Aaron E. Carroll's Blog, page 41
April 8, 2021
Vaccine Development, Covid-19, and mRNA vaccines
In this last episode of our six-part series on vaccinations, supported by the National Institute for Health Care Management Foundation, we cover vaccine development – particularly in the context of the current global pandemic. We discuss the timeline of Covid-19 vaccine development and the mRNA vaccine approach.
The post Vaccine Development, Covid-19, and mRNA vaccines first appeared on The Incidental Economist.
March 30, 2021
Incidents and Criticisms: Vaccine Backlash Part 2
Part five of our six-part series on vaccinations, supported by the National Institute for Health Care Management Foundation, continues to explore the history of societal backlash against vaccination, with particular attention to vaccine-adjacent incidents and misinformation.
The post Incidents and Criticisms: Vaccine Backlash Part 2 first appeared on The Incidental Economist.
Home cultivation of medical marijuana can result in higher hospitalizations and emergency department visits related to opioids
Jayani Jayawardhana, PhD, is an associate professor at the University of Georgia College of Pharmacy (@JayJayawardhana). Jose M. Fernandez, PhD, is an associate professor at the University of Louisville College of Business (@UofLEcon).
Before the COVID pandemic, the United States was in the midst of an opioid epidemic. A menu of health policies has been recommended to battle the rising cases of opioid overdoses including prescription drug monitoring programs (PDMPs), increasing access to naloxone (an opioid antagonist), and pain management clinic laws. Surprisingly, another set of policies adopted by some states—though not intended as a response to the opioid epidemic—was found to be effective in reducing opioid prescriptions: medical marijuana policies (MMPs).
A new study, published this month in Health Services Research, contributes to the literature on medical marijuana by examining the relationship between medical marijuana policies and hospitalizations and emergency department (ED) visits related to opioids while accounting for different types of medical marijuana policies.
Background
Medical marijuana policies take different forms, including permitting active dispensaries to sell medical marijuana and allowing home cultivation of medical marijuana. These policies differ in how much access they afford patients. Access contingent on dispensaries often means needing to register as a patient, gaining access to medical marijuana card, and being able to afford the cost of medical marijuana since it is not covered through health insurance. Furthermore, dispensaries may not be easily accessible for all users.
Home cultivation provides easier access to marijuana by allowing patients to grow marijuana at home. Although home cultivation policies may limit the number of plants that can be grown and the maturity level of plants at a given household, home cultivation provides access to marijuana at almost no cost except for the initial cost of purchasing plants/seeds for cultivation.
Previous literature has emphasized the importance of accounting for these specific types of policies when studying medical marijuana since they are different from each other. Existing research on MMPs have found states with home cultivation of medical marijuana only to be associated with reductions in opioid prescriptions among Medicare enrollees. While a few studies have found MMPs to be associated with reductions in opioid-related mortality, opioid-related hospitalizations, and opioid prescriptions among Medicaid enrollees, these studies have not accounted for different types of MMPs.
Methods
We used state-level quarterly data from Healthcare Cost and Utilization Project’s Fast Stats database to gain access to ED and inpatient visit rates by state. These data were linked with changes in medical marijuana polices in states from 2005 to 2016. Along with the medical marijuana polices, we controlled for a long list of state policies used to combat the opioid crisis including presence of PDMP, mandatory access of PDMP by providers, pain management clinic laws, Good Samaritan laws, availability of naloxone without a prescription, recreational marijuana policy implementation, and Medicaid expansion. In addition, we controlled for state socio-demographic characteristics such as unemployment rate, percent uninsured, population size, median household income, ethanol consumption per capita, and beer taxes.
We used a difference-in-differences regression approach to compare changes in opioid-related inpatient and ED visit rates per 100,000 population before and after a state has implemented a given MMP to those states that did not implement the given MMP. A key identifying assumption was that parallel trends existed in inpatient and ED visit rates among states that implemented MMPs (treatment) and states that did not implement MMPs (control) prior to policy implementation; an event study showed no significant difference between treatment and control groups prior to policy implementation.
Findings
The results of our study showed that states that allow home cultivation of medical marijuana experienced about 12% increase in opioid-related hospitalizations and about 44% increase in opioid-related ED visits compared with states without home cultivation of medical marijuana. However, study results did not find significant associations between medical marijuana dispensaries and opioid-related hospitalizations and ED visits.
We further disaggregated home cultivation into two categories, unsupervised and requiring a permit. We found unsupervised home cultivation to be associated with an increase of 15.6% in inpatient hospitalizations related to opioids though requiring a permit for home cultivation was not significantly associated with hospitalizations. These findings indicate that easier access to marijuana through unsupervised home cultivation may result in adverse health outcomes needing further treatment.
Additionally, implementation of recreational marijuana policy was associated with about 16-17% increase in opioid-related hospitalizations, while it had no significant association with opioid-related ED visits. Access to naloxone without a prescription was significantly associated with an 8% increase in opioid-related hospitalizations though it was not significantly associated with opioid-related ED visits. While naloxone may help reduce mortality by reversing opioid overdoses, individuals that experience overdoses may seek healthcare at inpatient setting. Thus, it is not surprising that availability of naloxone is associated with increased opioid-related hospitalizations.
There are a few limitations in this study. The study uses state-level aggregated data for inpatient and ED visits from only 47 states and 35 states respectively for the period of 2005-2016. Identifying specific reasoning behind opioid-related hospitalizations and ED visits or the source of drugs such as prescription or illicit (i.e., heroin) that resulted in those visits was not possible due to the aggregate nature of the data.
Conclusions
Despite these limitations, the findings of this study provide an important contribution to the policy debate on medical marijuana legalization. The findings indicate that increased access to marijuana via home cultivation is associated with increases in opioid-related hospitalizations and ED visits, suggesting that easier access to marijuana among opioid users may result in adverse health conditions that need treatment at inpatient or ED settings.
While it remains unclear whether marijuana liberalization may be a beneficial public health tool in the fight against the opioid epidemic, the results of this study support the argument that potential benefits and adverse health outcomes associated with different types of MMPs should be taken into consideration when discussing marijuana as a policy alternative in addressing the opioid epidemic.
The post Home cultivation of medical marijuana can result in higher hospitalizations and emergency department visits related to opioids first appeared on The Incidental Economist.
March 26, 2021
Healthcare Triage Podcast: Making Progress in Multiple Myeloma Research
Dr. Aaron Carroll talks with Dr. Rafat Abonour and Dr. Fabiana Perna about multiple myeloma research and ongoing studies, such as the Indiana Myeloma Registry. We’ll also hear about how losing weight may help lower your risk for getting cancer and why immunotherapy could be a promising treatment option for multiple myeloma patients.
Available wherever you get your podcasts! Including iTunes
This episode of the Healthcare Triage podcast is sponsored by Indiana University School of Medicine whose mission is to advance health in the state of Indiana and beyond by promoting innovation and excellence in education, research and patient care.
IU School of Medicine is leading Indiana University’s first grand challenge, the Precision Health Initiative, with bold goals to cure multiple myeloma, triple negative breast cancer and childhood sarcoma and prevent type 2 diabetes and Alzheimer’s disease.
The post Healthcare Triage Podcast: Making Progress in Multiple Myeloma Research first appeared on The Incidental Economist.
March 23, 2021
The History of Vaccine Backlash Part 1
Part four of our six-part series on vaccinations, supported by the National Institute for Health Care Management Foundation. It turns out, people have been resistant to the idea of vaccines pretty much since vaccines were invented. This video explores the history of anti-vaccine sentiments, vaccine legislation, and societal backlash.
The post The History of Vaccine Backlash Part 1 first appeared on The Incidental Economist.
March 22, 2021
HSR Special Issue Call for Abstracts: Translating Research into Policy and Action
Sponsored by: Health Services Research and Development (HSR&D) & Quality Enhancement Initiative (QUERI), Veterans Health Administration, U.S. Department of Veterans Affairs
Submission deadline: April 30, 2021
Health Services Research (HSR) and the VA HSR&D QUERI program are partnering to publish a Special Issue on Translating Research into Policy and Action, to be co-edited by Melissa Garrido, PhD, Arleen Brown, MD, PhD, and Amy Kilbourne, PhD.
A recent Presidential Memorandum emphasizes the need to make policy and programmatic decisions that are “guided by the best available science and data.” This memo follows the implementation of the Foundations for Evidence-Based Policymaking Act (Evidence Act), which requires all cabinet-level agencies in the United States government to support policy and budget decisions with rigorous evidence. The HSR&D QUERI program is leading the Veterans Health Administration’s response to the Evidence Act and fosters partnerships among researchers, clinicians, and system managers and leaders to maximize the policy impact of research and ultimately improve health outcomes and equity for patients.
Both within and outside of the VA, implementation and translation of research findings into action can be done more effectively if the needs of affected communities are taken into account. Community engagement is critical to disseminating, implementing, and sustaining evidence-based programs and policies in the real world. This engagement is crucial to improving health equity. However, the generation of evidence to inform policy and the community impact of policy are often considered separately. Most studies that end up informing implementation of evidence-based programs or policies are conducted in settings or populations that are not representative of those that are most adversely impacted by disparities in health or health care.
The goal of this special issue is to highlight research that bridges this gap and engages the community or relevant stakeholders to inform policy and lead to meaningful change.
HSR is soliciting papers that are relevant to the development of evidence-based policy and the translation or implementation of research into action. Papers that highlight novel findings and methodological research directions based on implementation science, community-based participatory research, and similar fields and/or seek to inform health equity and promote active participation of individuals most affected by the research are especially welcome, including those that focus on the VA health care system, as well as other systems and payers. Papers must report the results of original investigations. Framework, review, summary, and commentary articles will be solicited separately.
Illustrative examples of topics within the area of Translating Research into Policy and Action include but are not limited to:
Research conducted using community-based participatory methods, implementation strategies, or as pragmatic trials to ensure that results are relevant to affected communitiesInterventions to improve equity in health services delivery or public healthResearch on new strategies to expand opportunity and retention for a more diverse U.S. health care workforce that serves vulnerable and marginalized populationsDevelopment of evidence in underserved communities or settings not traditionally involved in clinical or health services research that directly informs policy at the state or federal levelActivities conducted in response to the Foundations for Evidence-Based Policymaking ActMonitoring the public health impact of policy changeThe deadline for initial submission of abstracts is April 30, 2021. Abstracts may not exceed 300 words and must otherwise be formatted as indicated in the HSR Author Guidelines. These abstracts will be evaluated by a multidisciplinary review panel that will select the best abstracts to receive invitations to submit full manuscripts. The evaluation criteria will include: (1) quality, rigor and originality; (2) significance and usefulness for advancing knowledge about evidence-based policy and the translation of research into action; and (3) clarity of writing and presentation.
Manuscripts submitted for the Special Issue will first undergo the same HSR peer review process as all regular manuscripts. However, due to the timeline for publishing the Special Issue, HSR will monitor the progress of manuscripts through the review process and try to shorten it; likewise, authors should expect to be especially prompt in returning revisions. All accepted articles will be published electronically within a few weeks of acceptance using Wiley’s Early View process. Articles published through Early View are fully published, appear in PubMed, and can be cited. Approximately 12 articles will be selected, based on the most original and significant work addressing the theme. Accepted manuscripts that are not selected for the Special Issue will be automatically scheduled for print publication in a regular issue. The print publication date for the Special Issue will be June 2022.
Key dates for authors:
April 30, 2021: Submission deadline for abstracts for the Special Issue
May 21, 2021: Notification of manuscript invitation for the Special Issue
July 17, 2021: Submission deadline of manuscripts for the Special Issue
June 2022: Publication of the Special Issue
If you would like to submit your abstract for consideration, please email your abstract and co-author contact information to the editorial office at hsr@aha.org, using the subject line “Special Issue on Translating Research into Policy and Action”.
The post HSR Special Issue Call for Abstracts: Translating Research into Policy and Action first appeared on The Incidental Economist.
Cancer Journal: How to Live with Cancer
A friend asked me if I had learned anything about how to live with cancer. I laughed — the “live with” part is still in play — but I’ll try to give a helpful answer.
That answer is: Even when you are very sick, do your best to maintain your health by getting or staying fit.
I need to apologize for that answer because it may be out of reach for many readers. I can focus on fitness because more important things have gone well for me:
Connection. I have spent lots of time with my wife, children, and friends. Sadly, my kids and many of my friends live in the States, and the pandemic has closed the border. So I haven’t been in the same room with them in a year. However, being sick has freed large blocks of time. That gift of time was generously matched by my friends and family, who have spent hours with me on Zoom.Religion. We are Christians. For better or worse, cancer might scare me a bit less than you expect it to. Secular readers: Go ahead and deduct 15 points from your estimate of my IQ. I don’t mind.Canada. My out-of-pocket costs for my care have been about $100, for co-pays on an ambulance ride and some prescriptions for generic hydromorphone (trade name Dilaudid, a pain medication). Of course, my health care was not free. I prepaid through my taxes at a rate that reflected my income. The Canadian system gave me access to advanced cancer care without the slightest fear that it would bankrupt my family. Likewise, my employer immediately granted me months of paid disability leave. God save the Queen.Without these foundations, I would surely have been overwhelmed. With them, I have maintained energy, mood, and purpose.
A few years ago, we lost a good friend to ovarian cancer that disseminated to her liver. She maintained her energy, dignity, and hospitality throughout the years of her illness. Part of her secret for thriving despite surgeries and chemotherapy was staying fit and upright through long daily walks with her friends and a standard poodle, which she logged on her Fitbit. Witnessing her exemplary life helped prepare us for my cancer.
I won’t cure my cancer through exercise (or diet, meditation, or prayer); this is how I live with it. I’m not ‘fighting’ cancer; that’s the Cancer Centre’s job. My job is to stay mobile, attend to my daily needs, care for those I love, write a bit, and prevent depression. Fitness is a means to those ends.
You get fit by developing a workout discipline. You don’t get disciplined by gritting your teeth, or at least not just by doing that. Workout discipline comes from joining a team, getting good coaching, evolving a program, and accurately monitoring your effort. Instead of a standard poodle and a Fitbit, I have a King Shepherd puppy and Peloton.

My workout partner, Mika (pronounced ‘Mee Ka’).
Mika joined our family in late June, just three days before I was diagnosed. Dogs are ideal teammates. The anthropologist Pat Shipman argues that the domestication of wolves to collaborate on hunts for large mammals enabled homo sapiens to outcompete the neanderthals for the apex predator niche in the Pleistocene. Mika loves to be with me, and she never gets bored. She unfailingly prompts me at walk time. She has a sweet disposition but can destroy anything if she doesn’t get multiple daily walks. Get a dog and, if you can, get a good trainer to help raise her.
The Peloton bike arrived on October 12, about a month after the end of radiation therapy but perhaps only a week after the physical experience’s nadir (radiation toxicity accumulates for weeks past your last session).
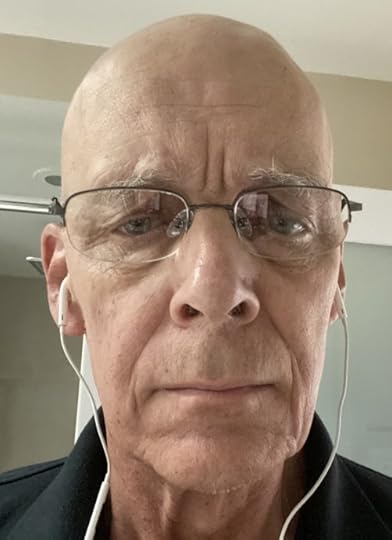
Me, a week before the end of radiation therapy. I have lost 14 kg (30 lbs) since it started.
The bike is overpriced, but what makes it superior to the standard gym stationary bike is the touchscreen display of your pedalling cadence, resistance, power (the watts/joules you are generating), and their averages. Your workout data are saved to the cloud, maintained in an easily accessible history, with lots of graphs and notifications to track your progress. Every fitness app does this kind of thing, but Peloton does it better than anything else I’ve tried.

Cloud-connected device for capturing exertion data and accessing a social network. Also: a stationary bike.
The Peloton brand is online spin classes, but that’s not the best way to think about it. Peloton has a touchscreen-equipped treadmill, as well as outdoor running, strength training, yoga, pilates, barre, stretching, and meditation classes that you can access from your phone or tablet. The instructors encourage you to cross-train, which is crucial. Trust me: if cycling is all you do, you will injure yourself. There is a huge library of recorded modular workouts of 5 to 90 minutes that you can do any time. Use these like Lego blocks to build a weekly fitness program. That sounds intimidating. However, although the instructors radiate spin class glamour, many of them are former physical therapists or strength/endurance coaches. Start by choosing workouts based on the music. You’ll absorb cross-training ideas from the instructors’ monologues and the prompts that follow the completion of a workout. What makes all this work is the pricing. You pay one monthly fee rather than paying by the class, so there is no disincentive to doing, for example, a 5-minute guided stretch after each ride.
Peloton has an active social network. The touchscreen has a camera, so if you do a live class, you can add a video chat with friends on the same ride. I haven’t explored this much, but I’d like to. I used to be an age group triathlete, and group rides were the core of my training (shout out to the Columbus Triathlon Club!).
Perhaps most importantly, the Peloton instructors supply good coaching at internet scale. I recommend Matt Wilpers and his PowerZone training,* but you can pursue lots of other tracks. PowerZone training gives you a method to tailor your workouts to your current fitness. If you are so sick that you can barely turn the pedals, that’s fine. PowerZone reconfigures your touchscreen to rescale the output wattage your pedals are generating to a scale anchored by 0 = no pedal rotation to 7 = a level of exertion that you can maintain for just seconds. The program has a procedure to set these zones to what you can do. Then, when you do a PowerZone class, the instructor calls out a zone, rather than an output wattage (or cadence or resistance) that might be impossible. This gives you a workout that is feasible — and, in measured doses, demanding — for you. The PowerZone workouts — interval training, in spin class drag — give you a path to build those capabilities.

Matt Wilpers. My cycling coach, and maybe 1 million other people’s too.
Effective coaching at internet scale is an amazing accomplishment. It is what wellness programs promise but fail to deliver. Of course, Peloton — and dog ownership — succeed mostly because the people who commit to them already love dogs and want to be fit. Perhaps this selection effect is the entire story. Who cares? Select yourself in. Fitness will help you live with and recover from cancer.
*Matt Wilpers didn’t invent power zones. Professional cyclists and triathletes all train this way. What he has done is figure out how to teach and support this style of technical, instrumented cycling training for a mass audience.
To read the Cancer Posts from the start, please begin here.
The post Cancer Journal: How to Live with Cancer first appeared on The Incidental Economist.
March 15, 2021
Unemployment Insurance Can Help Reduce Food Insecurity, the More Generous the Better
Cecille Joan Avila is a policy analyst at Boston University School of Public Health. She tweets at @cecilleavila.
Since the start of the COVID-19 pandemic in March 2020, more than 54 million Americans have lost jobs. Because of this loss in wages, two times as many Americans became susceptible to food insecurity, defined by the US Department of Agriculture as “a household-level economic and social condition of limited or uncertain access to adequate food.” Food insecurity was a significant problem even before the pandemic and is linked to worse physical and mental health outcomes for both children and adults.
The Coronavirus Aid, Relief, and Economic Security (CARES) Act was passed to provide immediate assistance for the entire US population struggling with the pandemic. One benefit of the CARES Act was an expansion of unemployment benefits, including a $600/week federal supplement to existing state unemployment insurance. While the $600/week supplement terminated at the end of July 2020, expanded eligibility and duration of unemployment benefits continued through December 26, 2020. These benefits were later extended through March 14, 2021 and included a $300/week federal supplement. The recently signed American Rescue Plan extended these benefits through September 6, 2021.
Existing research suggests an association between unemployment insurance and food insecurity — that unemployment insurance can help reduce it. The COVID-19 pandemic presented a unique opportunity to look at this relationship in a moment of simultaneous difficulty and, for a period, government generosity.
New Research
A recent paper by Julia Raifman, ScD, Jacob Bor, ScD, and Atheendar Venkataramani, MD, PhD, contributes to the literature by examining the relationship between unemployment insurance and food insecurity in the context of the pandemic. Academic affiliations include Boston University School of Public Health (Raifman, Department of Health Law, Policy, and Management; Bor, Department of Global Health); and The University of Pennsylvania (Venkataramani, Leonard Davidson Institute for Health Economics, Medical Ethics and Health Policy).
Methods
Using the Understanding Coronavirus in America study, researchers looked at nationally representative data collected by the University of Southern California Center for Economic and Social Research between April 1, 2020 and November 11, 2020 over 15 survey waves. They looked at households who earned less than $75,000 in the last 12 months and who reported employment at the start of the pandemic but since lost it. The main exposure of interest was the onset of unemployment benefits, with secondary analyses examining the effect of unemployment insurance both with and without the CARES supplement, and the impact of varying weekly amounts. This population was compared to those who never reported receiving unemployment insurance.
Food insecurity outcomes were measured based on a yes/no response to two questions: “In the past 7 days, were you worried you would run out of food because of a lack of money or other resources?” and “In the past 7 days, did you eat less than you thought you should because of a lack of money or other resources?”
Using difference-in-differences models for the exposures of interest, the researchers compared changes in food insecurity and eating less before and after an individual received unemployment insurance to those who did not receive unemployment insurance. This was under the assumption that both groups would both experience food insecurity in the same way, regardless of unemployment insurance or not. They also conducted a complementary event study model to evaluate and see that parallel trends existed before receipt of unemployment insurance and to reduce bias in treatment timing variation.
Findings
This research revealed that for households making less than $75,000 and who reported unemployment during the COVID-19 pandemic, receipt of any amount of unemployment insurance was associated with a 35% reduction in any reported food insecurity. Unemployment insurance was also associated with a 48% decline in reports of eating less due to financial limitations. Larger unemployment benefits resulted in larger reductions in food insecurity.
Researchers found that, in the study population, the greatest prevalence of food insecurity (22.2%) was reported at the beginning of the study period (April 1 – 28). The lowest prevalence food insecurity (8.9%) came in the second-to-last wave of the study period (September 30 – October 26). Despite this decline, these frequencies never equaled that of the employed comparison group.
To document the disparities resulting from structural racism, race and ethnicity data were also collected and included in the analyses. In the study population, participants who reported they were racial, sexual, or gender minorities; or younger; or lower income, were more likely than other groups to report food insecurity or eating less due to cost.
There are a few significant limitations in this study. Being able to distinguish the effects of receiving unemployment insurance benefits from receiving stimulus payments, as they occurred at similar points in time, was difficult. Also, this web-based survey might not accurately represent the totality of the US population, particularly under-represented minorities.
Conclusions
Despite these limitations, these findings contribute to existing literature by confirming the association between unemployment insurance and reduced food insecurity. Beyond that, these findings are significant for policymakers, as it reveals that the amount and length of unemployment benefits matter.
Not only does the research show that more generous supplements can have a greater impact, it also shows what groups are more susceptible to food insecurity, particularly important for policymakers seeking to address both food insecurity and equity.
The current extension of unemployment insurance benefits ends in September. But the need to appropriately address food insecurity will continue long after the pandemic ends, whenever that may be.
The post Unemployment Insurance Can Help Reduce Food Insecurity, the More Generous the Better first appeared on The Incidental Economist.
Expanding health coverage is good. But we also need to fix stingy plans.
Cecille Joan Avila is a policy analyst with the Boston University School of Public Health ( @cecilleavila ). Paul Shafer, PhD, is an assistant professor of Health Law, Policy, and Management at the Boston University School of Public Health ( @shaferpr ). Megan B. Cole, PhD, MPH, is an assistant professor of Health Law, Policy, and Management at Boston University School of Public Health ( @meganbcole ).
While on the campaign trail, President Biden focused on expanding the Affordable Care Act and addressing the problem of uninsurance through an affordable public option, expanding tax credits, and re-indexing plans. But focusing solely on uninsurance is not going to be enough, especially as enrollment in high deductible health plans has increased over the last decade, with no signs of slowing. Not only can these plans result in delayed care, it can also make existing health inequities worse.
In The Washington Post, Paul Shafer, Megan B. Cole and I go further into this issue. As we write:
Given political realities, however, [the public option] might not see the light of day. So it would be best to target underinsurance directly. Most people with high-deductible plans get them through an employer. Yet unlike in the marketplace plans, the degree of cost sharing in these employer plans is the same for low-income as well as high-income employees. To deal with that problem, the government could offer incentives for employers to expand the scope of health services they cover – which they can’t now – would help some people escape high-deductible plans. The public option would also eliminate premiums and involve minimal to no cost-sharing for low-income enrollees – especially helpful for uninsured (and underinsured) people in states yet to expand Medicaid.
While President Biden’s American Rescue Plan increased the Affordable Care Act subsidies and will help a significant number of those who are uninsured, there is still more work to be done. The focus needs to turn towards those who have health coverage, but only in the form of an unused insurance card.
Read the full piece here. It also appeared in the print edition of The Washington Post on March 7, 2021 on page B05.
Research for this piece was supported by the Laura and John Arnold Foundation.
The post Expanding health coverage is good. But we also need to fix stingy plans. first appeared on The Incidental Economist.
March 14, 2021
Completely, 100%, removing, killing, disabling, and canceling Google Family Link
Wow, Google Family Link, you have failed us. You seemed so helpful for a time — a way for parents to control their kids’ usage of Android devices (phones, Chromebooks). It worked so well for years, until it failed, big time.* Worse, it is so hard to remove, in large part because the removal instructions, by which I mean the full instructions, are not online, best I can tell.
I am here to fix that and spare you some misery. I lost several hours of my life to this so you don’t have to.
If you have a child for whom you control her screen time via Family Link on both her phone and Chromebook and you want to be rid of it for good, on all devices, you have to do the all of the following and in order.
Powerwash the Chromebook. Yup. That’s right. No way around this. (I tried.)Remove the Family Link account from your child’s phone. This actually removes her Google account entirely from her phone (which if f***ed up, but there it is). You cannot just delete the app. Do not just delete the app. This does not work. (I tried.)Unsupervise your child from the parent app. Yes, you have to do this. You can’t skip this step. Deleting the app does not unsupervise. (I tried.)Now go ahead and delete the Family Link app from child and parent devices. You should no longer need it. But you can’t do this deletion until you’ve done all of the above or you will be very sorry. (I tried, and I was.)Have your child recreate her personal and/or school accounts on her Chromebook and phone.It seems like a big headache, but actually it doesn’t take long to do all this. Maybe 10 minutes. The big thing that sucks is that Google has made it next to impossible to figure all this out. They don’t just come out and explain how to do this all in one place. It’s split over several links. It’s almost as if, once they have you tangled in their web of control, they don’t want you to leave. (No, I do not think Apple is better. I hate it more. Been there. Done that. Worse.)
With all of this, you are finally free and clear from the tyrannical oppression of Google Family Link, which as I said, used to be great. Somehow, they screwed it up and it’s just not worth it anymore to me (your mileage may vary).
* Best I can tell, and this is speculative, some update caused Google Family Link to freak out when my child had both personal and school Google accounts on her Chromebook, which, let’s face it, is a very normal thing to need these days. I was getting multiple emails a day about her logging onto a new device (she was not). Annoying.
Contacting Google Family Link via chat, they told me to just uninstall and reinstall the app. Boy was that bad advice. The app could not be reinstalled on my child’s phone because … wait for it … she had both school and personal accounts on the phone (again, a normal thing to need these days). Family Link would make her choose just one (bad). With this, we gave up. We wanted out. It’s not so easy … back to the main thread of the post.
The post Completely, 100%, removing, killing, disabling, and canceling Google Family Link first appeared on The Incidental Economist.
Aaron E. Carroll's Blog
- Aaron E. Carroll's profile
- 42 followers



