Aaron E. Carroll's Blog, page 35
August 30, 2021
HSR Special Issue on Health Equity: A Call for Abstracts

Health Services Research (HSR) is planning a special issue with the Catholic Health Association of the United States on the theme of health care equity, to be edited by Alexander Ortega, PhD, with guest editors Nate Hibner, PhD, Brian Kane, PhD, and Tanjala
Purnell, PhD.
The goal of this special issue is to feature studies that are not merely descriptive but instead focus on new methods, measures, practices, policies, theories, observations, or insights that will allow the field to better understand the causes, consequences, and solutions to eliminating health care inequities.
With a wide lens on the many inequities that exist (racial/ethnic, insurance status, socioeconomic, age, rural/urban, LGBTQ, disability, immigrant, etc.), we invite abstracts that highlight successes and barriers towards understanding and achieving health care equity. Observational studies, qualitative studies, natural experiments, interventions, evaluations, and systematic reviews are welcome. We invite researchers across many disciplines, across academia, professional societies, and health care institutions. The editors will favor articles that are action oriented, with evidence that will inform policies and practices to eliminate health care inequities.
Submitted abstracts will be evaluated by a multidisciplinary and interprofessional review panel, which will prioritize the best abstracts to receive invitations to submit full manuscripts. The evaluation criteria will include: (1) quality, rigor and originality; (2) relevance to the special issue theme, articulated above; and (3) clarity of writing and presentation. Invited manuscripts submitted for the Special Issue will first undergo the same HSR peer review process as all regular manuscripts.
Abstracts are due October 15, 2021. Full details about the issue and how to format and submit your abstract are found here and are also posted on the HSR website.
The post HSR Special Issue on Health Equity: A Call for Abstracts first appeared on The Incidental Economist.August 26, 2021
Acetaminophen, ADHD, and Autism

You’ve probably heard before that acetaminophen during pregnancy is associated with symptoms of ADHD and Autism in offspring. Well, we’ve got another study on that association. In today’s episode, we examine that study and revisit why we need to be cautious with observational data.
The post Acetaminophen, ADHD, and Autism first appeared on The Incidental Economist.
Recent publications from Boston University’s Department of Health Law, Policy and Management: Bonus August 2021 Edition

Below are recent publications from Boston University’s Department of Health Law, Policy and Management. You can find all posts in this series here.
August 2021 Edition #2 (Bonus!)
Apaydin EA, Rose DE, Yano EM, Shekelle PG, Stockdale SE, Mohr DC. Gender Differences in the Relationship Between Workplace Civility and Burnout Among VA Primary Care Providers. J Gen Intern Med. 2021 Apr 26. PMID: 33904049. Online ahead of print.
Beachler DC, Taylor DH, Anthony MS, Yin R, Li L, Saltus CW, Li L, Shaunik A, Walsh KE, Rothman KJ, Johannes CB, Aroda VR, Carr W, Goldberg P, Accardi A, O’Shura JS, Sharma K, Juhaeri J, Lanes S, Wu C. Development and validation of a predictive model algorithm to identify anaphylaxis in adults with type 2 diabetes in U.S. administrative claims data. Pharmacoepidemiol Drug Saf. 2021 Jul; 30(7):918-926. PMID: 33899314. Epub 2021 May 5.
Becker SJ, Scott K, Elwy AR. You have an effective brief intervention (BI) for young adults, now what? Concrete strategies to advance BI implementation in usual care settings. Psychol Addict Behav. 2021 May 03. PMID: 33939446.
Bokhour BG, Bolton RE, Asch SM, Dvorin K, Fix GM, Gifford AL, Hyde JK, McInnes DK, Parker VA, Richardson K, Skolnik AA, Vaughan-Sarrazin MS, Wu J, Ohl ME. How Should We Organize Care for Patients With Human Immunodeficiency Virus and Comorbidities? A Multisite Qualitative Study of Human Immunodeficiency Virus Care in the United States Department of Veterans Affairs. Med Care. 2021 Aug 1. PMID: 33900271.
Bosch NA, Crable EL, Ackerbauer KA, Clark K, Drainoni ML, Grim V, Ieong MH, Walkey AJ, Murphy J. Implementation of a Phenobarbital-based Pathway for Severe Alcohol Withdrawal: A Mixed-Methods Study. Ann Am Thorac Soc. 2021 May 04. PMID: 33945771. Online ahead of print.
Bosch NA, Teja B, Wunsch H, Walkey AJ. Practice Patterns in the Initiation of Secondary Vasopressors and Adjunctive Corticosteroids during Septic Shock in the US. Ann Am Thorac Soc. 2021 May 11. PMID: 33975530. Online ahead of print.
Buchholz I, Feng YS, Buchholz M, Kazis LE, Kohlmann T. Translation and adaptation of the German version of the Veterans Rand-36/12 Item Health Survey. Health Qual Life Outcomes. 2021 May 04; 19(1):137. PMID: 33947411.
Christopher PP, Stewart C, Manning W, Anderson BJ, Woodruff A, Monteiro J, Stein MD. Risk behaviors among persons civilly committed for opioid use. J Subst Abuse Treat. 2021 May 28; 132:108493. PMID: 34098213. Online ahead of print.
Connolly SL, Gifford AL, Miller CJ, Bauer MS, Lehmann LS, Charness ME. Provider Perceptions of Virtual Care During the Coronavirus Disease 2019 Pandemic: A Multispecialty Survey Study. Med Care. 2021 Apr 28. PMID: 34009880.
Crable EL, Feeney T, Harvey J, Grim V, Drainoni ML, Walkey AJ, Steiling K, Thurston Drake F. Re: Augmenting Follow-up of Incidental Findings. J Am Coll Radiol. 2021 Apr 28. PMID: 33932345. Online ahead of print.
Crosby SS, Sonis L, Annas GJ. The Boston Medical Center Immigrant Task Force: An Alternative to Teaching Immigration Law to Health Care Providers. J Law Med Ethics. 2021; 49(1):59-63. PMID: 33966656.
Drainoni ML, Biancarelli D, Jansen E, Bernstein J, Joseph N, Eun TJ, Fenton AHTR, Clark JA, Hanchate A, Legler A, Schuch TJ, Leschly K, Perkins RB. Provider and Practice Experience Integrating the Dose-HPV Intervention into Clinical Practice. J Contin Educ Health Prof. 2021 May 10. PMID: 33973928. Online ahead of print.
Eck RH, Trangenstein PJ, Siegel M, Jernigan DH. Company-Specific Revenues From Underage Drinking. J Stud Alcohol Drugs. 2021 May; 82(3):368-376. PMID: 34100705.
Fantasia KL, Stockman MC, Ju Z, Ortega P, Crable EL, Drainoni ML, Walkey AJ, Bergstrom M, O’Brien K, Steenkamp D. Professional continuous glucose monitoring and endocrinology eConsult for adults with type 2 diabetes in primary care: Results of a clinical pilot program. J Clin Transl Endocrinol. 2021 Mar; 24:100254. PMID: 33898271. Online ahead of print.
Garcia MA, Rucci JM, Thai KK, Lu Y, Kipnis P, Go AS, Desai M, Bosch NA, Martinez A, Clancy H, Devis Y, Myers LC, Liu VX, Walkey AJ. Association Between Troponin I Levels During Sepsis and Post-Sepsis Cardiovascular Complications. Am J Respir Crit Care Med. 2021 May 26. PMID: 34038701.
Garvin LA, Hu J, Slightam C, McInnes DK, Zulman DM. Use of Video Telehealth Tablets to Increase Access for Veterans Experiencing Homelessness. J Gen Intern Med. 2021 May 23. PMID: 34027612. Online ahead of print.
Grammer AC, Vázquez MM, Fitzsimmons-Craft EE, Fowler LA, Rackoff GN, Schvey NA, Lipson SK, Newman MG, Eisenberg D, Taylor CB, Wilfley DE. Characterizing eating disorder diagnosis and related outcomes by sexual orientation and gender identity in a national sample of college students. Eat Behav. 2021 May 15; 42:101528. PMID: 34049053. Online ahead of print.
Kållberg C, Hudson J, Salvesen Blix H, Årdal C, Klein E, Lindbæk M, Outterson K, Røttingen JA, Laxminarayan R. The effect of generic market entry on antibiotic prescriptions in the United States. Nat Commun. 2021 05 18; 12(1):2937. PMID: 34006862.
Martinez RN, Smith BM, Etingen B, Houston TK, Shimada SL, Amante DJ, Patterson A, Richardson LM, Vandenberg G, Cutrona SL, Quintiliani LM, Frisbee KL, Hogan TP. Health-Related Goal Setting and Achievement Among Veterans with High Technology Adoption. J Gen Intern Med. 2021 May 07. PMID: 33963510.
Miller CJ, Sullivan JL, Harvey KLL, Williamson AK, Stadnick NA. Promoting high-functioning mental health treatment teams in the context of low staffing ratios. Health Care Manage Rev. 2021 May 27. PMID: 34038917. Online ahead of print.
Morgan JR, Walley AY, Murphy SM, Chatterjee A, Hadland SE, Barocas J, Linas BP, Assoumou SA. Characterizing initiation, use, and discontinuation of extended-release buprenorphine in a nationally representative United States commercially insured cohort. Drug Alcohol Depend. 2021 May 21; 225:108764. PMID: 34051547.
Ogden SN, Harris MT, Childs E, Valente PK, Edeza A, Collins AB, Drainoni ML, Mimiaga MJ, Biello KB, Bazzi AR. “You need money to get high, and that’s the easiest and fastest way:” A typology of sex work and health behaviours among people who inject drugs. Int J Drug Policy. 2021 May 10; 103285. PMID: 33985886.
Park TW, Sikov J, dellaBitta V, Saitz R, Walley AY, Drainoni ML. “It could potentially be dangerous… but nothing else has seemed to help me.”: Patient and clinician perspectives on benzodiazepine use in opioid agonist treatment. J Subst Abuse Treat. 2021 Apr 30; 131:108455. PMID: 34098286.
Pletta DR, Kant JD, Ehrensaft D, MacNish M, Cahill S, Katz-Wise SL. The 2016 United States presidential election’s impact on families with transgender adolescents in New England. J Fam Psychol. 2021 May 27. PMID: 34043404. Online ahead of print.
Pytell JD, Sklar MD, Carrese J, Rastegar DA, Gunn C, Chander G. “I’m a Survivor”: Perceptions of Chronic Disease and Survivorship Among Individuals in Long-Term Remission from Opioid Use Disorder. J Gen Intern Med. 2021 May 23. PMID: 34027611. Online ahead of print.
Ross CS, Babor TF, Bartholow BD, DeJong W, Fitzgerald N, Jackson KM, Jernigan DH, Naimi TS, Noel JK, Petticrew M, Severi K, Siegel MB, Stockwell T, Tori M, Xuan Z. Call to restore funding to monitor youth exposure to alcohol advertising. Addiction. 2021 May 31. PMID: 34060173. Online ahead of print.
Shafer PR, Garrido MM, Pearson E, Palani S, Woodruff A, Lyn AM, Williams KM, Kirsh SR, Pizer SD. Design and implementation of a cluster randomized trial measuring benefits of medical scribes in the VA. Contemp Clin Trials. 2021 May 25; 106:106455. PMID: 34048944.
Simmons M, Kim B, Hyde J, Lemon TL, Scharer KE, McInnes DK. Protecting the Public’s Health Through Successful Reentry for Sex Offender After Incarceration. J Interpers Violence. 2021 May 26; 8862605211016344. PMID: 34039087. Online ahead of print.
Sprague Martinez L, Davoust M, Rajabiun S, Baughman A, Bachman SS, Bowers-Sword R, Campos Rojo M, Sullivan M, Drainoni ML. “Part of getting to where we are is because we have been open to change” integrating community health workers on care teams at ten Ryan White HIV/AIDS program recipient sites. BMC Public Health. 2021 05 14; 21(1):922. PMID: 33990190.
Vranceanu AM, Bakhshaie J, Reichman M, Doorley J, Elwy AR, Jacobs C, Chen N, Esposito J, Laverty D, Matuszewski PE, Fatehi A, Bowers LC, Harris M, Ring D. A Live Video Program to Prevent Chronic Pain and Disability in At-Risk Adults With Acute Orthopedic Injuries (Toolkit for Optimal Recovery): Protocol for a Multisite Feasibility Study. JMIR Res Protoc. 2021 Apr 28; 10(4):e28155. PMID: 33908886.
Wang BB, Patel KF, Wolfe AE, Wiechman S, McMullen K, Gibran NS, Kowalske K, Meyer WJ, Kazis LE, Ryan CM, Schneider JC. Adolescents with and without head and neck burns: comparison of long-term outcomes in the burn model system national database. Burns. 2021 Apr 20. PMID: 33975762.
Young GJ, Zepeda ED, Flaherty S, Thai N. Hospital Employment Of Physicians In Massachusetts Is Associated With Inappropriate Diagnostic Imaging. Health Aff (Millwood). 2021 05; 40(5):710-718. PMID: 33939515.
The post Recent publications from Boston University’s Department of Health Law, Policy and Management: Bonus August 2021 Edition first appeared on The Incidental Economist.August 25, 2021
The Delta Variant and Vaccine Protection

What’s the deal with Covid variants? How well do the different Covid vaccines protect against them? Today we’ll tell you about the several variants, including the Delta variant that is prevalent in the US, and we’ll talk about the studies that have looked at vaccine efficacy against these variants.
The post The Delta Variant and Vaccine Protection first appeared on The Incidental Economist.
August 16, 2021
Alcoholics Anonymous vs Other Treatments

Alcoholics Anonymous has long been a treatment for alcoholism, and many, many addiction experts and people in recovery swear by the 12 step process. But what does the research show? How does AA stack up against other treatments for alcohol abuse disorder? There have been several high quality studies in recent years, and in this video Aaron will explain what they mean.
The post Alcoholics Anonymous vs Other Treatments first appeared on The Incidental Economist.Optimism bias exists among teens who vape

Cecille Joan Avila is a policy analyst at Boston University School of Public Health. She tweets @cecilleavila.
Rates of combustible cigarette use have decreased over the years, but the rate of United States teenagers vaping or using e-cigarettes has recently increased. Perhaps this is because e-cigarettes are aesthetically enticing or come in fun flavors, or because many teenagers believe vaping is less dangerous and less addictive than smoking – although many e-cigarettes having comparable nicotine levels and absorption rates as traditional cigarettes. Another possible reason? Optimism bias.
Optimism bias is when an individual over-estimates their ability to quit an activity when compared to others. (This is despite believing they might still succumb to addiction.) Optimism bias is well documented when it comes to combustible cigarettes among adults, but there is limited research about e-cigarette use among youth.
Youth are arguably most at-risk for lifetime nicotine addiction, particularly if they perceive vaping to be easier to quit and are more enticed to start. Thus, more research exploring the role optimism bias plays in teen vaping behavior is critical.
Study Design
A recently published paper examines optimism bias in quitting vaping, specifically among youths aged 14 to 18 who were aware of e-cigarettes, and factors that might affect their optimism bias.
(Author affiliations for this paper include Kiersten Strombotne, Department of Health Law, Policy and Management at Boston University School of Public Health and Partnered Evidence-based Policy Resource Center, VA Boston Healthcare System; Jody Sindelar, Department of Health Policy and Management, Yale School of Public Health; and John Buckell, Health Economics Research Center, Nuffield Department of Population Health and Health Behaviours and Department of Primary Care Health Sciences, University of Oxford.)
The researchers conducted a nationally representative, online, cross-sectional survey in December 2018. Considering previous research on combustible cigarettes, they hypothesized that individuals would be more optimistic about their own ability to quit, while believing others would likely have a harder time, with perceived difficulty quitting increasing with social relationship distance.
Along with collecting demographic data, the survey measured optimism bias by asking respondents (N=1,610) how they perceived their own ability to quit vaping and how well they thought others would be able to quit vaping. Respondents were asked to rate the ability to quit for someone as close as their best friend, all the way to a distant but age-similar teenager.
Researchers analyzed this data not only to determine the extent to which optimism bias existed in this sample, but also to gain insight on how optimism bias was formed and what factors impacted it. Descriptive statistics were used to determine how much optimism bias existed in this study population. A regression model (ordinary least squares) was then used to examine what factors went into youth optimism bias.
Findings
Among the study population, the average age of respondents was 16 years, mostly suburban and white, 49% female, and 48% who reported being a free or reduced lunch recipient (a variable used as a proxy for socioeconomic status). Thirty-eight percent reported ever having tried e-cigarettes, and 37% reported having ever tried JUUL.
As expected with their hypotheses, researchers found that individuals were more optimistic about their ability to quit vaping than others’ ability. Results showed that as social relationship distance increased, so did an individual’s perceived difficulty of another person’s ability to quit.
Meanwhile, actual use of e-cigarettes and JUUL were associated with lower optimism bias, although findings related to e-cigarettes were not statistically significant. Optimism bias also decreased with reports of smoking in the last 30 days, if a respondent was Black or Hispanic, and if a respondent reported receiving free or reduced lunch.
This research is limited in that it may not be generalizable outside of this age group and, due to its cross-sectional design, causality cannot be determined. Also, because it is impossible to know how likely a respondent would be able to quit if they tried, reported perception cannot be compared to an actual attempt.
Next Steps
It’s critical to prevent teens from vaping before they even start – no matter how high their optimism bias is. Considering that Black and Hispanic youths and those of lower socioeconomic status generally report lower optimism bias, focusing on outright prevention could also have significant impact on nicotine use disparities. A more tailored approach that accounts for nuances in optimism bias may be more effective, such as targeting how difficult it is to quit vaping in general.
This research adds to the literature by providing evidence that optimism bias exists among youths as it pertains to vaping. It has significant policy implications, especially for targeting youths at a critical point: before they even initiate use of an addictive substance. Specific state or federal policies could include bans on appealing flavors, taxes on e-cigarettes, or even purchasing age restrictions, with all three options possibly preventing teens from even starting.
Although it will take considerable effort to change public behavior and perception, more research like this is needed to show what areas we can better target to address issues associated with vaping. While it might be a difficult challenge to curb the rapid rates of youth vaping, it is a doable one, considering how perception towards combustible cigarettes changed over time.
The post Optimism bias exists among teens who vape first appeared on The Incidental Economist.August 10, 2021
Use of Coercive Measures Linked to Organizational Climate and Morale

Alex Woodruff, MPH, is a Health Science Specialist at the Boston VA Healthcare System. He tweets at @aewoodru.
The use of restraints and seclusion is a long standing, yet controversial, measure for patients hospitalized in psychiatric settings. Reducing the unnecessary use of these interventions is imperative for patient health.
Restraint and seclusion fall under the umbrella of “coercive measures,” and are often used to address self-harm or violent behavior. But the use of these measures varies widely, suggesting that these criteria are subject to interpretation and may sometimes be used unnecessarily. The unnecessary use of coercive measures is problematic — they can be traumatizing to the patient, undermine effective psychiatric treatment, and are ethically suspect.
Reducing use of these practices to only when absolutely necessary is a priority for the treatment of psychiatric disorders. Research to date has suggested that a number of factors, such as staffing, internal policies, and leadership are linked to the use of these coercive measures. But new research highlights that clinicians’ morale and workplace culture are other factors to consider.
Study Design
Dr. Ekaterina Anderson, a health services researcher with the Center for Healthcare Organization and Implementation Research (CHOIR) at the VA Bedford Healthcare System, and colleagues from Boston Universities School of Medicine and School of Public Health, Department of Health Law, Policy and Management, UMASS Worcester, and UCLA analyzed Veterans Health Administration (VHA) data to better understand the impact of clinician morale and organizational climate on physical restraint and seclusion use in inpatient psychiatric units.
The study uses data from the All Employee Survey (AES), a survey routinely used by VHA to capture employee perceptions of organizational climate and well-being, and Centers of Medicare and Medicaid Services data on seclusion and restraint hours for VHA facilities in 2014 – 2016. The sampling of AES survey responses was focused to include those with direct inpatient psychiatric patient contact and those who could be involved in issuing seclusion and restraint orders (psychiatrists, registered nurses, or licensed practical nurses).
The AES measures included in the analysis were perceptions of burnout, engagement (sense of connection with one’s work), psychological safety (a sense of comfort with speaking up about issues in one’s workgroup), relational climate (a positive perception of teamwork and conflict resolution), and workload (a perception that one’s workload is reasonable). The CMS data for each VHA facility included the total average number of hours (per 1,000 patient hours) that patients in inpatient psychiatric units were maintained in physical restraints or held in seclusion. Using a Poisson model, restraint and seclusion hours were regressed on measures of clinician morale and workplace climate. The models also included covariates that could potentially have an influence on use of seclusion and restraint, such as average length of stay, patients per unit, and geography.
Findings
On average, facilities had a total of 0.33 restraint hours per month and 0.31 seclusion hours per month, although many sites used neither. The use of physical restraint in an inpatient psychiatric unit was associated with a number of factors. Facilities with higher rates of burnout were significantly more likely to report greater use of physical restraints, while those with greater ratings of psychological safety, relational climate, and employee engagement were significantly more likely to report lower rates of physical restraint use.
A different relationship was observed between seclusion and workplace attitudes. Greater psychological safety and relational climate were significantly associated with increased use of seclusion. There were also strong, but non-significant, relationships between the increased use of seclusion with lower burnout, as well as higher engagement.
Discussion
This study highlights an important relationship between organizational factors in inpatient psychiatric units and the use of coercive measures — particularly, that the use of these measures may be impacted by the clinical work environment. There are a number of explanations for the relationship between higher physician burnout and the use of restraints presented in the paper. For example, clinicians with higher burnout may be less empathetic towards patients engaging in disruptive behavior or may have less perceived or actual ability to deescalate disruptive patients. Conversely, units with higher psychological safety and workplace engagement may be more competent at conflict de-escalation and communicating about appropriate treatment expectations.
Unlike using restraints, staff who reported lower burnout and increased workplace safety also reported more seclusion hours. One possible explanation the authors provided is that staff with low burnout and increased workplace safety may consider the use of seclusion as a safe alternative to using restraints.
The authors note that that these findings may be limited by differences in clinic definitions of seclusion. Another limitation of the study is that there may be potential confounders that impact restraint and seclusion that are unobserved in this dataset. Additionally, because this study does not determine causality, it’s possible that the use of mechanical restraint and seclusion are driving poor clinician morale and organizational climate.
While this study was isolated to the impacts of clinician morale and organizational climate in psychiatric units, there are broader implications for these findings. Coercive measures are used across a variety of medical and social support systems. From similar uses of restraints, such as in police or emergency services settings, to alternative uses of coercive measures, such as restrictive child protection orders, there are many instances where the use of potentially damaging coercive measures could be influenced by workplace environments.
Teasing out all the factors that go into whether or not a psychiatric unit appropriately uses restraints can help health care regulators, administrators, and providers ensure that they are prioritizing patient safety. Focusing resources on organizational climate and morale may be key in interventions aimed at reducing the use of coercive measures.
The post Use of Coercive Measures Linked to Organizational Climate and Morale first appeared on The Incidental Economist.August 4, 2021
How to jump start a 2021 Toyota Rav4 Prime
My family recently purchased a 2021 Toyota Rav4 Prime. As I became familiar with it, and flipped through the owner’s manual a few times, it occurred to me that nowhere in the manual were instructions for how to jump start it.
I did what any normal person would do these days and searched the internet. No instructions there either. (Some for Rav4 hybrids, but not the Prime. Maybe the instructions are the same, but I don’t know! I also found recommendations to never jump start someone else’s car with a Rav4 Prime. Fine, I won’t. But what about jumping mine?)
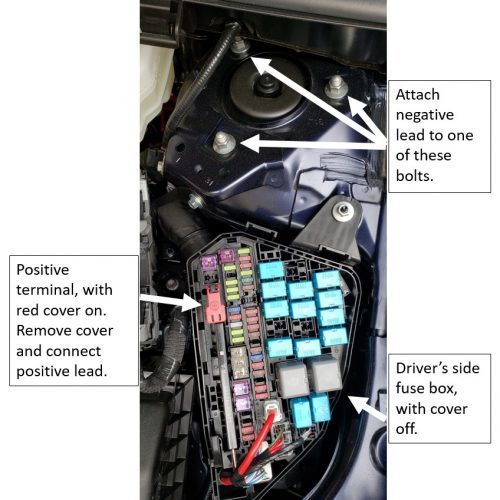
So, I texted the very friendly and helpful sales agent at Expressway Toyota in Boston who sold me the car and he told me how to do it. To fill the gap in the internet, here are his instructions by video (low res, but good enough). Below that is an image I created that includes all you really need.
Here’s what he’s talking about in a still image:
The post How to jump start a 2021 Toyota Rav4 Prime first appeared on The Incidental Economist.August 3, 2021
Rest in Peace, Tony. Please forgive us all.

My brother-in-law Vincent lives with an intellectual disability called fragile X syndrome. For more than a decade, he has lived in various group homes in Chicago’s south suburbs where we live. On Sunday, Vincent and I went to Walmart. By chance, we encountered one of his favorite staff members from a previous home. She told me that Vincent’s former housemate Tony recently passed away.

Statue, Homewood Memorial Gardens, Homewood, Illinois.
I knew Tony pretty well. As I perceived him, he possessed a noticeably higher IQ than most of his peers and housemates. He suffered from some sort of communication disorder. Frustrated by his inability to verbally connect, he would say hi or make requests for a hamburger by scribbling on scraps of paper and shove these in the faces of the house staff. The staff sometimes found this annoying. They didn’t always respond well.
I enjoyed Tony. We would schmooze when I visited. Ironically, I was pondering his unmet needs as I wrote a piece, with Kenton Johnston and Hefei Wen, for Milbank Quarterly last week about on disparities and disabilities. We discussed many things, including the awkward intersectional reality of socio-economic disparities within the disability community itself.
I always thought Tony could have had a different life—a better life—had he been given access to the right technologies and supports, and that this would have been more likely had he received services through more richly-resourced, and thus more-proficient, organizations on Chicago’s north side or within Chicagoland’s most affluent suburbs.
I wanted to buy Tony an iPad with software specifically developed for folk with IDD. That might have made a difference in his life. Of course, I never did. That would have crossed many boundaries. I had no way to make sure that he would have the proper training to use it, or that others would be in a position to support him in that.
I believe both the equipment and the human supports would have been more available had he received services at a group home or at an institution in the ritzier parts of Chicagoland. Or if he were born twenty years later than he was.
Men such as Tony spend their lives trying hard to make connections with people, to escape the quiet imprisonment of their conditions. I wish I had done more to help him. Life being what it is, Vinnie moved on. Tony and I lost touch.
Particularly during this COVID time of trial for so many people with disabilities, I’ve quite often been thinking about the shadows cast by surrounding lives along our journey with Vincent. We meet many people with biographies and struggles analogous to Tony’s. One tough aspect of disability caregiving is the sense of bystander moral injury. We cross paths with so many whose lives are not what they could or should be.
Rest in Peace, man. May your memory be a blessing. Please forgive us all for not giving you the life that you so richly deserved, and might well have had.
The post Rest in Peace, Tony. Please forgive us all. first appeared on The Incidental Economist.August 2, 2021
Recent publications from Boston University’s Department of Health Law, Policy and Management: August 2021 Edition

Below are recent publications from me and my colleagues from Boston University’s Department of Health Law, Policy and Management. You can find all posts in this series here.
August 2021 Edition
Anderson E, Mohr DC, Regenbogen I, Swamy L, Smith EG, Mourra S, Rinne ST. Influence of Organizational Climate and Clinician Morale on Seclusion and Physical Restraint Use in Inpatient Psychiatric Units. J Patient Saf. 2021 Apr 16. Online ahead of print. PMID: 33871417.
Beesley SJ, Sorensen J, Walkey AJ, Tonna JE, Lanspa MJ, Hirshberg E, Grissom CK, Horne BD, Burk R, Abraham TP, Paine R, Brown SM. Long-Term Implications of Abnormal Left Ventricular Strain During Sepsis. Crit Care Med. 2021 Apr 1;49(4):e444-e453. PMID: 33591007.
Beitler JR, Walkey AJ. The Staying Power of Pressure- and Volume-limited Ventilation in Acute Respiratory Distress Syndrome. Am J Respir Crit Care Med. 2021 Apr 23. Online ahead of print. PMID: 33891827.
Bindman AB, Frakt A. From the Editors’ desk: Publishing in HSR. Health Serv Res. 2021 Apr; 56(2):173-174. PMID: 33730764.
Bosch NA, Rucci JM, Massaro JM, Winter MR, Quinn EK, Chon KH, McManus DD, Walkey AJ. Comparative Effectiveness of Heart Rate Control Medications for the Treatment of Sepsis-Associated Atrial Fibrillation. Chest. 2021 Apr; 159(4) 1452-1459. PMID: 33619010.
Burke NL, Hazzard VM, Karvay YG, Schaefer LM, Lipson SK, Rodgers RF. Eating disorder prevalence among multiracial US undergraduate and graduate students: Is multiracial risk different than the sum of each identity? Eat Behav. 2021 Apr;41:101501. PMID: 33798830.
Ellison J, Cole MB, Hanchate AD, Kazis L, Lindsay S. Nonindicated pelvic examinations during contraceptive encounters: Prevalence and provider variations. Contraception. 2021 Apr; 103(4):239-245. PMID: 33373613.
Fitzsimmons-Craft EE, Taylor CB, Newman MG, Zainal NH, Rojas-Ashe EE, Lipson SK, Firebaugh ML, Ceglarek P, Topooco N, Jacobson NC, Graham AK, Kim HM, Eisenberg D, Wilfley DE. Harnessing mobile technology to reduce mental health disorders in college populations: A randomized controlled trial study protocol. Contemp Clin Trials. 2021 Apr;103:106320. PMID: 33582295.
Freibott CE, Phillips KT, Anderson BJ, Stewart C, Liebschutz JM, Stein MD. Under the Skin: The Relationship Between Subcutaneous Injection and Skin Infections Among People Who Inject Drugs. J Addict Med. 2021 Apr 02. Online ahead of print. PMID: 33813580.
Hahn SL, Bauer KW, Kaciroti N, Eisenberg D, Lipson SK, Sonneville KR. Relationships between patterns of weight-related self-monitoring and eating disorder symptomology among undergraduate and graduate students. Int J Eat Disord. 2021 Apr;54(4):595-605. PMID: 33399230.
Hazzard VM, Ziobrowski HN, Borg SL, Schaefer LM, Mangold AC, Herting NA, Lipson SK, Crosby RD, Wonderlich SA. Past-Year Abuse and Eating Disorder Symptoms Among U.S. College Students. J Interpers Violence. 2021 Apr 01; 8862605211005156. Online ahead of print. PMID: 33794702.
Holliday R, Liu S, Brenner LA, Monteith LL, Cappelletti MM, Blosnich JR, Brostow DP, Gelberg L, Hooshyar D, Koget J, McInnes DK, Montgomery AE, O’Brien R, Rosenheck RA, Strickland S, Workman GM, Tsai J. Preventing Suicide Among Homeless Veterans: A Consensus Statement by the Veterans Affairs Suicide Prevention Among Veterans Experiencing Homelessness Workgroup. Med Care. 2021 Apr 01; 59(Suppl 2):S103-S105. PMID: 33710080.
Jackson GL, Cutrona SL, White BS, Reardon CM, Orvek E, Nevedal AL, Lindquist J, Gifford AL, White L, King HA, DeLaughter K, Houston TK, Henderson B, Vega R, Kilbourne AM, Damschroder LJ. Merging Implementation Practice and Science to Scale Up Promising Practices: The Veterans Health Administration (VHA) Diffusion of Excellence (DoE) Program. Jt Comm J Qual Patient Saf. 2021 Apr;47(4):217-227. PMID: 33549485.
Livingston NA, Simpson T, Lehavot K, Ameral V, Brief DJ, Enggasser J, Litwack S, Helmuth E, Roy M, Rosenbloom D, Keane TM. Differential alcohol treatment response by gender following use of VetChange. Drug Alcohol Depend. 2021 Apr 1;221:108552. PMID: 33556659.
Nunez ER, Johnson SW, Qian SX, Powell WR, Walkey AJ, Wiener RS, Rinne ST. Patterns of Pulmonary Consultation for Veterans with Incident COPD. Ann Am Thorac Soc. 2021 Apr 01. Online ahead of print. PMID: 33794140.
Oppel EM, Mohr DC. Multilevel analysis exploring the relative importance of workplace resources in explaining nurses’ workload perceptions: Are we setting the right focus? Health Care Manage Rev. 2021 Apr-Jun 01; 46(2):E8-E17. PMID: 33630510.
Phillips KT, Stewart C, Anderson BJ, Liebschutz JM, Herman DS, Stein MD. A randomized controlled trial of a brief behavioral intervention to reduce skin and soft tissue infections among people who inject drugs. Drug Alcohol Depend. 2021 Apr 1;221:108646. PMID: 33677353.
Puzniak L, Gupta V, Yu KC, Ye G, Outterson K. The Impact of Infections on Reimbursement in 92 US Hospitals, 2015-2018. Am J Infect Control. 2021 Apr 20. PMID: 33891989.
Roncarati JS, Byrne TH, McInnes DK. Invited Commentary: Data sources that enumerate people experiencing homelessness in the United States: Opportunities and challenges for epidemiological research. Am J Epidemiol. 2021 Apr 16. Online ahead of print. PMID: 33861310.
Ruben MA, Kauth MR, Meterko M, Norton AM, Matza AR, Shipherd JC. Veterans’ Reported Comfort in Disclosing Sexual Orientation and Gender Identity. Med Care. 2021 Apr 01. Online ahead of print. PMID: 33797509.
Stefos T, Carey K, Shen ML, Poe S, Oh DH, Moran E. The Effect of Telehealth Services on Provider Productivity. Med Care. 2021 05 01; 59(5):456-460. PMID: 33821831.
Strombotne K, Sindelar J, Buckell J. Who, me? Optimism bias about US teenagers’ ability to quit vaping. Addiction. 2021 Apr 23. Online ahead of print. PMID: 33891783.
The post Recent publications from Boston University’s Department of Health Law, Policy and Management: August 2021 Edition first appeared on The Incidental Economist.Aaron E. Carroll's Blog
- Aaron E. Carroll's profile
- 42 followers