Aaron E. Carroll's Blog, page 40
May 3, 2021
Cancer Journal: SHATTERED
This journal is about being a cancer patient during the COVID epidemic. Last week I had a conversation with my doctor that shattered me. I have so much to say! But first, I need to convey what we have learned.
After completing radiation therapy in September, I have steadily regained my health. I am working and writing full-time. I spend an hour or more each day on my yoga mat and exercise bike. My sense of taste has almost wholly returned, so I can cook. Everything has pointed toward a complete recovery, an outcome consistent with the data showing that radiation is usually curative for oropharyngeal cancers caused by human papillomavirus exposure.
Everything, that is, except for two things. First, the pain at the site of my primary tumour has never gone away. Second, I have had a computerized tomography (CT) scan and a positron emission tomography (PET) scan that were consistent with persistent cancer. My clinicians were skeptical of these results because these tests have high false-positive rates, and the evidence shows that radiation usually works. To resolve this uncertainty, I had a surgical biopsy a week ago this Monday.
The pathology report from the biopsy appeared — amazingly quickly — in my electronic health record on Tuesday night. The pathologist found that my tumour had survived radiation and was continuing to grow.
On Thursday, I met with my surgeon. Evidently, the biopsy was sobering news, yet I was calm. When I was first diagnosed last July, I had assumed that I would need surgery. Moreover, I knew that surgery could cause severe morbidity because my tumour was near the root of my tongue. Specifically: I might lose the ability to speak, and I might be feeding permanently through a gastric tube. But in this worst case, I would still have far more than Stephen Hawking did, and I was confident that the procedure, as invasive as it was, would nevertheless leave me with a life I would greatly value. I was ready to do it.
Stephen Hawking.
So I went to the meeting assuming that its purpose was to discuss the resection of my throat to cut out the tumours.
But that didn’t happen. Here is the gist of our conversation:
Surgeon: I’ll review your options. First, there is palliative care.
What?
Surgeon: Second, there is medical assistance in dying. [This is legal in Canada.]
Me: That is not an option for religious reasons.
Surgeon: I understand. I mentioned these options first because we do not have much to offer in the way of treatment. I have spoken with Dr. X [my radiation oncologist]. As you know, you can’t tolerate additional radiation. Neither of us thinks that chemotherapy gives you any benefit at this stage. But I will arrange an appointment with Dr. Y [a medical oncologist with whom I had previously discussed chemotherapy] to discuss that further. Now let’s talk about surgery.
I explained to him that I understood that surgery could entail the loss of essential functions. But if it were curative, and I could be with my family and still write and do science, that would be acceptable.
Surgeon: And I would support that view. The problem is that the surgery would also damage your epiglottis, which protects your lungs from infection. You would experience repeated pneumonias, requiring hospitalization, one of which would likely kill you. And for all that, it would only offer you a slight chance — perhaps 10% — of a cure.
Oh.
Surgeon: The last option is to look for a clinical trial of experimental therapy. I know this is difficult to hear, and I would be happy to help you get a second opinion.
Please don’t criticize my surgeon for his direct style. We know each other well, and he knew how much I value his honesty.
How did I feel? Shattered.
By which I mean that I felt the urgent need to pursue a thousand lines of thought — “IS palliative care something to consider?” “How do I convey this news to my brother?” “They keep saying ‘salvage’; how is that different from any other type of medicine?”… — with each new thread interrupting the one that preceded it. And I felt grief. Not (thank you, God) despair, anger, resentment, or even fear. Instead, grief for the impending separation from my wife, children, work, home, future, and even my dog.
Grief, yes, but also confusion. We are all Bayesians now, and we expect each additional data point to move our beliefs, but not move them too much. That’s how things work, > 99% of the time.
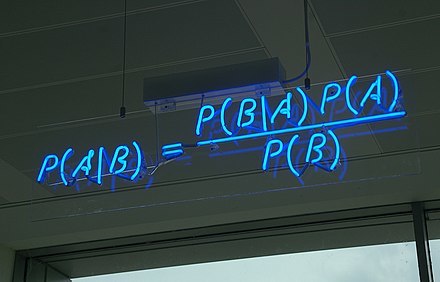
Bayes’ theorem. Tattoo it on the inside of your eyelids.
However, there are moments in every life when the data demolish your beliefs and change everything going forward.* You are informed that they have let you go from a job where you had excelled on every evaluation. You watch terrorists knock down skyscrapers with airliners.
What confused me was that I felt great. The night before the meeting, perhaps to prove that I was healthy, I had set a personal record for kilojoules of output during a 45-minute ride on my Peloton bike. And yet my doctor told me that I had 6 to 18 months to live. How could this be?
What’s challenging to hold in your mind is that a tumour is like an epidemic: it grows exponentially. The chart below shows daily new COVID-19 cases in Nepal. On March 20, 2021, was anyone prepared for what would happen in the next month?
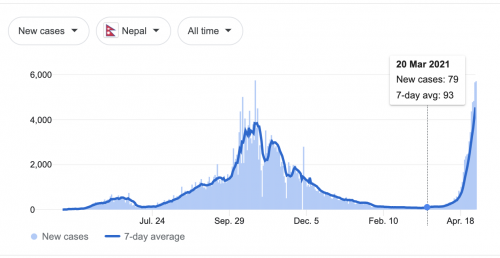
New COVID-19 cases in Nepal. Repeat after me: “The world is full of non-linearity.”
Likewise, a tumour starts off too tiny to matter. Then it doubles, but it is still small. Then it doubles again and again, and sooner rather than later, it kills you. Tracking back through the scans, my tumour seems to double every couple of months.
I haven’t stayed shattered. This is good because it turns out that dying — if that is what I’m doing — entails surprising numbers of meetings and lots of paperwork. It would be incautious to say I have hope, but I have a direction, including a second opinion. Thanks for listening, more later.
*Of course, my experience wasn’t truly inconsistent with Bayes’ theorem, but let’s not get too pedantic here.
To read the Cancer Posts from the start, please begin here.
The post Cancer Journal: SHATTERED first appeared on The Incidental Economist.
April 30, 2021
The Importance of Diversity and Equity in Medicine and Research: Healthcare Triage Podcast
In this episode, Dr. Brownsyne Tucker Edmonds and Dr. Sylk Sotto talk with Dr. Aaron Carroll about the importance of diversity and equity in research, higher education, and medicine. They share insights about underlying issues they’ve seen and talk about ways to encourage success for underrepresented minorities.
This episode of the Healthcare Triage podcast is sponsored by Indiana University School of Medicine whose mission is to advance health in the state of Indiana and beyond by promoting innovation and excellence in education, research and patient care.
IU School of Medicine is leading Indiana University’s first grand challenge, the Precision Health Initiative, with bold goals to cure multiple myeloma, triple negative breast cancer and childhood sarcoma and prevent type 2 diabetes and Alzheimer’s disease.
Available wherever you get your podcasts! Including iTunes
The post The Importance of Diversity and Equity in Medicine and Research: Healthcare Triage Podcast first appeared on The Incidental Economist.
*DEADLINE EXTENDED* | HSR Special Issue Call for Abstracts: Translating Research into Policy and Action
The following is cross-posted on the Health Services Research website.
Sponsored by: Health Services Research and Development (HSR&D) & Quality Enhancement Initiative (QUERI), Veterans Health Administration, U.S. Department of Veterans Affairs
Submission deadline: April 30, 2021 May 12, 2021
Health Services Research (HSR) and the VA HSR&D QUERI program are partnering to publish a Special Issue on Translating Research into Policy and Action, to be co-edited by Melissa Garrido, PhD, Arleen Brown, MD, PhD, and Amy Kilbourne, PhD.
A recent Presidential Memorandum emphasizes the need to make policy and programmatic decisions that are “guided by the best available science and data.” This memo follows the implementation of the Foundations for Evidence-Based Policymaking Act (Evidence Act), which requires all cabinet-level agencies in the United States government to support policy and budget decisions with rigorous evidence. The HSR&D QUERI program is leading the Veterans Health Administration’s response to the Evidence Act and fosters partnerships among researchers, clinicians, and system managers and leaders to maximize the policy impact of research and ultimately improve health outcomes and equity for patients.
Both within and outside of the VA, implementation and translation of research findings into action can be done more effectively if the needs of affected communities are taken into account. Community engagement is critical to disseminating, implementing, and sustaining evidence-based programs and policies in the real world. This engagement is crucial to improving health equity. However, the generation of evidence to inform policy and the community impact of policy are often considered separately. Most studies that end up informing implementation of evidence-based programs or policies are conducted in settings or populations that are not representative of those that are most adversely impacted by disparities in health or health care.
The goal of this special issue is to highlight research that bridges this gap and engages the community or relevant stakeholders to inform policy and lead to meaningful change.
HSR is soliciting papers that are relevant to the development of evidence-based policy and the translation or implementation of research into action. Papers that highlight novel findings and methodological research directions based on implementation science, community-based participatory research, and similar fields and/or seek to inform health equity and promote active participation of individuals most affected by the research are especially welcome, including those that focus on the VA health care system, as well as other systems and payers. Papers must report the results of original investigations. Framework, review, summary, and commentary articles will be solicited separately.
Illustrative examples of topics within the area of Translating Research into Policy and Action include but are not limited to:
Research conducted using community-based participatory methods, implementation strategies, or as pragmatic trials to ensure that results are relevant to affected communitiesInterventions to improve equity in health services delivery or public healthResearch on new strategies to expand opportunity and retention for a more diverse U.S. health care workforce that serves vulnerable and marginalized populationsDevelopment of evidence in underserved communities or settings not traditionally involved in clinical or health services research that directly informs policy at the state or federal levelActivities conducted in response to the Foundations for Evidence-Based Policymaking ActMonitoring the public health impact of policy changeThe deadline for initial submission of abstracts is April 30, 2021 May 12, 2021. Abstracts may not exceed 300 words and must otherwise be formatted as indicated in the HSR Author Guidelines. These abstracts will be evaluated by a multidisciplinary review panel that will select the best abstracts to receive invitations to submit full manuscripts. The evaluation criteria will include: (1) quality, rigor and originality; (2) significance and usefulness for advancing knowledge about evidence-based policy and the translation of research into action; and (3) clarity of writing and presentation.
Manuscripts submitted for the Special Issue will first undergo the same HSR peer review process as all regular manuscripts. However, due to the timeline for publishing the Special Issue, HSR will monitor the progress of manuscripts through the review process and try to shorten it; likewise, authors should expect to be especially prompt in returning revisions. All accepted articles will be published electronically within a few weeks of acceptance using Wiley’s Early View process. Articles published through Early View are fully published, appear in PubMed, and can be cited. Approximately 12 articles will be selected, based on the most original and significant work addressing the theme. Accepted manuscripts that are not selected for the Special Issue will be automatically scheduled for print publication in a regular issue. The print publication date for the Special Issue will be June 2022.
Key dates for authors:
April 30, 2021 May 12, 2021: Submission deadline for abstracts for the Special Issue
May 21, 2021: Notification of manuscript invitation for the Special Issue
July 17, 2021: Submission deadline of manuscripts for the Special Issue
June 2022: Publication of the Special Issue
If you would like to submit your abstract for consideration, please email your abstract and co-author contact information to the editorial office at hsr@aha.org, using the subject line “Special Issue on Translating Research into Policy and Action”.
The post *DEADLINE EXTENDED* | HSR Special Issue Call for Abstracts: Translating Research into Policy and Action first appeared on The Incidental Economist.
April 29, 2021
The Facts About Vaccine Passports
Vaccine passports are a big topic right now, even though “passport” might be the wrong word. We take a look at what they are and what they aren’t, and dig deeper into the concerns most commonly voiced about them.
The post The Facts About Vaccine Passports first appeared on The Incidental Economist.
April 26, 2021
*REMINDER* | HSR Special Issue Call for Abstracts: Translating Research into Policy and Action
The following is cross-posted on the Health Services Research website.
Sponsored by: Health Services Research and Development (HSR&D) & Quality Enhancement Initiative (QUERI), Veterans Health Administration, U.S. Department of Veterans Affairs
Submission deadline: April 30, 2021
Health Services Research (HSR) and the VA HSR&D QUERI program are partnering to publish a Special Issue on Translating Research into Policy and Action, to be co-edited by Melissa Garrido, PhD, Arleen Brown, MD, PhD, and Amy Kilbourne, PhD.
A recent Presidential Memorandum emphasizes the need to make policy and programmatic decisions that are “guided by the best available science and data.” This memo follows the implementation of the Foundations for Evidence-Based Policymaking Act (Evidence Act), which requires all cabinet-level agencies in the United States government to support policy and budget decisions with rigorous evidence. The HSR&D QUERI program is leading the Veterans Health Administration’s response to the Evidence Act and fosters partnerships among researchers, clinicians, and system managers and leaders to maximize the policy impact of research and ultimately improve health outcomes and equity for patients.
Both within and outside of the VA, implementation and translation of research findings into action can be done more effectively if the needs of affected communities are taken into account. Community engagement is critical to disseminating, implementing, and sustaining evidence-based programs and policies in the real world. This engagement is crucial to improving health equity. However, the generation of evidence to inform policy and the community impact of policy are often considered separately. Most studies that end up informing implementation of evidence-based programs or policies are conducted in settings or populations that are not representative of those that are most adversely impacted by disparities in health or health care.
The goal of this special issue is to highlight research that bridges this gap and engages the community or relevant stakeholders to inform policy and lead to meaningful change.
HSR is soliciting papers that are relevant to the development of evidence-based policy and the translation or implementation of research into action. Papers that highlight novel findings and methodological research directions based on implementation science, community-based participatory research, and similar fields and/or seek to inform health equity and promote active participation of individuals most affected by the research are especially welcome, including those that focus on the VA health care system, as well as other systems and payers. Papers must report the results of original investigations. Framework, review, summary, and commentary articles will be solicited separately.
Illustrative examples of topics within the area of Translating Research into Policy and Action include but are not limited to:
Research conducted using community-based participatory methods, implementation strategies, or as pragmatic trials to ensure that results are relevant to affected communitiesInterventions to improve equity in health services delivery or public healthResearch on new strategies to expand opportunity and retention for a more diverse U.S. health care workforce that serves vulnerable and marginalized populationsDevelopment of evidence in underserved communities or settings not traditionally involved in clinical or health services research that directly informs policy at the state or federal levelActivities conducted in response to the Foundations for Evidence-Based Policymaking ActMonitoring the public health impact of policy changeThe deadline for initial submission of abstracts is April 30, 2021. Abstracts may not exceed 300 words and must otherwise be formatted as indicated in the HSR Author Guidelines. These abstracts will be evaluated by a multidisciplinary review panel that will select the best abstracts to receive invitations to submit full manuscripts. The evaluation criteria will include: (1) quality, rigor and originality; (2) significance and usefulness for advancing knowledge about evidence-based policy and the translation of research into action; and (3) clarity of writing and presentation.
Manuscripts submitted for the Special Issue will first undergo the same HSR peer review process as all regular manuscripts. However, due to the timeline for publishing the Special Issue, HSR will monitor the progress of manuscripts through the review process and try to shorten it; likewise, authors should expect to be especially prompt in returning revisions. All accepted articles will be published electronically within a few weeks of acceptance using Wiley’s Early View process. Articles published through Early View are fully published, appear in PubMed, and can be cited. Approximately 12 articles will be selected, based on the most original and significant work addressing the theme. Accepted manuscripts that are not selected for the Special Issue will be automatically scheduled for print publication in a regular issue. The print publication date for the Special Issue will be June 2022.
Key dates for authors:
April 30, 2021: Submission deadline for abstracts for the Special Issue
May 21, 2021: Notification of manuscript invitation for the Special Issue
July 17, 2021: Submission deadline of manuscripts for the Special Issue
June 2022: Publication of the Special Issue
If you would like to submit your abstract for consideration, please email your abstract and co-author contact information to the editorial office at hsr@aha.org, using the subject line “Special Issue on Translating Research into Policy and Action”.
The post *REMINDER* | HSR Special Issue Call for Abstracts: Translating Research into Policy and Action first appeared on The Incidental Economist.
April 21, 2021
Blood Clots, FDA Approval, and the AstraZeneca Covid Vaccine
There’s a lot of anxiety about the AstraZeneca vaccine thanks to recent reports of incomplete data, as well as reports on blood clot risks. Let’s take a look at both issues in context, understanding the efficacy data before and after numbers were updated, and understanding blood clot risk in relation to other common situations where blood clots are a potential concern.
The post Blood Clots, FDA Approval, and the AstraZeneca Covid Vaccine first appeared on The Incidental Economist.
What’s Behind the Growth in Alcohol Consumption?
The following originally appeared on The Upshot (copyright 2021, The New York Times Company) and was coauthored by Nambi Ndugga and Austin Frakt.
American deaths from misuse of substances, including alcohol, have increased over the past two decades, but not uniformly across various demographic groups.
Overall rates of alcohol abuse and related deaths have consistently and significantly increased for white non-Hispanic Americans, while Black Americans have experienced a much slower and less significant incline, and some other groups have had declines.
More recently, alcohol use has been up during the pandemic, with one study showing a greater increase in misuse among women than among men.
(For men, recommended limits are four drinks per day and 14 drinks per week, and for women, three drinks per day and seven drinks per week, according to the National Institute on Alcohol Abuse and Alcoholism.)
“Alcohol kills many more people than many may realize,” said Yusuf Ransome, an assistant professor at Yale’s School of Public Health. “It is a major contributor to deaths linked to physical injuries, interpersonal violence, motor vehicle crashes, self-harm and other harmful outcomes.”
One reason for this might be that alcohol is often viewed as socially acceptable. “Alcohol use has been normalized because it is consumed sometimes at family and communal gatherings, casual outings, and that’s the type of drinking that is typically seen or showed within the media,” he said. “We rarely see the long-term health impacts of excessive alcohol use, nor do we show the acute dangers of alcohol misuse and abuse.”
Between 2000 and 2016, according to research published in JAMA, alcohol-related deaths continually increased for white men (2.3 percent per year on average) and white women (4.1 percent), with middle-aged white Americans accounting for the highest increase in deaths. Rapid increases during this period in mortality related to alcohol and drugs like opioids among white Americans — particularly those without a college degree — have been termed “deaths of despair.”
The trend mirrors one experienced by Black Americans living in cities in the 1970s and 1980s. The underlying sources suggested by scholars are similar for the two groups, just shifted in time: social and economic stressors including poverty, stagnant or declining incomes, loss of blue-collar jobs, and disintegration of family units.
For Black Americans, there was the added problem of structural and explicit racism that contributed (and continues to contribute) to reduced economic opportunity and worse mental and physical health outcomes.
Rates of alcohol-related deaths among Black Americans declined somewhat in the early years of the 21st century, though they began to rise once more in 2007 (among women) and 2012 (among men). Nonetheless, the rate of alcohol-related death remains lower than among white Americans.
One factor might be a high sense of community and high levels of religious service attendance within the Black community, which have consistently been associated with both lower and less severe alcohol use. Another possible reason for lower rates of alcohol use among Black Americans is the well-founded sense that the possible downsides are more severe for them compared with other racial and ethnic groups. African-Americans are more likely to be policed and to suffer negative outcomes during their interactions with law enforcement, as evidenced over the past year and historically.
“African-Americans, particularly men and those of lower income, are at a higher risk of more social and legal consequences associated with drinking and other substance use,” said Tamika Zapolski, an associate professor of clinical psychology at Indiana University-Purdue University, Indianapolis. “They are more likely to experience negative health complications and be arrested and convicted.”
For example, one study found that Black (and Hispanic) drinkers are 1.5 times more likely to report adverse social consequences from drinking compared with their white non-Hispanic counterparts. These results support earlier findings of significant racial disparities in alcohol-related consequences. Some studies attribute this to increased policing in lower-income Black neighborhoods.
Native Americans have experienced the highest rates of alcohol-related deaths, which have been on the rise since 2000. According to a JAMA study, Native Americans’ alcohol misuse can be traced to “poverty, family history of alcohol use disorder, availability of alcohol at a younger age,” as well as stress from historical trauma. The death rate in 2016 was 113.2 per 100,000 for Native American men and 58.8 per 100,000 for Native American women.
For other groups per 100,000, the death rate was 4.4 and 1.0 for Asian-American and Pacific Islander men and women; 13.8 and 4.6 for Black men and women; 21.9 and 4.7 for Hispanic American men and women; and 18.2 and 7.6 for white men and women.
While there has been an overall increase in such deaths among Asian-Americans, the trends in alcohol consumption tend to diverge by national origin. Among Asian-American and Pacific Islander populations, U.S.-born individuals have higher rates of alcohol abuse than their first-generation immigrant counterparts, which may be because of cultural assimilation, among other factors.
The enculturation process may have also had an impact on young Hispanic women, who are experiencing an increase in alcohol consumption and have the third-highest rates of female alcohol-related deaths, after Native American and white women.
In the past two decades, women died of alcoholic liver disease on average two to three years earlier than men, even though they generally had longer life expectancies. During the pandemic, they have experienced a 41 percent increase in heavy drinking episodes, a survey study showed. (The C.D.C. definition of binge drinking for women is four or more drinks over two hours.)
“Over the past two decades, underage females were exposed to and suffered the effects of alcohol marketing,” said David Jernigan, professor of health law, policy and management at the Boston University School of Public Health, who has researched the relationship between alcohol marketing and consumption of alcohol.
“Specific products and product categories were created primarily for females: sweeter, fizzier, and marketed as more ‘feminine’ drinks,” he said.
More than boys and young men, girls and young women are drawn to so-called alcopops — flavored, often fruity, alcoholic beverages — fueling their popularity, according to one study. Women absorb more alcohol than men when drinking equivalent amounts because it takes longer for them to metabolize it, so the risk of harm is higher.
“We are seeing the consequences now, with increasing rates of cirrhosis and liver cancer deaths for women being the canary in the coal mine for a range of negative effects,” Professor Jernigan said.
The post What’s Behind the Growth in Alcohol Consumption? first appeared on The Incidental Economist.
April 17, 2021
The Infosphere as a SDOH: Leveraging Providers’ Influence to Counter Vaccine Misinformation
The following, which originally appeared on the Drivers of Health blog, is authored by Luke Testa, Program Assistant, The Harvard Global Health Institute.
In 2018, a short video circulated on WhatsApp claiming that the MMR vaccine was designed by Indian Prime Minister Narendra Modi to stop the population growth of Muslims. Subsequently, hundreds of madrassas across western Uttar Pradesh refused to allow health departments to vaccinate their constituents.
In 2020, a three-minute video claiming that the coronavirus vaccination campaign was secretly a plan by Bill Gates to implant trackable microchips in people was one of the most widely shared pieces of misinformation online. Alongside a torrent of online COVID-19 vaccine falsehoods and conspiracy theories, sources of medical mis- and disinformation are fostering distrust in COVID-19 vaccines, undermining immunization efforts, and demonstrating how poor information is a determinant of health.
Medical misinformation, referring to inaccurate or unverified information that can drive misperceptions about medical practices or treatments, has flooded the infosphere (all types of information available online). Examples can vary from overrepresentations of anecdotes claiming that complications occurred following inoculation to misinterpretations of research findings by well-meaning individuals.
Considering the many ways in which medical misinformation can shape health behaviors, researchers at the Oxford Internet Institute recently suggested that the infosphere should be classified as a social determinant of health (SDOH) (designated alongside general socioeconomic, environmental, and cultural conditions). This classification, they argue, properly accounts for the correlation between exposure to poor quality information and poor health outcomes.
The connection between information quality and health has been especially pronounced during the COVID-19 pandemic. A 2021 study found that amongst those who indicated that they would definitely take a COVID-19 vaccine, exposure to misinformation induced a decline in intent of 6.2% in the U.K. and 6.4% in the U.S. Further, misinformation that appeared to be science-based was found to be especially damaging to vaccination intentions. These findings are particularly concerning considering the fact that during the pandemic, the 147 biggest anti-vaccine accounts on social media (which often purport to be science-based) gained 7.8 million followers in the first half of 2020, an increase of 19%.
During an unprecedented health crisis, medical misinformation within the infosphere is leaving both individuals and communities vulnerable to poor health outcomes. Those who are unvaccinated are at a higher risk of infection and increase the likelihood of community transmission. This places undue burden on those who cannot get vaccinated—due to inequities and/or preexisting conditions—and increases opportunities for variants to continue to mutate into more infectious and/or deadly forms of the virus. Poor quality information within the infosphere is undermining immunization efforts and threatens to prolong the ark of the pandemic.
Leveraging Healthcare Provider Influence in the Battle Against Poor Quality Information
Healthcare providers are uniquely suited to respond to this challenge. Throughout the pandemic, majorities of U.S. adults have identified their doctors and nurses as the most trustworthy sources of information about the coronavirus. In fact, 8 in 10 U.S. adults said that they are very or somewhat likely to turn to a doctor, nurse, or other healthcare provider when deciding whether or not to get a COVID-19 vaccine.
This influence is especially pertinent considering the state of vaccine resistance across the globe. In March 2021, a Kaiser Family Foundation poll found that 37% of U.S. respondents indicated some degree of resistance to vaccination. If that percentage of Americans remain unvaccinated, the country will be short of what is needed to achieve herd immunity (likely 70% or more vaccinated). Similar levels of resistance to vaccination remain high in countries across the globe, such as Lebanon, Serbia, Paraguay, and France.
Although medical misinformation is contributing to high rates of refusal, it is important to note that drivers of vaccine resistance are complex and intersectional. Vaccine distrust or refusal may be rooted in exposure to anti-vaccine rhetoric, racial injustice or medical exploitation in healthcare, fears that vaccine development was rushed, and/or other drivers. For this reason, responses must be tailored to unique individual or communal motivations. For example, experts have pressed the critical need for vaccine distrust within Black communities to be approached not as a shortcoming of community members, but as a failure of health systems to prove themselves as trustworthy.
With regard to resistance rooted in anti-COVID-19 vaccine misinformation, healthcare providers are leveraging their unique influence through novel, grassroots approaches to encourage vaccine uptake. In North Dakota, providers are recording videos and sending out messages to their patients communicating that they have been vaccinated and explaining why it is safe to do the same. On social media, a network of female doctors and scientists across various social media pages, such as Dear Pandemic (82,000 followers) and Your Local Epidemiologist (181,000 followers), are collaborating to answer medical questions, clear up misperceptions about COVID-19 vaccines, and provide communities with accurate information about the virus. Similarly, the #BetweenUsAboutUs online campaign is elevating conversations about vaccines with Black doctors, nurses, and researchers in an effort to increase vaccine confidence in BIPOC communities. This campaign is especially critical considering the fact that BIPOC communities are often the target of anti-vaccine groups in an effort to exploit existing, rational distrust in health systems.
In addition to these timely responses, evidence-based interventions offer promising opportunities for healthcare providers to improve vaccine uptake amongst their patients. For example, there is a growing consensus around the practice of motivational interviewing (MI).
MI is a set of patient-centered communication techniques that aim to enhance a patient’s intrinsic motivation to change health behaviors by tapping into their own arguments for change. The approach is based on empathetic, nonjudgmental patient-provider dialogue. In other words, as opposed to simply telling a patient why they should get vaccinated, a provider will include the patient in a problem-solving process that accounts for their unique motivations and helps them discover their own reasons for getting vaccinated.
When applying MI techniques to a conversation with a patient who is unsure if they should receive a vaccine, providers will use an “evoke-provide-evoke” approach where they will ask patients: 1) what they already know about the vaccine; 2) if the patient would like additional information about the vaccine (if yes, then provide the most up to date information); and 3) how the new information changes how they are thinking or feeling about vaccination. During these conversations, the MI framework encourages providers to ask open-ended questions, practice reflective listening, offer affirmations, elicit pros and cons of change, and summarize conversations, amongst other tools.
Numerous studies show motivational interviewing to be effective in increasing vaccine uptake. For example, one randomized controlled trial found that with parents in maternity wards, vaccine hesitancy fell by 40% after participation in an educational intervention based on MI. Given its demonstrated effectiveness, MI is likely to help reduce vaccine hesitancy during the COVID-19 pandemic.
With infectious disease outbreaks becoming more likely and resistance to various vaccines increasing across the globe, continuing to leverage healthcare providers’ unique influence through grassroots campaigns while honing motivational interviewing skills as a way to combat mis- and disinformation in the infosphere may prove critical to advancing public health now and in the future.
The post The Infosphere as a SDOH: Leveraging Providers’ Influence to Counter Vaccine Misinformation first appeared on The Incidental Economist.
April 16, 2021
Dark Chocolate is not a Superfood
Dark chocolate has gained a health food reputation, but is the hype too good to be true? Is it possible that a daily dose of something so delicious can improve cognitive function and heart disease risk? Let’s take a look at the science – both the studies and how they were funded – and let’s take on the question of how most dark chocolate products are processed and what that means in terms of health.
The post Dark Chocolate is not a Superfood first appeared on The Incidental Economist.
April 12, 2021
Cancer Journal: Ontario on the Edge
The Cancer Journal is my story about being a cancer patient during the COVID-19 epidemic. In the last week, my cancer care halted because the pandemic is breaking Ontario’s health care system.
I’ll start with an update about my case. Since my radiation treatment ended in September, I’ve gotten two scans to determine whether the treatment actually worked. The initial computerized tomography (CT) scan showed that there were still significant masses at the sites of my tumour and its metastases. A follow-up positron emission tomography (PET) scan showed that these masses glowed in the image, a result consistent with them retaining living cancer cells. This was an unwelcome finding, to say the least.
I can’t get any more radiation, so I was referred to a surgeon. The surgeon, interestingly, was not impressed by the PET scan result, which he believes could be a false positive. He explained that those areas might be glowing because badly injured tissue does that. Or it might be cancer. So we need to biopsy these maybe-tumours and find out. This will not be a needle biopsy in an office, but rather a surgical procedure under anesthesia. And before the biopsy, I will need to get another CT scan, this time with radioactive contrast.
Of diagnostic procedures and their uncertainties, there is no end.
I had the CT scan last Thursday. I’ve read the radiologist’s report (and so far as I know, my surgeon hasn’t, so I may have misread it). The report’s notable finding was that an ulcer is forming at the site of my primary tumour. This is frightening, although again, for all I know, badly damaged yet not cancerous tissue might nevertheless ulcerate. Still, at least the presence of the ulcer explains my experience of continued and, in fact, growing throat pain at the site of the primary tumour. All this will, I hope, be clarified by my biopsy, which according to my surgeon’s administrator, is going to be scheduled for next week.
Or is it? Because now we return to the larger story of the pandemic. On Thursday, April 8, Ontario began its third shut down in response to a third wave of the epidemic. As you can see from the graph, the counts of COVID-19 cases are rapidly approaching their highest levels.
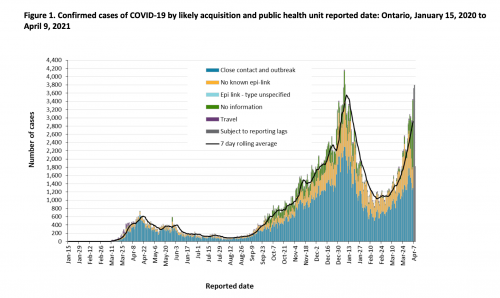
COVID-19 cases in Ontario, Canada.
Why are there so many cases in Ontario? First, Canada is several weeks behind the US in vaccination (see this great graph by @TrevorTombe).
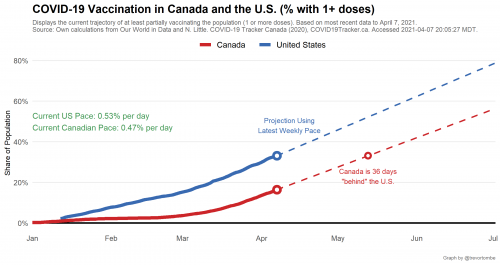
Cumulative vaccination rates in Canada and the US.
As of this morning, only 18.5% of Canadians have received at least one dose. I am not one of them, nor do I have a scheduled visit. In Ontario, you register online to be vaccinated and then wait for them to contact you. My phone hasn’t rung.
Why are fewer Canadians vaccinated? I see no evidence that vaccine hesitancy is greater than in the US. My impression is that, in general, Canadians have been more compliant with public health warnings than Americans. According to Tracey Lindeman, we negotiated a bad deal with the manufacturers.
Without much domestic manufacturing capacity to speak of, Canada had to sign advance-purchase deals with international vaccine companies. The country hedged its bet by mostly going with companies funded by Operation Warp Speed, and so far its strategy has been to overbuy doses in the hopes of securing enough to vaccinate all of its citizens. A mounting critique, however, is that perhaps Canada should have been more specific than “first quarter of 2021” in terms of arranging vaccine-delivery timing. [Toronto Globe & Mail health columnist André] Picard said that Canada, by not giving manufacturers a specific week, or even day, allowed them to push delivery until the outer limit of the quarter.
So why have the Pharma companies placed us at the end of the line for deliveries? Quoting a retired Pharma executive, Lindeman says that
long-standing Canadian policies in three areas [have been] particularly antagonistic to vaccine makers, especially multinationals: patents, prices, and procurement.
Perhaps so, but you could see this another way. Unlike the US, Canadians have bargained hard with the Pharma multinationals to get essential medications at reasonable prices. And now… this is their payback.
Another reason why cases have risen is that coronavirus is evolving, and at least some of the new variants have a substantially higher transmission rate than the earlier coronavirus. The faster spreading new variants will displace the older variants among new cases, and, everything else being equal, accelerate the growth in cases. As you can see in the following graph, the variant viruses have spread rapidly and now comprise 70% of new cases.
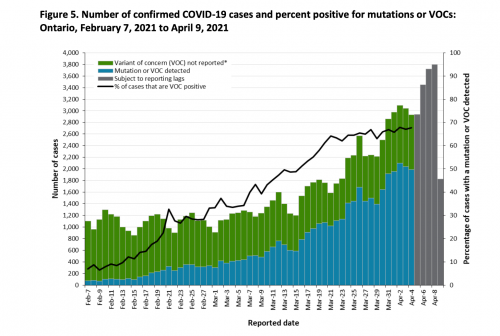
Infections with variant viruses as a proportion of total cases in Ontario.
The upshot of the wave of cases is that the number of COVID-19 cases in Ontario hospitals is growing, as you can see from this graph, which I found in @thevivafrei’s Twitter feed.

Increases over time in hospitalized and critical care COVID cases.
Unfortunately, I can’t find a data series that expresses these case counts as a percentage of the province’s total bed or ICU capacity. My spouse participates in daily briefings about hospital capacity, and what she hears from the provincial Ministry of Health is that in many hospitals, both acute and critical care beds are at greater than 100% capacity. That means that all the standard beds are filled and patients are being cared for on gurneys. See my earlier post on ‘hallway medicine.’
If so, this is a dangerous situation. During this pandemic wave, the rate of COVID-19 deaths seems to be lower than during previous waves, possibly because the patients are younger this time. Nevertheless, people in ICUs are there for a reason: they are more likely to die if they are less closely monitored and receive less aggressive care. Unfortunately, cases requiring hospitalization are proliferating, and available beds are not. If the overcrowding gets worse, death rates among both COVID-19 and non-COVID-19 hospitalized patients are likely to rise. This is the precarious edge on which the province stands.
To stem the rise in cases, the government of Ontario declared its third shutdown on Thursday. Likewise, the hospital where I have been getting my cancer care announced that it was cancelling elective surgeries. This is not due to a lack of surgeons or a lack of operating rooms. (However, I expect there is a shortage of surgical nurses due to their secondment to other COVID-related tasks.) The problem is that surgeries require hospital beds for post-operative care, including ICU beds for acutely ill patients. In effect, surgeries compete with COVID-19 for hospital beds. The upshot is that if you have a moving vehicle accident and you need a procedure right now, they will operate. Otherwise, you will wait. I’m fairly certain that they will cancel my biopsy. If so, this will delay any eventual surgery to attack my throat cancer.
So, what is it like to be a cancer patient during the COVID pandemic? Right now, it means that I cannot get the care I need. I am going to try to get more information this week about how long I can expect to wait. If it’s a long wait, or if I can’t get an answer, then I will need to explore whether I can get care in another province or, irony of ironies, in the States.
To read the Cancer Posts from the start, please begin here.
The post Cancer Journal: Ontario on the Edge first appeared on The Incidental Economist.
Aaron E. Carroll's Blog
- Aaron E. Carroll's profile
- 42 followers



