Margaret McCartney's Blog, page 4
January 9, 2013
Tweets from the emergency department
Free link to BMJ medicine and the media article
January 8, 2013
Inside health references 8/1/13
Dementia screening
I would highly recommend these films by Dr Peter Gordon, a psychiatrist in Scotland
References I used are here
UK National Screening Committee, The UK NSC policy on Alzheimer’s Disease screening in adults http://www.screening.nhs.uk/alzheimers
Screening for Dementia in Primary Care: A Summary of the Evidence for the US Preventive Services Task Force Ann Intern Med 2003;138: 927–937.
http://www.uspreventiveservicestaskforce.org/3rduspstf/dementia/dementsum.pdf
Screening for mild cognitive impairment: a systematic review, Lonie, Tierney, Ebmeier International Journal of Geriatric Psychiatry
This was a recent joint letter to the BMJ
Open letter to the Prime Minister and the Chief Medical Officer Regarding Proposals to Introduce Screening for Dementia BMJ, Rapid Response,14/12/12
http://www.bmj.com/content/344/bmj.e2347/rr/620234
Inside health references 8/1/12
Health Literacy
http://www.lsbu.ac.uk/news-php/news.p... (Please note: this study is not yet published, and used inferences – i.e. it did not directly test the literature in terms of people’s understanding, but instead worked out reading ages of material and compared to surveyed reading ages in population)
http://www.bmj.com/content/344/bmj.e1602
http://www.plosone.org/article/info%3...
http://europepmc.org/articles/PMC3444...
Dementia screening
I would highly recommend these films by Dr Peter Gordon, a psychiatrist in Scotland
References I used are here
UK National Screening Committee, The UK NSC policy on Alzheimer’s Disease screening in adults http://www.screening.nhs.uk/alzheimers
Screening for Dementia in Primary Care: A Summary of the Evidence for the US Preventive Services Task Force Ann Intern Med 2003;138: 927–937.
http://www.uspreventiveservicestaskforce.org/3rduspstf/dementia/dementsum.pdf
Screening for mild cognitive impairment: a systematic review, Lonie, Tierney, Ebmeier International Journal of Geriatric Psychiatry
This was a recent joint letter to the BMJ
Open letter to the Prime Minister and the Chief Medical Officer Regarding Proposals to Introduce Screening for Dementia BMJ, Rapid Response,14/12/12
http://www.bmj.com/content/344/bmj.e2347/rr/620234
January 5, 2013
References for Times on norovirus
http://www.hpa.org.uk/Topics/InfectiousDiseases/InfectionsAZ/Norovirus/
http://www.hpa.org.uk/webc/HPAwebFile/HPAweb_C/1287143931777
http://www.plosone.org/article/info%3Adoi%2F10.1371%2Fjournal.pone.0006671
http://www.cdc.gov/norovirus/hcp/clinical-overview.html
http://www.bbc.co.uk/news/health-20889382
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2609872/
http://roar.uel.ac.uk/1588/1/2010_Phillips_norovirus_incidence.pdf
http://journals.cambridge.org/action/displayAbstract?fromPage=online&aid=7873632
http://www.ncbi.nlm.nih.gov/pubmed/12948373
http://jid.oxfordjournals.org/content/205/11/1622.full
http://www.hpa.org.uk/Topics/InfectiousDiseases/InfectionsAZ/Rotavirus/
http://www.ajicjournal.org/article/S0196-6553(10)00985-5/abstract
http://wwwnc.cdc.gov/eid/article/14/8/07-1114_article.htm
http://aem.asm.org/content/76/2/394.abstract
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2805232/
http://www.nejm.org/doi/full/10.1056/NEJMoa1101245
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2609865/
A school outbreak of Norwalk-like virus: evidence for
airborne transmission Epidemiol. Infect. (2003), 131, 727–736.
http://198.246.124.22/nceh/ehs/Docs/Evidence_for_Airborne_Transmission_of_Norwalk-like_Virus.pdf
http://www.hpa.org.uk/Topics/Infectio......
http://www.hpa.org.uk/Topics/InfectiousDiseases/InfectionsAZ/Norovirus/
http://www.hpa.org.uk/webc/HPAwebFile/HPAweb_C/1287143931777
http://www.plosone.org/article/info%3Adoi%2F10.1371%2Fjournal.pone.0006671
http://www.cdc.gov/norovirus/hcp/clinical-overview.html
http://www.bbc.co.uk/news/health-20889382
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2609872/
http://roar.uel.ac.uk/1588/1/2010_Phillips_norovirus_incidence.pdf
http://journals.cambridge.org/action/displayAbstract?fromPage=online&aid=7873632
http://www.ncbi.nlm.nih.gov/pubmed/12948373
http://jid.oxfordjournals.org/content/205/11/1622.full
http://www.hpa.org.uk/Topics/InfectiousDiseases/InfectionsAZ/Rotavirus/
http://www.ajicjournal.org/article/S0196-6553(10)00985-5/abstract
http://wwwnc.cdc.gov/eid/article/14/8/07-1114_article.htm
http://aem.asm.org/content/76/2/394.abstract
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2805232/
http://www.nejm.org/doi/full/10.1056/NEJMoa1101245
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2609865/
A school outbreak of Norwalk-like virus: evidence for
airborne transmission Epidemiol. Infect. (2003), 131, 727–736.
http://198.246.124.22/nceh/ehs/Docs/Evidence_for_Airborne_Transmission_of_Norwalk-like_Virus.pdf
December 18, 2012
Reasons to be careful
On the recent ‘festival’ of live tweeting from A+E/ambulances/GP surgeries;
If done carelessly, thoughtlessly, or simply unimaginatively, this can be unpleasant or even dangerous.
Consider: (and I’m paraphrasing)
* A tweet commenting that ‘lots of ladies are coming in to A+E for emergency contraception. Didn’t they know they can get it from pharmacies!’
This could make someone, possibly a vulnerable someone, feel stupid, idiotic, clumsy, or/and that their personal details and failings had been passed to a media department for tweeting to make an example of them.
Why not tweet ’do you know you can get emergency contraception from high street pharmacies without a prescription?’ The PR department sending the tweet shouldn’t even know that this type of problem have been dealt with that day.
Or:
* A tweet saying that ‘a young person has been admitted with urinary problems and abdominal pain, and is going for a scan now.’
What if you knew someone that had went to hospital that day? What if you were not that person, but another person in hospital – it is clear that permission has been sought? And is it right that we should be asking someone who is acutely unwell if a press department can tweet details of their case – why is this necessary? Confidentiality is crucial to enable the relationship between doctors and patients. Hospitals can be difficult enough places to contain information – communal wards, busy A+E departments, waiting areas – but this should be reason to preserve details about patients even more, not less.
Why not just say ‘patients with serious illness are routinely brought through A+E to be triaged’.
*A tweet saying that ‘someone came in because they were deaf – the earphone from their ipod had got stuck in their ear’ or ‘someone came in because a false nail had fallen off’.
Apparently some tweeting Trusts used ‘historical’ or ‘anecdotes’ from staff. This was possibly one.
But
- these may not be wholly true – embellished for the story
- these will not have been given permission by the patient to be disseminated
-the patient may recognise him/herself
-the patient or family/carers may be left feeling a bit stupid
- other people reading the anecdotes may feel worried that their stories in future – if they don’t get attendance ‘right’ – might be used like this
- things that seem like ‘trivial’ to doctors and nurses may not seem so minor to patients. This does not excuse careless use of A+E by patients, but makes me uncomfortable about ‘public shaming’ exercises via twitter. For example, a person may have a mild flu like illness, but because a relative died from an illness that seemed to begin in a similar way, they be more anxious than a healthcare professional would expect from a minor infection.
* A tweet saying ‘an ambulance has been called for an elderly lady who has hit her head’.
- why do we need to know this? The area covered may be geographically small; what if a neighbour sees an ambulance and deduces the background? While it should be possible for people to know what public services are doing, do we need this level of detail – which is also pegged to a specific time frame, being twitter? Who is it helping – the patients, or a public image?
In conclusion
- the massive advantages of a real time connecting system for discussion – twitter – gives scope to erode confidentiality
- just because it can be difficult to maintain confidentiality in acute settings does not mean that we should further threaten or spoil it via thoughtless tweets discussing specific patient care
- Trust hinges on confidence in confidentiality between patients and healthcare professionals. We lack evidence that tweeting can improve use of emergency care and we have not investigated the potential harms
- We should consider whether tweeting is being done to benefit us, professionals, institutions or a media or PR department before patient care.
November 28, 2012
November 25, 2012
Loneliness and telehealth
Loneliness is endemic. There are people who live alone, and who will see someone else rarely. Often, people who are lonely can’t get out much – unsteady, lacking confidence, afraid, anxious – and rely on relatives or rare visitors to help with shopping or outings. Many people – often older people – will still dress up to come to the doctors. There are people in waiting rooms who chat, there are babies to admire, there is weather to discuss. When patients and doctors talk, there is an exchange of information, a touch of conversation. Many doctors are part of the community where they live and work; many say that they get back as much, if not more, than they give, a kind of living exchange.
I am also a fan of the internet. Social media has enhanced, not diminished, my friendships in the world at large. I have met people and had conversations with folk I wouldn’t have met otherwise. But here is Jeremy Hunt, declaring that GPs and district nurses should be doing more by ipad and Skype; the assertion that 2.9 billion could be saved ‘almost immediately’ by having online rather than real life consultations. Where this figure has arrived from is unknown; whether this new direction could work or be dangerous may be rightful concerns but have fallen by the policy over evidence, technological wayside. This latest initiative is staggering for it’s unreasoned nature and ignorance of what currently happens in the world of primary care.
I’ve been in practice for over a decade, and have never worked in a practice where the telephone wasn’t a vital part of communicating with patients. It does, however, have serious shortcomings. I can’t listen to the patients’ chest or check reflexes in the legs. But I can discuss results, plan for follow up, or explain hospital letters or tests. Used well, it can help continuity of care, and promote an ongoing relationship. Often a phone appointment is the most useful and efficient way of seeing a plan through. But I can’t do everything by phone. The very most difficult, rewarding, and essential part of general practice – and what we are trained to do- is to pick up on cues, to notice the unsaid and the almost unseen. It’s about understanding what a person is worried about and why, what symptom they may be almost too uneasy to disclose, what is behind and around what we say and the gestures that we make. This isn’t some kind of bizarre parapsychological nonsense – it’s about listening and responding in a human interaction.
When people consult with doctors, they tend to discuss more than one problem. What and why they are raised is a matter of urgency and trust, and of the space to speak being allowed. I have been a doctor for almost twenty years, and I am still a little nervous when I see my own doctors – I expect that many others do too. We are vulnerable, we want to discuss matters which are important to us, we have questions, and we may be afraid. The issues which are discussed are not simply functionary, but are packed with information which may seem inconsequential, as thin and slight as tissue paper, but are multilayered, explaining and aiding the story not just of this pain, but of where it came from, how it is being dealt with, but where it shall be endured. Some home visits could perhaps be dealt with by telephone, but there are many people – again, often older – who will try their best to minimise their symptoms, and where a visit will explain more about their social circumstances and illness than half a ton of technology ever could. Mental illness is a large portion of GP workload: I would want proof that Skype consultations were not harmful before proceeding.
For in the brave new world of telehealth, with multiple tests results being monitoring, and protocolised healthcare, it would be easy to think that one day your healthcare will be possible without needing to see a doctor or a nurse. Your symptoms or measurements will be fed into a computer which will calculate the tests that need to be done and the actions that are therefore required. This was revealed with NHS Direct, which has been noted to use multiple protocols and produce many vast over reactions to symptoms which appropriately qualified humans have been able to deal with far more nuance and less inappropriate ambulance intervention. Telehealth costs vast sums in terms of equipment, but is hoped – by the government – to eventually reduce staff time in directly caring for patients as well as to reduce hospital admissions. We do not have enough good evidence that this is the case, but policy dictates that we should do it anyway. Yet computers cannot attend to personal hygiene, offer a spoon to the lips, lift a person to the commode. Telehealth will not be able to sit down and have a cup of tea or fetch a pint of milk. There will be no point in wearing a pressed suit for a computer monitor, and there will be no conversation to be made in when we press a button to send our results down the line.
We can already do much healthcare without the patients’ presence in the room, by simple use of the telephone. The people who will gain from bigger technology spends the government plans are the companies who manufacture them, and the politicians who can say they are investing in them. Only some patients will gain. People who were capable and mobile to start with also have lower need of monitoring or consultations, and will paradoxically be more likely to use them. People who find technology difficult, or who are frail, or who need human care more than they need their blood pressure numbers extracted and transmitted down a wire will lose out.
Spending on unproven technology continues despite carers often being paid at minimum wage and with barely enough time to do essential tasks. We need science and technology to help us provide the best care for patients. But we also need humanity. Jeremy Hunt, proceed at your peril.
November 16, 2012
Notes on the Whole System Demonstrator
Whole system demonstrator cluster RCT
The introduction says that the “monitoring of blood glucose” is an example of of useful monitoring that can be done by patients. In fact, Cochrane is pretty clear about how useful this is for people with type 2 diabetes not using insulin (the majority of people with diabetes), saying that “there is no evidence that self monitoring of blood glucose affects patient satisfaction,, general well being, or health related quality of life”. Similarly, with self monitoring of blood pressure, there is evidence that this can lead to small changes in blood pressure only, and there is no data on mortality or morbidity improvements for this intervention.
The WSD study examined patients with chronic obstructive airways disease, heart failure and diabetes. This is a wide range of conditions and the effect of telehealth on each these conditions were not analysed separately.
The randomisation was not done in the usual way but in terms of practices either assigned to the telehealth or the control group. Why? ”Initial discussions with sites indicated that individual randomisation of patients would probably not be acceptable to stakeholders. Therefore, we used a pragmatic approach to randomise general practice”. However there are large problems with this approach, as we have seen in breast screening trials for example. Cluster randomisation is beset with tendency to bias and I am not sure that the reasons given, for such a large and expensive trial, are good enough.
What was the intervention being tested? This to me is the biggest problem with this trial. Take note “Choices of telehealth devices and monitoring systems varied among the three trial sites, and there was no attempt to standardise these technologies across sites. We included a broad class of technologies, and the study was not designed or powered to examine differences between specific devices or monitoring systems.” In other words, the intervention varied hugely. This is crucial: what was the trial showing the effect of? The only constants were glucometer for diabetes (effect described above) weighing scales for heart failure (a commonly used device already, well outwith ‘telehealth’ trials) and an oximeter for COPD (which is of uncertain benefit in monitoring patients compared with usual care – this is important, because it might lead to either false reassurance or false alarms.)
Indeed, what is telehealth anyway? I don’t think that telephones or email communications between doctors and patients count as telehealth. The DoH had spent millions on the ‘black box’ monitoring devices well before the results of the WSD trial were published. These are “base units” which send data about health from the patients’ home. , either as questionnaires or clinical readings. The outcomes analysed were for mortality and emergency admissions.
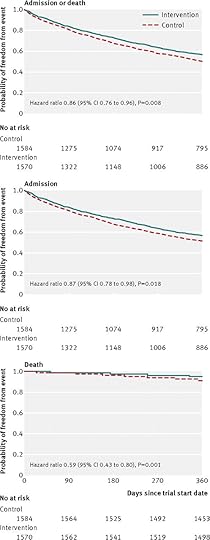
The graphs are here
How sure can we be that this apparent small benefit to intervention patients was real? The study was powered to detect a 17.5% change in admissions to hospital, however “ the magnitude of the group difference in admission proportion was relatively small (10.8%, 95% confidence interval 3.7% to 18.1%), and smaller than the size that the planned study design was able to detect (17.5%), raising questions about the clinical relevance of the results”. As for death rates “Intervention patients were significantly less likely to die within 12 months than controls. We also observed small differences in the mean number of emergency admissions per head between the intervention and control groups (crude rate 0.54 v0.68; difference 0.14). These changes were significant in the unadjusted comparisons and when we adjusted for a predictive risk score, but not when we adjusted for baseline characteristics”. In other words, the more the researchers tried to reduce the bias, the less sure the benefit appeared to be.
The study also found that there was an increased emergency admissions in the control group; “There could have been a propensity to select controls with a higher risk of short term admission and intervention patients with a lower risk.” It’s difficult to know, certainly we cannot exclude bias even with the case mix adjustments the researchers made.
So a comparable intervention wasn’t made, there are design issues in relation to the study design that increase the risk of bias, and the interventions being offered lack evidence themselves of benefit. The scale of savings is small. Neither has the WSD compared normal use of technology in practice (telephone, skype for remote access patients etc) against the expensive intervention being tested. For here is the conflict of interest. The DoH had bought these machines before the trial was completed, with publicity attached to it’s investment to “support the UK life sciences industry.” I’d personally like to see a bit more investment in the people who work as home carers, providing the unglamorous but essential help to wash, feed and assist people directly.
November 15, 2012
Links about telehealth
Radio 4 programme Inside Health on telehealth with references
BMJ article on press coverage
Cochrane on telehealth
JAMA telehealth in multimorbidity group showing increased mortality
BMJ Whole system demonstrator trial with excellent response from @trishgreenhalgh
Margaret McCartney's Blog
- Margaret McCartney's profile
- 13 followers



