodium levels. Reducing or eliminating these items from the diet is crucial. Opt for fresh, whole foods whenever possible.Read Food Labels: CKD patients should become adept label readers, looking for terms like sodium chloride, monosodium glutamate (MSG), and baking soda (sodium bicarbonate). Foods with high sodium content should be avoided.Use Herbs and Spices: To enhance flavor without adding sodium, use herbs, spices, and salt substitutes. These can make low-sodium meals enjoyable.Monitor Fluid Intake: Controlling fluid intake is another aspect of sodium management. A dietitian can provide guidance on how much fluid is appropriate for each patient.Regular Monitoring: Frequent monitoring of blood pressure, sodium levels, and overall health status is essential. Adjustments to the diet may be necessary based on these assessments.By diligently implementing low-sodium diets under the guidance of healthcare professionals, CKD patients can effectively manage their condition, alleviate kidney stress, and reduce the risk of related complications.
Managing Potassium Intake in a CKD DietManaging potassium intake is a critical aspect of maintaining kidney health in individuals with Chronic Kidney Disease. This section looks into the intricacies of potassium management within a CKD diet, focusing on potassium-rich foods to avoid.
Elevated potassium levels, known as hyperkalemia, can pose severe health risks, including heart rhythm disturbances. By understanding which foods to limit or avoid and how to maintain a balanced potassium intake, CKD patients can effectively protect their heart and overall well-being while navigating the complexities of renal nutrition.
Potassium-rich Foods to AvoidA renal diet necessitates vigilance in avoiding potassium-rich foods to maintain proper potassium balance in individuals with Chronic Kidney Disease. High-potassium levels, or hyperkalemia, can lead to heart rhythm disturbances and pose severe health risks. Foods that should be limited or avoided include:
Bananas: Known for their potassium content, they top the list of high-potassium foods.Oranges and Orange Juice: These citrus fruits are potassium-rich and should be consumed in moderation.Tomatoes: Fresh tomatoes, tomato sauce, and tomato-based products are potassium-packed.Potatoes: Especially when baked or mashed, they are high in potassium.Spinach: Leafy greens like spinach are a potent source of potassium.Avocado: While nutritious, avocados are potassium-dense and should be restricted.Beans and Lentils: These protein-rich foods are also potassium-rich.Dairy Products: Milk, yogurt, and cheese can contribute to potassium intake.Processed Foods: Many processed foods, canned soups, and fast food items contain hidden potassium.By carefully monitoring and restricting these high-potassium foods, CKD patients can effectively manage their potassium levels and minimize the risk of complications associated with hyperkalemia. Consulting with a dietitian is essential for creating a personalized meal plan that balances nutrition and potassium intake.
Consulting Healthcare for GuidanceExcessive potassium, or hyperkalemia, poses significant complications for individuals with Chronic Kidney Disease. The impaired kidney function in CKD makes it challenging for the body to regulate potassium levels effectively, leading to a buildup of this mineral in the bloodstream.
One of the most critical complications of hyperkalemia is the risk of irregular heart rhythms. High potassium levels can disrupt the electrical signals in the heart, leading to arrhythmias, palpitations, or even cardiac arrest. This is a potentially life-threatening situation, especially for those with pre-existing heart conditions.
Hyperkalemia can also affect muscle function, causing weakness and, in severe cases, paralysis. This can significantly impact a person's mobility and overall quality of life, making it important to manage potassium levels carefully.
Gastrointestinal symptoms are another consequence of high potassium levels, with nausea, vomiting, and abdominal pain being common. These symptoms can further contribute to malnutrition and dehydration in CKD patients.
Tingling sensations or numbness, particularly in the extremities, can also occur due to hyperkalemia, further adding to the discomfort experienced by CKD patients.
Preventing and managing hyperkalemia through dietary restrictions, medications, and close medical monitoring is essential for CKD patients to protect their cardiovascular health and overall well-being. Proper management can mitigate the risk of these complications and improve the quality of life for those living with CKD.
The Role of Fluid Intake in Managing CKDAs previously mentioned, kidney disease makes you retain fluid since your kidneys cannot excrete excess fluid in your body. This could lead to swelling, or worse, fluid buildup in your lungs, thus making it hard for you to breathe.
Your suggested fluid intake in your CKD diet will depend on your urine output, fluid buildup, and blood pressure. You should also remember that foods also contain fluids, and that these should be taken into account in your CKD diet.
Fluid Retention DangersFluid retention, or edema, is a common and potentially serious complication for individuals with Chronic Kidney Disease (CKD), particularly those undergoing dialysis treatment. CKD impairs the kidneys' ability to effectively regulate fluid balance, leading to the accumulation of excess fluids in the body.
Complications of fluid retention in CKD include:
Hypertension (High Blood Pressure): Edema increases blood volume, putting additional strain on the heart and blood vessels, which can lead to hypertension, further exacerbating kidney damage.Shortness of Breath: Excess fluid can accumulate in the lungs, causing difficulty in breathing, especially when lying down.Swelling: Edema commonly causes swelling in the legs, ankles, and around the eyes, making mobility uncomfortable and limiting daily activities. Pulmonary Edema: Severe fluid retention can result in pulmonary edema, a life-threatening condition where fluid fills the lungs, leading to breathing difficulties and a risk of respiratory failure.Cardiovascular Complications: Fluid overload can increase the risk of heart failure and contribute to other cardiovascular issues, such as arrhythmias.Managing fluid retention in CKD, often through dietary restrictions and careful monitoring of fluid intake, is essential to prevent these complications, particularly for dialysis patients who are more susceptible due to the nature of their treatment.
Managing Daily Fluid IntakeManaging daily fluid intake is crucial for preventing fluid retention in Chronic Kidney Disease patients. Here are key strategies:
Fluid Restriction: CKD patients, especially those on dialysis, may have specific daily fluid allowances. Adhering to these restrictions is vital.Monitor Thirst: Pay attention to your body's signals of thirst and drink only when genuinely thirsty.Limit High-Fluid Foods: Reduce consumption of high-fluid foods like soups, ice cream, and juicy fruits.Measure Fluids: Use measuring cups to monitor fluid intake accurately.Choose Ice Chips: Sucking on ice chips can help relieve dry mouth without excessive fluid consumption.Limit Sodium: High-sodium foods can lead to thirst. Avoiding excessive salt can help control fluid intake.Consult a Dietitian: Work with a renal dietitian to develop a personalized fluid management plan tailored to your specific needs and CKD stage.By carefully managing daily fluid intake and seeking guidance from healthcare professionals, CKD patients can prevent fluid retention, reduce the risk of complications, and support their overall kidney health.
Guidelines for Dining Out With CKDAs you navigate your journey with chronic kidney disease, it's essential to understand that dining out doesn't have to be off-limits. You can still enjoy meals at restaurants, but the key lies in choosing kidney-friendly establishments and understanding how to decipher menu wording.
In this discussion, we'll guide you on how to make informed decisions about where to eat and what dishes align best with your dietary needs, based on scientific evidence and expert recommendations.
Choosing Kidney-Friendly RestaurantsDining out with Chronic Kidney Disease requires thoughtful choices to ensure your meal aligns with renal dietary restrictions. When selecting kidney-friendly restaurants:
Research Ahead: Look for restaurants with online menus, nutritional information, or specific dietary sections, making it easier to assess meal options.Call Ahead: Contact the restaurant to discuss your dietary needs and inquire if they can accommodate special requests.Choose Wisely: Opt for restaurants offering lean protein sources like grilled chicken or fish and plenty of vegetable options. Avoid dishes with high sodium, potassium, or phosphorus content.Customize Your Order: Don't hesitate to ask for substitutions or modifications to fit your dietary requirements. Most restaurants are willing to accommodate.Portion Control: CKD patients often need smaller portions. Consider sharing an entree or taking leftovers home.Beverage Selection: Limit fluids by choosing water or herbal tea over high-sugar or high-sodium beverages.Sauce on the Side: Request sauces and dressings on the side to control sodium and phosphorus intake.Dessert Alternatives: Fresh fruit or sorbet can be suitable, kidney-friendly dessert options.Choosing kidney-friendly restaurants and making informed menu choices can make dining out an enjoyable experience while prioritizing your kidney health. Always consult with a dietitian for personalized guidance on dining out with CKD.
Understanding Menu WordingUnderstanding menu wording and food labels in restaurants is vital for individuals with Chronic Kidney Disease when dining out. Here are some tips and tricks:
Ask Questions: Don't hesitate to ask your server about ingredients, preparation methods, and potential modifications to meet your dietary needs.Beware of Trigger Words: Watch for words like "grilled," "roasted," or "steamed," which often indicate healthier cooking methods with fewer added fats and salt.Avoid High-Sodium Terms: Be cautious of menu items described as "brined," "pickled," "smoked," or "in broth," as they tend to be higher in sodium.Look for Kidney-Friendly Phrases: Seek out phrases like "low-sodium," "no-salt-added," or "freshly prepared," which suggest healthier options.Consider Side Dishes: Sometimes, side dishes or appetizers offer more kidney-friendly choices than the main courses.Review Food Labels: If available, review nutritional information on food labels or ask the restaurant for these details.Simplify Orders: Choose dishes with simpler ingredient lists to reduce the risk of hidden high-sodium, potassium, or phosphorus additives.Portion Control: Pay attention to portion sizes, as larger servings can contain more of certain nutrients.By becoming savvy at interpreting menu wording and food labels, CKD patients can make more informed dining choices that align with their dietary restrictions, contributing to better kidney health while enjoying restaurant meals.
Frequently Asked QuestionsWhat Are Some Common Misconceptions About the CKD Diet?Common misconceptions about the CKD diet include the belief that all protein should be restricted (when it should be controlled but not eliminated), that all fruits and vegetables are off-limits (when many can be enjoyed in moderation), and that simply reducing sodium is enough (while potassium and phosphorus also need monitoring).
Additionally, there's often a misunderstanding that dietary restrictions mean bland and unenjoyable meals, whereas with proper guidance, CKD patients can still savor flavorful, satisfying dishes that align with their nutritional needs.
In a CKD diet, it's crucial to avoid or strictly limit alcohol and fatty foods. Alcohol can burden the kidneys and interfere with medications, while fatty foods, especially those high in unhealthy trans fats, can contribute to heart disease, a significant risk for CKD patients.
Additionally, excessive alcohol intake can lead to dehydration, further stressing the kidneys. It's essential for CKD patients to prioritize hydration and choose heart-healthy fats over trans fats found in fried and processed foods to safeguard their kidney and overall health.
The CKD diet can impact medication absorption in patients due to dietary restrictions. For instance, certain phosphate binders, commonly prescribed for CKD patients to control phosphorus levels, must be taken with meals. However, if dietary restrictions result in reduced food intake, it can affect the medication's effectiveness.
Additionally, some medications interact with specific foods that CKD patients should limit or avoid, potentially altering their absorption. Therefore, it's crucial for CKD patients to coordinate their medication schedules and dietary choices with healthcare providers or pharmacists to ensure optimal treatment outcomes.
Yes, CKD patients with comorbid conditions like diabetes face unique dietary challenges. The CKD diet needs to strike a balance between managing both conditions. Diabetes requires blood sugar control, which often involves carbohydrate monitoring, while CKD necessitates restrictions on phosphorus, potassium, and sodium.
Coordinating these restrictions can be challenging, as some diabetes-friendly foods may be high in these restricted nutrients. CKD patients with diabetes require individualized dietary plans, often with the guidance of a registered dietitian, to manage both conditions effectively while maintaining overall health.
Managing your diet with CKD isn't easy, but it's crucial. Balancing protein and carbs, controlling phosphorus and sodium intake, and monitoring potassium and fluid can significantly impact your kidney health.
With careful planning and adherence to these guidelines, you'll not only manage your CKD symptoms better but also improve your overall health. Remember to always consult with a healthcare professional before making any dietary changes.
Remember to stick to your CKD diet so that you will be able to maintain the highest quality of living achievable for people with chronic kidney disease.
SEE MY RENAL DIET MEAL PLANNERS CLICK HERE!
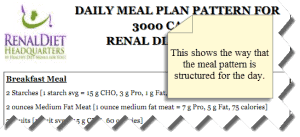 Your Daily Meal Pattern-Begins with Breakfast
Your Daily Meal Pattern-Begins with BreakfastThe post CKD Diet Guidelines appeared first on Renal Diet HQ.
Suggested Reading:
What Is Chronic Kidney DiseaseDiabetic Renal Diet Meal PlanFoods To Avoid With Kidney DiseaseAugust 17, 2023
Stages Of Chronic Kidney Disease
You're about to start learning about the complex world of chronic kidney disease. It's not easy, but understanding its stages could help you better support those dealing with this condition.
We'll break down each stage, explaining what's happening in the body and how it can be managed.
You'll also learn about treatment options like dialysis and transplant.
Get ready, we're diving deep into this crucial health topic to discuss loss of kidney function and end-stage kidney disease.Â
[feast_advanced_jump_to] Key TakeawaysEarly detection is crucial in order to slow down or stop the progression of chronic kidney disease.Lifestyle changes, such as exercise and stress management, play a significant role in managing the disease.Medical management, including medication adherence and understanding potential side effects, is important in stage three of the disease.Severe symptoms in stage four require necessary interventions, and emotional coping and support are essential for patients and their families, during the loss of kidney function.Â
Key TakeawaysEarly detection is crucial in order to slow down or stop the progression of chronic kidney disease.Lifestyle changes, such as exercise and stress management, play a significant role in managing the disease.Medical management, including medication adherence and understanding potential side effects, is important in stage three of the disease.Severe symptoms in stage four require necessary interventions, and emotional coping and support are essential for patients and their families, during the loss of kidney function. Understanding Chronic Kidney Disease: An OverviewFor More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
Are you dealing with symptoms of kidney disease? Let's straight into understanding what chronic kidney disease is all about.
The history of kidney disease shows a condition where your kidneys, which are integral parts of your body based on the kidney anatomy, can't clean your blood as they should. Over time, this leads to waste build-up which could result in other health complications.
Now, you might wonder how it happens. Here's the thing,while some people have a genetic predisposition to it, others get it due to lifestyle choices and conditions like diabetes or high blood pressure. That's why disease prevention is vital, regular check-ups and maintaining a healthy lifestyle go a long way.
But let's not forget about the emotional impacts of this disease too. The diagnosis can be overwhelming and may cause feelings of confusion or fear. However, remember you're not alone in this journey.
Treatment options vary depending on the stage of the disease. You've got conventional treatments like dialysis or transplantation but don't overlook alternative therapies either which could offer relief from symptoms.
In essence, understanding chronic kidney disease isn't just about knowing its medical implications; it's also about recognizing its emotional aspects and exploring varied treatment paths. These tips can even help if you have a kidney stone or need a kidney biopsy.
If you have any questions about CKD, you can always check what the National Kidney Foundation has to say about the signs of kidney damage and the stages of kidney disease.Â
Unpacking Stage One: Early Detection and Its ImportanceIn the first phase, early detection is crucial because it can slow down or even stop the progression of the condition. As a caregiver or medical professional, you can encourage patients to undergo kidney function tests to assess their renal health. The purpose of these tests is to measure levels of certain substances in your patient's blood and urine.
Risk factors like high blood pressure, diabetes, and a genetic predisposition can increase vulnerability to chronic kidney disease (CKD). Educate your patients about these risks, awareness is a powerful preventive measure, so that you don't reach progression to kidney failure, without being properly informed with the risk of kidney disease. Feel free to get in touch with your healthcare provider about any potential complications that may arise!Â
Here's a table for quick reference:
Risk FactorsPreventive MeasuresHigh blood pressureRegular check-ups & medication managementDiabetesMaintain healthy diet & regular exerciseGenetic predispositionRegular monitoring & lifestyle adjustmentsPatient education on preventive measures such as maintaining a balanced diet and regular exercise routine will help them manage their risk factors better. By identifying symptoms early, you're not just saving one life, but also creating an environment where everyone becomes proactive about their own health.
Let's make CKD less intimidating through information dissemination and empathetic healthcare practices.
Progression to Stage Two: The Role of Lifestyle ChangesYou're now moving onto the next phase, where lifestyle changes play a pivotal role in slowing down the progression of the condition. Exercise benefits your kidney health immensely by reducing blood pressure and aiding glucose metabolism.
On the flip side, smoking impacts negatively on your kidneys. The harmful chemicals damage kidney function, accelerating disease progression.
Alcohol consumption too can be detrimental. It dehydrates you and adds extra burden to your kidneys. Cutting back on alcohol not only aids hydration, but also reduces stress on renal functions.
Speaking of stress management, it's crucial in controlling blood pressure, a significant risk factor for kidney disease. Engage in relaxation techniques like yoga or meditation for maintaining mental well-being.
Hydration is vital as well, remember that adequate water intake helps clear toxins from your body, easing the load off your kidneys.
In short, adopting healthier habits is not just beneficial but necessary when dealing with chronic kidney disease stage two. To serve yourself best and slow this condition's progression further, focus on exercise benefits, reduce smoking impact and alcohol consumption, while managing stress properly and understanding hydration importance.
Navigating Stage Three: The Onset of Symptoms and Medical ManagementAs you navigate through this third phase, it's crucial to pay attention to the onset of symptoms and take a proactive approach towards medical management. Recognizing symptoms early on can make a significant difference. Fatigue, fluid retention, or changes in urination can indicate worsening kidney function.
Effective treatment at this stage often involves medication adherence. It's key that you adhere strictly to your prescribed medications, which could involve:
ACE inhibitors: These reduce blood pressure and protect kidney functions. Make sure to monitor for side effects like dry cough or high potassium levels.Diuretics: They help get rid of excess fluid and lower blood pressure. Watch out for potential dehydration.Erythropoiesis-stimulating agents (ESAs): They combat anemia by encouraging red blood cell production. Keep an eye out for any signs of excessive clotting. Emotional coping plays a vital role in managing chronic kidney disease. Connecting with others in similar situations, seeking mental health support, and practicing relaxation techniques can be beneficial.Equally important is healthcare communication; openly discuss your concerns with your healthcare team. Patient advocacy promotes self-care, by equipping you with the knowledge to actively participate in decision-making about your treatment plan.
There are many markers of kidney damage and markers of kidney disease. It's important that you recognize an abnormal kidney structure when possible. A decrease in kidney function is a red flag to your body and there are many treatment decisions you'll need to make over the next few days, months, and years.Â
Tackling Stage Four: Severe Symptoms and Necessary InterventionsTackling the fourth phase requires dealing with more severe symptoms and necessitates certain interventions. As kidney function significantly drops, you'll grapple with ailments like anemia, acidosis, and hypertension. Emotional coping becomes crucial at this stage, it's important to acknowledge any feelings of fear or anxiety and seek professional help if needed.
Medication adherence is paramount, missing doses or incorrect usage can exacerbate the disease progression. Your nephrologist will likely prescribe a cocktail of drugs to manage your symptoms, anti-hypertensives, erythropoiesis-stimulating agents, or phosphate binders might be part of your regimen. Understanding your medications' role aids in adherence as well as monitoring potential side-effects.
Patient education is vital here - knowing when to seek emergency care or recognizing worsening symptoms can save lives. Family support plays a significant role in ensuring consistent care and emotional wellbeing; they're often your first line of assistance during crises.
Exercise's importance can't be overstated, regular physical activity helps maintain healthy body weight, keeps blood pressure in check, reduces stress levels and boosts overall mood. However, don't overdo it, gentle exercises are beneficial without causing undue strain on your already taxed kidneys.
Stage 5 End Stage Renal DiseaseNavigating the fifth phase, known as End Stage Renal Disease (ESRD), demands even more vigilance and aggressive intervention. By this stage, your kidneys have lost nearly all their ability to do their job effectively. You need a comprehensive understanding of your treatment options and an effective emotional coping strategy.
Treatment OptionsEmotional CopingDialysisTherapy SessionsTransplantationSupport GroupsPalliative CareMeditationDialysis or transplantation become vital for survival. However, transplant eligibility depends on various factors such as age and overall health status. For those ineligible for transplantation or waiting for a donor, dialysis helps keep the body's balance in check.
Emotional coping is equally important at this stage. Therapies can help you deal with the stress associated with ESRD while patient support groups provide a platform to share experiences and gain strength from others going through similar challenges.
Don't forget about financial implications of treatments too, it's crucial to explore insurance coverage and options available to manage costs.
Lastly, if treatments are no longer beneficial or wished-for, palliative care focuses on managing symptoms and improving your quality of life. This isn't giving up, it's choosing comfort over cure when that makes most sense for you.
Dietary Adjustments Needed in Different StagesIt's equally crucial to note the importance of dietary adjustments required throughout the different phases of this journey. As a caregiver or healthcare provider, you'll need to guide your patients in managing their diets as part of their chronic kidney disease (CKD) treatment plan.
You must emphasize phosphorus limitations, as excessive phosphorus can damage the kidneys further. Encourage foods low in phosphorus like fresh fruits and vegetables, rice and pasta while avoiding dairy products, nuts and seeds which are high in phosphorus.
Sodium control is another key area. Excessive sodium can lead to fluid retention and high blood pressure, these are two complications that could exacerbate CKD.
Protein Restriction might seem counterintuitive because protein is essential for body repair and growth but excess protein can strain the kidneys. Opt for plant-based proteins over animal proteins.
Fluid Management is necessary to prevent swelling, shortness of breath, and other complications linked with fluid overload in CKD patients.
Potassium regulation should be implemented because too much potassium can cause irregular heart rhythms dangerous for CKD sufferers.
Your understanding of these dietary adjustments will significantly enhance your patient's quality of life along this challenging journey.
Role of Regular Monitoring in Managing Chronic Kidney DiseaseYou've got to keep a close eye on your patient's health status by regular monitoring, as it plays a crucial role in managing their condition effectively. Monitoring frequency is key in early detection of any progression or complication related to chronic kidney disease (CKD). Patient education is also vital. Here's a simple guide that could be used:
Monitoring FrequencyDiagnostic TestsTreatment AdjustmentsQuarterly reviewBlood pressure checks, serum creatinine testMedication dosages modified based on resultsBi-annual reviewGlomerular filtration rate(GFR) estimationDietary changes recommended based on GFR resultsAnnual reviewComprehensive metabolic panelLifestyle modifications suggestedConnections Between Chronic Health Conditions and Renal DiseaseThere's a significant link between long-term health conditions like hypertension and diabetes, and the development of renal disease. As a healthcare provider, it's crucial for you to understand these connections to aid in comorbidity management.
Diabetes Correlation: Diabetes damages small blood vessels throughout the body. When these vessels in the kidneys are damaged, they can't filter out toxins efficiently, leading to kidney disease.Hypertension Impact: Uncontrolled high blood pressure forces your kidneys to work overtime. This extra strain can lead to kidney failure over time.Heart Disease Link & Obesity's Influence: Both heart diseases and obesity increase the risk of developing kidney diseases, due to increased workload on the kidneys and damage to kidney tissues.By managing these chronic conditions effectively, you're able not only to slow down their progression but also reduce the risk of renal disease development in patients with these conditions.
It's also important to educate patients about lifestyle modifications, such as healthy eating habits and regular exercise that can help manage their conditions better.
Remember, prevention is just as important as treatment when it comes to maintaining long-term health outcomes for your patients!
The Importance of Early Intervention in Kidney DiseaseTransitioning from understanding the link between chronic health conditions and kidney disease, let's look into the crucial role of early intervention in maintaining kidney health.
You see, early diagnosis benefits are manifold. It can slow down disease progression, prevent severe complications, and improve your quality of life. You'll be able to take preventive measures, like dietary modifications and medication management at an earlier stage.
Here's a snapshot of how early diagnosis impacts treatment outcomes:
Early Diagnosis BenefitsLate Diagnosis ConsequencesSlows down disease progressionRapid deterioration of kidney functionPrevents severe complicationsHigh risk for serious health issuesImproves quality of lifeCompromised lifestyle due to illnessGenetic predisposition studies have also gained traction in recent years. These studies help identify those at risk even before symptoms manifest, allowing for proactive prevention strategies.
Community outreach initiatives are key drivers in promoting kidney health awareness. They encourage regular screenings and educate about lifestyle changes that support renal health.
What else comes with poor kidney function?
Irreversible damage to moderate damageKidney replacement therapyAntihypertensive medications Sometimes tubulointerstitial disease, glomerular diseases, Ischemic Nephropathy, and even renal function decline. Treatment Options: Dialysis and Kidney TransplantLet's explore your treatment options, if your condition has progressed beyond early intervention, specifically dialysis and kidney transplant.
When kidneys can't function adequately on their own, dialysis stands as a feasible solution. There are two types: hemodialysis, where blood is filtered out of your body and cleaned before being returned; peritoneal dialysis involves cleaning the blood within your body using a special fluid.
However, dialysis isn't without complications. Long-term use may lead to anemia or weakened bones due to changes in mineral metabolism. Therefore, it's imperative to monitor for these and promptly address any issues that arise.
On the other hand, you might be eligible for a kidney transplant depending on factors such as age, overall health status, and compatibility with potential donors. Ideally, living donors present a higher success rate because of better genetic matching.
Post-transplant care is crucial too. It entails strict adherence to medications that prevent organ rejection and regular check-ups to ensure the new kidney functions properly.
While both treatments have their challenges, understanding them empowers you in making informed decisions about your healthcare journey.
Frequently Asked QuestionsWhat Are the Potential Psychological Impacts of Living With Chronic Kidney Disease?Living with chronic kidney disease can have significant psychological effects. You might experience emotional stress and struggle with disease acceptance.
It's common to face challenges in coping with your condition, which can impact not only your mental health but also the wellbeing of your family. Remember, it's okay to seek help and support as you navigate this journey.
Taking care of your mental health is just as important as managing the physical aspects of your disease.
Chronic kidney disease can seriously impact your fertility and pregnancy. Your kidney health plays a vital role in hormonal balance, which affects fertility.
Pregnancy complications may rise due to high blood pressure or proteinuria caused by your condition. If you're on dialysis, the impact is even greater, making conception tough and pregnancies riskier.
However, with careful management and medical guidance, it's still possible for you to have a successful pregnancy.
Chronic kidney disease can't be completely cured, but it can be managed. Disease prevention is crucial, early detection helps slow its progression.
Kidney transplants are an option if your condition worsens. Alternative treatments, like diet changes and exercise, impact positively on your health too. Whether you're focused on a cardiovascular disease, loss of appetite, or even blood pressure medication, chronic kidney disease can be managed.Â
It's about managing symptoms and enhancing your quality of life. Remember, every person's journey with this disease is different, continuous medical guidance tailors the best approach for you.
Life expectancy with chronic kidney disease varies greatly. You will hear people talk about mild damage and renal failure. It's influenced by factors like age, overall health, and how well you manage your symptoms.
Diagnostic methods help track the disease progression. Dietary changes can slow this down significantly.
Knowing and controlling risk factors is also crucial for longer survival. Remember, a diagnosis isn't a death sentence, it's an opportunity to take control of your health through informed decisions and proactive symptom management.
If you have any specific questions about the history of kidney failure or kidney damage, then make sure you speak to a kidney doctor! Mild kidney damage is a real thing, so you'll want to make sure your blood sugar levels are being monitored as closely as possible.
So, you've learned about the stages of chronic kidney disease and the vital role early detection plays. It's clear that lifestyle changes can slow progression and medical management is key in later stages.
Regular monitoring helps manage this condition, as does understanding how other health issues may impact your kidneys. Early intervention is crucial, with treatments like dialysis or transplant available. if needed.
Remember knowledge is power, stay informed to protect your kidney health. You'll want to make sure you're monitoring for complications, while on a kidney-friendly diet.
The post Stages Of Chronic Kidney Disease appeared first on Renal Diet HQ.
Suggested Reading:
What Is Chronic Kidney DiseaseThe Importance Of Diet For Stage 3 Chronic Kidney DiseaseDiabetic Renal Diet Meal PlanAugust 16, 2023
Questions About Kidney Transplant
You're considering a kidney transplant and you've got questions. That's normal. It's a big decision and understanding the process can be overwhelming.
We've gathered all the crucial information you'll need to navigate this journey effectively. From evaluating eligibility to finding a donor, we'll guide you through every step.
So let's dive in, shed some light on your doubts, and empower you to make informed choices about your health.
[feast_advanced_jump_to] Key TakeawaysKidney transplant is a surgical procedure that replaces a non-functioning or diseased kidney with a healthy one.Eligibility for kidney transplant goes beyond age and medical history, considering physical health, psychological well-being, and support systems.Living and deceased donors are the two main sources of organ donors, and their emotional implications and ethical considerations should be taken into account.Navigating the kidney transplant process involves thorough assessments, understanding waitlisting procedures, and emotional preparation with family support.
Key TakeawaysKidney transplant is a surgical procedure that replaces a non-functioning or diseased kidney with a healthy one.Eligibility for kidney transplant goes beyond age and medical history, considering physical health, psychological well-being, and support systems.Living and deceased donors are the two main sources of organ donors, and their emotional implications and ethical considerations should be taken into account.Navigating the kidney transplant process involves thorough assessments, understanding waitlisting procedures, and emotional preparation with family support.Understanding the Basics of Kidney TransplantFor More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
You're about to dig into the complex and fascinating world of kidney transplant, a surgical procedure that replaces a non-functioning or diseased kidney with a healthy one sourced from a donor.
You'll discover the intricacies of this life-saving operation, understanding not just what it involves but why it's considered such an important medical breakthrough.
Moreover, we'll discuss the different sources of kidney donors, shedding light on the procedures, ethical considerations, and health implications surrounding organ donation.
Defining Kidney TransplantLet's start by understanding what a kidney transplant is. It's essentially when a healthy kidney from one person is placed into the body to take over the work of two failed kidneys.
There are several misconceptions about transplants that you need to dispel. Kidney diseases aren't always caused by lifestyle choices, genetics play a major role.
Recipient's psychological preparation is crucial. It's not just about physical readiness. Transplant legislation exists to ensure ethical and fair distribution of organs.
It's important to understand these facets, not only for potential recipients but also for those who desire to serve this community. Be aware too, of organ trafficking issues, it's an illegal act that exploits vulnerable individuals for profit.
Sources of Kidney DonorsThere are two main sources of organ donors, living and deceased. Donor demographics vary widely, influenced by transplant legislation in each jurisdiction. It's important to understand the emotional implications for both donor types.
Donor TypeLegislation InfluenceEmotional ImplicationsLiving Donor Kidney TransplantsVaries per location; often involves donor remunerationComplex; can involve feelings of altruism, fear, and anxietyDeceased Organ DonorStrictly regulated to prevent unethical organ tradeAffects loved ones left behindEvaluating the Eligibility for a Kidney TransplantIn exploring your path to a possible kidney transplant, it's vital that we consider two key elements, the Health Requirements Assessment and the Eligibility Criteria Discussion.
This is where we'll meticulously assess your overall health status, focusing on pertinent factors such as existing medical conditions, lifestyle habits, and any potential risks involved.
We'll also discuss in detail the specific criteria you must meet to qualify for this life-altering procedure, ensuring you're fully versed in what's expected and what lies ahead.
Health Requirements AssessmentYou'll need to undergo a comprehensive health assessment before you can be considered for a kidney transplant. This evaluation is designed to ensure that you're physically, psychologically, and socially prepared for the procedure and ensuing lifestyle changes.
Your healthcare transplant team will focus on several key factors:
Dietary modifications: You'll need to adhere to strict dietary rules both pre- and post-transplant.Physical activity: Regular exercise helps improve overall health and recovery rate.Psychological impact: It's crucial to understand the emotional toll of transplant surgery, including potential stress, anxiety, or depression.Family support plays a significant role in your journey through patient education sessions. Learning about the process together creates a supportive environment conducive to successful transplantation. Remember, this isn't just about you; it involves everyone close to you too.
Eligibility Criteria DiscussionLet's look into the eligibility criteria that must be met for this life-changing procedure. Contrary to transplant misconceptions, the process is not limited by age or medical history alone. It's a thorough evaluation ensuring both the donor's rights and the recipient's suitability.
Factors like physical health, psychological well-being, and support systems are scrutinized. Transplant coordinators work to manage the process with chronic kidney disease patients.
Understanding transplant legislation is crucial as it governs the ethical conduct of transplantation procedures. You must respect these laws while striving to serve others in need. This includes understanding the ethics around organ donation, it's not just about giving life but respecting each individual involved.
Lastly, don't underestimate the importance of recipient psychological support throughout this process. The emotional toll can be significant, so adequate counseling should be provided, to ease this journey for all parties involved.
The Role of Donors in Kidney TransplantationIn this next discussion, you'll delve into the critical role that kidney donation plays in kidney transplantation. You'll focus on two key areas, identifying potential donors and understanding the differences between living donor kidney transplants and deceased donor kidney transplants.
You'll discover how to effectively pinpoint individuals who could serve as potential life-savers through their donation.
Moreover, you'll gain a comprehensive view of the pros and cons associated with both living and deceased donor transplants. This will allow you to make informed decisions in your practice or research.
Identifying Potential DonorsFinding a suitable kidney donor isn't always easy, but it's an important step in the transplant process. You must consider several factors, when identifying potential donors:
Donor diversity: A diverse donor pool can increase the success rate of transplantation. It's true that some blood types, such as those with type 0 blood can only receive from other type O blood donors. But type O blood kidney transplant donors can give to every other type of blood.Psychological impacts: Understand that donation can have emotional effects on both the donor and recipient. Working with a transplant coordinator and a social worker can help you with the process both financial issues and medical insurance concerns.Family involvement: Families often provide essential support during this process.Ethical considerations are also paramount; you must ensure that donors are not exploited or coerced into donating. Consider international donations, as they expand your options for finding an appropriate match.
Living Vs Deceased DonorsLeaving behind the identification of potential donors, you're now grappling with a complex choice of living vs deceased donors.
Both options come with their unique psychological impacts. Donor emotions can run high in the case of living donors, often involving family members who feel a moral obligation to help. This family involvement sometimes leads to recipient guilt, as they might feel burdened by the sacrifice their loved ones are making.
On the other hand, choosing a deceased donor brings its own societal perceptions and challenges that require careful consideration and emotional preparedness. Â
Navigating the Process of Getting a Kidney TransplantNavigating your way through the process of getting a kidney transplant, but understanding key procedures such as Transplant Center Evaluation and Transplant Waitlisting Procedure can make all the difference. Being on the transplant list can take several months and years to be qualified for people with kidney failure and those on the waiting list may also wait several years for a transplanted organ.
When you're evaluated by a transplant center, they will examine your overall health, potential risks, and ability to adhere to post-transplant care. It's critical that you know what's involved.
Understanding how the waitlisting procedure works is important, from how priority is determined to what factors might affect your waiting time, this can equip you with the knowledge needed to navigate this complex journey.
Transplant Center EvaluationYou'll undergo a thorough evaluation at the transplant center to determine if you're a suitable candidate for kidney transplant. Center selection is critical, because it ensures it has proper Transplant Center Accreditation.
The transplant team, consisting of surgeons, kidney doctors, financial coordinators, and transplant coordinators, will guide this complex process. Kidney transplant recipients are carefully screened for eligibility and ability to tolerate the surgery as well as recovery.
Pre-Evaluation Preparations: These include medical history review and comprehensive physical examination. When your kidneys start to fail, you might develop high blood pressure and coronary artery disease which can affect your other organs. Evaluation Duration: This varies but typically lasts several hours to a few days. Post-Evaluation Follow-up: Based on your evaluation results, your eligibility is determined. Your medical treatment will continue whether it's with ongoing medical tests or continued dialysis treatment for end-stage kidney disease.Remember that serving others starts with taking care of yourself first. So be prepared for this life-changing decision, by understanding each element from center selection to post-evaluation follow-ups.
Your courage and strength are commendable as you embark on this journey towards improved health and well-being.  Your long term survival and life expectancy is much better for CKD if you are a transplant candidate who receives a kidney.Â
Transplant Waitlisting ProcedureAfter your evaluation at the transplant center, you're now ready to tackle waitlist challenges. The complexity of the waitlist procedure requires a solid foundation in transplant education. You need to understand how organs are allocated and stay updated on your status.
It's not just about waiting, it's also about emotional preparation for what lies ahead. Dealing with anticipation, anxiety, and at times, disappointment can be hard, which is why family involvement is crucial during this period. Having your loved ones by your side can provide invaluable comfort and support.
The Financial Aspect of Kidney TransplantationYou're about to explore the complexities of insurance coverage for transplants, a vital aspect often overlooked in the transplant journey. Understanding your policy's details isn't just necessary pre-transplant. It's crucial to familiarize yourself with post-transplant financial responsibilities as well.
Insurance Coverage for TransplantsIt's important to understand that insurance coverage for kidney transplants can vary greatly depending on your specific plan.
Insurance exclusions: Some plans may exclude certain transplant-related expenses, such as post-operative medication or home health care. You will require a lifetime of anti-rejection medications and have additional immunosuppressive medications that will involve recovery time and regular checkups.Policy limitations: Your policy might have a cap on the total cost it will cover for a transplant. Your follow up medical care can be extensive and working on other medical issues will also be important to manage your new kidney!Transplant specific policies: Certain policies offer specialized coverage for transplants, which could potentially reduce out of pocket costs. Working with a financial coordinator can help a great deal with navigating the process.You'll need to carefully review your policy's details and consult with your insurer directly if you encounter any confusion. In cases where coverage is denied or limited, remember you have options through the insurance appeal process.
Being well-informed will help you navigate these financial waters with confidence and ease in serving others going through similar situations.
Post-Transplant Financial ResponsibilitiesAfter examining insurance coverage for kidney transplants, let's now shift our focus to your post-transplant financial responsibilities. It's crucial to understand that the transplant process and the subsequent care involve significant costs.
To manage these expenses effectively, you'll benefit from financial counseling. This guidance can help you develop practical cost management strategies which may include exploring fundraising initiatives for medical bills or searching for grant opportunities.
Furthermore, don't overlook your employer benefits, they may offer resources that alleviate some of these financial pressures. Remember, securing your financial health is as essential as physical health in this journey.
Embracing Life Post-Transplant: Care and MaintenanceYou've successfully navigated the kidney transplant process, but your journey doesn't end there. It's crucial that you understand how to manage your post-transplant medication regimen to maintain the health and longevity of your new organ. Â
You'll need to adapt to lifestyle changes post-transplant. These changes may involve adjustments in diet, exercise, and overall wellness strategies. All of these elements are critical in ensuring a successful transition into this next phase of your life.
Post-Transplant Medication ManagementManaging your medications post-transplant is crucial to ensure your new kidney functions properly. Medication adherence isn't just about taking your medicine on time; it's also understanding the importance of anti-rejection medicines and immunosuppressive medicines in preventing rejection, managing side effects, and avoiding drug interactions.
Here are a few things to remember:
Regular medication reviews: Routine check-ins with your healthcare provider can help adjust dosages and manage any potential side effects.Drug interaction prevention: Be aware of how other medications or supplements could interact with your transplant medications.Immunosuppressant importance: Never skip these drugs as they're essential in ensuring your body accepts the new kidney. Health professionals can guide you on using generic medicines and antirejection medicines to ensure you are able to afford your medications.Your diligent efforts will contribute significantly to maintaining optimal health and longevity for your transplanted kidney.
Lifestyle Changes Post-TransplantYour new exercise regimen should ideally encompass both cardiovascular workouts and strength training. This not only bolsters your physical strength but enhances your mental wellness too.
Nutritional adjustments are necessary as well, you'll need to focus on protein-rich foods while limiting sodium and cholesterol.  Frequent checkups with your kidney care team and kidney doctor will be a key to continued health.
Equally important are social relationships that provide emotional support during this transformative phase. Don't isolate yourself, engage in meaningful interactions with family, friends or support groups.
Career implications should also be considered. You might need to make adjustments at work, such as reducing hours or modifying tasks initially post-transplant. Remember, your health is paramount when it comes to kidney transplant surgery.Â
Strategies for Finding a Suitable Kidney DonorYou're now stepping into the next phase of your journey, finding a suitable kidney donor candidate.
It's crucial to develop effective strategies for donor searching, and understanding how to navigate online donor communities can play a significant role in this process.
Let's delve deeper into these topics, examining various techniques and digital platforms that'll help streamline your search, connecting you with potential donors more efficiently and effectively.
Donor Searching StrategiesFinding the right kidney donor candidate can be a challenging process, but there are various strategies you can use to increase your chances. Here are some key factors:
Donor Motivation: Understand what motivates people to donate. Often, it's an altruistic desire to help others.Transplant Legislation: Familiarize yourself with local and global transplantation laws. Certain countries have more lenient rules that may favor your situation.Ethical Considerations: Always consider the ethics of transplant tourism. It's crucial to ensure any organ donation is legal and consensual.By focusing on these areas, you can navigate through the complexities of finding a suitable donor while respecting ethical considerations and transplant legislation. Â
Online Donor CommunitiesHaving explored donor searching strategies, let's navigate the landscape of online donor communities.
You'll find that digital outreach is key in fostering community engagement and driving donor motivation. These platforms provide a safe space for individuals to connect, share experiences, and encourage potential donors. Finding a kidney donor isn't easy but transplant patients can have a positive experience.Â
Nonetheless, online safety should be your top priority. Be cautious about sharing personal information and verify the credibility of users before engaging further.
Ethical considerations are also crucial. Ensure transparency in all interactions and respect everyone's privacy rights within these digital spaces.
The Crucial Evaluation Process for a Kidney TransplantDelve into the complex intricacies of the kidney transplant evaluation process, you'll find yourself navigating through a series of carefully designed steps. These are not merely procedural checkpoints. Each one plays a pivotal role in determining donor compatibility, an aspect that's absolutely essential for a successful transplant.
In this technical discussion, we'll explore these critical steps and highlight how they contribute to establishing a match between you and your prospective donor.
Evaluation Process StepsYou'll need to undergo several tests during the evaluation process for a kidney transplant. These tests are designed not just to assess your physical fitness, but also your psychological readiness. Ensuring that you're mentally prepared for the changes and challenges ahead.
Psychological Readiness: This ensures you're emotionally stable and have a robust support network in place.Transplant Legality: It's essential to verify that the donor organ is obtained legally, following stringent transplant ethics.Donor Counseling & Recipient Support: Both parties receive thorough counselingâdonors about potential risks, recipients about post-transplant care.Determining Donor CompatibilityHaving just navigated the evaluation process, you're now moving into a critical phase. This phase focuses on determining donor compatibility. This involves meticulous steps to ensure safety and success.
Donor communication, psychological readiness, ethical considerations, blood type matching, and genetic screening, with all of these in mind, your quality of life can be amazing! There are incompatible blood types such as type O blood that cannot accept a kidney from anyone other than someone with type O blood.
Open and honest donor communication is vital. It's important that both parties are psychologically ready for this life-altering decision. Ethical considerations also play a massive role, informed consent must be secured.
Then comes the scientific part, blood type matching and genetic screening. These tests ensure that your body won't reject the donated kidney.
ProcessImportanceBlood Type MatchesPrevents RejectionGenetic ScreeningDetects Disease RisksWhat to Expect During Kidney Transplant SurgeryYou're now stepping into a critical phase of your kidney transplant journey, the surgery itself.
It's important to understand both the duration and intricate process this surgical procedure encompasses, as well as what you can expect during the post-surgery recovery period.
Armed with this knowledge, you'll be better prepared for what lies ahead and can actively contribute to a successful outcome. The kidney transplant program will work with you as part of the transplant hospitals goal to make sure you are well taken care of and ensure your adequate kidney function returns.
Surgery Duration and ProcessIt's important to note that the duration of kidney transplant surgery typically ranges from 3 to 4 hours. As a person committed to serving others, you should be aware of several aspects involved in this procedure:
Patient preparation: This involves pre-operative tests and procedural clarifications.Family involvement: It's vital for emotional support and understanding the post-surgery care.Anesthesia risks: All surgeries carry some risk, including reactions to anesthesia.Knowledge of possible surgical complications can help you better assist patients. Post surgery complications may include infection or rejection of the new kidney. By understanding these details, you're well-positioned to provide comprehensive care and support during this crucial time.
Post-Surgery Recovery PeriodPost-surgery recovery period's length can vary, but patients typically spend several days in the hospital followed by a few weeks of close monitoring at home. During this time, you'll engage in rehabilitation exercises to restore strength and mobility. Emotional support is vital for psychological adjustment, don't hesitate to reach out to trusted individuals or professional counselors.
Dietary modifications are also necessary post-surgery to promote healing and kidney function. Wound care is another crucial aspect as proper attention ensures infection prevention.
Key AspectImportanceRehabilitation ExercisesRestores strength and mobilityEmotional Support & Psychological AdjustmentFacilitates coping with changesDietary Modifications & Wound CarePromotes healing and prevents infectionsRemember, each person's recovery journey is unique; patience and perseverance are key elements in your post-surgery phase.
The Risks, Complications, and Lifestyle Changes After a Kidney TransplantNavigating the post-transplant landscape can be a complex endeavor, and it's crucial you're well-informed about the necessary lifestyle modifications and risk management strategies.
You'll need to grapple with significant alterations in your daily routines, dietary habits, exercise regimen, medication schedules, among others as part of your journey towards optimal recovery.
Equally important is understanding how to effectively manage potential risks associated with kidney transplantation. From common complications like infection or organ rejection to more intricate issues, such as transplant-related malignancies or cardiovascular disease.
Post-Transplant Lifestyle ChangesYou'll need to make some major lifestyle changes after your kidney transplant to ensure the success of the operation. These modifications are not just physical but also impact your dietary patterns, mental health, and social interactions.
Dietary adjustments: You must maintain a balanced diet. Nutrient-rich foods aid in healing and maintaining kidney function.Mental health: It's crucial to manage stress effectively. Participate in mindfulness exercises or therapy sessions for emotional well-being.Physical activity: Regular exercise promotes overall health. Start with light activities and gradually increase intensity under medical guidance.Remember, regular routine check-ups are key to monitor your progress post-transplant. Embrace these changes as stepping stones towards a healthier life rather than viewing them as restrictions.
The service you're providing yourself is invaluable!
Managing Transplant RisksManaging potential risks after the operation is a crucial part of ensuring its long-term success. You'll need to monitor closely for signs of transplant rejections, such as fever or pain in the area of the kidney.
Practicing diligent infection prevention is key; you should wash your hands regularly, avoid large crowds and those who're sick, and keep your vaccination schedule up-to-date.
Dietary adjustments are also necessary, opt for low-sodium, kidney-friendly foods while reducing alcohol intake. The psychological impact shouldn't be undermined; rather, seek support if you're feeling anxious or depressed post-transplant.
Incorporating exercise post-transplant into your daily routine can help improve physical strength and mood stability too. Managing these risks helps secure a successful recovery.
Frequently Asked QuestionsHow Does the Emotional Wellbeing of a Patient Impact the Success of a Kidney Transplant?Your emotional well being significantly impacts the success of a kidney transplant. High stress levels can impair your body's ability to heal and accept the new organ.
Emotional resilience, coping mechanisms, and solid patient support are crucial for mental health maintenance during this time.
It's essential to manage stress effectively and maintain positive mental health as it directly affects your recovery trajectory post-operation.
If a kidney transplant isn't in the cards for you, don't lose hope. There are other options you can explore.
Dialysis is often effective, taking over some functions of healthy kidneys.
Recent stem cell research offers promising alternatives.
Immunotherapy has potential too, as it uses your body's immune system to fight disease.
Also, consider lifestyle modifications: healthier eating and regular exercise can do wonders for kidney health.
After a kidney transplant, you're free to travel, but with some precautions. Your travel preparations should include proper medication management.
Always carry a sufficient supply of your meds and know how to store them. Consider purchasing travel insurance that covers any health emergencies abroad.
Destination considerations are also vital. Avoid places with a high risk of infection. Post-transplant activity should be moderate, nothing too strenuous that might endanger your new organ's function.
The transplant process can greatly impact both the patient's and donor's family. Financial implications may arise from medical costs, potentially straining family resources. If a sibling is the donor, psychological adjustments might be necessary to manage fear or guilt.
Caregiver stress is another concern as loved ones juggle responsibilities and emotions. The need for open, clear communication within the family becomes paramount to deal with these challenges effectively and support each other through this demanding experience.
Kidney transplantation may seem complex, but it's a life-saving procedure. You've learned about eligibility, donor importance, the process itself, financial aspects, and finding a suitable donor.
You've also understood the evaluation procedure, surgery expectations, and post-transplant life. It's crucial to stay informed and proactive throughout your journey for better outcomes. Remember, knowledge is power when navigating through this transformative health decision.
The post Questions About Kidney Transplant appeared first on Renal Diet HQ.
Suggested Reading:
ESRD PrognosisWhat Is Chronic Kidney DiseaseHow Does Kidney Failure Affect the BodyAugust 15, 2023
Avoid Caregiver Burnout

You're a caregiver, tirelessly dedicating your time and energy to others. But are you taking care of yourself? Caregiver burnout is real and can sneak up on you, if you're not cautious. Sometimes the responsibilities of caregiving are warning signs to help you avoid caregiver burnout.
It's crucial to recognize the signs, understand what causes it, and learn how to avoid it. Let's empower you with knowledge and resources to keep giving your best without compromising your well-being.
Remember, you can't pour from an empty cup, so set reasonable expectations for yourself and the person you're caring for!
[feast_advanced_jump_to]Key TakeawaysCaregiver burnout is a state of physical, emotional, and mental exhaustion experienced by professional caregivers. Making sure you have access to helpful resources and internal resources if super important! Symptoms and triggers of caregiver burnout include emotional exhaustion, physical fatigue, feeling overwhelmed, lack of resources or support, and isolation.Role confusion and burnout can have a negative impact on caregivers and patients, including strained relationships, increased burden on the healthcare system, and reduced quality of care.Self-care techniques, such as regular exercise, meditation, respite, and prioritizing oneself, are essential in avoiding caregiver burnout. The stress of caregiving can take a toll on you, so make sure you have access to community resources! Understanding the Concept of Caregiver BurnoutYou're not alone if you're feeling overwhelmed and exhausted as a caregiver; this is often referred to as caregiver burnout.
It's important to understand what it means to experience burnout, including its causes and symptoms, so you can recognize the signs early on.
Let's get into defining caregiver burnout and exploring the factors that contribute to its onset. Providing you with valuable knowledge for maintaining your well-being, while caring for others.
Some signs of caregiver burnout can be hard to recognize, so keep reading to learn more.
Defining Caregiver BurnoutFor More Recipes and Ideas --->> Get Your Free Meals and Recipes That Are Perfect for Pre-Dialysis Diets, Pre-Dialysis with Diabetes, or Dialysis Diets.
It's important to understand what caregiver burnout is in order to prevent it. As a professional caregiver, you're susceptible to this state of physical, emotional, and mental exhaustion. Burnout prevalence is high, due to the constant demands of caregiving.
Burnout research can provide practical strategies for prevention.Burnout mitigation involves self-care routines and establishing boundaries.Seeking support from colleagues or therapy may aid in burnout recovery.Remember that it's okay to ask for help when needed. Regular breaks can reduce stress levels significantly.
Causes of BurnoutLong hours, high demands, and lack of support often lead to this debilitating state. Financial stressors may exacerbate the situation, stretching your resources thin, while pushing you towards burnout. You're doing vital work, but compassion fatigue can creep in subtly, coupled with caregiver guilt over feeling overwhelmed or not doing enough.
Inadequate training can heighten these feelings. You're expected to provide care that you haven't been fully prepared for, it's a tough spot to be in. But remember, seeking help isn't a sign of weakness. Therapeutic interventions exist for precisely these moments, which is a lifeline when the burden feels too heavy.
Reach out to professionals who understand your struggle and can offer guidance on managing this challenging journey with resilience and self-care practices.
It's easy to name the causes and sign of burnout and here they are:
Sleep deprivationStressful situationsUnrealistic expectationsNo access to respite care Challenges of caregivingNever ending medical conditions Lack of concentration Missing daily relaxationHeavy to-do list that is never doneMissing out on doing familiar tasks. Many emotional signsChronic stress and avoiding the signs of stress.How to help avoid burnout:
Adequate sleep Doing daily activities you enjoyComplete simple daily tasksCheck into adult day care programs Identifying Symptoms of Caregiver BurnoutAs you navigate the challenging path of caregiving, it's essential to understand and recognize when you're nearing burnout. Identifying emotional exhaustion signs can often be tricky as they're not always immediately apparent, but knowing what to look for can make a difference in your well-being.
Similarly, being aware of physical fatigue indicators is equally important. These symptoms often manifest earlier and are a clear signal that you need to step back and take care of yourself.
Recognizing Emotional Exhaustion SignsYou're likely feeling emotionally drained if you're constantly irritated, losing interest in activities you once enjoyed, or experiencing persistent sadness. These are signs of emotional exhaustion, a state often experienced by those serving others.
To tackle this, consider the following:
Implementing effective stress management techniques.Recognizing and treating compassion fatigue, a common consequence of helping others in distress.Practicing firm boundary setting to prevent overextending yourself.Adopting a stance of healthy detachment, allowing space between yourself and the emotional turmoil of others. Don't overlook the benefit of utilizing respite care services, these give you a necessary break to rejuvenate, while ensuring your loved one continues receiving quality care.Role of Mental Health ProfessionalsIn maintaining your well-being as a caregiver, it's essential to seek help from mental health professionals and social workers. They offer therapeutic interventions tailored for you, aiding in managing stressors and emotional fatigue.
Mental health professionals ensure:
Upholding professional boundaries: They respect your personal space and privacy.Tackling mental health stigma: By promoting open conversations, they break down barriers associated with seeking help.Ensuring patient confidentiality: Your shared experiences remain confidential.Resolving ethical dilemmas: They provide guidance during morally complex situations.Creating personalized coping strategies: Techniques are designed based on your unique circumstances.They provide resources for caregivers and can act as a community resource finder for you and your family.Don't let the fear of crossing professional boundaries or being stigmatized deter you. Remember, it's not just about providing care for others, it's also about taking care of yourself. Your caregiving responsibilities are an important part of your life, but so is self care.
Utilizing Respite Care ServicesRespite care services can be a lifesaver when you're feeling overwhelmed, offering temporary relief so you can recharge and continue providing quality support. Recognizing respite care benefits is the first step towards self-care; it allows for mental rejuvenation and reduces burnout.
Scheduling respite care might seem challenging, but it's important to prioritize your well-being consistently. Navigate the financial aspects by exploring insurance policies or grants that subsidize these services. It's crucial to remember that investing in your health now prevents costly complications later. Your healthcare provider can assist with this.
However, there are challenges with respite care such as locating trustworthy providers, avoiding bad caregivers, and working with insurance plans. As the primary caregiver, you can end up dealing with feelings of guilt. That's where choosing an appropriate service comes into play. Ensure their values align with your caregiving philosophy, enabling you to relax knowing your loved one is in capable hands.
What services are available for the older generation? Keep this list handy!
Mental Healthcare Professional, Professional Advice, and Medical AdviceSenior centersAdvance Care Planning (Take Advantage of Care Services)Adult Day Care Facilities and Access to Respite Care Nursing homes, adult daycare centers, contact a family care navigatorWhether you need help with your caregiving, or need to talk with caregiving experts, there are plenty of additional resources that you can access. As you can see there is a major advantage of respite care. Caregiving services and adult day care centers can be hard to find, but they are worth it!
Importance of Emotional Support in CaregivingYou're not alone in the challenges you face as a caregiver, emotional support can play an indispensable role in maintaining high quality care. Whether this support comes from friends, family, or professional services, it's essential to recognize its profound impact on your caregiving journey.
Let's delve into how various sources of emotional support can not only bolster your resilience but also significantly enhance the quality of care you provide.
Emotional Support SourcesFinding emotional support is crucial for caregivers to avoid burnout and maintain a healthy mindset. There are a variety of resources available that caregivers can tap into for support, ensuring their emotional wellness stays intact.
Consider these avenues:
Peer Counseling: Build relationships with others who understand your journey and can provide support.Support Groups: Share experiences and gather strength from others who are in similar situations.Online Forums: Connect with diverse caregivers worldwide, contributing valuable insights around the clock.Emotional Wellness Training: Learn strategies to better manage stress and maintain a positive outlook.Therapeutic Activities: Indulge in hobbies or activities that refresh you mentally and physically.Effects on Caregiving QualityHaving explored the importance of emotional support sources, let's now consider how burnout impacts the quality of your caregiving.
Burnout prevention is critical because when you're stressed and exhausted, it's challenging to deliver consistent, high-quality care. Stress management techniques can help preserve your caregiver resilience, keeping you strong in the face of demanding circumstances.
Coping strategies like mindfulness, self-care routines, or seeking professional guidance can be invaluable tools to maintain balance. Developing emotional intelligence also plays a pivotal role. By understanding and managing your emotions better, you can prevent feelings of overwhelm from affecting your ability to serve others effectively.
Remember that taking care of yourself isn't just about personal well-being; it's an essential part of ensuring that those in your care receive the best support possible.
Utilizing Resources to Help Combat BurnoutIn your journey as a caregiver, it's crucial to not only identify supportive resources but also understand how to utilize them effectively.
It can feel overwhelming at times, but remember, you're not alone and there are numerous resources designed to support and guide you.
Identifying what help is out there for you and learning how best to tap into it. Taking care of yourself is just as important as the caregiving you provide.
Identifying Supportive ResourcesYou'll need to know about the various supportive resources available to help manage caregiver stress. Understand that it's not selfish to seek help, it's vital for your wellbeing and those you're caring for. Here are some key resources:
Community Assistance: Local services like meal delivery, grocery shopping, meals on wheels, transportation, or home health care are often available.Caregiver Training: Learning new skills can make caregiving tasks less stressful and more manageable.Financial Aid: Programs exist that provide monetary support for caregivers.Legal Support: Navigating legal matters can be tricky. Seek out professionals who specialize in elder law or disability rights.Support Groups: Connecting with others experiencing similar challenges can offer emotional relief and practical advice.Effective Resource UtilizationHaving identified supportive resources, you're now prepared to step into the arena of effective resource utilization. It's not just about knowing what's available, but how best to use them.
Your caregiving journey can be significantly eased by skillful financial management, meticulous scheduling, and active community involvement. Don't hesitate to seek legal assistance when needed and continually update your skills through training programs.
Physical Fatigue IndicatorsPhysical fatigue indicators, such as frequent headaches or a constant feeling of tiredness, might be telling you it's time for a break. It's crucial to respect these signs and prioritize self-care in your routine.
Establishing regular exercise routines can energize you and improve your mood. A healthy diet nourishes your body, providing the necessary fuel to continue serving others effectively.
Never underestimate the importance of sleep; it is during this rest that your body recovers from daily stressors. Hydration is equally significant; keep drinking water throughout the day to maintain optimum functioning.
Lastly, effective stress management techniques are essential tools you should have in your arsenal. They're not just buzzwords, but vital practices that help prevent caregiver burnout by keeping both physical exhaustion and emotional fatigue at bay.
Recognizing the Causes of Caregiver BurnoutUnderstanding what triggers caregiver burnout is a crucial step in your journey to maintaining emotional health. It's apparent that role confusion can significantly contribute to stress levels, making it a key area of focus.
Let's get deeper into identifying these triggers and understanding the impact of role confusion, providing you with the tools necessary to navigate these challenges effectively.
Identifying Burnout TriggersIt's crucial to pinpoint what specifically causes your feelings of exhaustion and stress in order to effectively manage caregiver burnout. Identifying these triggers is key for Burnout Prevention and Stress Management.
You might feel overwhelmed by the amount of care your loved one needs.Perhaps you're frustrated with a lack of resources or support.Maybe it's the emotional toll of seeing someone you love suffer.It could be isolation, feeling like no one understands what you're going through.Or possibly, it's the physical demands of caregiving causing fatigue.Role Confusion's ImpactHaving identified your burnout triggers, let's now talk about the impact of role confusion and role reversal.
It is common to face challenges when assuming the role of a caregiver. Taking on the role of a caregiver can sometimes blur the lines between being a friend, spouse, and child. Role identification holds significant importance in this context. Understanding and acknowledging each individual's role contributes to maintaining balanced relationship dynamics.
Effective communication is vital in managing these dynamics. Openly discussing fears, expectations, and responsibilities can lessen misunderstandings and facilitate role transitions.
Remember, it's okay to feel unsettled due to role reversal, it's a significant change after all! Coping strategies such as seeking professional guidance or joining support groups can provide comfort during this transition.
Your journey is challenging but remember, you're not alone.
Evaluating the Impact of Caregiver BurnoutUnderstanding the effects of caregiver burnout is crucial, not only for your own wellbeing but also for those you're caring for. It's essential to recognize how this form of emotional exhaustion can impact both you as the caregiver and your patient. It can influence the quality of care and overall health outcomes.
In our discussion, we'll delve into these effects, providing a comprehensive look at why mitigating burnout should be an integral part of any caregiving strategy.
Burnout's Effects on CaregiversBurnout's effects on caregivers can't be understated, often leading to physical and emotional exhaustion. It's crucial to understand the depth of its impact:
Burnout's prevalence: It's widespread among caregivers due to demanding circumstances.Psychological impact: Stress, anxiety, depression are common outcomes.Financial implications: Caregivers may encounter financial strain due to missed work or medical expenses.Caregiver attrition: High burnout rates can lead to caregiver shortage.Societal ramifications: The community suffers when caregivers are less effective due to burnout.You're not alone in this struggle. Recognizing these factors is a step towards addressing them. Remember, caring for yourself isn't a luxury, it's a necessity for you and those who depend on you.
Burnout Impact on PatientsAs we've discussed, caregiver burnout significantly impacts you as a service provider.
Now let's shift our focus to its influence the patient. Burnout consequences can lead to patient neglect, not out of indifference, but because of your neglected self-care and reduced capacity to perform at your best.
This often incurs patient dissatisfaction and may also increase the risk of treatment errors. It's crucial for you to understand that your well-being ties directly into the quality of care provided to patients; their welfare is intrinsically linked with yours.
The Importance of RespiteDon't underestimate the importance of respite. Itâs your chance to recharge and regain balance in your life. The benefits are numerous - from stress management to personal growth.
By stepping away momentarily from caregiving duties, you give yourself a breather for leisure activities or pursuing caregiver hobbies that uniquely interest you.
Respite also allows space for reflection, fostering emotional resilience and enabling you to return with renewed vigor. It's like hitting a reset button! You're not just serving others more effectively, but also nourishing your own wellbeing.
Practical Strategies to Prevent Caregiver BurnoutAs you navigate the challenging terrain of caregiving, prioritizing self-care and learning to delegate tasks effectively can transform your experience. You're not alone in this journey, it's crucial to remember that taking care of yourself is not a luxury, but a necessity.
Self-Care TechniquesPracticing self-care techniques, like regular exercise and meditation, can help you manage stress and avoid caregiver burnout. It's not easy to balance your needs with those of others. Being mindful of your well-being is vital in serving others effectively.
Here are some self-care strategies that you can incorporate:
Mindful Meditation: Taking time daily to clear your mind effectively lowers stress.Physical Exercise: Regular workout boosts mood and energy levels.Nutritional Habits: Eating balanced meals fuels the body for demanding tasks.Therapeutic Hobbies: Engaging in activities you love provides an outlet for tension.Setting Boundaries: Knowing when to say no prevents exhaustion.Effective Task DelegationYou'll find that effective task delegation can greatly ease your workload and reduce stress levels. Delegation techniques are not innate, they require caregiver training, which focuses on time management and setting personal boundaries. It's essential to recognize when you're overwhelmed and need to delegate tasks to others.
Task automation is another tool in your arsenal, allowing you to dedicate more of your precious time towards direct care. This might involve using technology for medication reminders or scheduling appointments, freeing up mental space for other pressing issues.
As a caregiver desiring to serve others effectively, it's crucial that you balance responsibility with self-care. Remember, setting personal boundaries isn't selfish, it promotes sustainability in your role. Your wellbeing directly affects the quality of care provided, never forget that.
Seeking Professional Help for Caregiver BurnoutYou're not alone in this journey, and recognizing when to seek professional help is crucial. Mental health professionals play an invaluable role in providing tools and strategies to manage stress, maintain emotional balance, and prevent caregiver burnout.
These are tools for your journey. Use them wisely to serve your loved ones better, while also looking after yourself.
Making Recovery From Burnout a PriorityYou're not alone in this journey of recovery from burnout. It's essential to prioritize self-care techniques and make full use of support resources available to you.
Itâs vital to talk about aspects that not only promote your well-being, but also ensure a more balanced and sustainable lifestyle moving forward.
Self-Care TechniquesIt's essential to incorporate self-care techniques into your routine to prevent burnout as a caregiver. By putting yourself first, you're better equipped to serve others. That's where meditation benefits, establishing an exercise routine, healthy eating habits, mindfulness practice, and stress management come in.
Consider these five self-care strategies:
Meditation Benefits: Daily meditation helps manage anxiety and promotes mental clarity.Exercise Routine: Regular physical activity boosts mood and energy levels.Healthy Eating: Nutritious meals fuel your body for the demands of caregiving.Mindfulness Practice: Stay present; it'll help balance emotional health.Stress Management: Incorporate relaxation techniques like deep breathing or yoga.Utilizing Support ResourcesHaving explored self-care techniques, let's now focus on utilizing support resources.
You're not alone in your caregiving journey; there are support groups ready to provide emotional comfort and practical insights. They're a safe space to share experiences and learn from others facing similar challenges.
Financial assistance is available too, easing the burden of care-related costs. Look into online resources that can guide you in navigating these options.
Remember also to engage in therapeutic activities that rejuvenate your spirit and reinforce your resilience. Take advantage of art therapy or mindfulness exercises available online. These self-compassion practices will help you treat yourself with kindness amidst stress.
Never underestimate the power of connection and community in this journey; they're crucial for avoiding caregiver burnout.
Frequently Asked QuestionsWhat Financial Support Is Available for Caregivers Experiencing Burnout?You're seeking financial support as a caregiver, right? You've got options.
Government subsidies and social security benefits could be available to you. Insurance may offer some benefits too. If your patient is a Veteran in the US, you could be eligible for respite care. Ask your provider for more information.
Don't forget to explore non-profit grants designed for caregivers in your situation. Also, check if you qualify for caregiver tax credits which can ease the financial burden significantly.
Just remember, it's important to fully investigate each option to find what best supports your unique circumstances.
Yes, certain exercises can help alleviate stress and improve your mental health.
Mindful meditation focuses on breathing and being present, which can calm your mind.
Stress yoga targets tension hotspots in the body.
Aerobic exercises like jogging or swimming boost endorphins, lifting your mood.
Nature walks provide a peaceful setting for relaxation.
Therapeutic massages relieve muscle tension, aiding in physical and emotional relief.
These activities aren't just good for you physically; they also help maintain overall well-being.
To support caregivers, you as a community member can offer your time through volunteering. This provides much-needed respite care and gives caregivers a chance to recharge.
Consider advocating for emotional counseling services and caregiver education programs in your area. These not only equip caregivers with necessary skills but also provide emotional support.
Lastly, help foster social networks where caregivers can share experiences and advice, it's crucial they don't feel alone in their journey.
Yes, caregiver burnout can certainly lead to long-term health issues. When you're constantly stressed and not managing it effectively, both your mental and physical health can suffer.
Recognizing burnout symptoms early is crucial. Prioritize self-care because it's not just important, it's essential for your wellbeing.
You're not alone in feeling overwhelmed as a caregiver. It's crucial to recognize burnout symptoms early, seek professional help if needed, and prioritize self-care.
Your emotional well-being matters too, so don't hesitate to lean on your support system. Utilize resources available to you and remember, recovering from burnout is not just important, it's essential.
You can't pour from an empty cup, caring for yourself is the first step towards caring for others effectively.
The post Avoid Caregiver Burnout appeared first on Renal Diet HQ.
Suggested Reading:
Diabetic Renal Diet Meal PlanImprove My Stage of CKDAvoid Kidney Failure with Dietary Changes


