Cyndi Turner's Blog, page 11
April 4, 2022
Getting to the “Why?”
When working with clients on their substance use, there’s one tool I always use. Though it seems simple, it can be powerful and lead to insights. It’s a Cost/Benefit Analysis.
Cost/Benefit Analysis:
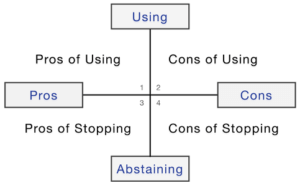
Clients are surprised when I tell them to put a big “X” in quadrants 2 and 3. I don’t care about these areas. People typically know the consequences if they use. It’s logical. Quadrants 1 and 4 is where the therapy happens. Working with these quadrants gets to their “why?”.For us it’s always the “why?” We must get clear on why they began using in the first place and what they get from their continued use.
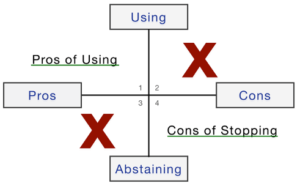
Particularly quadrant 4: What are the downsides of stopping your use? What would your life be like without the substances? What would you have to deal with? This gets to the “why?”. Only focusing on behavior without addressing the “why?”, often lacks the power to lead to lasting change.
While the substance use is having a negative impact overall, taking the substances away is a real loss. Strategies to help replace the benefits of using and working with underlying issues is what’s needed. By taking clients through this activity, I’m trying to push beyond their behavior – I’m trying to get to their “why?”
The post Getting to the “Why?” appeared first on Insight Into Action Therapy.
Alcohol and Mental Health
Whether you are celebrating, socializing, or just relaxing, there is a good chance that alcohol is involved. It can make you feel happy and more relaxed to have an alcoholic drink, especially when joined with others. However, the effects of too much alcohol consumption can be harmful to your physical health and your mental health. It is normal to want to have a drink when in a situation where it seems customary, but it is important to be cautious that you are not drinking for the wrong reasons.
If you only have alcoholic beverages because you are stressed or upset, it can severely worsen your mental health. If you or a loved one are using alcohol as a way of coping with your problems, then you might want to consider a dual diagnosis treatment program in Virginia. Contact us to find out more information at 703.935.8544.
Alcohol and Mental HealthBecause alcohol is a depressant, it is not uncommon to find that people who drink a lot also have mental health problems, including depression and anxiety. It can even sometimes cause psychosis. In some cases, people use alcohol to alleviate the symptoms of depression and anxiety; however, the effects are more harmful than helpful. Take a look at the following mental health concerns that alcohol abuse can complicate:
Depression: Alcohol affects chemicals in the brain that affect a person’s mood. When someone drinks too much, it can cause depression symptoms. Symptoms can also be worse for those who are taking antidepressants. It is important to stop drinking alcohol if you notice a significant decrease in your mood, which is known to help your mental health increase.Anxiety: Especially for someone who already has anxiety, alcohol can make any symptoms you are experiencing worse. Someone who often uses drinking as an excuse to relieve anxiety can cause that person to become reliant. This is why anxiety and alcohol abuse often go hand in hand.Self-Harm: In extreme situations, too much alcohol consumption can lead to someone harming him or herself. With inhibition lowered, a person cannot think clearly and in dangerous situations. This is especially apparent for those with anxiety and alcohol abuse issues. Quitting drinking is extremely important if you are having thoughts of harming yourself.There are, of course, other mental health issues that alcohol abuse can increase the risk of developing. Speaking with a counselor or therapist is perhaps the best way to not only address an alcohol use disorder but any underlying mental health issues prompting or growing out of it.
Treatment for Mental Health and Alcohol AbuseIt is very important for someone who has a dependency on alcohol to get treatment to make sure that their mental health is stable. Because alcohol and mental health are interlinked, it can be helpful to seek treatment for both. There are many treatment options to choose from, such as:
Dual diagnosisMental health treatmentPsychotherapyGroup therapyTherapy or some form of treatment allows a person to work with a counselor who will help them cope with their problems in a healthy way. They can also help prevent relapse for those suffering from alcohol abuse.
Getting Help at Insight Into Action TherapySeeking help for you or a loved one suffering from mental health and alcohol abuse problems is a difficult but important step. At Insight Into Action Therapy, we are committed to providing the best care for our clients to ensure a happy and healthy lifestyle. We offer a wide variety of therapy and treatment programs for those who need help with mental health and substance abuse problems.
Our team is ready to assist you or a loved one on your journey to recovery. We will be able to find the best fit for your needs. To find out how we can help you, visit our website or contact us at 703.935.8544.
The post Alcohol and Mental Health appeared first on Insight Into Action Therapy.
March 25, 2022
The Epidemic Within the Pandemic
This March, Craig James took part in a panel discussion sponsored by Parents of Addicted Loved Ones entitled ‘Addiction: The Epidemic Within the Pandemic’
 Close
CloseThe post The Epidemic Within the Pandemic appeared first on Insight Into Action Therapy.
Black History Month Spotlight with Craig James
Insight Into Action Therapy’s owner, Craig James, was recently interviewed by the Loudoun Chamber’s Diversity, Equity, Inclusion & Accessibility Committee as part of its Black History Month events.
Read the Interview HereThe post Black History Month Spotlight with Craig James appeared first on Insight Into Action Therapy.
Untangling DSM-5 Diagnoses
Sumit Anand, MD
The Diagnostic and Statistical Manual of Mental Health Disorders, 5th edition (DSM), is clinicians’ tool to form a diagnosis. I have seen plenty of DSM labels stacked together when encountering new patients. They say: I have ADD, PTSD, MDD, BPD, Bipolar and SAD. This tells me more about our current diagnostic system and how it is being used than anything it does about the actual patient. In short, it’s quite a mess. It requires untangling these DSM-5 diagnoses so there’s more clarity.
By the time I encounter them, patients are already confused, annoyed, and unclear about what the label means, let alone why they are taking so many different pills at once. Inevitably, they turn to Dr. Google. However, they just become more drenched in what I call information vomit. It’s a plethora of words, rehashed criteria, and endless lists of side effects and warnings about suicidal thoughts. Enough to give anyone anxiety and even panic.
How Do We Clean Up DSM-5 Diagnoses?Is it possible to have several disorders at once? Yes. However, as the list gets longer, each diagnosis requires closer scrutiny to ensure it is not “better accounted for by” (that’s DSM guidance) one of the other listed diagnoses. I have not seen this happen as often as it should in my decades of practice. The opposite occurs, namely, the diagnostic list growing longer and longer.
I interpret this phenomenon in several ways. The first is that healthcare practitioners may not use the DSM as it was rightly intended. It takes effort to sift through. Our current healthcare system in the United States isn’t geared to do that thoughtful, discerning practice.
Instead, practitioners must check a box to ensure a billing code is generated. It’s not for want of trying, but because of how the system conditions clinicians to practice mental health: checking boxes and trying to put the square peg of what they are seeing into the round hole of a rigid diagnosis, which inevitably leaves them unsure when they have so little time per patient.
The second is the inherent design of the DSM-5 diagnoses, with its lists of criteria. Clinicians were never trained to think of diagnoses as lists. Behavioral healthcare providers tend to resort to the use of “unspecified type” because the criteria that have to be met for a disorder don’t qualify for any of those listed in the DSM.
The cluster of symptoms gives them an intuitive feel of a syndrome. This includes the life stresses that may have led to symptoms, how the patient experiences something and the overall impact on their life.
Getting the Right DiagnosisThe DSM does not focus on these causal elements. It has lists of symptoms it has arbitrarily decided are a diagnosis and which are divorced from their causes. That’s not how it works in real life. Then every 7-10 years or so, criteria are added or deleted by a committee based on trials of patients in the field, again using criteria-based checklists in a dry, statistical way of distinguishing diagnoses.
If you ask most clinicians, they will tell you that diagnoses often merge. I have frequently seen symptoms of Generalized Anxiety Disorder alongside Social Anxiety Disorder, Panic Disorder, and even PTSD. All of them are characterized by exaggerated fearful reactions, hypervigilance, avoidance/escape behaviors, and anxious anticipation.
This tells me that the patient has developed an anxiety consciousness or predisposition that cuts across these artificial diagnoses and likely has roots in past traumatic experiences. In addition, I know that medication with the ability to increase brain serotonin transmission will be most effective for all these symptoms in the long term.
How Multiple DSM-5 Diagnoses Should Be HandledIt is possible to have multiple diagnoses. But that requires detailed history taking, which is often not performed. This has led to the other unsafe practice I commonly see of piecemeal prescribing: trying to treat each disorder as though it were a single symptom.
There are approaches to diagnoses than can be subject to historical swings of the pendulum. Over the decades, much debate has occurred as to whether diagnoses should be minimized to as few as possible by lumping them together or conversely split into subtypes or even different disorders. The current DSM system favors the latter. For that reason, we have seen an explosion in the number of psychiatric diagnoses over successive iterations of this internationally used manual.
I think that is a mistaken approach. For example, although clinicians are trained to address sleep complaints by considering it as part of the big picture manifestation of an anxiety or depressive disorder, they are now being increasingly encouraged to think of insomnia disorder and prescribe a sleeping pill rather than treat the underlying issue.
A symptom in and of itself is never a diagnosis. I try to ascertain what else is going on in their life, what susceptibilities their childhood may have rendered them, and what other symptoms the patient is reporting. Then I try to connect the dots between the different symptoms, their timing, and context, thus coming up with the most obvious diagnosis that explains the patient’s symptoms.
As I get to know the patient better, the context of their life, their use of substances, and with the perspective of time, I will either revise or consolidate my original diagnosis. Based on one or two symptoms, I avoid jumping to one particular diagnosis.
The Art of Practicing PsychiatryWhat works for me in coming to a diagnostic conclusion is simply letting the patient narrate what they are going through, with me asking a few clarifying questions to help me better distinguish what it is from what it is not. When one starts to take into account the associated life stresses and the onset, pattern, and severity of symptoms, the story starts to take shape. This overarching story says it all because it will resonate with the pattern of the patient’s symptoms and their responses to them.
Nobody wants to feel like someone is just checking boxes when it comes to diagnoses. It feels dehumanizing because it is! Just because the computer is an everyday part of our lives, it should not dictate how we think about psychiatric dysfunction, especially when it does not consider what comprises the totality of one’s own life. I make extra effort to listen through the noise and fog of symptoms to what the patient is trying to tell me. This is the art of practicing psychiatry: a universe away from the endless diagnostic checklists, billing, and diagnostic codes, and something that requires a more clinically intuitive sense of what is wrong. A bit like the art of using a stethoscope–only in the case of clinicians, it should be their listening skills.
Throughout the first evaluation, it will become evident how and why the patient is suffering, what the tangible impact on them is, and what type of relief they are seeking. Why does that sound like basic humanity and common sense? I suspect that our current system doesn’t compute that part.
Finding What’s Necessary at Insight Recovery CentersWith all the noise and clutter of diagnostic confusion, what hopeful adage can I leave you with? Rather than asking patients to “talk to your doctor,” we should be asking doctors to rely more on their clinical intuition and listen more to the patient.
You can learn more about DSM-5 diagnoses by calling Insight Recovery Centers at 703.935.8544.
The post Untangling DSM-5 Diagnoses appeared first on Insight Into Action Therapy.
March 17, 2022
Common Health Effects of Marijuana Abuse
Between work, relationships, and other daily tasks, there are a lot of stressors that people have to take on each day. It is normal to find ways to decompress and relax. However, not everybody makes the best decisions when it comes to winding down.
It may seem harmless to partake in a recreational drug like marijuana, but health effects can be dangerous for your health. It is possible to become addicted to marijuana, and it is important to get help as soon as possible. If you or a loved one needs dual diagnosis treatment, contact Insight Into Action Therapy at 703.935.8544.
Common Health Effects of Marijuana AbuseBoth short-term and long-term health effects of marijuana abuse affect your mental and physical well-being. Depending on the amount and potency, it is possible to become dependent on the drug. For those who already have a mental illness, marijuana can exasperate those symptoms. The longer you have been dependent, the worse the symptoms can get.
Some short-term effects include:
Panic attacks – Especially for those with a mental health disorderMemory issues – Not remembering things that were just told to youParanoid thoughts – Being suspicious of people with no evidenceSome long-term effects include:
Issues with retaining information – Learning new information becomes harderHigh risk of psychoses – Higher chance of disorders like schizophreniaPossible chronic cough – The smoke can cause constant coughingCannabinoid hyperemesis syndrome (repeated vomiting) – Uncontrollable bouts of vomiting after cannabis useThe longer a person uses marijuana or the more frequently it is abused, the worse the effects can become, and the likelier it can become an addiction. Often marijuana abuse is a sign of an underlying mental health issue like depression or anxiety. Similarly, when someone habitually abuses marijuana, then put themselves at greater risk of developing mental health concerns.
Signs of Marijuana AbuseWhen used too often, the signs of a marijuana abuse disorder become more apparent. Everyday activities become more difficult as your cognitive abilities and motivation will decrease. It affects everyone differently. However, some signs can point to someone having a problem.
Cravings – Constantly feeling the urge to use marijuanaLoss of social interest – Lack of interest in relationships, work, and hobbiesTrouble focusing – Unable to keep your mind on a taskDepression – Lower dopamine levels can cause depressionBesides the negative health effects, marijuana abuse can affect your work-life, friendships, romantic relationships, and recreational activities. It becomes harder to find the motivation to enjoy the things you used to love if you have become dependent.
Treatment Options for Marijuana Use DisorderTrying to quit something that you are dependent on is difficult and overwhelming. In a lot of cases, getting professional help is the best option. Trained professionals are great for giving the best advice to help a person safely quit something dangerous. Some therapies and treatment programs to consider are:
Dual diagnosis treatmentGroup therapyRelapse preventionEvery person’s needs are different in recovery, so speaking with a doctor to decide what works best for you is important when deciding what treatment option to pursue.
Getting Treatment at Insight Into Action TherapyKnowing the signs of a marijuana abuse disorder is the first step to recovery. At Insight Into Action Therapy, our goal is to get you the treatment you need to help you on your way to a dependency-free life. Our outpatient center specializes in mental health and substance use disorders with a wide variety of therapies and treatment options.
Our team is always happy to assist you or a loved one with any problems or questions. To find out more details about how we can help you, contact us at 703.935.8544.
The post Common Health Effects of Marijuana Abuse appeared first on Insight Into Action Therapy.
March 11, 2022
What Medications Do and What They Don’t
This is a big question for patients. It speaks to individual and societal expectations that we collectively heap onto medications. We see advertisements with happier faces after taking a specific drug, that we should “Talk to your doctor about.” We know of people who are taking antianxiety and antidepressant medications for mental health symptoms ranging from anxiety, fatigue and ADHD, to mood swings and even anger and aggression.
So what do medications do? People ask: Are they a cure for my problems? Will they make me feel better? Will I finally have a good night’s sleep or be free of anxiety and depression?
We come to a physician’s office with some variation of these expectations. They probably know that medication might help them from sinking further but are fearful of leaping into the unknown, tempered by curiosity and that fragment of hope that things might get better. As a practicing psychiatrist, I regularly encounter these feelings, hopes and uncertainties from my patients.
After understanding their symptoms and suffering, I view it as my primary duty to properly educate my patients about medications. That’s not easy. Over the years I have encountered deeply held prejudices, myths, piecemeal bits of information, anecdotes of bad experiences, and misconceptions that come from a patient’s circle of influence as to what a specific medication is (addictive, dangerous, ineffective, experimental, unproven).
It takes a candid and open conversation about facts in order to debunk such distorted reasoning. It also necessitates time to explain things in a way one can never get from an internet page or a non-trained professional. Of course, experience of actually having treated patients is another valuable and credible information source that gives me the confidence to recommend what I do. My motive in so doing is to help set the patient off on the right path toward recovery, not a quick fix.
What does this actually entail? It means giving realistic time frames for what symptom(s) the medication will address, how it does that at the receptor level in the brain, and what they can expect to see. At the same time, I encourage them not to write it off if they think it’s not working in the interim.
The reasons medications don’t work are manyfold: primarily time, genetics, and most importantly, the dose. Many times, a patient has told me that a medication didn’t work. When I ask what dose or how long they were on it, it soon becomes obvious that they were not dosed adequately and/or they were not on it long enough.
Another important factor is side effects. These are varied, not a given, mostly mild, will often dissipate, and rarely, not be tolerable at all. The effectiveness of medication depends on a host of factors, not all of which are entirely predictable at the outset. Based upon my clinical experience of almost two decades, I can tell you that the vast majority of medications do work for what they are intended, but only if taken, as prescribed.
Here’s where we come back to the question of what medications do and what they don’t. I’m sure you will agree that if you don’t take the medication, it will have 0 effectiveness. Yet, that is the most common reason why patients’ symptoms recur. This is such a common phenomenon that when I am training students and resident physicians, I make sure they ask this most basic question first. Of course, there may be a good reason why they stopped it, but if we don’t ask why, we may never be able to convince them to try a different dose or something else.
Sometimes (and this is more common than one might suppose), they were treated for years with the wrong medication after being misdiagnosed (like Wellbutrin® for anxiety symptoms, which typically makes it worse). They may stop taking medication altogether, walking away with a distorted, unpleasant narrative to tell others in the future.
That is why, as part of the educative process, I try to explain why it is important to take the right medication and consistently. Then, they can tell me honestly what it did and didn’t do by the time of our next appointment.
This way, the patient and I can decide if the dosing was inadequate, if there were other medications interfering with it, or if substance use (which speeds up liver metabolism) rendered the medication ineffective at that dose. Like a puzzle, we jointly figure out what road to take next, and why, testing out our hypothesis as we continue to treat symptoms.
That is how the science of medications works: individually. Even though a trial of 30,000 people may have indicated a 90% reduction in symptoms across the board, that does not mean it will necessarily work for you. But, with those odds, it would certainly be worth a try, wouldn’t you say?
We know that medications can work, provided they’re actually taken, adequately dosed, are tolerated by the patient, and that there is nothing else affecting their effectiveness (like daily marijuana or alcohol use, which is common in those “self-medicating” unbearable symptoms).
Does that mean medications work for everything and will eliminate all suffering? That fantasy is peddled by advertisements. They do reduce the intensity of symptoms and can provide meaningful relief from them over time. But they do not eliminate all symptoms. Those that work fast (Xanax, Klonopin and Ativan) tend to be addictive and sedating. It would be wrong to look for the instant fix on a regular basis.
That may sound a bit depressing, but there’s a second half to this part: the patient. Here’s where I ask them to meet me halfway. If we are to achieve recovery, they have to do their part.
Thus, a sleeping pill will not be as effective if your sleeping habits are bad. An antidepressant cannot be as effective if you continue to drink alcohol heavily. An antianxiety medication cannot make inroads into chronic anxiety if you are not practicing skills and thinking exercises learned in therapy.
There is some onus on the patient if we are to grasp the role and limitations of medications. The fantasy of not being rescued from suffering can be quite a let-down in this respect. Perhaps that’s where more efforts need to be put, in order to have the greatest yield? Does it entail responsibility of sorts? It does. Or another way of putting it: owning your own recovery. For some, this can be a lightbulb moment, whereby they feel empowered to get back in the driver’s seat of their own life.
Others may require more support and guidance as they are simply too demoralized by the time they come to see me. In such cases, we take it slower, and achieve mini victories, while I work on the medication part simultaneously. I call this my parallel tracks approach.
I take this seriously because if I can help boost their low energy as is classic in a depressive disorder, then that may help get their sleep habits on track that much faster. We’re in it together, that’s for sure.
What else don’t medications do? They are certainly not going to stop day to day stresses from coming and they may not repair a broken relationship. But, by improving overall functionality through relief of interfering symptoms, the air might clear to the extent that you can then make healthier choices, develop better communication and coping abilities and be less sensitive to hits from life.
Of course, the latter will also require therapy as an additional, powerful intervention, to help you better problem-solve the issues at hand. This is why medications should always be combined with therapy in order to achieve the best outcomes. Research has been proven this over and over again.
To conclude, I suggest we adopt a “can do” mentality to the topic of medications. There is a lot that they can do and you can help them work better by working with us on the things medications cannot.
Dr. Anand is a psychiatrist with Insight Into Action Therapy.He is available in both the Ashburn and Fairfax locations as well as telehealth for evaluations and medication monitoring appointments. You can reach Dr. Anand at 703-646-7664 or sanand@insightactiontherapy.com
The post What Medications Do and What They Don’t appeared first on Insight Into Action Therapy.
March 4, 2022
The Impact of Covid on Teens’ Mental Health Part Two
In my last video and blog post, I discussed why the pandemic might be affecting teens’ mental health in unique ways. Here, I’d like to share some observations from working with teens’ during the pandemic – from the days of scrubbing groceries with Clorox wipes, to googling: “how do you pronounce omicron?’”. What follows are some trends I’ve noticed, and of course do not represent the full scope of teens’ experience during the pandemic.
I’ll refer to these trends as:
“The great malaise” (“this doesn’t feel real…”)“The social anxiety swing”, andA Rise in Self-harm Close The great malaise:
Close The great malaise:As unbelievable as it now seems, in the early days of the pandemic we believed that the lockdowns, school closures, and social distancing would be short-lived sacrifices. However, there came a point when we collectively acknowledged, “oh, this isn’t going away any time soon.”
For many of my teen clients, the transition from the pandemic being a departure from normal, to being the new normal, triggered a downward slide. Many began presenting with depression-like symptoms. They reported having less energy, their sleep schedules became erratic and things that they typically enjoyed became less interesting. There was a general undercurrent of helplessness.
And then there was school. Many once high-achieving students began to feel less and less motivated. I often was told “it (school) doesn’t feel real.” The virtual learning wasn’t working for them. The routine became wake up, log-on, turn off the camera and microphone, and go back to sleep or play video games.
Many of these clients weren’t technically in a major depressive episode (though I did see a significant uptick in teens presenting with a major depressive disorder during this time). Rather, what I observed was a pervasive fog of low-level depression amongst teens.
The social anxiety swing:For my teen clients with social anxiety, the pandemic initially led to relief from their symptoms. The reason was obvious: lockdowns and social distancing removed the triggers of the anxiety. More than that, they were being required to not interact with others. So, there wasn’t the uncomfortable push from parents (or their therapist) to continue doing the anxiety-provoking work of exposing themselves to social situations.
Why do I call this the social anxiety swing? Well, as restrictions lifted and they began in-person school and activities, their social anxiety was more intense than when the pandemic began. This is also not surprising given how anxiety often works. If something triggers anxiety, it is avoided, leading to temporary relief. However, as one gets stuck in these anxiety/avoidance loops, that same trigger brings on more intense anxiety over time. Additionally, two years of significant isolation during adolescence can stunt the development of social skills, which can also contribute to social anxiety.
Rise in self-harm:A rise in suicide attempts during the pandemic, particularly among young girls, has rightfully received a lot of attention. Indeed, the surgeon general report states:
In early 2021, emergency department visits in the United States for suspected suicide attempts were 51% higher for adolescent girls and 4% higher for adolescent boys compared to the same time period in early 2019.
However, the form of self-harm I’m discussing is different. I’m referring to my teen clients cutting, burning, hitting, or scratching of themselves as a coping mechanism. Typically to help deal with intense, out of control feelings, or conversely, if they’re unable to feel anything at all.
I had many parents bring their teenage kids in after discovering they were self-harming. In most of these cases there was no prior history of self-harm. Now,the causes for any particular client are typically complex. However, a common theme expressed to me was that they felt that their and their family’s lives, and the world itself, was out of control. A feeling I believe we can all empathize with.
I hope this helps give a feel for the struggles many adolescents experienced during this pandemic. If you or your teen is having a hard time, you’re not alone. Please reach out for help!
The post The Impact of Covid on Teens’ Mental Health Part Two appeared first on Insight Into Action Therapy.
February 18, 2022
Relationships and Addiction
Addiction affects the person with or recovering from a substance use disorder and the people in their lives. Family and friends want what is best for their loved ones, and it hurts them to see someone they care about struggle with addiction. It’s not always easy to figure out the best course of action when trying to get help for someone you know who needs it, and that can cause a strain on your relationship.
Relationships and addiction are tricky; however, there are ways to help mend relationships that have faced hardships. Going to relationship repair counseling is one way for families to solve issues they can’t work out on their own. You can contact us at 703.935.8544 to learn more about this.
Relationships and AddictionIt can be both scary and sad to watch the relationship you built with somebody completely change because of addiction. Often because both the person living with addiction and their loved ones struggle in different ways, neither one knows how to help the other. There may be more fights and less communication than usual.
The effects of drug addiction on families vary depending on the situation, but it is never easy whether you have experience with addiction or it’s completely new. Knowing the signs of a family or relationship struggling because of a substance use disorder can help determine if you and a loved one need help. Effects that it may have on families is:
Overprotectiveness of the person with addiction – becoming increasingly codependent to keep a close watch on the person with a substance use disorderViolence – someone with a drug addiction may have violent urges and outburstStruggling financially – money that should go to bills may go to drugsAll of these can lead to a family becoming more stressed and less able to live harmoniously as they might have previously been able to do.
Fixing Relationships Affected by AddictionThe effects of addiction on families can seem irreversible. You may even feel helpless that you can’t seem to resolve your issues. There are ways to help get your family the help they need to get back to a happy and healthy status. Working together at home is important; however, seeking professional help is also something to consider when dealing with relationships and addiction.
One easy thing every couple or family should take is to work on communication. Letting each other know how you are feeling, whether scared, hurt, or angry, is an important first step to letting each other know that you care about the other person. You may even consider after talking to go to therapy.
Relationship repair therapy helps couples overcome any obstacles causing problems in their relationship, whether with a romantic partner or family member. Couples and families will be able to figure out the source of what is causing the issues in their relationship. By working with a professional, you will be able to learn more about how you can help yourself and work on your relationships together.
Getting Help at Insight Into Action TherapyAt Insight Into Action Therapy, we understand that relationships and addiction cannot be easily worked on alone. We are here to help those struggling with addiction and their families. With our wide variety of therapy and treatment programs, such as relapse prevention therapy, family therapy, and psychotherapy, there is something to help everyone. Whether you are battling addiction or know a loved one, Insight Into Action Therapy is here to assist. For more information, contact us at 703.935.8544.
The post Relationships and Addiction appeared first on Insight Into Action Therapy.
February 9, 2022
The Impact of Covid on Teens’ Mental Health
We’re now two years (and who knows how many variants) into this pandemic, and it’s been rough on us all. However, just as the risks from Covid itself are different for different age groups, the psychological and social effects have been different as well. While the pandemic has brought so much uncertainty, one thing is clear: many of our young people are struggling. Anxiety, depression, and self-harm are all on the rise. The U.S. Surgeon General has even released an advisory to detail this crisis.
As a therapist who works with many teens and their families, I thought I’d share some observations from the therapist’s office. But first, let’s look at the bigger question: why might this be affecting teens differently in the first place?
One way to approach this question is to look at the developmental stage of adolescence. Some important features of adolescence are:
 Close Exploring and developing their identity and beliefs,Achieving greater independence and re-negotiating roles with their parentsDeveloping greater social skills and empathy,Navigating their maturing bodies and romantic relationships, andA greater ability to imagine and plan for their future.
Close Exploring and developing their identity and beliefs,Achieving greater independence and re-negotiating roles with their parentsDeveloping greater social skills and empathy,Navigating their maturing bodies and romantic relationships, andA greater ability to imagine and plan for their future.Importantly, much of this happens through the interaction with peers. I know this isn’t exactly a “hot take” for parents, but peer relationships take on a huge importance in adolescence. The lockdowns, social distancing, school closures, and loss of activities have been tough on them.
And this is the heart of the point I’m making – that due to their developmental stage, extreme isolation is damaging for teens in unique ways.
Now, there are of course many other factors that play a significant role. For example: socioeconomic status, the effect of a parent getting sick or losing their job, or a kid being stuck at home all day with an abusive family member, to name a few.
Indeed, let’s give this some crucial context. The pandemic hasn’t caused a mental health crisis in young people. Rather, there has been a growing crisis for at least a decade, and then COVID came and exacerbated what was already there.
I won’t offer up the trope that “kids are resilient” (which they are), because doing so often feels like a way of avoiding the real need. However, I believe wholeheartedly in teens’ and their family’s ability to heal and flourish, no matter their starting point.
In future videos and blog posts I’ll discuss observations from working with teens during the pandemic and some things we can do to support our teens.
But if your teen is struggling, it can never hurt to reach out to a mental health professional in your community.
The post The Impact of Covid on Teens’ Mental Health appeared first on Insight Into Action Therapy.



