More on this book
Community
Kindle Notes & Highlights
Read between
January 2 - January 12, 2021
There is some debate among experts about whether viruses are living things. But this virus is surely acting like any other living thing would: it found available and untouched habitat, and it seized it. And the virus will keep infecting humans until we develop immunity or invent a vaccine. Even then, SARS-2 will most likely become like other viruses that circulate in our species, such as influenza, measles, and the common cold. No matter what, humans will have to reach a modus vivendi with this virus. But it will kill many of us before we do. A new pathogen has been introduced into our
...more
There have been as many plagues as wars in history, yet always plagues and wars take people equally by surprise. —Albert Camus, The Plague (1947)
Epidemiologists quantify the lethality of pathogens in two primary ways. The infection fatality rate (IFR) is the probability a person will die if he or she gets infected. The case fatality rate (CFR) is the probability a person will die after being diagnosed with the condition by a health-care provider. Sometimes an alternative for the CFR is used, the symptomatic case fatality rate (sCFR), which is the probability that a person will die if he or she simply shows symptoms of the infection.
To summarize, SARS-1 was ten times deadlier than SARS-2, which in turn is ten times deadlier than the ordinary flu.
While SARS-2 is less deadly than SARS-1 in a given single case, that does not mean that it’s less dangerous overall. Imagine a population of one thousand people and a pathogen that infects twenty of them; this pathogen makes those people seriously ill and kills two of them. That yields a CFR of 10 percent. Now imagine another population of one thousand people and another pathogen that does the same thing—it makes twenty people seriously ill and kills two of them—but this pathogen also infects another one hundred eighty people, making them mildly or moderately ill but not killing them. The CFR
...more
The time between when a person is infected and when he or she shows signs or symptoms is called the incubation period. This ranges from two to fourteen days in SARS-2 (hence the recommended fourteen days of isolation) and is typically about six to seven days. For SARS-1, the incubation period was shorter, ranging from two to seven days. But there is another important interval, the latent period, which is the time between when a person is infected and when he or she becomes infectious—that is, able to spread the disease to others.
How many new cases does each case give rise to? For each person who becomes infected, how many other people, on average, does that individual infect? This number is known as the effective reproduction number, denoted Re (sometimes also known as the effective reproductive rate).
The R0 captures the capacity of a pathogen to start an outbreak, and it reflects the degree to which it is infectious in the absence of any measures to control it. Re, however, reflects the real-time spread of the epidemic later in its course, when the population is no longer “naive.” The Re is susceptible to human responses.
measles is one of the most infectious diseases known, with an R0 estimated to be 12 to 18 (that is, a single infected person typically can infect somewhere between twelve and eighteen other people). Chicken pox is 10 to 12. Smallpox is 3.5 to 6. Ebola is 1.5 to 1.9. Seasonal influenza ranges from 0.9 to 2.1.
The Re declines naturally as an epidemic proceeds because susceptible people become infected and either die or survive and acquire immunity (to a greater or lesser extent).
If this variation in R0 is large, the risk of an outbreak starting from any given person falls substantially because there will be many more people who cannot spread the germ than people who can. In such a case, many importations of infected people from one place to another are required to seed the epidemic in the new location.
Consider the following simplified illustration of this idea. Say there is a group of one hundred people who are infected with a virus. One is a super-spreader who can spread disease to three hundred people, and ninety-nine are not infectious at all. The average R0 in this hypothetical population of one hundred is 3.0, but there is a very large variation in infectiousness. If just one person from such a population is chosen at random to travel to another place, that means that, ninety-nine out of a hundred times, there will be no epidemic as a result. By comparison, if there is a group of one
...more
For SARS-2, it looks like the variation in R0 is somewhat lower than for SARS-1, so while super-spreading events do occur, they are less common than the more frequent, humdrum chains of transmission.43
popular people with many connections (like person C) tend to be infected earlier in the course of an epidemic than random people chosen from the same population. Because of their many social interactions, popular people have an increased risk of exposure.
But this also means that popular people are more likely to become immune early on in the course of an epidemic. And if all the popular people became immune early, relatively more paths for the virus to spread through society would be cut off.
This also means, incidentally, that vaccinating people with many connections is more helpful than vaccinating people with few connections.
Most estimates place the R0 of SARS-2 as roughly the same as that of SARS-1, about 3.0. This is actually rather worrisomely high for a pathogen; compare it to the R0 of ordinary influenza, which is 0.9 to 2.1.55 But SARS-2 has a smaller dispersion in Re, meaning that transmission chains are somewhat less likely to be dead ends, which makes it easier to reliably spread SARS-2 than SARS-1. SARS-2 is also less deadly than SARS-1, with a CFR of less than 1 percent (compared to around 10 percent for SARS-2). As we saw, this makes SARS-2 paradoxically more concerning, because larger numbers of
...more
For SARS-2, however, probably at least 40 percent of the human population worldwide will be infected in the end, and perhaps as much as 60 percent.
immunizing the elderly, while it will reduce their deaths, does not have much effect on the actual course of the epidemic. Immunizing working-age people helps break chains of transmission through social networks and can be much more effective in preventing deaths on a population level
The actual cause, McKeown argued, was socioeconomic improvements and the implementation of public health measures.
Flattening the curve buys time to save more lives. Ventilators and medications do not run out. Doctors and nurses are not exhausted, so they can do a better job of caring for the people who are sick, which means fewer deaths. With less cramped conditions, fewer health-care workers contract the disease themselves, keeping them on the front lines. Buying time also allows us to get the public health system ready; we can develop tests and procedures for contact tracing and learn more about the virus in our laboratories. When we flatten the curve, we also push some of the infections into the future
...more
With exponential growth, for a very long time, nothing seems to be happening. And then all of a sudden, a lot happens.
The formula (R0-1)/R0 gives this percentage. Using an R0 for SARS-2 of 3.0 means that the calculated percentage of the population that must be immune is 67 percent.
For instance, a mask with just 50 percent efficacy in reducing droplet transmission worn by just 50 percent of people can reduce the Re from 2.4 to about 1.35—roughly the level of seasonal influenza. This means that, if there were one hundred cases of such an infection at the beginning of the month, in a no-mask scenario, there would be 31,280 cases at the end of the month; but in a mask scenario, there would be only 584.
Two types of tests can assess coronavirus infection. The first is a test for the virus itself; it involves taking a swab of mucus (or soon, saliva) from inside the patient’s throat or nose (often quite deep inside—one patient described it as a “stab in the brain”) and processing this mucus to extract the RNA that comes from the virus. This RNA has its sequence assessed and compared to a reference standard of the RNA for the pathogen.
A second type tests not for the virus but for antibodies to it—the proteins that our bodies make to fight the virus. This requires taking a sample of the patient’s blood, via fingerstick or venipuncture, and testing it for the specialized antibodies to the virus (saliva tests have also been developed).
testing and tracing rely heavily on each other to be truly effective. Testing on its own does little to help control a virus. It tells us only who already has the virus, not where it has spread. Similarly, tracing alone does not help much if we cannot identify asymptomatic individuals. Tracing is also compromised if it’s not feasible to quarantine those individuals whom we find, either because they are unwilling or unable to self-isolate at home or because we lack places where they can stay—for example, if they are homeless or if they live in a crowded environment. It’s only when you can test,
...more
The fewer people that the average person comes into contact with each day, the better.
the primary purpose of school closure is to reduce social mixing, not necessarily to protect children from infection.
Dr. Tom Frieden, the former head of the CDC, would later estimate that if New York had adopted widespread physical-distancing measures even a week or two earlier, the death toll might have been reduced by 50 to 80 percent.84
Age affects the infection process in several ways. First, there is the attack rate, which is the likelihood of someone in the population getting the condition.19 The attack rate for COVID-19 varies by age, and younger people are less likely to get infected.
Triage is by definition a hard and imperfect and utilitarian calculus. And we engage in triage in medicine all the time—with transplantation candidates, for instance, where some patients are prioritized to receive organs.44
dismissing racial differences in health outcomes on the grounds of their being mediated by other factors is a bit like saying that, after adjusting for the quality of ingredients, the ambience, the sophistication of the menu, and the existence of a good wine list, there is no difference between a meal at McDonald’s and a meal at the fanciest restaurant in New York City.
One of the features of COVID-19 that made it hard for people to take the disease seriously was the lack of visible symptoms (in most cases).
key objective of flattening the curve, to which so much effort was directed, was precisely to give us time to invent new treatments or a vaccine to forestall some of the deaths.
there are so many different approaches to developing a vaccine for SARS-2 that the variety offers a sense both of the likelihood of success and of human ingenuity.
The coronavirus infects cells by using the spike proteins on its surface to bind to proteins on the surface of human cells known as ACE2 receptors, especially those cells that line the respiratory tract, but other tissues as well, as we saw in chapter 1. After a sequence of steps, the virus enters the cell, where it takes over cellular machinery in order to reproduce itself, releasing more virus into the body, which can both harm the individual and spread to other people.
Still another approach, which has never previously been employed successfully, is to use nucleic acids from the virus instead of proteins—that is, to use fragments of DNA or RNA that resemble the genetic information of the virus. In the case of the DNA approach, the idea is to instruct the body to make a viral protein inside its own cells, as if it had been infected by the virus, and this in turn elicits the usual immune response. A variant of this approach is to add DNA that matches genes of a virus to an entirely different species of another, milder virus.68 This altered virus is then
...more
the emergence of drugs such as remdesivir and dexamethasone, and others to come, vindicated the whole strategy of deploying the nonpharmaceutical interventions to flatten the curve. By buying time, we allowed ourselves the opportunity to use our capacities for teaching and learning in order to enhance our survival.
By using a standard benchmark of five hundred thousand dollars as the economic value of a year of life (or ten million dollars per life, regardless of age), we can estimate that one million coronavirus deaths (at the rough age distribution at which they occur) would be worth about six trillion dollars. Even at the highest end of a range of estimates of the consequences to our economy, including the expenditures by our government, we do not reach that sum.
from a Darwinian point of view, it does not suit a pathogen’s interest to kill its victims, since it would rather that its hosts move around and transmit it to other people.
Over the short term, it’s possible that the virus could change to be either better or worse for us (in terms of its transmissibility, lethality, or both)—even though any long-term changes are likely to be positive for us, the unfortunate hosts.
But it’s possible that once we reach herd immunity in the coming years, people will simply be exposed to the SARS-2 virus as children, have a mild disease (most of the time!), get some immunity, and then avoid serious disease if they are re-exposed thereafter. Such a scenario is a quite possible eventual end to the story of SARS-2.
So we will reach herd immunity, or the pathogen will evolve to be less lethal, or (after a very long time) humans will evolve to be resistant. That is the biological end of the story.
If we see pandemics purely as a function of biological details—such as the mutations that make it possible for the pathogen to leave bats and spread in humans or the pharmacokinetics of drugs in our bodies—we may be lulled into thinking that there is nothing we can do to prevent or arrest such events. But if we see pandemics as sociological phenomena as well, we can more clearly recognize the role of human agency. And the more we see our own role in shaping the emergence and unfolding of pandemic disease, the more proactive and effective our responses can be.
Americans began with denial and anger, moved on to bargaining and depression, and will end with acceptance, which will mark the final, sociological end to the pandemic.
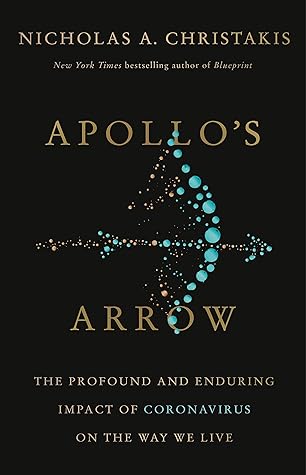
Figure 17: Serious influenza pandemics have recurred every few decades over the past three centuries.